Abstract
Background
Because of the complex anatomy of the head and neck region, conventional projection radiography alone is unreliable and carries a high risk of misdiagnosis. The poor risk-benefit ratio of conventional radiography has led to their replacement by tomographic imaging for nearly all studies in this region.
Method
This review is based on pertinent articles retrieved by a selective search in the PubMed database (January 1980 to May 2013) as well as on the relevant guidelines from Germany and abroad.
Results
The indication for diagnostic imaging in the anatomically complex head and neck region should be established for a specific type of imaging study on the basis of a thorough clinical examination. Conventional films, though easy to obtain, often cannot answer the diagnostic question and may yield confusing information leading to misdiagnosis. Computed tomography (CT) has the best risk-benefit profile and a high diagnostic value, but low-dose protocols have not yet been put into use in all centers. Magnetic resonance imaging (MRI) is best for bone and soft-tissue diagnosis, but consumes more resources. Digital volume tomography (DVT) is another type of three-dimensional, sectional imaging with high local resolution; the associated radiation exposure and image quality are generally both low, but may vary depending on the apparatus used. DVT cannot be used to evaluate the soft tissues. Ultrasonography can be used to evaluate superficial structures in the head and neck region; nuclear imaging can be used to evaluate thyroid disease and cancer.
Conclusion
Inflammatory, traumatic, and neoplastic diseases of the head and neck are best evaluated with cross-sectional imaging (CT, MRI) in accordance with current guidelines. Conventional x-rays should, in general, only be used for dental evaluation, with rare exceptions.
When only conventional x-ray methods were available, radiologic studies had little role to play in the diagnostic assessment of many types of lesion in the head and neck area, as they often led to false conclusions (1). It was only the introduction of modern tomographic imaging that enabled precise, non-distorted, and non-overlapping visualization of head and neck anatomy, with high spatial and contrast resolution (2).
Tomographic images reveal not only the spatial extent of disease, but also anatomical danger areas for surgery, on the basis of which the treatment can be appropriately chosen and precisely planned (3). For this reason, computed tomography (CT), above all, has made a major contribution to the development of endoscopic and other minimally invasive surgical techniques and has become an indispensable component of preoperative evaluation in all cases (4– 7).
Ultrasonographic imaging has also improved over the years and is now highly valuable in the diagnostic evaluation of the salivary glands and the soft tissues of the neck.
In recent years, digital volume tomography (DVT) has been developed as a further x-ray-based technique for sectional imaging of the teeth and bony structures of the skull. DVT is now recognized as a valuable diagnostic tool for such high-contrast structures in dental, oral, and maxillofacial medicine and surgery; it is under evaluation for use in further specialty areas (8, 9).
The low diagnostic value of classic projection x-ray films and the misleading information that they can provide have been well documented in scientific publications over the past three decades, and the guidelines of all relevant specialty societies with the exception of the German Society of Dentistry and Oral Medicine (DGZMK) no longer recommend them, or do so only in exceptional cases. Some guidelines explicitly state that they are no longer to be performed. Nonetheless, in clinical practice, standard x-ray views continue to be requested and obtained in large numbers. This may be, in part, because of the low associated radiation exposure, the relatively low expense, and the (deceptively) clear anatomical pictures that standard x-rays provide. The risk of incorrect evaluation—even by experienced readers—because of projection effects is often underestimated, and too little attention is paid to the the risk–benefit profiles of the currently available diagnostic techniques (1, 9– 28).
The notion that CT automatically confers a higher radiation exposure than projection films is an overgeneralization based on past situations and conditions. The radiation exposure from a CT study largely depends on the diagnostic question to be answered. A soft-tissue study with intravenous contrast medium, under current radiation safeguards, yields a radiation dose that is only about 30% of what it was 15 years ago, while the radiation dose from a pure high-contrast diagnostic study, e.g., of bone, paranasal sinuses, or teeth, is now as low as that of a conventional x-ray (29– 32).
To our knowledge, the question whether a conventional x-ray should be performed to evaluate a problem in the head and neck region arises very frequently. This review is intended to meet the evident need for a better understanding of this matter among treating physicians (Box, eTable).
Box. The main advantages and disdavantages of imaging modalities in the head and neck region.
-
Ultrasonograpny
+ widely available
+ no exposure to ionizing radiation
- limited to superficial regions
- diagnostic value is examiner-dependent
-
Nuclear imaging
+ whole-body evaluation
+ functional, not merely anatomical, evaluation
- limited structural information
- cancer specific diagnostic value of positron emission tomography (PET) not generally accepted
-
Conventional x-rays
+ low cost
+ low radiation exposure
- poor risk–benefit profile, owing to diagnostic uncertainty from projection effects
- therefore, restricted to certain specific indications (e.g., dental diagnosis)
-
Computed tomography (CT)
+ 3D sectional imaging technique with high diagnostic value
+ widely available
+ best risk–benefit profile for standard care
- low-dose protocols have not yet come into use in all centers
-
Digital volume tomography (DVT)
+ 3D sectional imaging technique
+ high spatial resolution
+ usually low radiation exposure (but depends on apparatus and examiner)
- cannot be used to examine soft tissues, incl. tumors
-
Magnetic resonance imaging (MRI)
+ 3D sectional imaging technique with the highest diagnostic value
+ best modality for imaging the soft tissues
+ no exposure to ionizing radiation
- requires expensive special equipment
eTable.
Indications for imaging studies of the head and neck
| Indication | Primary | Alternative/Complementary |
|---|---|---|
| Temporal bone | ||
| Suspected complications of acute otitis media and otitis externa | ||
|
CT | |
|
MRI | |
| Chronic otitis media | ||
|
CT | (DVT?); MRI |
| Infectious processes: labyrinthitis | ||
|
MRI | CT |
| Sequelae of trauma | CT | MRI |
| Neoplasia | ||
|
CT | MRI |
|
MRI | CT |
|
CT + MRI | DSA + embolization |
| Other | ||
|
CT (DVT?) | |
|
CT (DVT?) | MRI |
|
MRI | CT (DVT?) |
|
MRI + CT (DVT?) | |
| Postoperative | ||
|
CT (DVT?) | MRI |
|
MRI | (CT) |
|
no imaging | (CT, MRI) |
|
CT (DVT?) | MRI |
|
CT (DVT?) | |
| Isolated, non-traumatic peripheral facial palsy | ||
|
MRI | |
|
US | MRI |
|
MRI | |
|
CT | MRI |
| Tinnitus | ||
|
no imaging | |
|
CT | MRI |
|
Doppler-US | |
|
MRI | |
| Masticatory apparatus | ||
|
dental films, OPG | |
|
dental films, OPG | CT, DVT |
|
OPG | CT, DVT |
|
CT, (DVT?) | MRI |
|
X-ray | CT |
|
OPG | CT, DVT |
|
OPG | CT, DVT |
|
MRI | |
| Pharynx, oral cavity, larynx | ||
|
MRI | CT, US, DSA + embolization |
|
CT or MRI | US, DSA + embolization |
|
US | CT, MRI |
|
cf. neoplasia | |
| Dysphagia | ||
|
cf. neoplasia, inflammation | |
|
US, medical work-up | |
|
fluoroscopy (contrast swallow, with cinematography if ‧indicated) | C-spine films if a ventral ‧spondylophyte is suspected |
|
MRI | (CT) |
| Salivary glands | ||
|
US | endoscopy, MRI, CT |
|
US | MRI if staging unclear |
|
US | MRI |
| Craniofacial region (e.g., paranasal sinuses) | ||
|
dental films, OPG | CT, DVT |
|
no imaging | CT, MRI for complications |
|
CT (DVT?) | MRI |
|
MRI | |
|
special x-rays (zygoma, nasal bone), otherwise CT | MRI for intracranial complications |
|
CT | MRI for (possibly) malignant tumors; DSA + embolization |
|
US | MRI, (DSA + embolization) |
| Disorders of the nose and of the sense of smell | ||
|
CT | MRI |
|
CT | MRI, DSA + embolization |
|
MRI | CT, DSA + embolization |
|
CT | MRI |
| Epistaxis | ||
|
DSA with embolization | |
|
medical work-up | |
|
CT | MRI, DSA+embolization |
| Neck | ||
|
CT | MRI, DSA + embolization |
|
US | MRI- or CT-angiography |
|
MRI | CT; US for further investigation of lymph nodes |
| Orbits | ||
|
US | MRI |
|
CT or MRI | |
|
MRI | |
|
CT | MRI |
|
US; retrobulbar, MRI | MRI, CT |
|
US | CT for trauma, otherwise MRI |
CT, computed tomography; MRI, magnetic resonance imaging; DVT, digital volume tomography; DSA, digital subtraction angiography; OPG, orthopantomography; TMJ, temporomandibular joint; US, ultrasonography
Methods
This review is based on the results of a selective literature search in the PubMed database that yielded several thousand hits. We judged the clinical relevance of each publication from the journal it was published in, the title, and the abstract. No pertinent randomized trials or Cochrane Reviews have been published to date; thus, most of the relevant publications are observational studies. This review is, further, based on the current guidelines of the specialty societies that deal with each of the clinical questions under discussion and on the guidelines of the German Radiation Protection Commission (Strahlenschutz-Kommission, SSK) and other German and foreign institutions.
Projection radiography
Projection films (conventional x-rays) are now considered obsolete for studies in the head and neck area. They have been almost entirely replaced by cross-sectional imaging, except for a few special indications including diagnostic assessment of the teeth and jaws (9, 10, 33, 34).
The indications for imaging studies in head and neck disease, and the types of study that are to be used, are well defined in the guidelines of the German and foreign specialty societies and in the recommendations of the SSK. There is little divergence among the different sets of recommendations (8– 10, 33– 40).
Paranasal sinuses
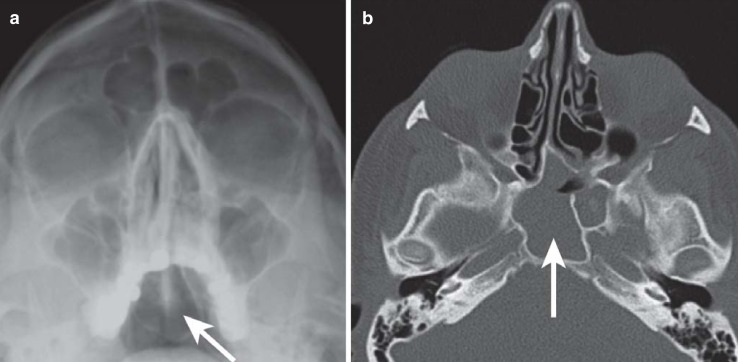
The standard x-ray study of the paranasal sinuses consists of an occipitofrontal and an occipitomental view. It can be obtained simply and rapidly but generally does not enable a clear distinction of pathological soft-tissue shadows from projection effects, because the sinuses vary widely from one individual to another in their shape and degree of pneumatization. Thus, such images are of limited diagnostic value. Their risk-benefit ratio is unacceptable, as they are fraught with the risk of misdiagnosis in both positive and negative directions—e.g., with regard to the diagnosis of sinusitis (Figure 1) (9– 11, 13– 23, e1). In the current guidelines, conventional x-rays are classified as “not recommended” (9, 10); if an imaging study is needed, modern tomographic techniques are recommended instead (9, 10, 13, 19, 22, e2). In particular, conventional x-rays of the paranasal sinuses are not indicated for screening purposes—e.g., to evaluate headache, cystic fibrosis in children (33, e3), asthma, or allergies (e4)—or for the detection of an infectious focus in patients with unclear inflammatory symptoms or the exclusion of such disease in persons at elevated risk (e5, e6).
Figure 1.
Imaging of the paranasal sinuses. a) A conventional occipitomental x-ray. b) An axial CT obtained shortly after the image in a), clearly revealing an opacification in the sphenoid sinus (arrow). The plain film is falsely negative despite its good technical quality
Rhinosinusitis, the most common disease of the paranasal sinuses, is a major economic, as well as clinical, burden for the overall population. According to the current DGHNO (German Society of Oto-Rhino-Laryngology, Head and Neck Surgery) guidelines (9, 10), it should be diagnosed on clinical grounds; confirmation with an imaging study is generally unnecessary. If a complication such as muco- or pyocele or extension beyond the paranasal sinuses is suspected, then CT is the imaging modality of choice for local (e.g., orbital) complications, and magnetic resonance imaging (MRI) for intracranial complications (9, 10).
Low-dose CT is the imaging method of first choice for chronic rhinosinusitis (9, 10). It is important to treat the patient with antibiotics before the CT study is performed to eliminate any acute inflammatory component that may be present. The preoperative CT documents the site and extent of chronic inflammatory changes that have not responded to conservative treatment; it also documents any anatomical variants that may have contributed to the causation of sinusitis or that might be danger areas for the current state-of-the-art, minimally invasive, endoscopic surgical approach (4, 5, 41, e7).
Initial publications on the use of DVT, instead of CT, for this indication suggest that these two techniques are of equivalent clinical value, as long as DVT is performed on suitable, appropriately configured equipment (e8, e9). MRI can also be used as an alternative technique without ionizing radiation. If a neoplastic or granulomatous disease is suspected, MRI with contrast is the method of first choice.
Skull
Plain films of the skull were once very commonly obtained in the evaluation of trauma cases. As early as the 1980s, however, multiple studies uniformly revealed that a skull survey view and an occipital view are of no use for this indication; indeed, they carry the risk of clinically significant misdiagnosis (1, 24– 28). The main reason is that skull fractures recognizable on projection views poorly correlate with intracranial injuries (26), while the clinically relevant entity is not the skull fracture itself, but rather the intracranial hemorrhage that may be associated with it. Jend et al. found that only 40% of patients with a skull fracture had an intracranial injury as well; on the other hand, 44% of patients with an intracranial injury had no skull fracture (26). Thus if an imaging study is needed, CT is clearly the method of choice (27, e10, e11).
Conventional skull films are, exceptionally, still indicated to exclude isolated fractures of the zygomatic bone, maxilla, mandible, or nasal bone, to diagnose congenital anomalies and premature synostoses, to demonstrate pneumocephalus after intracranial procedures, to detect metallic foreign bodies before MRI, and to check the setting of a programmable ventriculoperitoneal shunt (34).
Orbit
Conventional x-rays of the orbit were, likewise, used in the past almost exclusively for the evaluation of trauma cases. Their sensitivity for fractures is only 15–50%; thus, clinical decisions based on conventional orbital views can easily be wrong (1, 18, e12). Conventional orbital x-rays have now been replaced by tomographic imaging for nearly all indications. As an exception, they can still be used (as an alternative to plain films of the skull) to rule out the presence of metallic foreign bodies before MRI (1, 34). Conventional orbital x-rays are not mentioned in the current AWMF guidelines; they are obsolete for orbital diagnosis (9).
The imaging method of choice for trauma involving the orbit, midface, and skull base is thin-section CT (9). Multiplanar and three-dimensional reconstructions of the CT dataset yield the details that are needed for the comrehensive assessment of complex fractures affecting the entire midface or any part of it.
The proper imaging study to evaluate visual disturbances is an MRI or CT of the whole neurocranium, orbits included (9). For the evaluation of orbital tumors or endocrine orbitopathy, MRI is the imaging study of first choice, after ultrasonographic examination by an ophthalmologist (9). CT can be particularly useful for the demonstration of calcifications or bony changes (9).
Temporal bone
The main conventional x-ray views of the temporal bone are those of Stenvers and Schüller. The former is still used today to document the position of the electrode carrier for cochlear implantation; it is obsolete for all other indications. The latter yields a rough estimate of the degree of pneumatization of the mastoid bone but does not permit any judgment whether diminished pneumatization is due to a congenital anomaly, tympanic sclerosis, or chronic inflammation (bland or aggressive). Schüller views are still occasionally obtained in patients with suspected mastoiditis or otitis media; this has no medical justification (e13, e14).
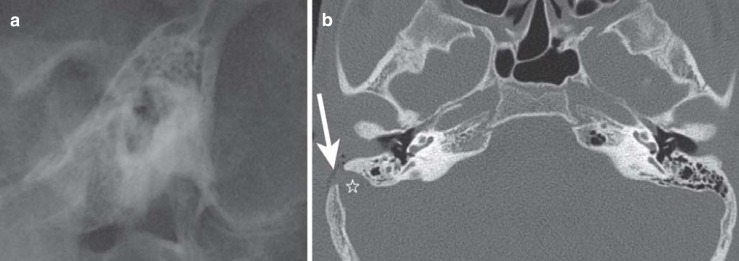
Nor should conventional temporal bone x-rays be taken preoperatively to demonstrate anatomical relationships, as an aid to surgery: projection effects make them unreliable for the identification and quantitative measurement of surgically relevant anatomical variants (Figure 2). Temporal bone x-rays are also wholly unsuitable for the assessment of trauma, malformations, and tumors of the temporal region. They have been replaced by sectional imaging for these purposes—CT, DVT, or MRI, depending on the indication (9, 10, 34, e13, e15, e16).
Figure 2.
Imaging of the petrous bone. a) Schüller view. b) Axial CT. The preoperative x-ray, taken because of a clinical suspicion of mastoiditis, revealed nothing more than a low degree of pneumatization of the temporal bone. Intraoperatively, when the surgeon began to drill the mastoid bone, a pulsating, blue structure was seen, and the operation was terminated. A CT obtained thereupon to clarify the situation revealed, as a normal variant, a strongly lateralized sigmoid sinus (star) with an iatrogenic (post-surgical) bony dehiscence (arrow). This surgically relevant anatomical variant was not recognizable on the plain film, even retrospectively
CT is preferred for the assessment of trauma, aggressive inflammatory diseases and other extracranial processes, and conductive or mixed hearing loss, as well as for the planning of cochlear implantation and other surgical procedures in the temporal region. Athough there have been a few reports of the use of DVT, rather than CT, in the planning of cochlear implants (e8, e17), a definitive judgment of the use of DVT for this indication is not yet possible.
MRI is the method of choice to assess anomalies of in the inner ear, sensorineural hearing loss/deafness, dizziness, and intracranial processes.
The dental and maxillary region
The primary imaging modality for assessment of the teeth and jaws is conventional radiography: specifically, intraoral dental views or an (extraoral) panoramic tomographic view (orthopantomogram, OPG). Intra-oral dental views enable the assessment of endodontal and periodontal disease with high local resolution and minimal radiation exposure. OPG, on the other hand, provides a comprehensive survey of all of the teeth and the underlying bone, with a low radiation exposure. Dental views and OPG are currently used, not only for the evaluation of inflammatory diseases, but also for orthopedic evaluation of the jaws, for trauma assessment, for the evaluation of unclear symptoms, and for the planning of dental implantation procedures. Conventional lateral views are used (optionally) in orthognathic surgery.
Tomographic imaging is indicated for the evaluation of large cysts and other benign or malignant lesions of the jaws (8, 9, 38) and for the evaluation of trauma with potentially extensive midface involvement (8, 9, 38). It is also increasingly being used for the planning of implantation procedures (8, 9, 38). Compared to conventional x-rays, it enables a more accurate assessment of the bone substance, exact measurement of the height and width of the jaws, three-dimensional localization of the mandibular nerve canal, and an assessment of the topography of the maxillary sinuses and of inflammatory processes than may affect them.
DVT is superior to conventional x-rays (dental views and OPG) for the assessment of dental trauma (e18).
The preferred methods of tomographic imaging are CT and DVT. Both methods are subject to the same restrictions with regard to radiation safety (8, 38).
CT and DVT provide better spatial and contrast resolution than conventional x-rays, and are therefore superior in the evaluation of osteomyelitis, tumors, and osteonecrosis of the jaw (8, 38). Nonetheless, of all imaging methods, MRI has the highest diagnostic value for these diseases (9).
Other imaging methods
Ultrasonography
Diagnostic ultrasonography of the head and neck is mainly used to assess organs and lesions that lie near the surface, including the salivary glands, the thyroid gland, the major vessels, enlarged superficial lymph nodes, and other superficial pathologic lesions (9, 10, 34, e19).
A fluid level or empyema in the maxillary sinus (present in some, but not all, cases of acute sinusitis) may be difficult to visualize with B-mode ultrasonography (10); the ethmoid and sphenoid sinuses are inaccessible to ultrasonography, for anatomical reasons. Thus, the overall utility of ultrasound in the evaluation of rhinosinusitis is very limited and examiner-dependent (10). In chronic sinusitis, ultrasonography is not indicated (9, 10, 34).
Nuclear imaging
Nuclear imaging plays an important role in the evaluation of thyroid disease. Bone scanning can be used to evaluate potential craniofacial or other skeletal involvement by chronic inflammatory or neoplastic processes. PET or PET-CT/PET-MRI can be of additional use in the staging and monitoring of malignant head and neck tumors (34). Nonetheless, in the judgment of the German Institute for Quality and Efficiency in Health Care (Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen, IQWiG), the available scientific evidence does not adequately document improved diagnosis through the use of PET (e20). As a result, statutory health insurance in Germany generally does not cover the cost of such studies.
Computed tomography
CT is the most commonly used imaging modality for all indications in the head and neck region (9, 10). The spiral CT mode currently involves the acquisition of only one thin-section axial volume dataset. From this dataset, tomographic images in all of the required planes can be computed without any further radiation exposure or loss of image quality (e7, e21– e24).
Intravenously administered contrast media improve the delineation of soft-tissue pathologies and are indispensable in the diagnosis of malignant tumors and inflammatory complications.
When CT is used to evaluate high-contrast structures such as bone, the paranasal sinuses, the temporal region, or the teeth, as opposed to the soft tissues, more image noise can be accepted without any clinically relevant decline in image quality. Therefore, a low-dose technique is used for these indications (e25), with radiation exposures that may be in the same low range as in conventional x-rays of the same region, or are at any rate no more than 10 times higher (29– 32, e23, e26).
Digital volume tomography
Digital volume tomography (DVT; synonym, cone beam CT, CBCT) is a sectional imaging technique similar to CT that was used at first only for dental diagnosis because of a restriction to small volumes. Technical advances have made DVT applicable in larger volumes as well; it can now be used as an alternative to CT for evaluation of the craniofacial and temporal high-contrast structures (e8, e9, e17, e27, e28).
The advantages of DVT are high spatial resolution, low radiation exposure in the same range as low-dose CT, and reduced metal artefact. It is unsuitable for soft-tissue diagnosis, because the image noise is too high. Apart from clinical use in the diagnosis of high contrast structures such as the teeth and the jaws, a definite judgement, particularly as an alternative method to CT, is not possible as yet. Therefore, the current guidelines designate DVT as a possible alternative to CT in individual cases but give no specific recommendations regarding its use (8, 10, 38, 40).
Magnetic resonance imaging
MRI is currently the imaging modality that yields the most detailed view of the soft tissues. Its main advantage, in comparison to CT, is the absence of ionizing radiation; its main disadvantage is the much longer time during which the patient must keep still during the study. Patients who cannot cooperate may need sedation or even general anesthesia.
In the head and neck, MRI is mainly used for pre- and postoperative tumor imaging and to evaluate suspected intracranial complications of sinusitis. Other rare indications include congenital anomalies of the temporal bone as well as the preoperative assessment for chochlear implants (9, 10, 40, e29). MRI can be used instead of CT as the primary imaging modality whenever ionizing radiation is to be avoided, e.g., in children who need imaging of the paranasal sinuses before surgery (e30– e34) or in the evaluation of cystic fibrosis (e35), or for pediatric applications in general. MRI is contraindicated in patients with cardiac pacemakers (e36) or (on a case-by-case basis) active implants of other types, or ferromagnetic foreign bodies. Claustrophobia is a relative contraindication; combatting it with sedation or anesthesia can be considered on an individual basis.
Conclusion
Diagnostic imaging in the anatomically complex head and neck region is performed for specific indications after thorough clinical examination. Conventional x-rays are easy to obtain but often cannot answer the clinical question and may yield confusing information leading to misdiagnosis. Therefore, inflammatory, traumatic, and neoplastic diseases of the head and neck are best evaluated with tomographic techniques, optimally chosen to answer the specific clinical question, in accordance with current guidelines. Conventional x-rays should, in general, only be used for dental evaluation, with rare exceptions that are discussed in detail in this article.
Key Messages.
Head and neck imaging today essentially consists of two cross-sectional techniques: computed tomography (CT) and magnetic resonance imaging (MRI).
Conventional projection radiography remains the imaging method of choice for dental diagnosis but is generally obsolete for other applications in the head and neck, with a few exceptions.
CT for soft-tissue diagnosis is performed with IV contrast medium and at a normal radiation dose. Focused diagnostic CT of high-contrast structures, such as bone, is performed with a low-dose technique.
Digital volume tomography (DVT) is a potential alternative to low-dose CT for small regions of interest. Its clincal value has not yet been conclusively demonstrated, except for studies of the teeth and jaws.
Other imaging techniques (ultrasonography, nuclear imaging including PET) are used for special indications.
Acknowledgments
Translated from the original German by Ethan Taub, M.D.
Footnotes
Conflict of interest statement
Prof. Haßfeld has received research support (third-party funding) from Sirona.
Prof. Dammann, Prof. Bootz, Prof. Cohnen, Prof. Tatagiba, and Prof. Kösling declare that no conflict of interest exists.
References
- 1.Sanders R, MacEwen CJ, McCulloch AS. The value of skull radiography in ophthalmology. Acta Radiol. 1994;35:429–433. [PubMed] [Google Scholar]
- 2.Mödder U. Nasennebenhöhlenerkrankungen - Möglichkeiten und Grenzen der Radiologie. Röntgenblätter. 1989;42:166–169. [PubMed] [Google Scholar]
- 3.DeLano MC, Fun FY, Zinreich SJ. Relationship of the optic nerve to the posterior paranasal sinuses: a CT anatomic study. AJNR Am J Neuroradiol. 1996;17:669–675. [PMC free article] [PubMed] [Google Scholar]
- 4.Klimek L, Kainz J, Reul J, Mosges R. Vermeidung vaskulärer Komplikationen bei der endonasalen Nasennebenhöhlenchirurgie. Teil II: Prä- und intraoperative Bildgebung. HNO. 1993;41:582–586. [PubMed] [Google Scholar]
- 5.Mafee MF, Chow JM, Meyers R. Functional endoscopic sinus surgery: anatomy, CT screening, indications, and complications. AJR Am J Roentgenol. 1993;160:735–740. doi: 10.2214/ajr.160.4.8456654. [DOI] [PubMed] [Google Scholar]
- 6.Sonkens JW, Harnsberger HR, Blanch GM, Babbel RW, Hunt S. The impact of screening sinus CT on the planning of functional endoscopic sinus surgery. Otolaryngol Head Neck Surg. 1991;105:802–813. doi: 10.1177/019459989110500606. [DOI] [PubMed] [Google Scholar]
- 7.Wayoff M. Medicolegal implications of sinus surgery. Acta Otorhinolaryngol Belg. 1992;46:343–350. [PubMed] [Google Scholar]
- 8.AWMF. Dentale Volumentomographie. Leitlinien der Deutsche Gesellschaft für Zahn-, Mund- und Kieferheilkunde (DGZMK) AWMF Leitlinienregister Nr. 083-005. www.awmf.de (last accessed on 2 January 2014)
- 9.AWMF. Radiologische Diagnostik im Kopf-Hals-Bereich. Leitlinien der Deutschen Röntgengesellschaft (DRG) AWMF Leitlinien-Register 039-022 bis 039-090. www.awmf.de (last accessed on 2 January 2014)
- 10.AWMF. Rhinosinusitis. Leitlinie der Deutschen Gesellschaft für Hals-Nasen-Ohrenheilkunde, Kopf und Halschirurgie. AWMF Leitlinienregister Nr. 017-049. www.awmf.de (last accessed on 2 January 2014)
- 11.Burke TF, Guertler AT, Timmons JH. Comparison of sinus x-rays with computed tomography scans in acute sinusitis. Acad Emerg Med. 1994;1:235–239. doi: 10.1111/j.1553-2712.1994.tb02437.x. [DOI] [PubMed] [Google Scholar]
- 12.Croft CB, Whittet HB, Fisher EW, Lloyd GA, Wright A. Polytomographic radiology in the diagnosis and management of maxillary antral disease as determined by antroscopy. Clin Otolaryngol. 1991;16:62–69. doi: 10.1111/j.1365-2273.1991.tb01945.x. [DOI] [PubMed] [Google Scholar]
- 13.Garcia DP, Corbett ML, Eberly SM, Joyce MR, Le HT, Karibo JM, et al. Radiographic imaging studies in pediatric chronic sinusitis. J Allergy Clin Immunol. 1994;94:523–530. doi: 10.1016/0091-6749(94)90209-7. [DOI] [PubMed] [Google Scholar]
- 14.Iinuma T, Hirota Y, Kase Y. Radio-opacity of the paranasal sinuses. Conventional views and CT. Rhinology. 1994;32:134–136. [PubMed] [Google Scholar]
- 15.Innis W, Byrne P, Tufano RP. Image-guided osteoplastic frontal sinusotomy. Am J Rhinol. 2005;19:430–434. [PubMed] [Google Scholar]
- 16.Klose KC, Elies W, Sondermann U. Treffsicherheit der Nativradiologie im Nachweis von Verschattungen der pneumatisierten Räume des Schädels - Vergleich mit der Computertomographie. Fortschr Röntgenstr. 1991;155:199–206. doi: 10.1055/s-2008-1033247. [DOI] [PubMed] [Google Scholar]
- 17.McAlister WH, Lusk R, Muntz HR. Comparison of plain radiographs and coronal CT scans in infants and children with recurrent sinusitis. AJR Am J Roentgenol. 1989;153:1259–1264. doi: 10.2214/ajr.153.6.1259. [DOI] [PubMed] [Google Scholar]
- 18.Moseley IF. The plain radiograph in ophthalmology: a wasteful and potentially dangerous anachronism. J R Soc Med. 1991;84:76–80. doi: 10.1177/014107689108400207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schuknecht B, Simmen D. Stellenwert radiologischer Bildgebung der Nasennebenhöhlen. Laryngorhinootologie. 2002;81:126–146. doi: 10.1055/s-2002-23114. [DOI] [PubMed] [Google Scholar]
- 20.Vestring T, Erlemann R, Wiesmann W, Bongartz G, Adolph J, Classen U, et al. Die diagnostische Sicherheit der okzipitomentalen Nasennebenhöhlenaufnahme. Korrelation mit der Magnetresonanztomographie. Radiologe. 1991;31:545–549. [PubMed] [Google Scholar]
- 21.Vogl TJ, Mack MG, Balzer J. Chronische Infektionen der Nasennebenhöhlen. Radiologe. 2000;40:500–506. doi: 10.1007/s001170050747. [DOI] [PubMed] [Google Scholar]
- 22.Yousem DM. Imaging of sinonasal inflammatory disease. Radiology. 1993;188:303–314. doi: 10.1148/radiology.188.2.8327669. [DOI] [PubMed] [Google Scholar]
- 23.Zinreich SJ. Imaging of chronic sinusitis in adults: X-ray, computed tomography, and magnetic resonance imaging. J Allergy Clin Immunol. 1992;90:445–451. doi: 10.1016/0091-6749(92)90167-z. [DOI] [PubMed] [Google Scholar]
- 24.Feuerman T, Wackym PA, Gade GF, Becker DP. Value of skull radiography, head computed tomographic scanning, and admission for observation in cases of minor head injury. Neurosurgery. 1988;22:449–453. doi: 10.1227/00006123-198803000-00001. [DOI] [PubMed] [Google Scholar]
- 25.Gibson TC. Skull X-rays in minor head injury. A review of their use and interpretation by casualty officers. Scott Med J. 1983;28:132–137. doi: 10.1177/003693308302800207. [DOI] [PubMed] [Google Scholar]
- 26.Jend HH, Helkenberg G. Über den Wert der konventionellen Schädelaufnahmen nach Kopfverletzungen. RöFo. 1995;162:7–12. doi: 10.1055/s-2007-1015826. [DOI] [PubMed] [Google Scholar]
- 27.Lloyd DA, Carty H, Patterson M, Butcher CK, Roe D. Predictive value of skull radiography for intracranial injury in children with blunt head injury. Lancet. 1997;349:821–824. doi: 10.1016/S0140-6736(96)09356-7. [DOI] [PubMed] [Google Scholar]
- 28.Masters SJ, McClean PM, Arcarese JS, Brown RF, Campbell JA, Freed HA, et al. Skull x-ray examinations after head trauma. Recommendations by a multidisciplinary panel and validation study. N Engl J Med. 1987;316:84–91. doi: 10.1056/NEJM198701083160205. [DOI] [PubMed] [Google Scholar]
- 29.Cohnen M, Fischer H, Hamacher J, Lins E, Kotter R, Mödder U. CT of the head by use of reduced current and kilovoltage: relationship between image quality and dose reduction. AJNR Am J Neuroradiol. 2000;21:1654–1660. [PMC free article] [PubMed] [Google Scholar]
- 30.Cohnen M, Kemper J, Mobes O, Pawelzik J, Mödder U. Radiation dose in dental radiology. Eur Radiol. 2002;12:634–637. doi: 10.1007/s003300100928. [DOI] [PubMed] [Google Scholar]
- 31.Diederichs CG, Engelke WG, Richter B, Hermann KP, Oestmann JW. Must radiation dose for CT of the maxilla and mandible be higher than that for conventional panoramic radiography? AJNR Am J Neuroradiol. 1996;17:1758–1760. [PMC free article] [PubMed] [Google Scholar]
- 32.Lorenzen M, Wedegartner U, Weber C, Lockemann U, Adam G, Lorenzen J. Dosisoptimierung der Mehrzeilen-Spiral-CT (MSCT) des Mittelgesichts. Fortschr Röntgenstr. 2005;177:265–271. doi: 10.1055/s-2004-813951. [DOI] [PubMed] [Google Scholar]
- 33.AWMF. AWMF Leitlinien-Register 064-011. Kopfschmerz bei Kindern - Bildgebende Diagnostik. Leitlinien der Gesellschaft für Pädiatrische Radiologie (GPR) www.awmf.de (last accessed on2 January 2014) [Google Scholar]
- 34.Strahlenschutzkommission (SSK) Empfehlung der Strahlenschutzkommission, verabschiedet in der 231. Orientierungshilfe für bildgebende Untersuchungen. Sitzung der SSK am 09./10.12.2008. BAnz. 2010; Nr. 5a vom 12.01.2010. [Google Scholar]
- 35.American College of Radiology (ACR) www.acr.org/Quality-Safety/Appropriateness-Criteria. ACR Appropriateness Criteria. (last accessed on 2 January 2014) [Google Scholar]
- 36.AWMF. AWMF Leitlinienregister Nr. 030-110. Diagnostik und apparative Zusatzuntersuchungen bei Kopfschmerzen. Deutsche Gesellschaft für Neurologie (DGN) www.awmf.de (last accessed on 2 January 2014) [Google Scholar]
- 37.European Commission. Update Mars. 2008. Radiation Protection 118: Referral guidelines for imaging. http://ec.europa.eu/energy/nuclear/radioprotection/publication/doc/118_update_en.pdf(last accessed on 2 January 2014) [Google Scholar]
- 38.European Commission. Evidence based guidelines. Radiation Protection 172: Cone Beam CT for Dental and Maxillofacial Radiology. http://www.sedentexct.eu/files/radiation_protection_172.pdf (last accessed on 2 January 2014) [Google Scholar]
- 39.AWMF. AWMF Leitlinienregister Nr. 064-011. Kopfschmerz - Bildgebende Diagnostik. Leitlinie der Ges. f. Pädiatrische Radiologie. www.awmf.de (last accessed on 2 January 2014) [Google Scholar]
- 40.Strahlenschutzkommission (SSK) Zusammenfassung und Bewertung der Jahrestagung 2010 der Strahlenschutzkommission: Medizinischer Fortschritt und Strahlenschutz. Stellungnahme der Strahlenschutzkommission Verabschiedet in der 248. Sitzung der Strahlenschutzkommission am 14./15. April 2011. BAnz. 2011; Nr. 168 vom 09.11.2011 [Google Scholar]
- e1.Zinreich SJ, Kennedy DW, Rosenbaum AE, Gayler BW, Kumar AJ, Stammberger H. Paranasal sinuses: CT imaging requirements for endosopic surgery. Radiology. 1987;163:769–775. doi: 10.1148/radiology.163.3.3575731. [DOI] [PubMed] [Google Scholar]
- e2.Schwickert HC, Cagil H, Kauczor HU, Schweden F, Riechelmann H, Thelen M. CT und MRT der Nasennebenhöhlen [CT and MRT of the paranasal sinuses] Aktuelle Radiol. 1994;4:88–96. [PubMed] [Google Scholar]
- e3.Eggesbo HB, Sovik S, Dolvik S, Eiklid K, Kolmannskog F. Proposal of a CT scoring system of the paranasal sinuses in diagnosing cystic fibrosis. Eur Radiol. 2003;13:1451–1460. doi: 10.1007/s00330-003-1825-8. [DOI] [PubMed] [Google Scholar]
- e4.Ramadan HH, Fornelli R, Ortiz AO, Rodman S. Correlation of allergy and severity of sinus disease. Am J Rhinol. 1999;13:345–347. doi: 10.2500/105065899781367500. [DOI] [PubMed] [Google Scholar]
- e5.Borman KR, Brown PM, Mezera KK, Jhaveri H. Occult fever in surgical intensive care unit patients is seldom caused by sinusitis. Am J Surg. 1992;164:412–415. doi: 10.1016/s0002-9610(05)81171-7. [DOI] [PubMed] [Google Scholar]
- e6.Oberholzer K, Kauczor HU, Heussel CP, Derigs G, Thelen M. Klinische Relevanz der NNH-CT vor Knochenmarktransplantation. Fortschr Röntgenstr. 1997;166:493–497. doi: 10.1055/s-2007-1015465. [DOI] [PubMed] [Google Scholar]
- e7.Koitschev A, Baumann I, Remy CT, Dammann F. Rationelle CT-Diagnostik vor Operationen an den Nasennebenhöhlen. HNO. 2002;50:217–222. doi: 10.1007/s001060100540. [DOI] [PubMed] [Google Scholar]
- e8.Knörgen M, Brandt S, Kösling S. Qualitätsvergleich digitaler 3D-fähiger Röntgenanlagen bei HNO-Fragestellungen am Schläfenbein und den Nasennebenhöhlen. RöFo. 2012;184:1153–1160. doi: 10.1055/s-0032-1325343. [DOI] [PubMed] [Google Scholar]
- e9.Zoumalan RA, Lebowitz RA, Wang E, Yung K, Babb JS, Jacobs JB. Flat panel cone beam computed tomography of the sinuses. Otolaryngol Head Neck Surg. 2009;140:841–844. doi: 10.1016/j.otohns.2009.01.010. [DOI] [PubMed] [Google Scholar]
- e10.Fischer B, Wit J. Das Schädel-Hirn-Trauma des Kindes in der Notfallambulanz. Unfallchirurg. 2007;110:226–232. doi: 10.1007/s00113-006-1209-z. [DOI] [PubMed] [Google Scholar]
- e11.AWMF. AWMF Leitlinienregister Nr. 012-019. S3 - Leitlinie Polytrauma/ Schwerverletzten-Behandlung. Leitlinien der Deutsche Gesellschaft für Unfallchirurgie. www.awmf.de (last accessed on 2 January 2014) [Google Scholar]
- e12.Langen HJ, Daus HJ, Bohndorf K, Klose K. Konventionelle Röntgenuntersuchung und Computertomographie bei der Diagnostik von Orbitafrakturen. RöFo. 1989;150:582–587. doi: 10.1055/s-2008-1047081. [DOI] [PubMed] [Google Scholar]
- e13.Kösling S, Brandt S, Neumann K. Bildgebung des Schläfenbeins. Radiologe. 2010;50:711–734. doi: 10.1007/s00117-010-2027-4. [DOI] [PubMed] [Google Scholar]
- e14.Lemmerling MM, De FB, Verbist BM, VandeVyver V. Imaging of inflammatory and infectious diseases in the temporal bone. Neuroimaging Clin N Am. 2009;19:321–337. doi: 10.1016/j.nic.2009.06.006. [DOI] [PubMed] [Google Scholar]
- e15.Brunner E, Turk R, Swoboda H, Imhof H, Schratter M. Die Bedeutung der Computertomographie für die Mittelohrdiagnose. Laryngol Rhinol Otol. Stuttgart. 1986;65:327–330. [PubMed] [Google Scholar]
- e16.Struffert T, Grunwald IQ, Papanagiotou P, Politi M, Roth C, Reith W. Diagnostik des Felsenbeins. Ein Überblick. Radiologe. 2005;45:816–827. doi: 10.1007/s00117-005-1269-z. [DOI] [PubMed] [Google Scholar]
- e17.Dalchow CV, Weber AL, Yanagihara N, Bien S, Werner JA. Digital volume tomography: radiologic examinations of the temporal bone. AJR Am J Roentgenol. 2006;186:416–423. doi: 10.2214/AJR.04.1353. [DOI] [PubMed] [Google Scholar]
- e18.Bornstein MM, Wolner-Hanssen AB, Sendi P, von AT. Comparison of intraoral radiography and limited cone beam computed tomography for the assessment of root-fractured permanent teeth. Dent Traumatol. 2009;25:571–577. doi: 10.1111/j.1600-9657.2009.00833.x. [DOI] [PubMed] [Google Scholar]
- e19.AWMF. AWMF Leitlinienregister Nr. 017-025. Obstruktive Sialadenitis. Leitlinie der Deutschen Gesellschaft für Hals-Nasen-Ohrenheilkunde, Kopf und Halschirurgie. www.awmf.de (last accessed on 2 January 2014)) [Google Scholar]
- e20.IQWiG - Institut für Qualität und Wirtschaftlichkeit im Gesundheitswesen. www. 2011; https://www.iqwig.de/download/D06-01B_Kurzfassung_AB_PET_und_PET-CT_bei_Kopf-Halstumoren.pdf. Abschlussbericht D06-01B - PET und PET/CT bei Kopf- und Halstumoren. (last accessed on 2 January 2014) [Google Scholar]
- e21.Alder ME, Deahl ST, Matteson SR. Clinical usefulness of two-dimensional reformatted and three-dimensionally rendered computerized tomographic images: literature review and a survey of surgeons’ opinions. J Oral Maxillofac Surg. 1995;53:375–386. doi: 10.1016/0278-2391(95)90707-6. [DOI] [PubMed] [Google Scholar]
- e22.Bernhardt TM, Rapp-Bernhardt U, Fessel A, Ludwig K, Reichel G, Grote R. CT scanning of the paranasal sinuses: axial helical CT with reconstruction in the coronal direction versus coronal helical CT. Br J Radiol. 1998;71:846–851. doi: 10.1259/bjr.71.848.9828797. [DOI] [PubMed] [Google Scholar]
- e23.Dammann F, Bode A, Heuschmid M, Kopp A, Georg C, Pereira PL, et al. Mehrschicht-Spiral-CT der Nasennebenhöhlen: Erste Erfahrungen unter besonderer Berücksichtigung der Strahlenexposition. Fortschr Röntgenstr. 2000;172:701–706. doi: 10.1055/s-2000-7175. [DOI] [PubMed] [Google Scholar]
- e24.Lang S, Jäger L, Grevers G. Zur Aussagefähigkeit koronarer Sekundärrekonstruktionen computertomographischer Sequenzen der Nasennebenhöhlen. Laryngorhinootologie. 2002;81:418–421. doi: 10.1055/s-2002-32212. [DOI] [PubMed] [Google Scholar]
- e25.Deutsche Röntgengesellschaft. http://www.ag-kopf-hals.drg.de/seite/295/stellungnahmen-und-empfehlungen. Empfehlungen CT-Untersuchungsprotokolle. (last accessed on 2 January 2014) [Google Scholar]
- e26.Kropil P, Cohnen M, Andersen K, Heinen W, Stegmann V, Mödder U. Bildqualität in der Multidetektor-CT der Nasennebenhöhlen: Potenzial zur Dosisreduktion bei Anwendung eines adaptiven Nachverarbeitungsfilters. Fortschr Röntgenstr. 2010;182:973–978. doi: 10.1055/s-0029-1245586. [DOI] [PubMed] [Google Scholar]
- e27.Guldner C, Diogo I, Windfuhr J, Bien S, Teymoortash A, Werner JA, et al. Analysis of the fossa olfactoria using cone beam tomography (CBT) Acta Otolaryngol. 2011;131:72–78. doi: 10.3109/00016489.2010.506653. [DOI] [PubMed] [Google Scholar]
- e28.Peltonen LI, Aarnisalo AA, Kaser Y, Kortesniemi MK, Robinson S, Suomalainen A, et al. Cone-beam computed tomography: a new method for imaging of the temporal bone. Acta Radiol. 2009;50:543–548. doi: 10.1080/02841850902839700. [DOI] [PubMed] [Google Scholar]
- e29.Abolmaali N, Hummel T, Damm M. Moderne bildgebende Diagnostik bei Riechstörungen. Laryngorhinootologie. 2009;88:10–16. doi: 10.1055/s-2008-1077630. [DOI] [PubMed] [Google Scholar]
- e30.Antila J, Sonninen P, Grenman R. MRI and plain radiographics in acute frontal sinus infections. Rhinology. 1993;31:145–149. [PubMed] [Google Scholar]
- e31.Boeddinghaus R, Whyte A. Current concepts in maxillofacial imaging. Eur J Radiol. 2008;66:396–418. doi: 10.1016/j.ejrad.2007.11.019. [DOI] [PubMed] [Google Scholar]
- e32.Grindle CR, Curry JM, Kang MD, Evans JJ, Rosen MR. Preoperative magnetic resonance imaging protocol for endoscopic cranial base image-guided surgery. Am J Otolaryngol. 2011;32:451–454. doi: 10.1016/j.amjoto.2010.08.003. [DOI] [PubMed] [Google Scholar]
- e33.Hähnel S, Ertl-Wagner B, Tasman AJ, Forsting M, Jansen O. Relative value of MR imaging as compared with CT in the diagnosis of inflammatory paranasal sinus disease. Radiology. 1999;210:171–176. doi: 10.1148/radiology.210.1.r99ja36171. [DOI] [PubMed] [Google Scholar]
- e34.Weiss F, Habermann CR, Welger J, Knaape A, Metternich F, Steiner P, et al. MRT in der präoperativen Diagnostik der chronischen Sinusitis im Vergleich mit der CT. RöFo. 2001;173:319–324. doi: 10.1055/s-2001-12458. [DOI] [PubMed] [Google Scholar]
- e35.Eggesbo HB, Ringertz S, Haanaes OC, Dolvik S, Erichsen A, Stiris M, et al. CT and MR imaging of the paranasal sinuses in cystic fibrosis. Correlation with microbiological and histopathological results. Acta Radiol. 1999;40:154–162. doi: 10.3109/02841859909177731. [DOI] [PubMed] [Google Scholar]
- e36.Bovenschulte H, Schluter-Brust K, Liebig T, Erdmann E, Eysel P, Zobel C. Kernspintomographie bei Schrittmacherpatienten - Überblick und prozedurales Management. Dtsch Arztebl Int. 2012;109:270–275. doi: 10.3238/arztebl.2012.0270. [DOI] [PMC free article] [PubMed] [Google Scholar]