Abstract
Background
Symptoms of gastroparesis based on patient recall correlate poorly with gastric emptying.
Aim
To determine if symptoms recorded during gastric emptying scintigraphy (GES) correlate with gastric emptying and with symptoms based on patient recall.
Methods
Patients undergoing GES completed the Patient Assessment of GI Symptoms (PAGI-SYM) assessing symptoms over the prior 2 weeks and a questionnaire for which patients graded six symptoms during GES. A Symptom Severity Index (SSI) represented the mean of six symptoms at each time point.
Key Results
560 patients underwent GES for clinical evaluation of symptoms. Of 388 patients included in the study: 232 patients had normal GES (NGES), 156 delayed GES (DGES), and 11 rapid GES (RGES). SSI increased pre- to postprandial for each group: NGES: 0.51±0.07 to 0.92±0.03, DGES: 0.60±0.09 to 1.13±0.05, and RGES: 0.56±0.12 to 0.79±0.13. DGES patients had a higher postprandial SSI than NGES patients (1.13±0.05 vs 0.92±0.03, p<0.05). Postprandial symptoms of stomach fullness (1.9±0.12 vs 1.5±0.09; p=0.011), bloating (1.4±0.11 vs 1.1±0.09; p =0.033), and abdominal pain (1.1±0.08 vs 0.7±0.12; p=0.012) were higher in DGES than NGES. Symptom severity based on PAGI-SYM for 2 weeks prior to GES correlated with symptoms during the test for nausea (NGES r=0.61, DGES r=0.70), stomach fullness (NGES r=0.47, DGES r=0.60), and bloating (NGES r=0.62, DGES r=0.66).
Conclusions & Inferences
Stomach fullness, bloating, and abdominal pain recorded during GES were higher in patients with delayed gastric emptying than in patients with normal gastric emptying. Symptoms recorded during GES correlated with those during daily life by patient recall.
Keywords: gastroparesis, gastric emptying
INTRODUCTION
Gastroparesis is a chronic disorder characterized by delayed gastric emptying (1). Common categories of gastroparesis include idiopathic, diabetes mellitus, and post-surgical vagus nerve damage. Symptoms may include nausea, vomiting, abdominal discomfort, bloating, early satiety, and stomach fullness. Though extensively studied, the mechanism(s) causing symptoms in gastroparesis remains unknown (2). Symptoms may be related to the global delay in gastric emptying that defines gastroparesis or to other causes including antral hypomotility, impaired fundic accommodation, antral distention, gastric dysrhythmias, and visceral hypersensitivity (3,4).
Symptom correlations with delayed gastric emptying are variable for diabetic gastropathy, idiopathic gastroparesis, and functional dyspepsia. Early satiety, postprandial fullness, and vomiting have been reported to be associated with delayed emptying in patients with functional dyspepsia (5,6). Of dyspeptic patients undergoing GES for clinical evaluation, nausea and vomiting were found to be associated with the rate of GES (7). Interestingly, some patients with functional dyspepsia may have rapid gastric emptying with symptoms similar to patients with delayed gastric emptying (8). In patients with diabetes, abdominal fullness, bloating, and upper abdominal pain have been associated with delayed gastric emptying (9,10). Some studies, however, have shown a poor correlation between gastric emptying and severity of gastric symptoms in diabetic patients (11,12).
Prior studies exploring the relationship of symptoms to gastric emptying abnormalities have generally been limited to a small sample size with symptoms quantified based on patient recall. A lack of a standardized gastric emptying test also has limited uniformity of testing and credibility of results (13). To overcome these deficiencies, this study investigated real-time gastroparetic symptoms during GES using the consensus-standardized 4 hour GES (13,14). The aim of this study was to determine if there is an association between delayed gastric emptying and symptoms of gastroparesis as recorded during GES. Symptoms based on a 2 week recall also were compared with symptoms during the gastric emptying test. The relationships between diabetes, symptom severity, and GES results were investigated.
METHODS
Overview
The study population included patients undergoing gastric emptying scintigraphy for clinical evaluation over the time period September 1, 2007 to September 1, 2008.
Gastric emptying scintigraphy (GES)
Patients reported to the Nuclear Medicine imaging department in the fasting condition. GES was performed after ingestion of a standard 99mTc-sulfur colloid radiolabeled liquid egg white (Eggbeaters®) sandwich with jam and 300 cc of water. Specifically, the meal consisted of 4 oz. (120 g, equal to two large eggs) liquid egg white (99% real eggs, cholesterol-free, fat-free, and low-calorie); two slices of white bread (120 kcal), strawberry jam (30 g, 74 kcal), water (120 mL). The total caloric value of the meal was 255 kcal (72% carbohydrate, 24% protein, 2% fat and 2% fiber) (13,14). The egg white was radiolabeled with technetium-99m sulfur colloid, 0.5 mCi. The radiolabeled meal was consumed and scintigraphic images were obtained at 0, 30, 60, 120, 180, and 240 minutes after meal ingestion. The geometric center of the decay-corrected anterior and posterior counts was calculated for each time point. Gastric emptying was analyzed as the percent of radioactivity retained in the stomach over time (14,15). Abnormalities in gastric emptying were defined using the imaging data from the 1, 2, and 4-hour imaging intervals (13,14). Solid emptying was considered delayed if gastric retention was >60% at 2 hours and/or >10% at 4 hours as reported by Tougas et al (14). Rapid emptying was defined as having <35% retention (>65% emptied) at 1 hour (13). Normal [NGES]) was defined if the result was neither delayed nor rapid.
Symptom questionnaires
Patients filled out 3 questionnaires during GES. First, they completed a demographics questionnaire that asked about age, gender, main symptom for which GES is being performed, presence of diabetes, morning glucose level, medications (including pain and prokinetic medications), and prior gastrointestinal surgery. Second, patients completed the Patient Assessment of GI Symptoms Questionnaire (PAGI-SYM) (16,17) which asks patients to grade twenty symptoms of gastroparesis, functional dyspepsia, and gastroesophageal reflux disease for their severity over the prior 2 weeks. The PAGI-SYM includes the nine symptoms of the Gastroparesis Cardinal Symptom Index (GCSI) (18,19). Additional questions asked about constipation, diarrhea, the number of vomiting episodes per day and the number of bowel movements per week. Third, patients filled out a GES Symptom Questionnaire devised from Arts et al (19) for which patients grade six gastroparetic symptoms (abdominal pain, bloating, stomach fullness, nausea, belching, abdominal burning) on a scale of 0 (none) to 3 (severe). Patients graded their symptoms preprandially and at 0, 0.5, 1, 2, 3, 4 hrs postprandially at the time of imaging for the solid-phase EggBeaters GES.
Data analysis
Symptoms during GES were compared with the GES results and with the PAGI-SYM results. A Symptom Severity Index (SSI) for each time point during the GES represented the mean of the six symptoms at each time point. The serial postprandial SSI values at 0, 0.5, 1, 2, 3, 4 hrs postprandially during the GES were averaged for an Overall Postprandial SSI.
Symptoms of diabetics with delayed gastric emptying (diabetic gastroparesis) and non-diabetic non-postsurgical gastroparesis (idiopathic gastroparesis) were determined and compared. Only patients with known diabetes or known to be non-diabetic were compared.
Results are expressed as mean ± SEM. Groups were compared using ANOVA and students t test with Bonferroni correction for multiple comparisons where appropriate. Spearman’s correlation was used to determine the correlation between the symptoms during GES with symptoms passed on patient recall using the PAGI-SYM.
RESULTS
560 patients underwent GES between September 1, 2007 and September 1, 2008 for clinical evaluation of dyspeptic symptoms. Of these, 409 patients met the study inclusion criteria: no prior gastric surgery, and no use of prokinetics or narcotic analgesic medications within 48 hrs of GES. 232 patients had NGES, 156 had DGES, and 11 had RGES. Table 1 shows demographic information for the different study groups.
Table 1.
Patient Characteristics
| Overall Study Group |
Patients with Normal GES (NGES) |
Patients with Delayed GES (DGES) |
Patients with Rapid GES (RGES) |
|
|---|---|---|---|---|
| Number of Patients | 409 | 232 | 156 | 11 |
| Average Age (yrs) | 46.1 | 46.5 | 45.6 | 51.8 |
| Gender (%) | 73% F | 70% F | 78% F | 63% F |
| Weight (avg lbs) | 163.2 | 165.1 | 159 | 221.7 |
| BMI (average) | 26.8 | 26.7 | 27.2 | 35.6 |
| Diabetes (# of Patients) | 73 | 33 | 35 | 5 |
Table 2 shows the mean symptom scores during the GES for each of the six symptoms and the SSI for each group (NGES, DGES, RGES) for each time point during the gastric emptying test. Each group’s SSI, representing the average of the six symptoms, increased pre- to postprandial. For NGES, the SSI increased from 0.51±0.03 to a maximum of 0.92±0.03 (p<0.05) at one hour postprandially. For DGES, the SSI increased from 0.60±0.04 to a maximum of 1.13±0.05 (p<0.01) at one hour postprandially. For RGES, the SSI increased from 0.56±0.12 to a maximum of 0.79±0.13 (p<0.05) at 30 minutes postprandially. The DGES patients had a higher maximal postprandial SSI than NGES patients (1.13±0.05 vs 0.92±0.03, p<0.05).
Table 2.
Symptoms During Egg Beaters Test for the NGES, DGES, and RGES groups.
| Before meal |
0 hour | 0.5 hour | 1 hour | 2 hour | 3 hour | 4 hour | |
|---|---|---|---|---|---|---|---|
| Patients with Normal Gastric Emptying (n=232) | |||||||
| Abdominal pain | 0.47±0.07 | 0.67±0.08 | 0.75±0.08 | 0.72±0.08 | 0.62±0.08 | 0.60±0.08 | 0.63±0.08 |
| Nausea | 0.67±0.08 | 0.87±0.09 | 0.89.±0.09 | 0.91.±0.09 | 0.80±0.09 | 0.75±0.09 | 0.71±0.09 |
| Stomach fullness | 0.60±0.08 | 1.61±0.09 | 1.58±0.09 | 1.47±0.09 | 1.23±0.09 | 1.01±0.09 | 0.82±0.10 |
| Bloating | 0.60±0.08 | 1.01±0.09 | 1.07±0.10 | 1.12±0.09 | 0.94±0.09 | 0.89±0.09 | 0.730±.09 |
| Abd burning | 0.26±0.06 | 0.33±0.06 | 0.35±0.07 | 0.48±0.08 | 0.45±0.08 | 0.39±0.07 | 0.40±0.08 |
| Belching | 0.48±0.07 | 0.78±0.08 | 0.81±0.08 | 0.81±0.08 | 0.740±.08 | 0.65±0.08 | 0.65±0.08 |
| SSI | 0.51±0.07 | 0.88±0.03 | 0.91±0.03 | 0.92±0.03 | 0.80±0.03 | 0.71±0.03 | 0.65±0.03 |
| Patients with Delayed Gastric Emptying (n=156) | |||||||
| Abdominal pain | 0.69±0.10 | 0.94±0.11 | 1.08±0.12 | 1.10±0.12 | 1.10±0.11 | 1.03±0.12 | 0.81±0.11 |
| Nausea | 0.80±0.11 | 1.08±0.12 | 1.10±0.12 | 1.16±0.13 | 1.11±0.12 | 1.07±0.12 | 0.80±0.12 |
| Stomach fullness | 0.66±0.10 | 1.84±0.12 | 1.84±0.12 | 1.87±0.12 | 1.53±0.11 | 1.30±0.11 | 1.10±0.12 |
| Bloating | 0.72±0.10 | 1.20±0.11 | 1.35±0.12 | 1.45±0.11 | 1.27±0.11 | 1.15±0.11 | 1.02±0.11 |
| Abd burning | 0.27±0.08 | 0.33±0.08 | 0.37±0.08 | 0.40±0.08 | 0.56±0.10 | 0.62±0.10 | 0.54±0.09 |
| Belching | 0.49±0.09 | 0..82±0.10 | 0.90±0.10 | 0.81±0.10 | 0.87±0.11 | 0.77±0.11 | 0.77±0.11 |
| SSI | 0.60±0.09 | 1.04±0.05 | 1.11±0.05 | 1.13±0.05 | 1.08±0.04 | 0.99±0.04 | 0.82±0.04 |
| Patients with Rapid Gastric Emptying (n=11) | |||||||
| Abdominal pain | 0.50±0.26 | 0.66±0.28 | 0.66±0.28 | 0.55±0.29 | 0.44±0.24 | 0.50±0.28 | 1.16±0.37 |
| Nausea | 0.50±0.26 | 1.11±0.42 | 0.77±0.36 | 0.66±0.28 | 0.55±0.29 | 0.44±0.17 | 0.88±0.42 |
| Stomach fullness | 0.50±0.37 | 1.00±0.44 | 0.77±0.36 | 0.77±0.40 | 0.66±0.33 | 0.66±0.33 | 0.88±0.38 |
| Bloating | 0.75±0.31 | 0.77±0.36 | 1.00±0.37 | 1.00±0.37 | 0.77±0.32 | 0.88±0.30 | 1.37±0.46 |
| Abd burning | 0.37±0.26 | 0.66±0.37 | 0.66±0.37 | 0.55±0.29 | 0.55±0.29 | 0.22±0.14 | 0.55±0.37 |
| Belching | 0.75±0.36 | 0.33±0.16 | 0.88±0.30 | 0.44±0.29 | 0.55±0.33 | 0.88±0.26 | 1.22±0.36 |
| SSI | 0.56±0.12 | 0.75±0.14 | 0.79±0.13 | 0.66±0.12 | 0.59±0.11 | 0.60±0.10 | 0.65±0.15 |
Results expressed as mean± SEM for each time point.
The serial postprandial SSI values at 0, 0.5, 1, 2, 3, 4 hrs postprandially during the GES were averaged for an Overall Postprandial SSI. The Overall Postprandial SSI was higher than the preprandial SSI for NGES, DGES and RGES patients. Patients with DGES had a significantly higher Overall Postprandial SSI (1.02±0.05; p<0.05) than patients with NGES (0.81±0.03) and patients with RGES (0.67±0.12).
The individual six symptoms recorded by the patients during the GES were also assessed (Table 2). During the gastric emptying test, postprandial symptoms of stomach fullness (1.87±0.12 vs 1.61±0.09; p=0.011), bloating (1.45±0.11 vs 1.12±0.09; p =0.033), and abdominal pain (1.10±0.11 vs 0.75±0.08; p=0.012) were significantly higher in DGES than in NGES patients, but there was no statistical difference for the symptoms of belching (p=0.24), nausea (p=0.13), or abdominal burning (p=0.19) (Table 2 and Figures 1,2,3,). Most of these postprandial symptoms were maximal at 1 hour after meal ingestion (Figures 1,2,3). Of the six symptoms measured, stomach fullness was the graded highest in severity in patients with DGES (Table 2).
Figure 1.
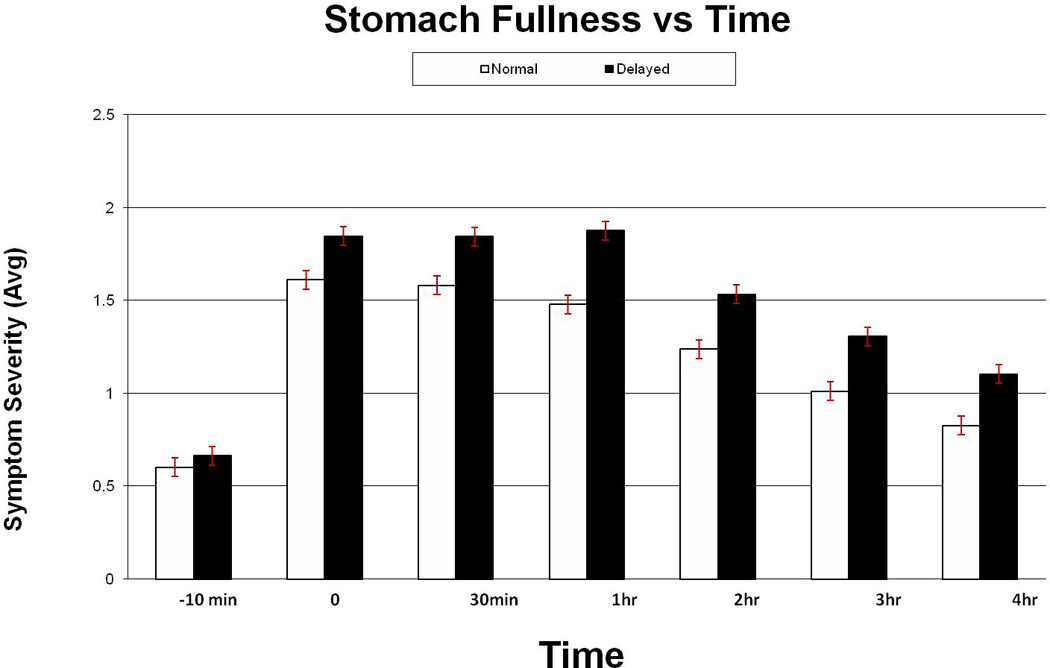
Temporal relation of stomach fullness severity during GES. Symptoms of stomach fullness during GES were significantly higher in DGES compared to NGES patients at 1 hour (p=0.01), 2 hours (p=0.05), and 3 hours (p=0.05).
Figure 2.
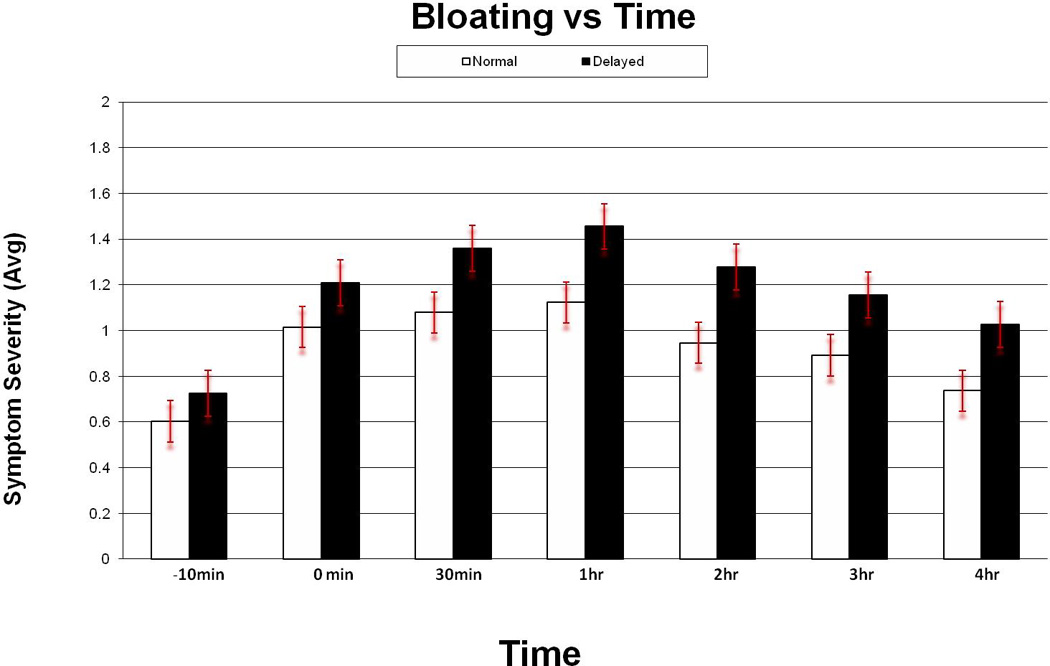
Temporal relation of abdominal bloating severity during GES. Symptoms of bloating during GES were significantly higher in DGES compared to NGES patients at 1 hour (p=0.03) and at 2 hours (p=0.02).
Figure 3.
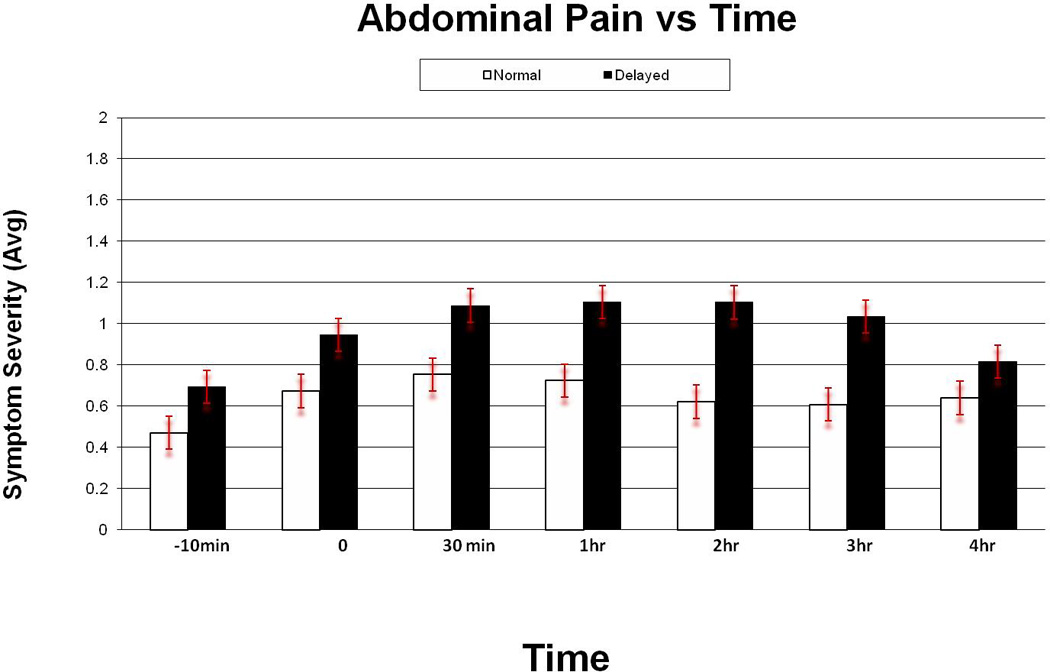
Temporal relation of abdominal pain severity during GES. Symptoms of abdominal pain during GES were significantly higher in DGES compared to NGES patients at 30 minutes (p=0.02), 1 hour (p=0.01), 2 hours (p=0.001), and at 2 hours (p=0.004).
Symptoms based on recall of the 2 week period prior to the GES as assessed with the PAGI-SYM are shown in Table 3. Patients with delayed GES had higher symptom recall scores for nausea (p=0.040), loss of appetite (p=0.020), not able to finish a meal (p =0.016), feeling excessively full after meals (p=0.048), and lower abdominal pain (p=0.04) than patients with normal GES. Two symptoms (not able to finish a normal size meal and feeling excessively full after meals) were rated with the highest severity in patients with DGES. Symptoms based on patient recall using the PAGI-SYM were mildly correlated with the 4 hour percent retention on gastric emptying scintigraphy for loss of appetite (r=0.129), feeling excessively full after meals (r=0.126), and not able to finish a full meal (r=0.125).
Table 3.
Symptoms by PAGI-SYM for the NGES, DGES, and RGES groups.
| NGE | DGE | RGE | |
|---|---|---|---|
| Nausea | 2.34±0.12 | 2.74±0.15 | 2.00±0.55 |
| Retching | 1.36±0.12 | 1.57±0.15 | 1.00±0.32 |
| Vomiting | 1.39±0.12 | 1.60±0.16 | 1.45±0.59 |
| Stomach fullness | 2.81±0.18 | 2.96±0.15 | 2.25±0.50 |
| Not able to finish a normal-size meal | 2.40±0.11 | 3.26±0.14 | 2.16±0.60 |
| Feeling excessively full after meals | 2.87±0.11 | 3.26±0.14 | 3.00±0.53 |
| Loss of appetite | 2.05±0.11 | 2.60±0.15 | 2.00±0.56 |
| Bloating | 2.53±0.11 | 2.60±0.14 | 2.25±0.41 |
| Stomach or belly visibly larger | 2.02±0.13 | 2.09±0.16 | 1.75±0.46 |
| Upper abdominal pain | 2.12±0.12 | 2.27±0.15 | 1.08±0.43 |
| Upper abdominal discomfort | 2.51±0.12 | 2.64±0.14 | 1.83±0.47 |
| Lower abdominal pain | 1.33±0.11 | 1.73±0.14 | 1.33±0.48 |
| Lower abdominal discomfort | 2.51±0.12 | 2.64±0.14 | 1.83±0.47 |
| Heartburn during the day | 1.84±0.11 | 1.57±0.14 | 1.25±0.32 |
| Heartburn when lying down | 1.75±0.12 | 1.75±0.12 | 1.58±0.35 |
| Feeling of discomfort inside chest during the day | 1.5±0.11 | 1.62±0.14 | 1.50±0.35 |
| Feeling of discomfort inside chest at night | 1.24±0.11 | 1.23±0.14 | 1.33±0.39 |
| Regurgitation or reflux during the day | 1.85±0.11 | 1.77±0.15 | 1.18±0.50 |
| Regurgitation or reflux when lying down | 1.86±0.11 | 1.68±0.16 | 1.54±0.45 |
| Bitter, acid or sour taste in mouth | 1.73±0.11 | 1.70±0.14 | 158±0.48 |
| Constipation | 1.76±0.12 | 2.04±0.16 | 1.25±0.49 |
| Diarrhea | 1.35±0.11 | 1.63±0.14 | 1.77±0.52 |
| Episodes of vomiting per week | 5.88±0.19 | 7.89±0.29 | 2.66±0.33 |
| Bowel movements per week | 9.08±0.70 | 8.09±0.83 | 16.9±1.10 |
Results expressed as mean ± SEM
Symptom severity based on PAGI-SYM for symptoms 2 weeks prior to GES correlated with symptoms during the test for nausea (NGES r=0.61; p<0.001, DGES r=0.70; p<0.0001), stomach fullness (NGES r=0.47; p<0.001, DGES r=0.60; p<0.001), and bloating (NGES r=0.62; p<0.001, DGES r=0.66; p<0.001). Overall, DGES patients had a higher correlation with the PAGI-SYM than the NGES patients.
Diabetes Mellitus
The symptoms of diabetic patients with delayed gastric emptying (diabetic gastroparesis) were compared to nondiabetic nonsurgical patients with delayed gastric emptying (idiopathic gastroparesis) (Table 4). Compared to fasting, during the GES, diabetic patients had an increase in their stomach fullness (0.68±0.21 to 1.57±0.27) and bloating (0.73±0.25 to 1.45±0.25). For idiopathic patients, the GES meal increased abdominal pain (0.66±0.12 to 1.25±0.14), stomach fullness (0.51±0.11 to 2.05±0.14), nausea (0.82±0.14 to 1.19±0.15), and bloating (0.64±0.12 to 1.43±0.14). Numerically, both groups graded stomach fullness as the most severe symptom. Stomach fullness was rated as more severe in patients with idiopathic gastroparesis than patients with diabetic gastroparesis at 0, 30 min, and 3 hrs postprandial. Idiopathic gastroparetics had a significantly higher SSI than diabetic gastroparetics at two time points during GES (0 hr, 0.5 hr) (table 4).
Table 4.
Symptoms during Eggbeaters Gastric Emptying Scintigraphy Test for patients with diabetic gastroparesis and idiopathic gastroparesis.
| Before Meal |
0 hour | 0.5 hour | 1 hour | 2 hour | 3 hour | 4 hour | |
|---|---|---|---|---|---|---|---|
| Diabetic Gastroparesis (n=35) | |||||||
| Abdominal pain | 0.68±0.23 | 0.65±0.24 | 0.80±0.25 | 0.85±0.24 | 0.80±0.23 | 0.77±0.26 | 0.86±0.30 |
| Nausea | 0.73±0.20 | 1.00±0.26 | 0.88±0.24 | 1.05±0.24 | 0.89±0.24 | 0.88±0.25 | 0.86±0.27 |
| Stomach fullness | 0.68±0.21 | 1.50±0.29 | 1.50±0.28 | 1.57±0.27 | 1.35±0.25 | 1.17±0.27 | 1.20±0.29 |
| Bloating | 0.73±0.25 | 1.00±0.22 | 1.10±0.25 | 1.45±0.25 | 1.26±0.25 | 1.11±0.25 | 1.14±0.27 |
| Abd burning | 0.20±0.11 | 0.21±0.12 | 0.21±0.12 | 0.15±0.11 | 0.40±0.19 | 0.61±0.25 | 0.65±0.27 |
| Belching | 0.65±0.25 | 0.71±0.25 | 0.86±0.24 | 0.78±0.27 | 1.0±0.28 | 0.94±0.30 | 0.96±0.32 |
| SSI | 0.61±0.08 | 0.84±0.10 | 0.90±0.10 | 0.98±0.10 | 0.94±0.10 | 0.91±0.10 | 0.94±0.11 |
| Idiopathic Gastroparesis (n=121) | |||||||
| Abdominal pain | 0.66±0.12 | 1.04±0.15 | 1.19±0.14 | 1.20±0.15 | 1.25±0.14 | 1.16±0.14 | 0.83±0.12 |
| Nausea | 0.82±0.14 | 1.10±0.15 | 1.14±0.15 | 1.18±0.16 | 1.19±0.15 | 1.09±0.15 | 0.76±0.14 |
| Stomach fullness | 0.51±0.11 | 2.00±0.14 | 2.05±0.14 | 2.01±0.14 | 1.60±0.14 | 1.34±0.14 | 1.09±0.14 |
| Bloating | 0.64±0.12 | 1.26±0.15 | 1.42±0.15 | 1.43±0.14 | 1.22±0.13 | 1.12±0.13 | 0.96±0.12 |
| Abd burning | 0.31±0.11 | 0.38±0.11 | 0.41±0.12 | 0.44±0.11 | 0.60±0.12 | 0.59±0.12 | 0.50±0.10 |
| Belching | 0.41±0.11 | 0.84±0.12 | 0.90±0.12 | 0.81±0.12 | 0.83±0.13 | 0.72±0.12 | 0.55±0.11 |
| SSI | 0.56±0.05 | 1.11±0.06 | 1.19±0.06 | 1.18±0.06 | 1.12±0.05 | 1.01±.05 | 0.78±0.05 |
Results expressed as mean ± SEM for each time point.
DISCUSSION
This study has examined patients undergoing gastric emptying scintigraphy in order to better appreciate the symptoms of patients with gastroparesis. We have shown that the postprandial symptoms of stomach fullness, bloating, and abdominal pain were higher in patients with delayed gastric emptying than in patients with normal gastric emptying. Furthermore, the symptoms reported by the patients during the GES test with the low fat Eggbeaters meal generally correlated with symptoms recorded by the patient’s recall of their symptoms using the PAGI-SYM.
The three symptoms that had the strongest relationship with delayed gastric emptying were stomach fullness, bloating, and abdominal pain. These symptoms peaked at one hour postprandially in patients with normal and delayed gastric emptying and at 30 min postprandially for RGES patients. However, symptoms of nausea, abdominal burning, and belching were found to have a different postprandial relationship with only a minimal nonsignificant increase postprandially. Few other studies have evaluated symptoms during gastric emptying and there have been fewer studies correlating symptoms present during the gastric emptying test to the result of the gastric emptying test. One study performed with octanoate breath testing for measuring gastric emptying found no significant correlation between meal related symptom scores and solid or liquid gastric emptying (20). Another study also using octanoate breath testing in patients with functional dyspepsia found a temporal relationship of symptoms during gastric emptying (21). The time-course of individual symptoms varied, with early peaks for fullness and bloating, intermediate peaks for nausea and belching, and late peaks for pain and burning. The time profile of individual symptoms might suggest different causes and might be of importance in the future when coordinating patient-specific pharmacologic intervention. The early onset of symptoms during the gastric emptying process seen in this study might be related to impaired fundal accommodation. Prior studies have suggested that the proximal rather than the distal stomach plays a major role in the pathogenesis of many upper GI symptoms (4). Regional gastric emptying can assess intragastric meal distribution and transit from the proximal to distal portions of the stomach and may provide greater information regarding fundal and antral function (22). Studies have shown an association between symptoms of nausea, early satiety, abdominal distention with proximal gastric retention; whereas vomiting is associated more with delayed distal gastric emptying (23,24). In functional dyspepsia, three pathophysiological factors have been suggested to play a role in symptom generation: impaired accommodation associated with early satiety; delayed gastric emptying associated with postprandial fullness, nausea, vomiting; and hypersensitivity to gastric distension associated with epigastric pain (25).
This study demonstrates a good correlation between real time symptoms recorded during GES and the PAGI-SYM for which the patient grades their symptoms over the prior two weeks. The results appear to support the low-fat egg white meal (e.g., Eggbeaters meal) as an appropriate provocative meal to induce postprandial symptoms (12). This is interesting as it is relatively low fat meal (13). Interestingly, patients with DGES had a higher correlation of the SSI during the GES compared to the PAGY-SYM quantitating symptoms over two weeks prior to the GES. The PAGI-SYM, which includes the nine symptoms of the Gastroparesis Cardinal Symptom Index (GCSI; 18,19), was developed as a questionnaire to assess symptoms of gastroparesis, functional dyspepsia, and gastroesophageal reflux (16,17,18,19). The higher correlation in DGES might also be due to a larger range of symptom scores in patients with delayed gastric emptying. A recent study suggests that the PAGI-SYM scores are mainly correlated with gastric emptying rate and with gastric hypersensitivity (26) and suggested that the PAGI-SYM questionnaire may be useful in the evaluation of gastroprokinetic agents.
This study compared the symptoms of diabetic gastroparesis and idiopathic gastroparesis analyzing symptoms during the gastric emptying test. The data show that stomach fullness was the most severe symptom in both diabetic and idiopathic gastroparesis. This symptom was rated as more severe in patients with idiopathic gastroparesis than patients with diabetic gastroparesis at 0, 30 min, and 3 hrs postprandial. Patients with idiopathic gastroparesis had a significant increase in abdominal pain during the GES with Eggbeaters meal. In contrast, abdominal pain did not significantly increase in patients with diabetic gastroparesis. One shortcoming of this study is that the glucose levels were not assessed during the gastric emptying test. Hyperglycemia is known to slow gastric emptying and might impact symptom production (13).
In summary, this study has looked carefully at symptoms of patients with delayed gastric emptying. Overall symptom severity recorded during GES was higher in DGES than NGES patients. In addition, the individual symptoms of stomach fullness, bloating, and abdominal pain were higher in DGES than in NGES. Furthermore, there is good correlation between symptoms recorded during GES and the PAGI-SYM-symptoms recorded for the 2 weeks prior to GES.
Supplementary Material
Acknowledgments
This study was supported in part by a NIH Midcareer Investigator Award in Patient-Oriented Research to HP Parkman (NIH DK02921).
Footnotes
Preliminary results presented at the 2009 Digestive Disease Week in Chicago, Illinois
REFERENCES
- 1.Parkman HP, Hasler WL, Fisher RS. American Gastroenterological Association Technical Review on the Diagnosis and treatment of Gastroparesis. Prepared by the American Gastroenterological Association Clinical Practice Committee. Gastroenterology. 2004;127:1592–1622. doi: 10.1053/j.gastro.2004.09.055. [DOI] [PubMed] [Google Scholar]
- 2.AMS Gastroparesis Task Force. Abell TL, Bernstein RK, Cutts T, Farrugia G, Forster J, Hasler WL, McCallum RW, Olden KW, Parkman HP, Parrish CR, Pasricha PJ, Prather CM, Soffer EE, Twillman R, Vinik AI. Treatment of Gastroparesis: A Multidisciplinary Review. Neurogastroenterology and Motility. 2006;18(4):263–283. doi: 10.1111/j.1365-2982.2006.00760.x. [DOI] [PubMed] [Google Scholar]
- 3.Waseem W. Gastroparesis: Current diagnostic challenges and management considerations. World J Gastroenterol. 2009 Jan 7;15(1):25–37. doi: 10.3748/wjg.15.25. ISSN 1007-9327 CN 14-1219/R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tack J, Arts J, Caenepeel P, Karamanolis G. Determinants of symptom pattern in idiopathic severely delayed gastric emptying: gastric emptying rate or proximal stomach dysfunction? Gut. 2007;56:29–36. doi: 10.1136/gut.2005.089508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stanghellini V, Tosetti C, Paternico A, Barbara G, Morselli-Labate AM, Monetti N, Marengo M, Corinaldesi R. Risk indicators of delayed gastric emptying of solids in patients with functional dyspepsia. Gastroenterology. 1996;110:1036–1042. doi: 10.1053/gast.1996.v110.pm8612991. [DOI] [PubMed] [Google Scholar]
- 6.Sarnelli G, Caenepeel P, Geypens B, Janssens J, Tack J. Symptoms associated with impaired gastric emptying of solids and liquids in functional dyspepsia. Am J Gastroenterol. 2003;98(4):783–788. doi: 10.1111/j.1572-0241.2003.07389.x. [DOI] [PubMed] [Google Scholar]
- 7.Cassilly DW, Wang YW, Friedenberg FK, Nelson DB, Maurer AH, Parkman HP. Symptoms of gastroparesis. Use of the Gastroparesis Cardinal Symptom Index in patients referred for gastric emptying scintigraphy. Digestion. 2008;78:144–151. doi: 10.1159/000175836. [DOI] [PubMed] [Google Scholar]
- 8.Delgado-Aros S, Camilleri M, Cremonini F, Ferber I, Stephens D, Burton DD. Contributions of gastric volumes and gastric emptying to meal size and postmeal symptoms in functional dyspepsia. Gastroenterology. 2004;127(6):1685–1694. doi: 10.1053/j.gastro.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 9.Jones KL, Wishart JM, Russo A, Berry MK, Stevens JE, Horowitz M. Predictors of delayed gastric emptying in diabetes. Diabetes Care. 2001;24:1264–1269. doi: 10.2337/diacare.24.7.1264. [DOI] [PubMed] [Google Scholar]
- 10.Samsom M, Vermeijden JR, Smout AJ, et al. Prevalence of delayed gastric emptying in diabetic patients and relationship to dyspeptic symptoms: a prospective study in unselected diabetic patients. Diab Care. 2003;26:3116–3122. doi: 10.2337/diacare.26.11.3116. [DOI] [PubMed] [Google Scholar]
- 11.Horowitz M, Harding PE, Maddox AF, Wishart JM, Akkermans LM, Chatterton BE, Shearman DJ. Gastric and oesophageal emptying in patients with type 2 (non-insulin-dependent) diabetes mellitus. Diabetologia. 1989;32:151–159. doi: 10.1007/BF00265086. [DOI] [PubMed] [Google Scholar]
- 12.Horowitz M, Harding PE, Maddox AF, Maddern GJ, Collings PH, Chatterton BE, Wishart J, Shearman DJC. Gastric and oesophageal emptying in insulin-dependent diabetes mellitus. J Gastroenterol Hepatol. 1986;1:97–113. [Google Scholar]
- 13.Abell TL, Camilleri M, Donohoe K, Hasler WL, MD, Lin HC, MD, McCallum RW, Nowak T, Nusynowitz ML, Parkman HP, Shreve P, Szarka LA, Snape WJ, Jr, Ziessman HA. Consensus Recommendations for Gastric Emptying Scintigraphy. A Joint Report of the Society of Nuclear Medicine and The American Neurogastroenterology and Motility Society. Am J Gastroenterology. 2008;103:753–763. doi: 10.1111/j.1572-0241.2007.01636.x. [DOI] [PubMed] [Google Scholar]
- 14.Tougas G, Eaker EY, Abell TL, et al. Assessment of gastric emptying using a low-fat meal: Establishment of international control values. Am J Gastroenterol. 2000;95:1456–1462. doi: 10.1111/j.1572-0241.2000.02076.x. [DOI] [PubMed] [Google Scholar]
- 15.Guo J-P, Maurer AH, Urbain J-L, Fisher RS, Parkman HP. Extending gastric emptying scintigraphy from two to four hours detects more patients with gastroparesis. Digestive Diseases Sciences. 2001;46:24–29. doi: 10.1023/a:1005697422454. [DOI] [PubMed] [Google Scholar]
- 16.Rentz AM, Kahrilas P, Stanghellini V, et al. Development and psychometric evaluation of the patient assessment of upper gastrointestinal symptom severity index (PAGI-SYM) in patients with upper gastrointestinal disorders. Qual Life Res. 2004;13(10):1737–1749. doi: 10.1007/s11136-004-9567-x. [DOI] [PubMed] [Google Scholar]
- 17.Revicki DA, et al. Responsiveness and interpretation of a symptom severity index specific to upper gastrointestinal disorders. Clinical Gastroenterology and Hepatology. 2004;2:769–777. doi: 10.1016/s1542-3565(04)00348-9. [DOI] [PubMed] [Google Scholar]
- 18.Revicki DA, Rentz AM, Dubois D, Kahrilas P, Stanghellini V, Talley NJ, Tack J. Development and validation of a patient-assessed gastroparesis symptoms severity measure: the Gastroparesis Cardinal Symptom Index. Aliment Pharmacol Ther. 2003;18:141–150. doi: 10.1046/j.1365-2036.2003.01612.x. [DOI] [PubMed] [Google Scholar]
- 19.Revicki DA, Rentz AM, Dubois D, Kahrilas P, Stanghellini V, Talley NJ, Tack J. Gastroparesis Cardinal Symptom Index (GCSI): Development and validation of a patient reported assessment of severity of gastroparesis symptoms. Qual Life Res. 2004;13(4):833–844. doi: 10.1023/B:QURE.0000021689.86296.e4. [DOI] [PubMed] [Google Scholar]
- 20.Arts J, Caenepeel P, Verbeke K, Tack J. Influence of erythromycin on gastric emptying and meal related symptoms in functional dyspepsia with delayed gastric emptying. Gut. 2005;54:455–460. doi: 10.1136/gut.2003.035279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bisschops R, Karamanolis G, Arts J, Caenepeel P, Verbeke K, Janssens J, Tack J. Relationship between symptoms and ingestion of a meal in functional dyspepsia. Gut. 2008;57(11):1495–1503. doi: 10.1136/gut.2007.137125. [DOI] [PubMed] [Google Scholar]
- 22.Troncon LE, Bennett RJ, Ahluwalia NK, Thompson DG. Abnormal intragastric distribution of food during gastric emptying in functional dyspepsia patients. Gut. 1994;35:327–332. doi: 10.1136/gut.35.3.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gonlachanvit S, Maurer AH, Fisher RS, Parkman HP. Regional Gastric Emptying Abnormalities in Functional Dyspepsia and Gastroesophageal Reflux Disease. Neurogastroenterology and Motility. 2006;18(10):894–904. doi: 10.1111/j.1365-2982.2006.00811.x. [DOI] [PubMed] [Google Scholar]
- 24.Piessevaux H, Tack J, Wairand S, Pauwels S, Geubel A. Intragastric distribution of a standardized meal in health and functional dyspepsia: correlation with specific symptoms. Neurogastroenterol Motil. 2003;15:447–455. doi: 10.1046/j.1365-2982.2003.00431.x. [DOI] [PubMed] [Google Scholar]
- 25.Tack J, Bisschops R, Sarnelli G. Pathophysiology and treatment of functional dyspepsia. Gastroenterology. 2004;127:1239–1255. doi: 10.1053/j.gastro.2004.05.030. [DOI] [PubMed] [Google Scholar]
- 26.Kindt S, Dubois D, van Oudenhove L, Caenepeel P, Arts J, Bisschops R, Tack J. Relationship between symptom pattern, assessed by the PAGI-SYM questionnaire, and gastric sensorimotor dysfunction in functional dyspepsia. Neurogastroenterol Motil. 2009 Aug 4; doi: 10.1111/j.1365-2982.2009.01374.x. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


