Abstract
There is an upward trend in facial injuries following changes in population pattern, increasing industrialization and urbanization, hence maxillofacial trauma is becoming a burden and a leading medical problem in emergency rooms worldwide. This study was performed to evaluate the pattern of maxillofacial fractures, associated injuries, and treatment used at Jai Prakash Narayan Apex Trauma Center (JPNATC), All India Institute of Medical Sciences (AIIMS), New Delhi, India, between January 2007 and June 2010. The study provides basis for establishment of trauma as major etiology of maxillofacial injuries and planning for preventive strategies. A retrospective study of patients seen and treated at JPNATC, AIIMS, New Delhi, between January 2007 and June 2010 was performed. Data extracted from patient records included etiology, age, sex, types and sites of fractures, treatment modality, and concomitant injuries. There were 795 fractures of the maxillofacial skeleton and 86 concomitant injuries from 542 patients. Road traffic accident (RTA) (56.8%) was the most common etiologic factor, followed by falls (22.3%) and fights (18.5%). The age range was from 3 to 75 years (mean, 34.7 years) with a peak incidence in the third decade with a male-to-female ratio of 3.7:1. The most common location of maxillofacial fractures was the mandible 615 (77%) and middle third 180 (23%). With regard to mandibular fractures, the body (29.6%) was the most common site, followed by the angle (24.4%), ramus (19.5%), dentoalveolar (14.6%), symphysis (11.0%), condyle (0.8%) while in the middle third, the nasal bone (36.7%) was the most common, followed by zygomatic bone (27.8), Lefort II (14.4), Lefort I (7.8%), dentoalveolar (10.0%), and Lefort III (3.3%). Majority of the patients were treated by open reduction and internal fixation (70.6). Concomitant injuries were 84 (10.8%) with orthopedic injuries accounting for the majority (63.9%). Head injury was associated in 16.3% of cases. RTA was the major etiologic factor of maxillofacial injuries in our setting and the young adult males were the main victims. Henceforth, establishment of regionalized, efficient, and focused trauma centers in various parts of the country particularly for acute trauma should be emphasized. Also, the laws regarding the precautions such as seat belts, speed limits, and traffic rules must be observed strictly to reduce the incidence of RTA.
Keywords: maxillofacial injuries, injury characteristics, concomitant, treatment outcome
The maxillofacial region occupies the most prominent position in human body, thus commonly vulnerable to injuries.1 2 Because of the increasing industrialization and urbanization, maxillofacial trauma is becoming a burden and a leading medical problem in emergency rooms worldwide.3 4 5 According to Adekeye, maxillofacial injuries are increasing in frequency and severity because of the heavy reliance on road transportation and the increasing socioeconomic activities of the population.6 7 The variability in the global incidence of facial fractures is attributed to a variety of factors such as sex, age, level of industrialization, socioeconomic status of the patient, geographical location, and seasonal variation.3 4 5 It is estimated that more than 50% of patients with these injuries have multiple trauma requiring coordinated management between emergency physicians and surgical specialists in otolaryngology, trauma surgery, plastic surgery, ophthalmology, and oral and maxillofacial surgery.1 8 9
Surveys of facial injuries have shown that the etiology varies from one country to another and even within the same country depending on the prevailing socioeconomic cultural and environmental factors.1 10 Road traffic accident (RTA) is reported to be the leading cause of maxillofacial fractures in developing countries, whereas interpersonal violence is the leading cause in developed countries. The causes and pattern of maxillofacial injuries reflect trauma patterns within the community. Thus, they can provide a guide to the design of programs geared toward prevention and treatment.1 6
Maxillofacial injuries involve soft and hard tissue injuries of face extending from frontal bone superiorly to mandible inferiorly. They vary from soft tissues lacerations to complex fractures of maxillofacial skeleton.1 11 The management of injuries to the maxillofacial complex remains a challenge for oral and maxillofacial surgeons, demanding both skills and a high level of expertise.1 3 12 13
This study aims to evaluate the pattern of maxillofacial fractures, associated injuries, and treatment used at Jai Prakash Narayan Apex Trauma Center (JPNATC), All India Institute of Medical Sciences (AIIMS), New Delhi, India, between January 2007 and June 2010. The study provides basis for establishment of treatment guideline and planning for preventive strategies.
Patients and Methods
JPNATC (fully functional since 2007) is one of the leading and busiest trauma care service in India (with more than 50,000 visits annually in emergency department) and is also entrusted to carry out pioneering research in its field. It started seminal attempts at maintaining a hospital-based dedicated trauma registry in 2009 with gradual refinements each year (last major change was in 2011).
Inclusion and Exclusion Criteria: The study included all patients with etiology of RTA within 24 hours of the incidence. Patients of all ages and either sex were included in the study. Patients who underwent treatment in some other trauma center, patients who came for secondary problems, and patients who came after 24 hours were excluded from the study.
Study Design: Between January 2007 and June 2010, a total of 795 fractures of the maxillofacial skeleton and 86 concomitant injuries from 542 patients were encountered and analyzed. Trauma patients were first seen at the emergency department where resuscitation was performed according to advanced trauma life support principles. From the emergency department, these patients were admitted in their respective surgical wards or intensive care unit (ICU) after definitive treatment.
Data extracted from the patient records included etiology, age, sex, types, sites of fractures, treatment modality, and concomitant injuries. Anatomic location of mandibular fractures was classified according to Ivy and Curtis systems, whereas maxillary fractures were classified using Le Fort system. Concomitant injuries were categorized into orthopedic, craniocerebral, pulmonary, ocular, and abdominal injuries.
Results
During the period under study, a total of 542 patients were reviewed. The age ranged from 5 to 70 years with a peak incidence in the fourth decade (n = 197, 36.3%) (Table 1). The male predilection was 78.9%, with a male-to-female ratio of 3.7:1. Males were frequently more involved irrespective of the age.
Table 1. Distribution of age and sex.
| Age (y) | Male | Female | Total (%) |
|---|---|---|---|
| 0–10 | 9 | 4 | 13 (2.4) |
| 11–20 | 45 | 17 | 62 (11.4) |
| 21–30 | 123 | 24 | 147 (27.3) |
| 31–40 | 157 | 40 | 197 (36.3) |
| 41–50 | 64 | 22 | 86 (15.8) |
| 51–60 | 19 | 4 | 23 (4.2) |
| 61–70 | 11 | 3 | 14 (2.6) |
| Total | 428 | 114 | 542 (100) |
RTA (56.8%) was the most common causative factor, followed by falls (22.3%) and assault (18.5%), respectively (Fig. 1). Of the 542 patients, 274 (50.5%) patients had isolated mandibular fractures, 171 (31.5%) had isolated middle third fractures, and 97 (18.0%) had combined middle third and mandibular fractures. There were 615 (77.3%) mandibular fractures and 180 (22.6%) middle third fractures. With regard to mandibular fractures, the body (29.6%) was the most common site, followed by the angle (24.4%), ramus (19.5%), dentoalveolar (14.6%), symphysis (11.0%), condyle (0.8%), whereas in the middle third, the nasal bone (36.7%) was the most common, followed by zygomatic bone (27.8%), Lefort II (14.4%), Lefort I (7.8%), dentoalveolar (10.0%), and Lefort III (3.3%) (Tables 2 and 3). Associated injuries were recorded in 86 (15.8%) patients with orthopedic injuries accounting for majority (63.9%) (Fig. 2). Treatment modalities of mandibular fractures were open reduction and internal fixation (ORIF) (81.2%) and closed reduction with intermaxillary fixation (18.8%) (Fig. 3).
Figure 1.
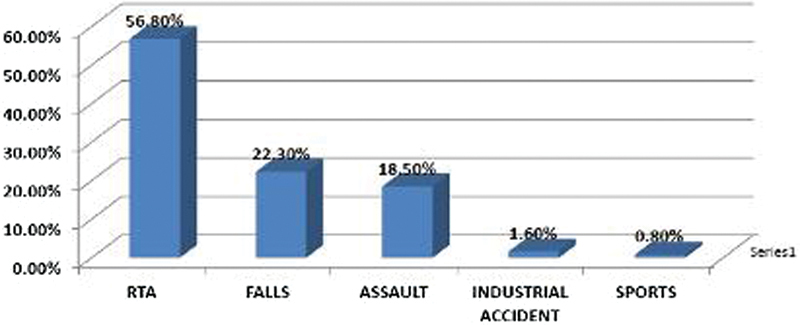
Etiology of maxillofacial injuries.
Table 2. Anatomical distribution of mandibular fractures.
| Location | No. of fractures (%) |
|---|---|
| Symphysis | 68 (11.05) |
| Body | 182 (29.59) |
| Angle | 150 (24.39) |
| Condyle | 5 (0.81) |
| Ramus | 120 (19.51) |
| Dentoalveolar | 90 (14.63) |
| Total | 615 (100) |
Table 3. Middle one-third fractures.
| Site | Number (%) |
|---|---|
| Nasal bone | 66 (36.66) |
| Zygomatic | 50(27.77) |
| Lefort I | 14(07.77) |
| Lefort II | 26 (14.44) |
| Lefort III | 06 (03.33) |
| Dentoalveolar | 18 (10.00) |
| Total | 180 (100) |
Figure 2.
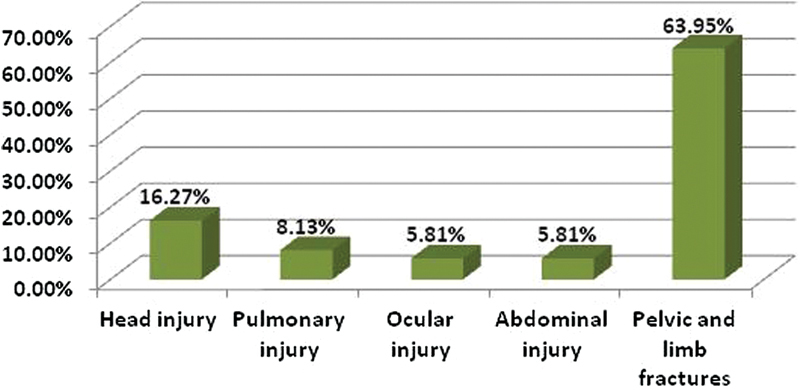
Associated injuries with maxillofacial fractures.
Figure 3.
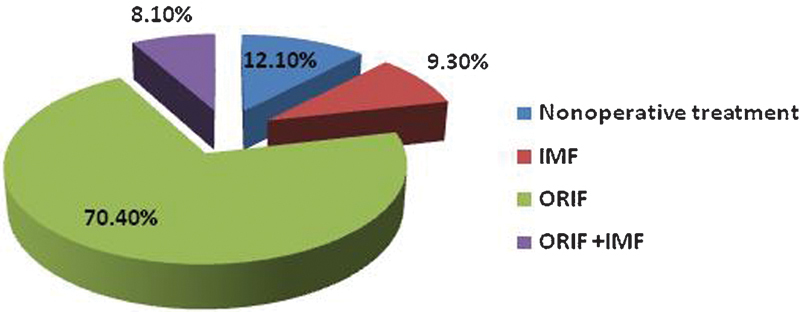
Management of maxillofacial fractures. IMF, intermaxillary fixation; ORIF, open reduction and internal fixation.
Discussion
The etiologic factors and patterns of maxillofacial injuries have been reported to vary from one geographical area to another depending upon the socioeconomic status, geographic condition, and cultural characteristics.1 14 15 16 In this study, an incidence of 542 patients with 795 maxillofacial fractures gave a fracture patient ratio of 1.5:1, which conformed to reported incidence in other countries. The report of 563 patients with 756 maxillofacial fractures by Bataineh is in close agreement with our study. Another epidemiological survey done in Nigeria by Ajike et al agrees with our study.3 17
The male predominance in our study agrees with what is reported in the literature. Males are at a greater risk due to greater participation in high risk activities which increases their exposure to high risk factors such as driving vehicles, sports involving physical contact, an active social life, and drug use, including alcohol.3 11 12 13 18
Ever since the report of RTA fatality on August 17, 1896, there is an upward trend in RTA as a cause of mortality and morbidity. RTA remains the leading cause of facial fractures particularly in the developing countries accounting for between 56 and 80.77%.3 6 19 20 21 22 In the developed countries, assaults, alcohol/drug abuse, and interpersonal violence account for more cases (range, 40–68.09%) than RTA.4 20 21 22 Furthermore, there is absence of safety driving mechanisms (seat belts, airbags and enforcement of traffic regulations, and wearing of crash helmets) in many developing countries. van Beek and Merkx emphasized the benefits of these measures. The 2002 world health report documented 1.18 million mortality and 20 to 50 million morbidity following RTA.22 The global burden of disease index for Africa predicts an upward movement of mortality due to RTA from the ninth position in 1990 to the third position in 2020.3 21
Our findings suggest highest frequency of facial fractures in the third to fourth decade of life, which is the most active phase of life. This is in agreement with studies reported elsewhere. The low incidence in first decade of life is due to the anatomico-morphologic peculiarities of the infantile bone, the small body size in proportion to the head, high bone-to-tooth ratio, low social and outdoor activities, and parental guidance and supervision.3 23 24
Developing world has recorded orthopedic injuries as the most frequent concomitant injury, but reports from the developed world have favored cranial injuries. In this study, 8.5% of maxillofacial fracture cases had concomitant orthopedic injuries as majority (67.1%).3 6
A total of 274 (50.5%) patients had isolated mandibular fractures, 171 (31.5%) had isolated middle third fractures, and 97 (18.0%) had combined middle third and mandibular fractures. With regard to mandibular fractures, the body (29.6%) was the most common site. In the middle third, nasal bone fracture (36.7%) was the most common. Mandible fracture was the one which occurred most often in all trauma categories. According to the literature, assaults are usually responsible for mandible body and angle fractures, automobile accidents are responsible for condyle fracture, mandibular body fractures or problems on the condyle and symphysis. Accidents with motorcycles, without wearing helmets, are responsible for fractures on the body, symphysis, parasymphysis, and condyle.25 The results from this study are in close agreement with the literature, considering the most prevalent fractures on parasymphysis, condyle, and body. Some studies report that nose is the main site of fractures on the face, followed by the zygomatic bone because it has a central position on the face and it is an easy structure to be fractured because of thin thickness of the nasal bones. However, in this study, mandibular fractures were the most prevalent maxillofacial fractures.25 26
There are many treatment regimens in maxillofacial fractures, but the treatment chosen may differ depending on many factors such as cost of treatment, affordability by the patient, feasibility in the hospital, doctor's decision and skill, and patient's willingness to avail the treatment advised—all of which may vary from one country to another. In our study, hospitalization was necessary in 84.5% of the patients while 3.7% required care in the ICU.
ORIF with miniplates was done in 87.9% of the cases, when compared with the closed reduction and intermaxillary fixation (12.1%). Undisplaced fractures were treated conservatively and the displaced ones by open reduction and rigid internal fixation with miniplates. Rigid fixation of a facial fracture helps in the support and strength of masticatory function. Nonoperative treatment for undisplaced fractures provides acceptable cosmetic and functional results.27 28
Conclusion
RTA is the major etiologic factor of maxillofacial injuries in our setting with young adult males being the main victims. Soft tissue injuries and mandibular fractures were the most common type of maxillofacial injury. The majority of fracture management was done by ORIF. Prevention is always better than cure hence precautions such as seat belts, speed limits, and traffic rules must be followed and observed strictly. In India, RTA is most common cause of maxillofacial trauma today, thus, an awareness campaign to educate the public especially the drivers about the importance of restraints and protective measures in motor vehicles can be an innovation. Maxillofacial fractures if managed by ORIF as early as possible reduce the morbidity resulting from these injuries. This study is suggestive of ORIF as the line of treatment for displaced fractures because we did 84.5% cases with ORIF. This study is not complete to lay down the treatment plan for all cases but evaluates the etiology, pattern, and rise in trend of maxillofacial injuries in India. Further studies to provide long-term success of treatment results in cases with ORIF verses closed reduction are being done at our center.
References
- 1.Chalya P L, McHembe M, Mabula J B, Kanumba E S, Gilyoma J M. Etiological spectrum, injury characteristics and treatment outcome of maxillofacial injuries in a Tanzanian teaching hospital. J Trauma Manag Outcomes. 2011;5(1):7. doi: 10.1186/1752-2897-5-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adeyemo W L, Ladeinde A L, Ogunlewe M O, James O. Trends and characteristics of oral and maxillofacial injuries in Nigeria: a review of the literature. Head Face Med. 2005;1:7. doi: 10.1186/1746-160X-1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ajike S O, Adebayo E T, Amanyiewe E U, Ononiwn C N. An epidemiologic survey of maxillofacial fractures and concomitant injuries in Kaduna, Nigeria. J Surg Res. 2005;7(3–4):251–255. [Google Scholar]
- 4.Sojot A J, Meisami T, Sandor G K, Clokie C ML. The epidemiology of mandibular fractures treated at the Toronto general hospital: A review of 246 cases. J Can Dent Assoc. 2001;67(11):640–644. [PubMed] [Google Scholar]
- 5.Majumder B, Karmakar R, Bose T, Dasgupta S, Basu R. Some host factors and seasonal variations in the fatal road traffic accidents occurring in eastern suburban Calcutta. Indian J Public Health. 1996;40(2):46–49. [PubMed] [Google Scholar]
- 6.Adebayo E T, Ajike O S, Adekeye E O. Analysis of the pattern of maxillofacial fractures in Kaduna, Nigeria. Br J Oral Maxillofac Surg. 2003;41(6):396–400. doi: 10.1016/s0266-4356(03)00165-7. [DOI] [PubMed] [Google Scholar]
- 7.Adekeye E O. The pattern of fractures of the facial skeleton in Kaduna, Nigeria. A survey of 1,447 cases. Oral Surg Oral Med Oral Pathol. 1980;49(6):491–495. doi: 10.1016/0030-4220(80)90068-7. [DOI] [PubMed] [Google Scholar]
- 8.Rosen P Face B R, eds. Emergency medicine concepts and clinical practice. 5th ed St Louis, MO: Mosby-Year Book; 2002315–329. [Google Scholar]
- 9.Tintinalli J E Kelen J D Stapczynski J S, eds. Maxillofacial Trauma New York, NY: McGraw-Hill; 20041583–1589. [Google Scholar]
- 10.Olasoji H O, Tahir A, Arotiba G T. Changing picture of facial fractures in northern Nigeria. Br J Oral Maxillofac Surg. 2002;40(2):140–143. doi: 10.1054/bjom.2001.0716. [DOI] [PubMed] [Google Scholar]
- 11.Umar K B, Shuja R A, Ahmad K, Mohammad T K, Abdus S. Occurrence and characteristics of maxillofacial injuries-A study. Pak Oral Dent J. 2010;30:57–71. [Google Scholar]
- 12.Al Ahmed H E, Jaber M A, Abu Fanas S H, Karas M. The pattern of maxillofacial fractures in Sharjah, United Arab Emirates: a review of 230 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98(2):166–170. doi: 10.1016/j.tripleo.2004.01.020. [DOI] [PubMed] [Google Scholar]
- 13.Sirimaharaj W, Pyungtanasup K. The epidemiology of mandibular fractures treated at Chiang Mai University Hospital: a review of 198 cases. J Med Assoc Thai. 2008;91(6):868–874. [PubMed] [Google Scholar]
- 14.Leles J L, dos Santos E J, Jorge F D, da Silva E T, Leles C R. Risk factors for maxillofacial injuries in a Brazilian emergency hospital sample. J Appl Oral Sci. 2010;18(1):23–29. doi: 10.1590/S1678-77572010000100006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shah A, Shah A A, Salam A. Maxillofacial fractures: analysis of demographic distribution in 230 patients. Pak Oral Dent J. 2006;26:235–237. [Google Scholar]
- 16.Kamulegeya A, Lakor F, Kabenge K. Oral maxillofacial fractures seen at a Ugandan tertiary hospital: a six-month prospective study. Clinics (Sao Paulo) 2009;64(9):843–848. doi: 10.1590/S1807-59322009000900004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bataineh A B. Etiology and incidence of maxillofacial fractures in the north of Jordan. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998;86(1):31–35. doi: 10.1016/s1079-2104(98)90146-9. [DOI] [PubMed] [Google Scholar]
- 18.Hussain S S, Ahmad M, Khan M I. et al. Maxillofacial trauma: current practice in management at Pakistan Institute of Medical Sciences. J Ayub Med Coll Abbottabad. 2003;15(2):8–11. [PubMed] [Google Scholar]
- 19.Abiose B O. Maxillofacial skeleton injuries in the western states of Nigeria. Br J Oral Maxillofac Surg. 1986;24(1):31–39. doi: 10.1016/0266-4356(86)90037-9. [DOI] [PubMed] [Google Scholar]
- 20.Tanaka N, Tomitsuka K, Shionoya K. et al. Aetiology of maxillofacial fracture. Br J Oral Maxillofac Surg. 1994;32(1):19–23. doi: 10.1016/0266-4356(94)90166-x. [DOI] [PubMed] [Google Scholar]
- 21.van Beek G J, Merkx C A. Changes in the pattern of fractures of the maxillofacial skeleton. Int J Oral Maxillofac Surg. 1999;28(6):424–428. doi: 10.1034/j.1399-0020.1999.280605.x. [DOI] [PubMed] [Google Scholar]
- 22.Prokop D, Boeckler H H. Morbidity analysis of 1484 facial bone fractures between 1968 and 1987 [in German] Dtsch Z Mund Kiefer Gesichtschir. 1990;14(4):287–292. [PubMed] [Google Scholar]
- 23.Fasola A O, Lawoyin J O, Obiechina A E, Arotiba J T. Inner city maxillofacial fractures due to road traffic accidents. Dent Traumatol. 2003;19(1):2–5. doi: 10.1034/j.1600-9657.2003.00073.x. [DOI] [PubMed] [Google Scholar]
- 24.Nørholt S E, Krishnan V, Sindet-Pedersen S, Jensen I. Pediatric condylar fractures: a long-term follow-up study of 55 patients. J Oral Maxillofac Surg. 1993;51(12):1302–1310. doi: 10.1016/s0278-2391(10)80132-6. [DOI] [PubMed] [Google Scholar]
- 25.Chrcanovic B R, Freire-Maia B, Souza L N, Araújo V O, Abreu M HNG. Facial fractures: a 1-year retrospective study in a hospital in Belo Horizonte. Braz Oral Res. 2004;18(4):322–328. doi: 10.1590/s1806-83242004000400009. [DOI] [PubMed] [Google Scholar]
- 26.Kelley P, Crawford M, Higuera S, Hollier L H. Two hundred ninety-four consecutive facial fractures in an urban trauma centre: lessons learned. Plast Reconstr Surg. 2005;116:42–49. doi: 10.1097/01.prs.0000177687.83247.27. [DOI] [PubMed] [Google Scholar]
- 27.Rajendra P B, Mathew T P, Agrawal A, Sabharawal G. Characteristics of associated craniofacial trauma in patients with head injuries: An experience with 100 cases. J Emerg Trauma Shock. 2009;2(2):89–94. doi: 10.4103/0974-2700.50742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ansari M H. Maxillofacial fractures in Hamedan province, Iran: a retrospective study (1987-2001) J Craniomaxillofac Surg. 2004;32(1):28–34. doi: 10.1016/j.jcms.2003.07.010. [DOI] [PubMed] [Google Scholar]