Abstract
Study design Prospective cohort study.
Objective The purpose of the present study was to identify the predictors of patient satisfaction with outcome after cervical laminoplasty for compressive cervical myelopathy.
Methods A cohort of 143 patients with compressive myelopathy who underwent cervical double-door laminoplasty between 2008 and 2011 was studied prospectively. The principal outcome was patient satisfaction with outcome at 1 year after surgery. Patient satisfaction was graded on an ordinal scale from 1 to 7. Subjective health-related quality of life (QOL) and objective disease-specific outcome was measured by Short Form-36 (SF-36) and the Japanese Orthopaedic Association (JOA) score, respectively, before surgery and at 1-year follow-up. We evaluated the association between patient satisfaction at 1-year follow-up and various baseline parameters, including patient demographics, duration of symptoms, comorbidities, imaging findings, JOA score, and SF-36 scores.
Results A total of 116 patients completed subjective and objective follow-up for a minimum of 1 year. Of 116 patients, 95 patients (81.9%) were satisfied with the outcome (“satisfied a little” or more). The unsatisfied group (“neutral” or less) showed significantly lower baseline SF-36 scores in bodily pain (BP), general health perceptions (GH), and vitality (VT) domains compared with the satisfied group. At the 1-year follow-up, SF-36 scores showed significant differences between the groups in all eight domains, whereas the JOA score showed no significant difference.
Conclusions Lower baseline QOL measured by SF-36 scores, specifically in BP, GH, and VT domains, are associated with lower satisfaction with outcome after cervical laminoplasty.
Keywords: cervical spine, myelopathy, laminoplasty, outcome, patient satisfaction
Introduction
Over the past decade, there has been increasing interest in the use of patient-based measures of medical care. Patient-based measures include generic measures, disease-specific measures, and measures of patient satisfaction. Measuring patient satisfaction has a variety of clinical and economic implications. For example, it can be used for validating the quality of care, developing patient care models, and facilitating quality improvement.1 2 3 Despite several potential benefits to both clinicians and patients, measurement of patient satisfaction has not been used effectively in clinical settings.
The assessment of outcome after cervical spine surgery has historically involved objective disease-specific scales, such as the Nurick score,4 the European myelopathy scale,5 the myelopathy disability index,6 and the Japanese Orthopaedic Association (JOA) score.7 Because these scales evaluate only physician-based outcomes, limited information is available regarding patient-based outcomes, including patient satisfaction, after cervical spine surgery. Identification of factors that determine patient satisfaction after surgery would be useful for improving the quality of care. Moreover, identifying predictors of patient satisfaction after surgery is of primary concern for surgeons.
The purpose of the present study was to identify the preoperative predictors of patient satisfaction with outcome after cervical laminoplasty for compressive cervical myelopathy.
Materials and Methods
Study Population
A cohort of 143 patients with compressive myelopathy who underwent cervical double-door laminoplasty between 2008 and 2011 was studied prospectively. The research protocol was approved by the Institutional Review Board of the authors' institute. The diagnosis of myelopathy was confirmed both by thorough neurologic examination and by imaging studies showing spinal cord compression, which is generally associated with an intramedullary high-intensity area on T2-weighted magnetic resonance imaging (MRI). Exclusion criteria included concurrent lumbar spine surgery, traumatic spinal cord injury, and other disorders that might impair motor function such as cerebral infarction, rheumatoid arthritis, or cerebral palsy. Based on these criteria, 20 patients were excluded. Of the remaining 123 patients, 116 patients completed the objective and subjective follow-up evaluations done at a minimum of 1 year (mean 35 ± 13 months; range: 14 to 55 months) after surgery. Six patients were lost to follow-up, and one patient died due to a malignant tumor. In addition to patient characteristics, the duration of symptoms and the severity of comorbidity were investigated. The severity of comorbidity was graded by the Cumulative Illness Rating Scale (CIRS).8 The procedure for double-door laminoplasty has been described in detail elsewhere.9
Imaging Parameters
Preoperative cervical alignment was measured as the C2/7 angle on a lateral radiograph taken in the neutral position. The range of motion between C2 and C7 was also measured on flexion-extension radiographs. All but one patient with a pacemaker underwent MRI before surgery. Preoperative MRI was analyzed using the following two parameters: transverse area of the spinal cord at the levels of maximal compression and intramedullary signal intensity (SI) changes on T2-weighted images. SI changes were classified as type 0 if no intramedullary high SI on T2-weighted images was noted, type 1 if a predominantly (>50%) faint and fuzzy border of high SI was noted, or type 2 if a predominantly (>50%) intense and well-defined border of high SI was noted.10 The classification of SI changes was performed independently by two blinded readers (A.K. and E.T.). If they disagreed with each other's reading, a third reader (A.S.) was consulted as a tiebreaker.
Subjective and Objective Outcomes
The principal outcome was patient satisfaction with outcome evaluated at the time of 1-year follow-up. This was assessed with the use of a paper questionnaire that asked the patient, “How satisfied are you with the outcome?” Patient satisfaction was graded on an ordinal scale from 1 to 7 (1, “very dissatisfied”; 2, “dissatisfied”; 3, “dissatisfied a little”; 4, “neutral”; 5, “satisfied a little”; 6, “satisfied”; and 7, “very satisfied”). The response was then dichotomized into two categories: satisfied and unsatisfied. The satisfied group comprised patients with grade 5 satisfaction (“satisfied a little”) or more, and the unsatisfied group comprised patients with grade 4 satisfaction (“neutral”) or less. Subjective health-related quality of life (QOL) and objective disease-specific function was measured by Short Form-36 (SF-36) and JOA scores, respectively, before surgery and at 1-year follow-up.
Statistical Analysis
Group data are presented as means ± standard deviations. Within-group comparisons were performed using the Wilcoxon signed rank test for paired samples, and between-group comparisons were made using the Mann-Whitney U test (except for the type of intramedullary SI on MRI, which was analyzed by the chi-square test). All data was analyzed using statistical software (SPSS version 17, SPSS Inc., Chicago, Illinois, United States).
Results
Patient Characteristics
Patients comprised 78 men and 38 women (mean age, 63 years; age range: 20 to 88 years). The follow-up rate was 95.1%. Patient characteristics, duration of symptoms, the severity of comorbidity measured by CIRS, and the levels of maximal compression are summarized in Table 1.
Table 1. Patient characteristics (n = 116).
| Characteristics | |
|---|---|
| Age (y) | 63.3 ± 12.7 |
| Gender (M/F) | 78/38 |
| Etiology of myelopathy | |
| Spondylosis | 77 (66%) |
| OPLL | 39 (34%) |
| Duration of symptom (mo) | 34.3 ± 47.2 |
| CIRS | 6.9 ± 3.1 |
| Level of the maximum compression | |
| C2–C3 | 2 |
| C3–C4 | 39 |
| C4–C5 | 48 |
| C5–C6 | 26 |
| C6–C7 | 1 |
Abbreviations: CIRS, Cumulative Illness Rating Scale; OPLL, ossification of posterior longitudinal ligament.
Note: Data are reported as numbers (%) or mean ± standard deviation.
Objective and Subjective Outcomes
Of the 116 patients, 95 (81.9%) were satisfied with the outcome (“satisfied a little” or more; Fig. 1). These 95 patients were categorized into the satisfied group, and the remaining 21 patients (“neutral” or less) were categorized into the unsatisfied group. At the 1-year follow-up, the mean SF-36 scores improved significantly compared with baseline scores in all eight domains (Fig. 2). The SF-36 general health perceptions (GH) domain showed the smallest postoperative change in the mean value (3.6 ± 15.8) among the eight domains. The median JOA score also improved significantly from a preoperative score of 11 to a postoperative score of 14 (p < 0.0001, Wilcoxon signed rank test).
Fig. 1.

The distribution of grades for patient satisfaction with outcome evaluated at 1-year follow-up.
Fig. 2.
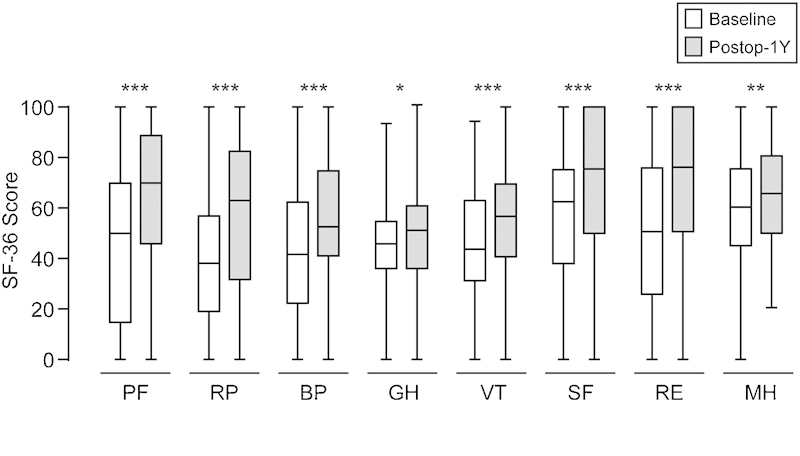
Postoperative changes in SF-36 scores. White bars indicate baseline values and gray bars indicate 1-year follow-up values. SF-36 scores increase significantly compared with baseline values in all eight domains. *p < 0.05, **p < 0.01, ***p < 0.001; the Wilcoxon signed rank test. Abbreviations: BP, bodily pain; GH, general health perceptions; MH, mental health; PF, physical functioning; RE, role-emotional; RP, role-physical; SF, social functioning; SF-36, MOS 36-Item Short-Form Health Survey; VT, vitality.
Comparisons between the Satisfied and Unsatisfied Groups
To identify parameters for predicting patient satisfaction with outcome after surgery, various baseline data, including patient demographics, imaging findings, and preoperative subjective and objective outcomes, were compared between the satisfied and unsatisfied groups (Table 2). The mean age and the severity of comorbidity evaluated by CIRS were higher in the unsatisfied group than in the satisfied group (67.4 versus 62.4, and 7.8 versus 6.7, respectively), although the difference was not significant. The ratio of type 2 SI, which is reportedly associated with poor functional outcome, was also higher in the unsatisfied group than in the satisfied group (0.43 versus 0.35); however, the difference was not significant. On the other hand, the unsatisfied group had significantly lower SF-36 scores in bodily pain (BP), GH, and vitality (VT) domains than the satisfied group.
Table 2. Comparison of patient demographics and baseline outcomes between satisfied and unsatisfied groups.
| Parameters | Satisfied group | Unsatisfied group | p value |
|---|---|---|---|
| Age at the operation (y) | 62.4 ± 12.6 | 67.4 ± 12.7 | 0.071 |
| Gender (M/F) | 62/33 | 16/5 | 0.334 |
| Ratio of OPLL patients | 0.35 (33/95) | 0.29 (6/21) | 0.588 |
| Duration of symptom (mo) | 34.5 ± 49.5 | 33.8 ± 34.9 | 0.412 |
| CIRS | 6.7 ± 3.2 | 7.8 ± 2.2 | 0.052 |
| Radiograph | |||
| C2/7 angle (degree) | 12.4 ± 10.0 | 10.1 ± 10.7 | 0.257 |
| Range of motion (degree) | 35.8 ± 12.7 | 36.2 ± 10.0 | 0.917 |
| MRI | |||
| Narrowest canal area (mm3) | 62.4 ± 16.4 | 66.5 ± 12.7 | 0.158 |
| Ratio of type 2 intramedullary SI | 0.35 (33/94) | 0.43 (9/21) | 0.505 |
| JOA score | 11.0 ± 2.7 | 11.5 ± 1.6 | 0.628 |
| SF-36 | |||
| Physical functioning | 46.5 ± 28.3 | 38.8 ± 27.4 | 0.323 |
| Role-physical | 39.2 ± 28.6 | 39.6 ± 34.1 | 0.880 |
| Bodily pain | 47.7 ± 26.3 | 33.5 ± 18.3 | 0.031a |
| General health perceptions | 46.2 ± 17.5 | 35.5 ± 14.1 | 0.018a |
| Vitality | 45.4 ± 21.3 | 35.2 ± 13.9 | 0.027a |
| Social functioning | 57.6 ± 27.8 | 61.7 ± 31.8 | 0.511 |
| Role-emotional | 47.8 ± 31.8 | 53.3 ± 37.4 | 0.581 |
| Mental health | 58.7 ± 21.1 | 48.8 ± 23.0 | 0.094 |
Abbreviations: CIRS, Cumulative Illness Rating Scale; JOA, Japanese Orthopaedic Association; OPLL, ossification of posterior longitudinal ligament; SF-36, MOS 36-Item Short-Form Health Survey; SI, signal intensity.
Note: Unless otherwise indicated, values are expressed as the mean ± standard deviation.
Statistically significant (p < 0.05, Mann-Whitney U test or chi-square test).
Comparisons of postoperative outcomes between the satisfied and unsatisfied groups are summarized in Table 3. At the 1-year follow-up, the unsatisfied group showed a lower mean JOA score than the satisfied group (13.2 versus 14.2), but the difference was not significant. When postoperative JOA scores were analyzed separately for the six function categories (motor functions of upper and lower limbs; sensory functions of upper limbs, lower limbs, and torso; and bladder function), only sensory function of upper limbs showed a significant difference between the satisfied and the unsatisfied groups (1.3 ± 0.5 versus 1.0 ± 0.6, p = 0.010, Mann-Whitney U test). In contrast, the satisfied group showed significantly higher SF-36 scores than the unsatisfied group in all eight domains. With regard to JOA score improvement, 55 patients showed good score improvement after surgery (>50%). Although the ratio of patients with good improvement was higher in the satisfied group than the unsatisfied group, there was no statistically significant difference between the groups (49/95 versus 6/21, p = 0.090, Fischer exact test).
Table 3. Comparison of postoperative outcomes between satisfied and unsatisfied groups.
| Parameters | Satisfied group | Unsatisfied group | p value |
|---|---|---|---|
| JOA score | 14.2 ± 2.1 | 13.2 ± 2.1 | 0.052 |
| SF-36 | |||
| Physical functioning | 69.4 ± 24.9 | 49.5 ± 27.7 | 0.003a |
| Role-physical | 64.3 ± 28.9 | 33.8 ± 28.3 | <0.001a |
| Bodily pain | 59.7 ± 22.5 | 41.8 ± 25.2 | 0.001a |
| General health perceptions | 51.0 ± 19.9 | 33.5 ± 16.2 | <0.001a |
| Vitality | 57.6 ± 19.5 | 42.2 ± 22.5 | 0.007a |
| Social functioning | 77.8 ± 24.1 | 61.3 ± 22.3 | 0.003a |
| Role-emotional | 72.4 ± 29.8 | 37.1 ± 32.2 | <0.001a |
| Mental health | 68.2 ± 19.5 | 53.3 ± 16.6 | 0.002a |
Abbreviations: JOA, Japanese Orthopaedic Association; SF-36, MOS 36-Item Short-Form Health Survey.
Note: Values are expressed as the mean ± standard deviation.
Statistically significant (p < 0.05, Mann-Whitney U test).
Three patients (two in the satisfied group and one in the unsatisfied group) experienced C5 palsy, which recovered spontaneously within 3 months after surgery. Six patients (five in the satisfied group and one in the unsatisfied group) had cerebrospinal fluid leakage, which also recovered spontaneously within 2 weeks after surgery. The incidence of these complications did not differ significantly between the two groups (p > 0.99 and p = 0.44, respectively, Fisher exact test).
Discussion
This prospective study evaluated various patient parameters and baseline functional outcomes as predictors of postoperative patient satisfaction. The key finding of this study was that lower preoperative QOL measured by SF-36 scores, specifically in the BP, GH, and VT domains, was associated with lower postoperative satisfaction. Another finding was that patient satisfaction was closely associated with the current state of patient-based outcome rather than that of physician-based functional outcome. These results highlight the importance of patient-based outcome as a determinant of patient satisfaction after cervical spine surgery.
Predictors of patient satisfaction have been reported almost exclusively in patients undergoing lumbar spine surgery. Soroceanu et al examined the relationship between preoperative expectations, satisfaction, and functional outcomes in patients undergoing lumbar and cervical spine surgery.11 They identified preoperative expectations as a predictor of patient satisfaction after surgery; however, the result was obtained from a mixed patient group, the majority of whom underwent lumbar spine surgery. To the best of our knowledge, no research has been reported in the current literature examining predictors of satisfaction exclusively in patients undergoing cervical spine surgery.
Predictors of patient satisfaction after lumbar spine surgery include patients' assessments of their own health, comorbidity, and the degree of expectations for surgery.11 12 13 Katz et al demonstrated that a powerful predictor of satisfaction was patients' rating of their own health, which was derived from a simple question: “How would you rate your health?”12 This result is similar to the present result that patients who were not satisfied with their outcome had significantly lower preoperative general health perception as measured by the SF-36 GH domain. Moreover, Yee et al found that the SF-36 GH domain predicted patients with a high expectation for surgery and that patients with high expectation showed greater functional recovery after surgery.13 These results are similar to the present result in cervical spine surgery that satisfied patients showed significantly higher preoperative scores in the SF-36 GH and VT domains. Although the underlying common mechanism remains to be elucidated, poor health perceptions and low vitality may play a role in magnifying the perception of residual symptoms after surgery, leading to lower satisfaction with outcome.
Several studies have shown predictors of functional outcome after surgical treatment of cervical spondylotic myelopathy.14 15 16 These include age, duration of symptoms, preoperative neurologic function, and SI change of the spinal cord on MRI. In the present study, none of these factors differed significantly between the satisfied and unsatisfied groups. These results suggest that patient dissatisfaction does not stem solely from a poor functional outcome, and that traditional objective measures are insufficient for predicting patient satisfaction. Because the vast majority of studies have used physician-based outcome for the analysis of predictors, further detailed studies are needed to identify predictors of patient-based outcome after cervical spine surgery.
This study has several important limitations. First, this study did not evaluate the influence of patient expectation for surgery. Patient expectation has been suggested as a predictor of patient satisfaction after lumbar spine surgery.13 Thus, future studies should include patient expectation as a candidate predictive factor. Second, because this study focused on preoperative predictors of patient satisfaction, we have limited information on perioperative complications such as axial pain, which might affect patient satisfaction. Detailed prospective studies on bodily pain would be valuable, because unsatisfied patients showed significantly lower SF-36 BP scores than satisfied patients, both at baseline and at 1-year follow-up. Finally, the small number of patients in the unsatisfied group suggests increased possibility of type II statistical error. A larger patient cohort is required to allow more accurate comparisons between the groups.
Predictors of poor surgical outcome are useful if they can be modified and if modification of the factors improves outcomes. It is unclear whether general health perceptions are modifiable before surgery; however, given the smallest postoperative change in SF-36, it might be difficult to gain a dramatic change in general health perception by short-term interventions before surgery. Careful preoperative explanation of the course and outcome is recommended for patients with poor baseline general health perceptions because low fulfillment of expectations is associated with low patient satisfaction after spine surgery.11 In particular, it may be important to convey information about the possibility of persistent numbness and pain in the extremities even after complete decompression of the spinal cord, because the unsatisfied group showed significantly deteriorated sensory function in the upper extremities.
It remains to be elucidated how much surgeons should pay attention to patient satisfaction and whether surgeons should alter the decision-making process to please patients rather than adhere to evidence-based medicine. Lyu et al recently demonstrated that patient satisfaction is not related to standard process-of-care measures that have long been used to increase surgical quality.17 Moreover, patient satisfaction may be driven by the patients' feelings and emotions at the moment of surveillance rather than the assessment of the entire experience.18 Given the limited availability of universal and standardized instruments in measuring patient satisfaction, it may be too early to treat patients solely on the basis of patient satisfaction. Further study is required before patient satisfaction is widely applied to surgeons as a quality indicator.
Footnotes
Disclosures The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this article.
References
- 1.Carr-Hill R A. The measurement of patient satisfaction. J Public Health Med. 1992;14(3):236–249. [PubMed] [Google Scholar]
- 2.Ware J E Jr, Davies-Avery A, Stewart A L. The measurement and meaning of patient satisfaction. Health Med Care Serv Rev. 1978;1(1):3–15. [PubMed] [Google Scholar]
- 3.Ware J E Jr, Hays R D. Methods for measuring patient satisfaction with specific medical encounters. Med Care. 1988;26(4):393–402. doi: 10.1097/00005650-198804000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Nurick S. The pathogenesis of the spinal cord disorder associated with cervical spondylosis. Brain. 1972;95(1):87–100. doi: 10.1093/brain/95.1.87. [DOI] [PubMed] [Google Scholar]
- 5.Herdmann J, Linzbach M, Krzan M, Dvorák J, Bock W J. Berlin: Springer; 1994. The European Myelopathy Score; pp. 266–268. [Google Scholar]
- 6.Casey A T, Bland J M, Crockard H A. Development of a functional scoring system for rheumatoid arthritis patients with cervical myelopathy. Ann Rheum Dis. 1996;55(12):901–906. doi: 10.1136/ard.55.12.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yonenobu K, Abumi K, Nagata K, Taketomi E, Ueyama K. Interobserver and intraobserver reliability of the Japanese Orthopaedic Association scoring system for evaluation of cervical compression myelopathy. Spine (Phila Pa 1976) 2001;26:1890–1894. doi: 10.1097/00007632-200109010-00014. [DOI] [PubMed] [Google Scholar]
- 8.Salvi F, Miller M D, Grilli A. et al. A manual of guidelines to score the modified cumulative illness rating scale and its validation in acute hospitalized elderly patients. J Am Geriatr Soc. 2008;56(10):1926–1931. doi: 10.1111/j.1532-5415.2008.01935.x. [DOI] [PubMed] [Google Scholar]
- 9.Kimura A, Seichi A, Inoue H, Hoshino Y. Long-term results of double-door laminoplasty using hydroxyapatite spacers in patients with compressive cervical myelopathy. Eur Spine J. 2011;20(9):1560–1566. doi: 10.1007/s00586-011-1724-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chen C J, Lyu R K, Lee S T, Wong Y C, Wang L J. Intramedullary high signal intensity on T2-weighted MR images in cervical spondylotic myelopathy: prediction of prognosis with type of intensity. Radiology. 2001;221(3):789–794. doi: 10.1148/radiol.2213010365. [DOI] [PubMed] [Google Scholar]
- 11.Soroceanu A, Ching A, Abdu W, McGuire K. Relationship between preoperative expectations, satisfaction, and functional outcomes in patients undergoing lumbar and cervical spine surgery: a multicenter study. Spine (Phila Pa 1976) 2012;37:103–108. doi: 10.1097/BRS.0b013e3182245c1f. [DOI] [PubMed] [Google Scholar]
- 12.Katz J N, Stucki G, Lipson S J, Fossel A H, Grobler L J, Weinstein J N. Predictors of surgical outcome in degenerative lumbar spinal stenosis. Spine (Phila Pa 1976) 1999;24:2229–2233. doi: 10.1097/00007632-199911010-00010. [DOI] [PubMed] [Google Scholar]
- 13.Yee A, Adjei N, Do J, Ford M, Finkelstein J. Do patient expectations of spinal surgery relate to functional outcome? Clin Orthop Relat Res. 2008;466(5):1154–1161. doi: 10.1007/s11999-008-0194-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holly L T, Matz P G, Anderson P A. et al. Clinical prognostic indicators of surgical outcome in cervical spondylotic myelopathy. J Neurosurg Spine. 2009;11(2):112–118. doi: 10.3171/2009.1.SPINE08718. [DOI] [PubMed] [Google Scholar]
- 15.Karpova A, Arun R, Davis A M, Kulkarni A V, Massicotte E M, Mikulis D J, Lubina Z I, Fehlings M G. Predictors of surgical outcome in cervical spondylotic myelopathy. Spine (Phila Pa 1976) 2013;38:392–400. doi: 10.1097/BRS.0b013e3182715bc3. [DOI] [PubMed] [Google Scholar]
- 16.Tetreault L A Karpova A Fehlings M G Predictors of outcome in patients with degenerative cervical spondylotic myelopathy undergoing surgical treatment: results of a systematic review Eur Spine J 2013; February 6 (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 17.Lyu H, Cooper M, Freischlag J A, Makary M A. Patient satisfaction as a possible indicator of quality surgical care—reply. JAMA Surg. 2013;148(10):986–987. doi: 10.1001/jamasurg.2013.3411. [DOI] [PubMed] [Google Scholar]
- 18.Kane R L, Maciejewski M, Finch M. The relationship of patient satisfaction with care and clinical outcomes. Med Care. 1997;35(7):714–730. doi: 10.1097/00005650-199707000-00005. [DOI] [PubMed] [Google Scholar]


