Abstract
Background Basilar thumb arthritis, or first carpometacarpal arthritis, is a common condition, predominantly affecting women. Surgical treatment of this condition is highly varied. One common method consists of trapezium excision and a concomitant procedure for treatment of the “floating” thumb metacarpal. That procedures vary suggests that no method has an “outcome” advantage over another. However, the frequency of side effects is higher in more complex procedures.
Question/Purposes We speculated that in vitro testing might identify a potential outcome difference that has been difficult to measure in vivo. Since the more complex procedure to treat this condition has a higher frequency of clinical side effects, we hoped to determine its functional value compared with less complex procedures.
Methods A two-degrees-of-freedom biomechanical cadaver study examined simulated pinch strength and metacarpal subsidence during pinch. Three methods were compared with each other and against the normal pretreatment state: trapezial excision alone; trapezial excision and suture suspensionplasty (TESS); and trapezial excision followed by a ligament reconstruction using one-half of the flexor carpi radialis and tendon interposition (LRTI).
Results After TESS, the loaded mean height of the arthroplasty space was 1.20 cm. This was statistically less than the pretreatment height of 1.50 cm (P < 0.05). However, the height maintained after LRTI (1.00 cm) was also statistically less than pretreatment state (P < 0.05) and less than TESS (P < 0.05). Trapezial excision alone was least successful at maintaining height. In contrast, the mean key pinch measured after treatment could not be predicted by treatment employed.
Conclusions In summary, the tested technique of TESS appears to be biomechanically sound as related to maintenance of first metacarpal height. In in vitro testing it is superior to excision alone and at least equal to the ligament reconstruction method tested. Analysis of our data shows that 96% of the overall height (distance) maintained post excision is explained by surgical state.
Clinical Relevance Trapezial height is preserved using support schemes in a laboratory setting. In the in vivo postsurgical state, clinical intrinsic muscle function may be superior when support is used compared with trapeziectomy alone.
Keywords: Basilar thumb arthritis, first carpometacarpal (1st CMC) arthritis, in-vitro testing, biomechanical cadaver study, trapezial excision
Basilar thumb arthritis is a common condition, which has a prevalence of 33% in a radiological study by Armstrong et al.1 The ideal treatment method has not been found if one is to judge by the number of published techniques ranging from arthrodesis2 to prosthetic arthroplasty3 to an isolated trapeziectomy4 5 to multiple variations of ligament reconstruction and tendon interposition.6 7 8 9 10 11 12
Meta-analysis of published material on this common condition has been problematic since reports are small and have not standardized measurement of X-rays and clinical impact. Nonetheless, Wajon and coworkers have completed a review of the available literature up to 2009 and found (1) no clear clinical benefit between procedures reported, (2) a risk of bias among reporters, and (3) a substantially increased risk of an adverse effect (RR 2.21) when the more complex (ligament reconstruction) procedure was performed.13.
The purpose of our study was to study the effectiveness of three different surgical procedures in maintaining the height of the arthroplasty space in a cadaver model following a trapeziectomy and to determine whether this affected the simulated key pinch strength.
Materials and Methods
This in vitro biomechanical study was performed using 8 fresh frozen below- elbow cadaver arms. There were 5 right and 3 left arms. Seven were from male patients and one was from a female.
We measured the key pinch force with a transducer after applying a physiological load to the extrinsic and intrinsic thumb tendons based on a virtual five-link model of the thumb described by Giurintano et al.14 Simultaneously we also measured the height between the base of the first metacarpal and the scaphoid radiographically in the following situations: (1) intact trapezium, (2) trapezial excision without stabilization, (3) trapezial excision with suture stabilization using a bone anchor in the index metacarpal base (TESS), and (4) a ligament reconstruction using half of the flexor carpi radialis (FCR) tendon (LRTI) as described by Burton and Pellegrini (1986).7 Subsidence was measured radiographically during simulated key pinch with an intact trapezium and following each type of reconstruction. All eight adult cadaveric specimens were tested sequentially following each surgical procedure (surgical state).
Our cadaveric model mimicked the act of key pinch. Cooney et al evaluated upper extremity electromyographic activity for key pinch.15 Thumb motors were designated primary or secondary on the basis of electrical potential activity. The primary motors were found to be the flexor pollicis longus, adductor pollicis, and opponens pollicis. The secondary motors were the extensor pollicis longus and brevis. The first dorsal interosseous was discussed as being “synergistically active through index finger function.”
In our model, thumb key pinch was performed against a transducer, not the index finger; therefore the first dorsal interosseous was not included. To closely approximate the actual work that each muscle is performing, we used the tension fraction for each muscle, as described by Brand et al.16 They weighed the muscle mass of each forearm muscle in five relatively normal-sized cadaver specimens, converted the mass to volume, and then divided the volume by the mean fiber length in that muscle. This gave the “physiologic” cross-sectional area of that muscle. The cross-sectional areas of the muscles of a given forearm and hand were then totaled, and each muscle's percentage of the total was calculated. This percentage, which they termed the tension fraction for that muscle, represents the muscle's percentage contribution to the total single-contraction tension capability of all muscles below the elbow. The tension fractions for the muscles involved in key pinch are shown in Table 1 as “whole-arm” tension fractions, and study-specific fractions. For the purpose of this study, we were interested in the relative tension fractions, found by dividing whole-arm tension fractions by the lowest value (1.3%), thereby converting that same lowest value to 1 in the column of study-specific tension fractions and, similarly, altering the other study-specific tension fraction values so as to simplify the math for actual study load application. These are shown in Table 1 as “study-specific” tension fractions, all numbers ≥ 1.
Table 1. Tension fractions and applied loads (at a clinically meaningful pinch force) on motors of key pinch.
| Motor | Whole-arm tension fraction |
Study-specific tension fraction | Actual study load N (lb) |
|---|---|---|---|
| ADD Pol (Whole) | 3% | 2.3 | |
| ADD Pol (Transverse) | − | − | 11.65 N (2.6 lb) |
| ADD Pol (Oblique) | − | − | 11.65 N (2.6 lb) |
| FPL | 2.7% | 2.1 | 23.31 N (5.24 lb) |
| OPP Pol | 1.9% | 1.5 | 16.73 N (3.76 lb) |
| EPL | 1.3% | 1.0 | 11.12 N (2.5 lb) |
| EPB | 1.3% | 1.0 | 11.12 N (2.5 lb) |
Combining electromyographic (EMG) data from Cooney et al and tension fraction data from Brand et al enabled us to choose motors and relative loading to simulate key pinch. To assist in maintaining normal anatomic vectors, eyelet pulleys were employed in locations specified in the following paragraphs. All pulleys employed were positioned to maintain a 1:1 reduction ratio. Weights delivering load to the target insertions/tendons were allowed to displace fully during the successive testing sessions. All cadavers were tested in one setting and not allowed to desiccate during testing. None of the suture–tendon interfaces failed during the testing process.
The adductor pollicis transverse and oblique heads were exposed at the insertion into the adductor aponeurosis at the thumb metacarpophalangeal (MP) joint. Number 5 Ethibond™ suture (Ethicon, Inc., Ciudad Juarez, Mexico) was woven in Bunnell fashion into the distal tendon portion of each. A metal eyelet screw (#214 Eyelet Screw, GateLatch, Gearhart, OR, USA) pulley was secured to bone at the origin of each adductor head. The transverse head pulley was placed in the volar mid third metacarpal. The oblique head pulley was placed in the volar capitate. The sutures were passed through their respective pulleys.
The flexor pollicis longus (FPL) tendon was exposed proximal to the radiocarpal joint. An eyelet pulley was placed in the distal radius at the volar ridge level along the course of the FPL tendon. The FPL was transected at the musculotendinous junction. The tendon was passed through the pulley and a suture weave performed in the proximal tendon.
The opponens pollicis insertion was exposed at the radial thumb MP joint. A suture weave was performed in the distal tendon. An eyelet pulley was placed in the hamate. The opponens originates off the radial carpals and transverse carpal ligament (TCL). So as not to violate our study area (first CMC joint) with the metal pulley, the transverse carpal ligament was used as an initial pulley. The suture simulating th tendon passed deep to the TCL at the opponens origin and then passed through the metal pulley at the volar hamate.
The extensor pollicis longus (EPL) tendon was exposed proximal to the Lister tubercle, transected at the musculotendonous junction, secured, and passed through an eyelet pulley placed in the dorsal distal radius ∼3 cm proximal to the Lister tubercle.
The extensor pollicis brevis (EPB) tendon was exposed proximal to the first dorsal compartment, transected at the musculotendonous junction, secured, and passed through an eyelet pulley placed in the dorsoradial distal radius ∼2 cm proximal to the first dorsal compartment.
To prepare for the future ligament reconstruction procedure, the radial half of the FCR was released proximally at the musculotendinous junction and split distally to the 2nd metacarpal base in all specimens. The FCR was not loaded during testing.
All dynamic sutures were passed proximally through the forearm and securely tied to monofilament fishing line (Monofilament 25# Test [XT3025–15]; Berkley, Spirit Lake, IA).
Each forearm was mounted in neutral rotation on a stable platform. A 4.0-mm diameter threaded stainless steel pin was passed from radial to ulnar transversely through the mid to distal third junction of the radius and ulna, then passed through a preformed hole in the platform, and then secured to the platform with a nut. A second 4.0 mm diameter threaded pin was passed through the index and long metacarpal midshafts in a similar fashion and also secured to the platform. No motion was observed at the forearm or wrist during load testing.
Motion at the first CMC joint was free. The thumb pulp rested in a key pinch position against a force transducer (manufactured and calibrated internally at the University of Minnesota Biomechanics Laboratory, Minneapolis, MN). The plate of the force transducer simulated a stabilized index finger. The force transducer consisted of a lever arm connected to a load cell attached to a stainless steel post. Depression of the lever arm against the load cell provided a direct measure of the key pinch strength. Figs. 1a–c depict the model described. The force transducer plate is seen immediately below the thumb pulp, the forearm and hand are secured to the horizontal plate, and the lines from tendons to free-hanging weights are visible.
Fig. 1.
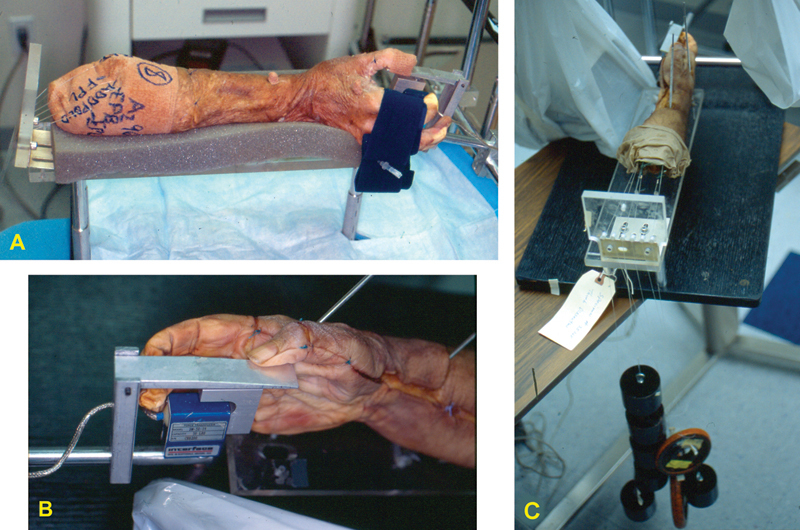
(a) Secured cadaveric arm (elbow to hand) plus tendon lines and pinch transducer (see text for a more complete description). (b) Palm side view of loaded pinch transducer. The force plate is positioned to resist flexion of the thumb pulp, in effect acting as the index distal phalanx/pulp region that would be contacted during key (c) Top-down view of prepared test specimen with freely suspended weights.
The monofilament line secured to our motors was passed proximally along the platform. Each line passed through a vertically oriented plastic block that contained 3-mm diameter holes with smooth tapered edges. The block acted as a proximal 1:1 pulley through which load was applied to the individual motors. The motors were loaded with weights secured to the monofilament line. Pinch strength was measured in units of pounds and observed on a digital display.
Actual load applied to each motor with calibrated weights is shown in Table 1. These loads were proportionate to the relative (study-specific) tension fractions of the muscles, as outlined previously. No load exceeded the strength of the weakest possible link/interface. Two weaknesses to the study are noted here. First, we did not load the system to failure to find an upper loading limit. Instead, we loaded the system until we measured a clinically significant pinch force. Two, the loads (weights) were able to travel in an unrestricted manner. That is, unlike muscles that have a specific excursion, the weights had no specific limit to their excursion. Thus, it is possible that the pinch effectiveness of each surgical state is overestimated. Note that all specimens were tested three times in each state. All values recorded for results comparison represent the average of these three tests.
A mini C-arm (Hologic Inc.; Burlington, MA) was used to obtain a posterior-to-anterior view perpendicular to the long axis of the trapezium. The first metacarpal, second metacarpal, trapezium, and scaphoid were included in the image. A 5-cm diameter standardized circular radiographic marker (Biomet, Inc., Warsaw, IN) was placed volar to the metacarpals in the A/P plane of the first CMC joint to correct for image magnification. Loaded C-arm images and key pinch strength were recorded for each specimen for each of the four testing states.
Each specimen was tested in the following manner: After setup in the schema just described, the thumb metacarpal base to distal scaphoid height was measured in the intact specimen, post trapeziectomy, post TESS, and finally post LRTI. The pinch strength was measured using the motors and loads just described. An image magnification value was first determined using a 5-cm marker (Fig. 2). All further measurements were multiplied by the magnification factor. The height of the trapezial space was measured directly. The proximal point of measure was at the intersection of a line extending through the central axis of the scaphoid and a perpendicular to this line located at the distal scaphoid articular margin. The distal point of measure was at the intersection of a line extending through the central axis of the first metacarpal and a perpendicular to this line extending through the central concavity of the articular margin. The C-arm images were stored on disk and evaluated with Adobe Photoshop software (Adobe, Adobe.com). The images were analyzed blinded to a member of this study (FW) who was not involved in the data acquisition.
Fig. 2.
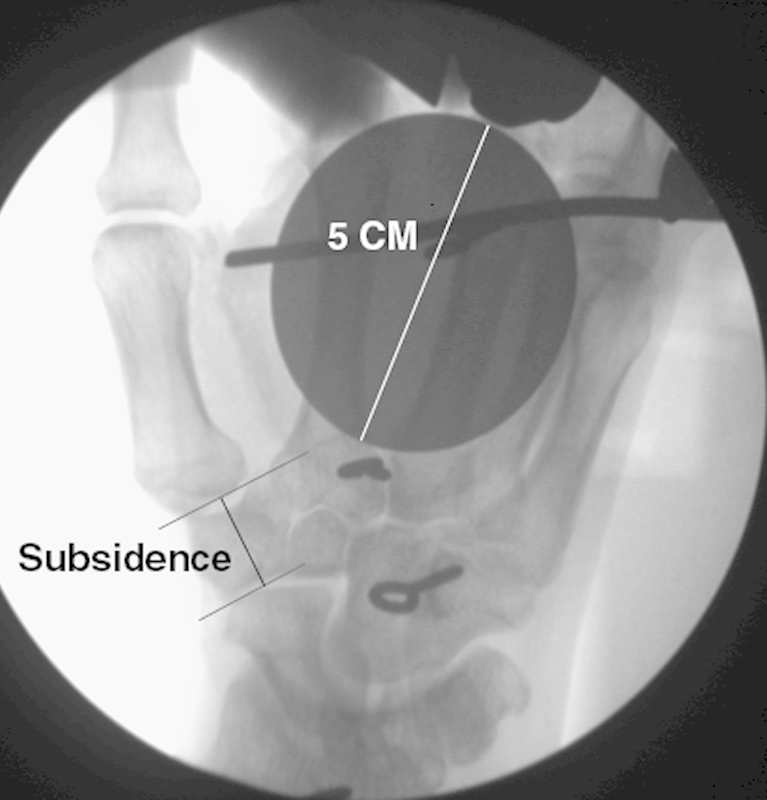
Thumb image X-ray via C-arm. The marker used to gauge image magnification and the view/location used to measure trapezial height are shown.
The method of TESS employed used a Mitek™ G2 suture anchor (DePuy Mitek, Inc., Raynham, MA). Barber et al previously studied this tool and found it to be of sufficient strength to be used in the hand and wrist.17 The placement of the anchor and the suture path through the first metacarpal are shown in Fig. 3a, b. The end of the suture is sewn into the abductor pollicis longus insertion in part to reattach what was partially released to accomplish trapezial excision and also so as to have the tendon act as a button. The suture is tied so as to enable it to slide through the pulley of the suture anchor, thus creating an internal traction force to narrow the space between the first and second metacarpals.
Fig. 3.
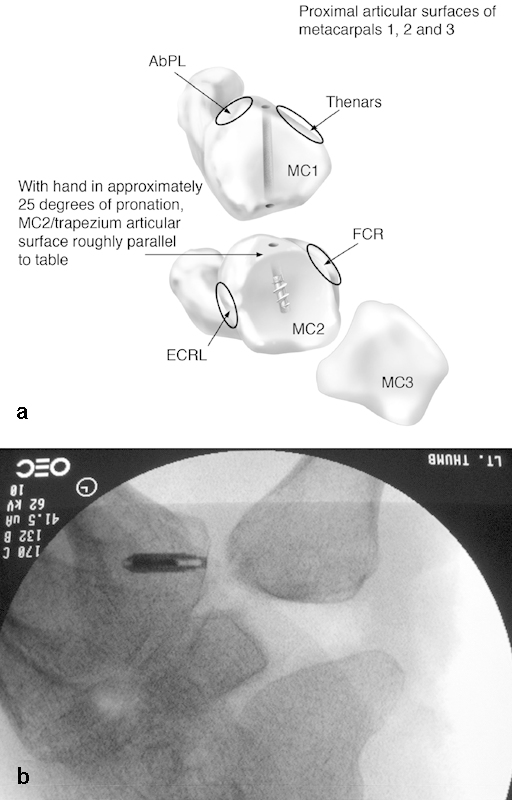
(a) Path of suture through first metacarpal in TESS procedure. A generic suture anchor screw is illustrated; the actual anchor tested is noted in text). (b) In vivo clinical appearance of first MC to 2nd MC relative to scaphoid with anchor in place.
As previously noted, the method of ligament reconstruction employed has been described by Burton and Pellegrini.7 In particular, we took care to bring half of the FCR through the base of the metacarpal along the same path previously employed by the suture in the suture suspensionplasty (Fig. 3a) with the additional step of looping the FCR around its own insertion and then tightening this as much as possible back upon itself and securing the tendon-to-tendon weave with the suture.
Statistical Analysis
We compared loaded mean height in the three surgical states, and in the pre-treatment state, by one-way analysis of variance (ANOVA) using SAS 9.3 for Windows (SAS Institute, Cary, NC, USA). We used the Tukey Honestly Significant Difference (HSD) to compare state means post hoc at a significance level (α) of 0.05. We estimated effect size (as η2) from the ratio of treatment sum of squares (SS) to total SS. We examined pinch strength the same way.
Results
The mean trapezial space height with the thumb loaded is shown for the intact state and each surgical state tested in Fig. 4. The one-way ANOVA was strongly significant (P < 0.001), and all states were different from each other at P < 0.05 by post hoc Tukey HSD. The intact-specimen mean trapezial height was 1.50 cm (standard deviation (sd) = 0.12 cm). After trapeziectomy alone the first metacarpal was found to collapse into the trapezial space with simulated pinch loading. This collapse was near total. The post-trapeziectomy mean height with loading was 0.100 cm (sd = 0.12 cm). The post-trapeziectomy mean height decrease was statistically significant compared with the intact specimen (P < 0.05) as well as the other methods tested. After TESS, the loaded mean height was 1.20 cm (sd = 0.117 cm). After LRTI the loaded mean height was 1.00 cm (sd = 0.12 cm). The height in LRTI was statistically different from that in the TESS method (P < 0.05) and the intact specimen (P < 0.05). The TESS maintenance of height appeared most similar to the intact state. However, TESS and the other two surgical states tested were statistically different from the intact state, with 96% of overall height variance (the effect size) explained by specific state.
Fig. 4.
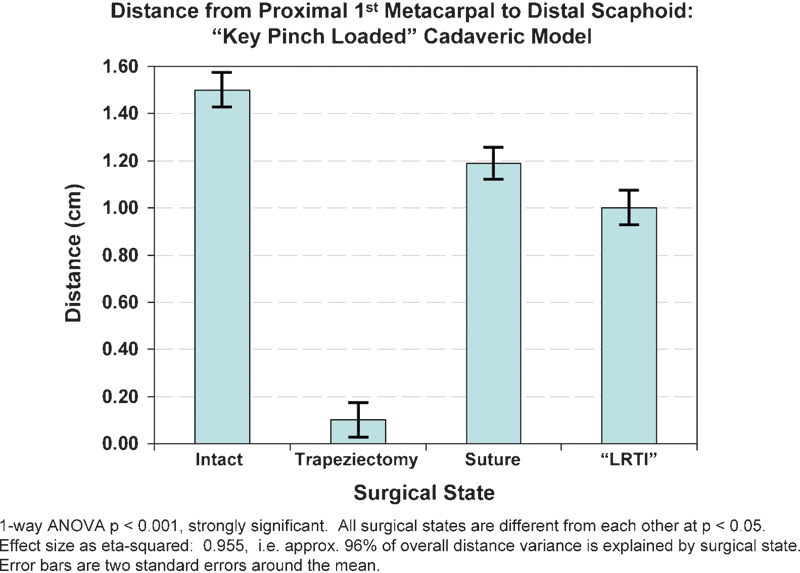
Graph showing trapezial space during pinch loading with intact trapezium, after trapeziectomy alone, after LRTI, or TESS (marked “Suture”). Error bars included.
Using identical motor loading parameters, the mean pinch strength for each state is shown in Fig. 5. The intact specimens' mean strength was 32.92 N (7.40 lbs) (SD 8.85 N [1.99 lbs]). After trapeziectomy alone the strength decreased to 25.35 N (5.70 lbs) (SD 9.25 N [2.08 lbs]). After TESS the strength improved to 29.40 N (6.61 lbs) (SD 7.16 N [1.61 lbs]). After LRTI the strength was 25.09 N (5.64 lbs) (SD 8.63 N [1.94 lbs]), lower than that seen after trapeziectomy alone. However, the one-way ANOVA was not significant; thus, no state was different from any other. Surgical state explained 14% (the effect size) of overall pinch variance.
Fig. 5.
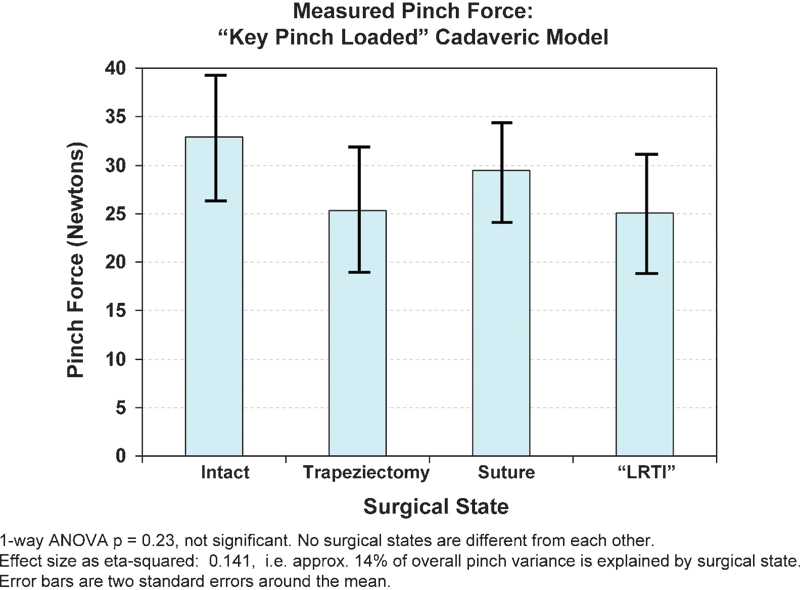
Graph showing pinch force with intact trapezium, after trapeziectomy alone, after LRTI, or TESS (marked “Suture”). Error bars included.
Discussion
Many common hand conditions have multiple published, and probably more “practiced,” surgical treatment options. Trapezial excision, with or without ligament reconstruction and tendon interposition, has gained popularity and acceptance over the years, and this treatment has reported good or excellent outcomes in many, but not all patients (73–94%), as previously described.4 5 6 7 8 9 10 11 12 18 Metacarpal subsidence, insufficient pain relief, weakness, and instability have been reported with the LRTI procedure and the other procedures previously noted. Unfortunately, a single biomechanical study cannot settle the debate regarding the best treatment option. Logically, and similar to predicted effect of metacarpal shortening on intrinsic muscle function as studied by Meunier et al,19 clinical outcome should correlate with maintenance of the most normal muscle length based upon the known impact upon muscle force potential calculated using Blix or Starling's curves. In this context, the following biomechanical observations may be of note:
Biomechanically significant differences between the three tested procedures exist. Logically, if the biomechanically observed difference in trapezial space height could be maintained in the clinical setting, this would be mechanically preferable in the two degrees of freedom tested.
Similarly, if the observed testing differences between trapezial excision alone versus ligament reconstruction versus suture suspensionplasty were maintained in the clinical setting, suture suspensionplasty would be mechanically preferable in the two degrees of freedom tested.
The greatest weakness of the current model is the failure to account for muscle excursion in our loading model. Had the loads applied been forced to occur within a specific excursion, the measured pinch loads would be expected to differ and might be significantly different between states.
Dorsal-to-volar and medial-to-lateral stability of the first CMC are almost certainly important related to biomechanical testing and clinical outcome. These variables were not measured. Thus, assignment of their relative importance would be purely speculative. This comment denotes our awareness of this issue and hopefully fosters future investigation.
We believe the near-total collapse of the unsupported first metacarpal after trapeziectomy gained support from resting against the scaphoid and was therefore able to demonstrate better pinch in vitro than would be seen in vivo because of the stabilized position and already noted unrestricted tendon excursion used to create pinch force in this model.
The observed difference between the suture support (TESS) and the tendon support (LRTI) methods was unexpected. Possibly this is the result of the surgeon's ability to pull more firmly against the anchored pulley (second metacarpal base) and thereby distally displace the first metacarpal as well as enhance its stability relative to the second metacarpal. This position (distally displaced) may offer a mechanical advantage. Comparatively, in the LRTI state the FCR tendon wrap is being secured back to the FCR insertion and cannot, by anatomic position, be positioned as distally as the anchor and therefore is disadvantaged in restoring anatomic height.
This biomechanical study might be used to argue for or against a current clinical practice. This was not the intent of our study. Meaningful clinical outcome differences are best determined by using large patient and surgeon numbers in a prospective study to identify clinically significant differences related to effectiveness and efficiency. This study cannot make any clinical claims regarding the methods tested. Our study does show that biomechanical differences related to maintenance of first metacarpal height are significant between tested surgical states and that state is 96% predictive of trapezial space maintained after trapezial excision. The suture suspension procedure tested (TESS) came closest to mirroring the intact trapezial/first metacarpal height in this in vitro model. Perhaps more importantly, this study describes a model that can be used to test and compare surgical methods intended to address first-CMC arthritis. Future modifications of this model should consider restricting excursion of applied loads and attempt to analyze all degrees of freedom affecting this joint/condition.
Conflict of Interest None
Note
This study was performed in the Biomechanics Laboratory at the University of Minnesota under the direction of Jack Lewis, PhD. Portions of this work were previously presented in poster format as the ASSH Annual Meeting (2000) and in podium presentation format at the AAOS Annual Meeting (2006).
References
- 1.Armstrong A L, Hunter J B, Davis T R. The prevalence of degenerative arthritis of the base of the thumb in post-menopausal women. J Hand Surg [Br] 1994;19(3):340–341. doi: 10.1016/0266-7681(94)90085-x. [DOI] [PubMed] [Google Scholar]
- 2.Fulton D B, Stern P J. Trapeziometacarpal arthrodesis in primary osteoarthritis: a minimum two-year follow-up study. J Hand Surg Am. 2001;26(1):109–114. doi: 10.1053/jhsu.2001.20964. [DOI] [PubMed] [Google Scholar]
- 3.Putnam M D, Chapman J. Interpositional titanium hemiarthroplasty for trapezial metacarpal arthritis. Atlas Hand Clin. 1997;2:203–216. [Google Scholar]
- 4.Jones N F, Maser B M. Treatment of arthritis of the trapeziometacarpal joint with trapeziectomy and hematoma arthroplasty. Hand Clin. 2001;17(2):237–243. [PubMed] [Google Scholar]
- 5.Kuhns C A, Emerson E T, Meals R A. Hematoma and distraction arthroplasty for thumb basal joint osteoarthritis: a prospective, single-surgeon study including outcomes measures. J Hand Surg Am. 2003;28(3):381–389. doi: 10.1053/jhsu.2003.50078. [DOI] [PubMed] [Google Scholar]
- 6.Atroshi I, Axelsson G. Extensor carpi radialis longus tendon arthroplasty in the treatment of primary trapeziometacarpal arthrosis. J Hand Surg Am. 1997;22(3):419–427. doi: 10.1016/S0363-5023(97)80008-1. [DOI] [PubMed] [Google Scholar]
- 7.Burton R I, Pellegrini V DJ Jr. Surgical management of basal joint arthritis of the thumb. Part II. Ligament reconstruction with tendon interposition arthroplasty. J Hand Surg Am. 1986;11(3):324–332. doi: 10.1016/s0363-5023(86)80137-x. [DOI] [PubMed] [Google Scholar]
- 8.Dell P C, Brushart T M, Smith R J. Treatment of trapeziometacarpal arthritis: results of resection arthroplasty. J Hand Surg Am. 1978;3(3):243–249. doi: 10.1016/s0363-5023(78)80088-4. [DOI] [PubMed] [Google Scholar]
- 9.Gibbons C E, Gosal H S, Choudri A H, Magnussen P A. Trapeziectomy for basal thumb joint osteoarthritis: 3- to 19-year follow-up. Int Orthop. 1999;23(4):216–218. doi: 10.1007/s002640050354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kriegs-Au G, Petje G, Fojtl E, Ganger R, Zachs I. Ligament reconstruction with or without tendon interposition to treat primary thumb carpometacarpal osteoarthritis. A prospective randomized study. J Bone Joint Surg Am. 2004;86-A(2):209–218. doi: 10.2106/00004623-200402000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Lins R E, Gelberman R H, McKeown L, Katz J N, Kadiyala R K. Basal joint arthritis: trapeziectomy with ligament reconstruction and tendon interposition arthroplasty. J Hand Surg Am. 1996;21(2):202–209. doi: 10.1016/S0363-5023(96)80101-8. [DOI] [PubMed] [Google Scholar]
- 12.Thompson J. Suspensionplasty technique. Atlas Hand Clin. 1997;2:101–125. [Google Scholar]
- 13.Wajon A, Ada L, Edmunds I. Surgery for thumb (trapeziometacarpal joint) osteoarthritis. Cochrane Database Syst Rev. 2005;(4):CD004631. doi: 10.1002/14651858.CD004631.pub2. [DOI] [PubMed] [Google Scholar]
- 14.Giurintano D J, Hollister A M, Buford W L, Thompson D E, Myers L M. A virtual five-link model of the thumb. Med Eng Phys. 1995;17(4):297–303. doi: 10.1016/1350-4533(95)90855-6. [DOI] [PubMed] [Google Scholar]
- 15.Cooney W P III, An K N, Daube J R, Askew L J. Electromyographic analysis of the thumb: a study of isometric forces in pinch and grasp. J Hand Surg Am. 1985;10(2):202–210. doi: 10.1016/s0363-5023(85)80106-4. [DOI] [PubMed] [Google Scholar]
- 16.Brand P W, Beach R B, Thompson D E. Relative tension and potential excursion of muscles in the forearm and hand. J Hand Surg Am. 1981;6(3):209–219. doi: 10.1016/s0363-5023(81)80072-x. [DOI] [PubMed] [Google Scholar]
- 17.Barber F A, Herbert M A, Click J N. The ultimate strength of suture anchors. Arthroscopy. 1995;11(1):21–28. doi: 10.1016/0749-8063(95)90084-5. [DOI] [PubMed] [Google Scholar]
- 18.Bamford D, Page R E. Ligament reconstruction in tendon interposition arthroplasty of the trapezium. J Hand Surg [Br] 1990;15(3):387–388. doi: 10.1016/0266-7681_90_90031-x. [DOI] [PubMed] [Google Scholar]
- 19.Meunier M J, Hentzen E, Ryan M, Shin A Y, Lieber R L. Predicted effects of metacarpal shortening on interosseous muscle function. J Hand Surg Am. 2004;29(4):689–693. doi: 10.1016/j.jhsa.2004.03.002. [DOI] [PubMed] [Google Scholar]


