Abstract
The ADVANCE (Accelerating Data Value Across a National Community Health Center Network) clinical data research network (CDRN) is led by the OCHIN Community Health Information Network in partnership with Health Choice Network and Fenway Health. The ADVANCE CDRN will ‘horizontally’ integrate outpatient electronic health record data for over one million federally qualified health center patients, and ‘vertically’ integrate hospital, health plan, and community data for these patients, often under-represented in research studies. Patient investigators, community investigators, and academic investigators with diverse expertise will work together to meet project goals related to data integration, patient engagement and recruitment, and the development of streamlined regulatory policies. By enhancing the data and research infrastructure of participating organizations, the ADVANCE CDRN will serve as a ‘community laboratory’ for including disadvantaged and vulnerable patients in patient-centered outcomes research that is aligned with the priorities of patients, clinics, and communities in our network.
Keywords: Patient Centered Clinical Research Network, Health Information Technology, Federally Qualified Health Centers, Addressing Disparities, Comparative Effectiveness Research, Patient Centered Outcomes Research
Introduction
ADVANCE (Accelerating Data Value Across a National Community Health Center Network) is led by the OCHIN Community Health Information Network in partnership with the Health Choice Network (HCN) and Fenway Health. Funded by the Patient Center Outcomes Research Institute as a clinical data research network (CDRN) of PCORnet (award number CDRN-1306-04716), ADVANCE is a unique ‘community laboratory’ for conducting patient-centered outcomes research with populations generally under-represented in clinical trials. This article describes our community-based CDRN, its significant stakeholder engagement, nimble yet robust infrastructure, and the opportunities it provides for partnership with us.
A safety net clinical data research network
ADVANCE aims to significantly enhance the heterogeneity and representativeness of populations included in research. Led by OCHIN's research team and Practice-Based Research Network,1 2 ADVANCE will include groups of patients receiving care in community health centers and federally qualified health center (FQHC) in the OCHIN network, HCN, and Fenway Health. The health systems in the ADVANCE CDRN serve disadvantaged and vulnerable populations; for example, over half of our patients earn less than the federal poverty level, 36% are Hispanic, and 15% are African American. In the past, FQHC patients have been under-represented in clinical trials owing, in part, to a lack of access as well as distrust in traditional research institutions.3 ADVANCE is designed to work in direct partnership with FQHCs, which reflect the social, cultural, and linguistic characteristics of their communities and have developed trusting, long-term relationships.
Horizontal and vertical data integration
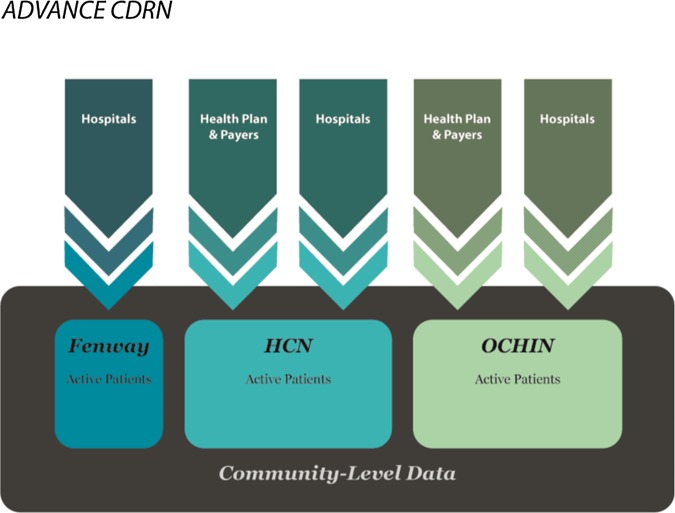
ADVANCE will build a national ‘community laboratory’ of FQHCs by bringing together longitudinal electronic outpatient clinical data for over one million FQHC patients, and integrate hospital and community-level data for this population. We describe our aggregation processes as both horizontal and vertical data integration. First, there is the horizontal integration of all the outpatient electronic health records (EHRs) across the three health systems (OCHIN, HCN, and Fenway); second, data from this same population of patients are enhanced by a vertical integration of their outpatient data with hospital, health plan, and community data (figure 1).
Figure 1.
Horizontal and vertical integration of data in the ADVANCE clinical data research network.
Working in four phases over 18 months, ADVANCE will develop the capacity to integrate and share data from all ADVANCE partners as well as across the national PCORnet network. Central to these efforts will be the Acuere Quality of Life (often shortened to AcuereQOL or Acuere) data aggregation system, developed by OCHIN and HCN. First, ADVANCE will integrate longitudinal outpatient EHR data from OCHIN, HCN, and Fenway Health into the Acuere warehouse. Second, we will develop and test a plan for aggregating hospital data (ie, inpatient, emergency department) for this same population. Third, we will develop systems for incorporating important social determinants of health, community data (eg, neighborhood vital statistics, census data), and patient-reported outcomes (eg, personal health records, education, occupation). Finally, we will develop and implement a plan to make these data available in the national PCORnet common data model.
Engaging patient, community, and academic investigators in research
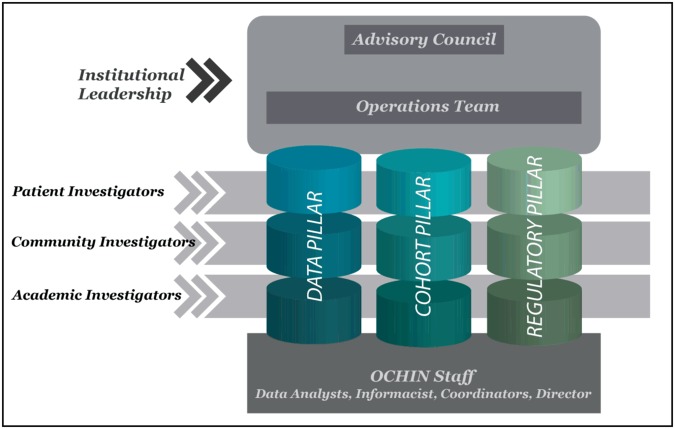
ADVANCE will involve multiple stakeholders with diverse expertise helping to build the CDRN infrastructure, focusing on three project ‘pillars.’ The pillars are workgroups of patient investigators, community investigators, and academic investigators collaborating to meet project goals (figure 2).
Data pillar: This pillar will develop and implement plans to normalize, validate, and expand our clinical data repository. As described above, data teams will create an integrated horizontal database of outpatient data from FQHC patients in 22 states, into which we will vertically integrate data from hospitals and health plans that serve the same population. We will also incorporate neighborhood-level data from the communities in which these patients live and patient-reported data.
Cohort pillar: This pillar will develop and implement approaches for collecting patient-reported data that can be integrated into the clinical record; these patient-centered systems will be designed to support the engagement of patients in their care as well as in all aspects of research, including identifying and recruiting cohorts of patients interested in participating in future PCORnet studies.
Regulatory pillar: Building on OCHIN's existing policies, and working closely with our compliance officer and data stewardship committee, this pillar will streamline our existing policies for data security, privacy, and confidentiality, identify one central institutional review board (IRB) for our CDRN, and develop a system for assisting FQHCs with obtaining a Federal-Wide Assurance that designates oversight to that IRB.
Figure 2.
ADVANCE clinical data research network organizational chart. ADVANCE, Accelerating Data Value Across a National Community Health Center Network; HCN, Health Choice Network; OCHIN, Oregon Community Health Information Network.
The data, cohort, and regulatory pillar workgroups coordinate efforts, with oversight by the ADVANCE Advisory Council. Each workgroup has dedicated members serving on PCORnet task forces and liaising with the national coordinating center to ensure ADVANCE activities are well coordinated and synergistic with national efforts, and that PCORnet is able to include vulnerable and diverse FQHC patient populations in all aspects of patient-centered outcomes research.
Advance partners: OCHIN, HCN, and Fenway
OCHIN was originally called the Oregon Community Health Information Network and shortened its name to ‘OCHIN’ as the network expanded into numerous states. The OCHIN collaborative began as a health center-controlled network in 2001 when five Oregon FQHCs, partnering with CareOregon (the state's largest Medicaid managed care organization), obtained federal funding to build an organization that would provide health information technology and related support to FQHCs in Oregon. These FQHCs and others like them across the USA have a core mission to serve uninsured and indigent patient populations in need of primary care services. These clinics individually could not afford to implement an EHR system, but together they were able to obtain and share the Epic practice management and ambulatory EHR system. By 2013, OCHIN's community health network had expanded to include 64 FQHC systems and other community-based primary care organizations in 13 states, with eight additional FQHC systems in five more states preparing to ‘go live’ on the EHR in 2014.4 OCHIN is now the nation's largest FQHC network using a single-enterprise EHR system (and the only one with Epic, which is used in more than one-third of hospitals nationwide).
Pioneering the implementation of a single, hosted instance of the Epic EHR across multiple ambulatory care clinics, OCHIN maintains one enterprise-wide master patient index. Thus, OCHIN patients have a single medical record across all clinics in the network, and all data are managed centrally. OCHIN also developed some of the first EHR-based decision support functions for FQHCs, and has tailored other health IT tools to meet their specific needs. OCHIN provides its member clinics with interfaces that supplement the EHR with external information (eg, laboratory data, images); secure data interchange with state and federal agencies (eg, Social Security Administration for disability determination, ‘real-time’ influenza surveillance); and an electronic data warehouse that supports reporting, data analytics, and diverse research efforts. OCHIN recently helped over 3600 healthcare providers attest to the first stage of federal ‘meaningful use’ requirements for EHRs, serving as the federally designated regional extension center for Oregon.5 OCHIN leveraged these unique resources to develop a research-ready data infrastructure containing aggregated, longitudinal clinical data going back to 2002.2 OCHIN's Practice Based Research Network was created in 2005 and is registered with the Agency for Healthcare Research and Quality.1 2 4 Since then, OCHIN has led, or been a partner on, numerous federally funded research projects.1 2 4 6–29
HCN is a health center-controlled network with a history and organizational structure similar to that of OCHIN. In 1994, HCN was founded in Florida by a group of FQHCs collaborating to recover from hurricane Andrew. It now has members in 11 states. HCN members are hosted on a centralized EHR platform (Intergy by Vitera), and supported by network-wide clinical informatics and analytic tools customized to improve the quality of service delivery in FQHCs. HCN has also implemented centralized systems for dental and behavioral health EHRs. HCN staff includes professionals with specialized expertise in project management, software customization, network operations, clinical informatics, customer support, quality improvement, and research. HCN's community board of directors includes several committees seeking to ensure broad input from member FQHCs’ operational, clinical, and health IT staff, and thus promote collaborative decision-making and dissemination of network-wide best practices. In 2011, HCN partnered OCHIN to form THQLink (Connecting Technology, Health, and Quality). This partnership provides consulting and health IT tools to help FQHCs integrate technology into their practices, achieve EHR ‘meaningful use,’ and attain a formal designation as a patient-centered medical home.
Fenway Health, a free-standing FQHC, was founded in 1971. In its early community-based response to the AIDS epidemic, Fenway Health developed the ability to support clinical research, and has since received significant funding from the National Institutes of Health.30 Fenway has expertise in providing culturally competent services for sexual and gender minority populations, and is the home of the National Center for Lesbian, Gay, Bisexual and Transgender Health Education.31 Fenway's staff of over 350 includes about 100 who conduct research, education, and information dissemination through The Fenway Institute.32 Fenway Health has had an EHR for over 15 years (Centricity) and has participated in several national research consortia using EHR-based data. Fenway is New England's only member of the Center for AIDS Research Network of Clinical Information Systems.33
ADVANCE Acuere quality-of-life data warehouse
ADVANCE builds on the collective abilities of OCHIN and HCN to aggregate and use clinical data from different EHRs as well as many other types of data to inform improvements in care. As health center-controlled networks, a model supported by the US Health Resources and Services Administration to support cross-clinic sharing of EHR systems and data, both OCHIN and HCN are non-profit 501(c)(3) member-based organizations that share similar governance structures and involve stakeholders in decision-making on their health IT systems. Over the past 10 years, OCHIN and HCN have developed the technical and personnel infrastructures required to access comprehensive EHR outpatient clinical and financial data from all FQHCs in their respective networks and advanced the use of these data to inform health IT system optimizations for enhancing care for safety net populations, improving patient outcomes, increasing clinic and provider productivity, and reducing provider burden.
Central to ADVANCE will be the use of the Acuere data aggregation and analytics system developed by OCHIN and HCN. Acuere was developed to enable FQHC providers to participate in the analytics required to improve processes, performance, and patient care. The Acuere system was built on the Caradigm Intelligence Platform, and was developed by OCHIN and HCN for the unique needs of their FQHC networks. Caradigm Intelligence Platform, a joint GE Healthcare and Microsoft software solution, is a cloud-based analytics and population health system for aggregating and normalizing data from multiple sources.
Acuere will aggregate data from the three partner EHR systems (Epic, Centricity, and Intergy) using the Health Level Seven International's (HL7) standard (a unifying communications protocol providing a framework for near ‘real-time’ exchange, integration, sharing, and retrieval of the electronic health information required to support clinical practice, and health services management and evaluation). This standard enables the seamless exchange of the Continuity of Care Document (CCD), a universal protocol standard designed to specify the encoding, structure, and semantics of a patient summary clinical document for exchange purposes.34 The CCD contains a core dataset that includes relevant administrative, demographic, and clinical information. It also provides a standard protocol that allows one healthcare practitioner, system, or setting to aggregate all pertinent data about a patient and forward it to any other practitioner, system, or setting, as a ‘snapshot’ of all pertinent patient data.35 Patients are also de-duplicated using the Acuere Master Patient Index so that reports, analyses, and research on distinct cohorts of patients are possible.
To supplement the information contained in the CCD snapshot, OCHIN and HCN developed a combination strategy that depends on the capability of the EHR being used. This strategy may include a robust extract, transform, load (ETL) that involves extracting data from outside sources, transforming it to fit operational needs, and loading it into the end target database. It may also include discrete HL7 interfaces of a direct ingestion of data from the EHR core database. Because data warehouses are typically assembled from a variety of sources with different formats, protocols, and purposes, these processes will enable the ADVANCE data warehouse team to combine these data in a standardized, homogeneous environment. Using these CCD and ETL strategies will ensure that all additional information is acquired and configured into a robust data warehouse designed to support mapping data to real-world entities. Acuere is designed to support research as well as many other health center priorities aiming to improve care delivery and patient health outcomes (eg, clinical care, panel management, chronic disease management, patient engagement, and improvement initiatives).
Interfaces and procedures
Integrating data from many clinics, hospitals, health plans, and community data sources into the ADVANCE CDRN warehouse will require multiple interfaces to laboratories, hospitals, health information exchanges, etc. OCHIN and HCN currently support over 400 real-time interfaces, with an average of 400 000 unique messages a day across multiple laboratories, hospitals, and community exchanges. Within its Epic system alone, OCHIN processes more than 100 000 documents (eg, CCDs, lab interfaces, etc) a week. OCHIN and HCN built health IT systems to maintain and operate these complex exchange solutions and contribute directly to supporting care delivery to safety net patients.
The ADVANCE CDRN will enable OCHIN and HCN's technical, clinical, and data teams to build collaboratively on this expertise and capacity, and to oversee the ingestion of information from multiple EHRs and other community information systems into a single, structured database. By improving and accelerating such data exchange and warehousing capabilities, ADVANCE will facilitate the aggregation of data from multiple FQHC health systems and hospitals on different EHR platforms. This level of connectivity in FQHC settings will directly support ADVANCE efforts to develop patient-centered outcomes research capacity in the safety net.
Summary
The ADVANCE CDRN includes FQHCs in 22 states. As demand for FQHC services continues to grow, so will the ADVANCE CDRN population. The increased data collection and integration supported by ADVANCE will facilitate richer, more impactful patient-centered outcomes research that involves this growing population.36–42 Increasing numbers of FQHCs are implementing quality improvement and research as an integral part of care delivery. ADVANCE is committed to supporting these innovation efforts in FQHCs across the country and ensuring that patient-centered outcomes research is aligned with the priorities of patients, clinics, and communities in our network, and that future patient-centered outcomes research includes FQHC patients and other previously under-represented populations.
Acknowledgments
We would like to acknowledge the federally qualified health center providers and patients for their time and insight that have shaped this work and the efforts of many others who helped to prepare this manuscript, including Heather Angier, Jill Arkind, Melissa Laurie, and Diana Wolford.
Footnotes
Funding: This work was financially supported by the Patient Center Outcomes Research Institute (PCORI) grant number CDRN-1306–04716.
Competing interests: None.
Provenance and peer review: Commissioned; internally peer reviewed.
References
- 1.DeVoe JE, Gold R, Spofford M, et al. Developing a network of community health centers with a common electronic health record: description of the Safety Net West Practice-based Research Network (SNW-Pratice Based Research Network). J Am Board Fam Med 2011;24:597–604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DeVoe JE, Likumahuwa S, Eiff MP, et al. Developing a new Pratice Based Research Network: lessons learned and challenges ahead [Commentary]. J Am Board Fam Med 2012;25:560–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: race-, sex-, and age-based disparities. JAMA 2004;291:2720–6 [DOI] [PubMed] [Google Scholar]
- 4.DeVoe JE, Sears A. The OCHIN Community Information Network: bringing together community health centers, information technology and data to support a patient-centered medical village. J Am Board Fam Med 2013;26:271–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.HealthIT.gov. Regional Extension Centers (RECs) 2013. [cited 2013 September 20]. http://www.healthIT.gov/providers-professionals/rec-highlights
- 6.DeVoe JE, Tillotson CJ, Lesko SE, et al. The case for synergy between a usual source of care and health insurance coverage. J Gen Intern Med 2011;26:1059–66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.DeVoe JE, Ray M, Graham A. Public health insurance in Oregon: underenrollment of eligible children and parental confusion about children's enrollment status. Am J Public Health 2011;101:891–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Angier H, Wiggins N, Gregg J, et al. Increasing the relevance of research to underserved communities: lessons learned from a retreat to engage community health workers with researchers. J Health Care Poor Underserved 2013;24:840–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Devoe JE, Gold R. Community of solution for the U.S. health care system: lessons from the U.S. educational system. J Am Board Fam Med 2013;26:323–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Likumahuwa S, Song H, Singal R, et al. Building Research Infrastructure in Community Health Centers: a Community Health Applied Research Network (CHARN) Report. J Am Board Fam Med 2013;26:579–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Devoe JE, Tillotson CJ, Angier H, et al. Recent health insurance trends for US families: children gain while parents lose. Matern Child Health J 2014;18:1007–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Angier H, DeVoe JE, Tillotson C, et al. Changes in health insurance for US children and their parents: comparing 2003 to 2008. Fam Med 2013;45:26–32 [PMC free article] [PubMed] [Google Scholar]
- 13.Gold R, Muench J, Hill C, et al. Collaborative development of a randomized study to adapt a diabetes quality improvement initiative for federally qualified health centers. J Health Care Poor Underserved 2012;23(Suppl 3):236–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Casciato A, Angier H, Milano C, et al. Are pediatric quality care measures too stringent? J Am Board Fam Med 2012;25:686–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Angier H, Devoe JE, Tillotson C, et al. Trends in health insurance status of US children and their parents, 1998–2008. Matern Child Health J 2012;17:1550–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DeVoe JE, Likumahuwa S, Eiff MP, et al. Lessons learned and challenges ahead: report from the OCHIN Safety Net West practice-based research network (Pratice Based Research Network). J Am Board Fam Med 2012;25:560–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Devoe JE, Tillotson CJ, Wallace LS, et al. The effects of health insurance and a usual source of care on a child's receipt of health care. J Pediatr Health Care 2012;26:e25–35 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gold R, Angier H, Mangione-Smith R, et al. Feasibility of evaluating the CHIPRA care quality measures in electronic health record data. Pediatrics 2012;130:139–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gold R, DeVoe JE, McIntire PJ, et al. Receipt of diabetes preventive care among safety net patients associated with differing levels of insurance coverage. J Am Board Fam Med 2012;25:42–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.DeVoe JE, Tillotson CJ, Wallace LS, et al. Is health insurance enough? A usual source of care may be more important to ensure a child receives preventive health counseling. Matern Child Health J 2012;16:306–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Davis MM, Keller S, DeVoe JE, et al. Characteristics and lessons learned from Practice-based Research Networks (Pratice Based Research Networks) in the United States. J Health Care Leadersh 2012;4:107–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.DeVoe JE, Tillotson CJ, Wallace LS, et al. Parent and child usual source of care and children's receipt of health care services. Ann Fam Med 2011;9:504–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Devoe JE, Gold R, McIntire P, et al. Electronic health records vs Medicaid claims: completeness of diabetes preventive care data in community health centers. Ann Fam Med 2011;9:351–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.DeVoe JE, Tillotson CJ, Wallace LS, et al. Comparing types of health insurance for children: a public option versus a private option. Med Care 2011;49:818–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hazelhurst B, McBurnie MA, Mularski RA, et al. Automating care quality measurement with health information technology. Am J Manag Care 2012;18:313–9 [PubMed] [Google Scholar]
- 26.Hazelhurst B, Stevens V, McBurnie MA, et al. Development of a measure set for routine, comprehensive, automated assessment of obesity care quality. Clin Med Res 2011;9:161 [Google Scholar]
- 27.Gold R.2007. The Guide to Conducting Research in the OCHIN Practice Management Data.
- 28.Gold R, DeVoe J, Shah A, et al. Insurance continuity and receipt of diabetes preventive care in a network of federally qualified health centers. Med Care 2009;47:431–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yamauchi M, Carlson MJ, Wright BJ, et al. Does health insurance continuity among low-income adults impact their children's insurance coverage? Matern Child Health J 2013;17:248–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mayer K, Appelbaum J, Rogers T, et al. The evolution of the Fenway Community Health model. Am J Public Health 2001;91:892–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.The Fenway Institute. The National LGBT Health Education Center. Boston, MA, 2013. [cited 2013 September 20]. http://www.LGBThealtheducation.org [Google Scholar]
- 32.The Fenway Institute. The Fenway Institute. Boston, MA, 2013. [cited 2013 September 20]. http://www.thefenwayinstitute.org [Google Scholar]
- 33.CFAR Network of Integrated Clinical Systems. The CNICS Research Network. Birmingham, AL, 2013. [cited 2013 September 20]. http://www.uab.edu/cnics/ [Google Scholar]
- 34.ANSI. Implementation Guide for CDA R2 health IT SP C32, C83, and C80 Summary Documents. Model-Driven Health Tools (MDHT) for CDA. In: The Office of the National Coordinator for Health Information Technology, editor 2010
- 35.Department of Health and Human Services. Health Information Technology: standards, implementation specifications, and certification criteria for electronic health record technology. Fed Regist 2012;77:13832–85 [PubMed] [Google Scholar]
- 36.Ku L, Jones E, Shin P, et al. Safety-net providers after health care reform: lessons from Massachusetts. Arch Intern Med 2011;171:1379–84 [DOI] [PubMed] [Google Scholar]
- 37.Ku L, Jones K, Shin P, et al. The states’ next challenge--securing primary care for expanded Medicaid populations. N Engl J Med 2011;364:493–5 [DOI] [PubMed] [Google Scholar]
- 38.Morgan D. U.S health centers for poor, uninsured see ranks swell Reuters, 2012 [Google Scholar]
- 39.Decker S, Kostova D, Kenney G, et al. Health status, risk factors, and medical conditions among persons enrolled in Medicaid vs uninsured low-income adults potentially eligible for Medicaid under the Affordable Care Act. JAMA 2013;309:2579–86 [DOI] [PubMed] [Google Scholar]
- 40.Polsky D. How the newly insured use health services: a lesson for the U.S. from Medicare. Philadelphia, Pennsylvania, USA: University of Pennsylvania, 2011 [Google Scholar]
- 41.The White House. The Obama Administration and Community Health Centers Washington, DC, 2012. http://www.whitehouse.gov/sites/default/files/05-01 12_community_health_center_report.pdf (accessed 22 Apr 2014) [Google Scholar]
- 42.U.S. Department of Health & Human Services. Key Features of the Affordable Care Act by Year. Washington, DC, 2010. http://www.hhs.gov/healthcare/facts/timeline/timeline-text.html (accessed 22 Apr 2014) [Google Scholar]