Abstract
The Patient-Centered Outcomes Research Institute (PCORI) has launched PCORnet, a major initiative to support an effective, sustainable national research infrastructure that will advance the use of electronic health data in comparative effectiveness research (CER) and other types of research. In December 2013, PCORI's board of governors funded 11 clinical data research networks (CDRNs) and 18 patient-powered research networks (PPRNs) for a period of 18 months. CDRNs are based on the electronic health records and other electronic sources of very large populations receiving healthcare within integrated or networked delivery systems. PPRNs are built primarily by communities of motivated patients, forming partnerships with researchers. These patients intend to participate in clinical research, by generating questions, sharing data, volunteering for interventional trials, and interpreting and disseminating results. Rapidly building a new national resource to facilitate a large-scale, patient-centered CER is associated with a number of technical, regulatory, and organizational challenges, which are described here.
Keywords: comparative effectiveness research, distributed databases, patient-centered outcomes research institute, clinical data research networks, patient-powered research networks
Launching PCORnet, a national clinical research network
The potential of comparative effectiveness research (CER) for dealing with practical clinical questions, enhancing the quality and effectiveness of care, and personalizing evidence-based care, is clear.1 Yet CER strains the current clinical research paradigm because of its emphasis on assessing effectiveness in typical care delivery settings, its requirement for very large study populations to study effectiveness heterogeneity, and, often, its need for treatments to be allocated by randomization.
In July 2012, the Patient-Centered Outcomes Research Institute (PCORI) convened a national multi-stakeholder workshop to advance the use of electronic health data in CER.2 Building on research networks that include among others, the HMO Research Network, the Agency for Healthcare Research and Quality (AHRQ) American Recovery and Reinvestment Act (ARRA) investments in data networks, the US Centers for Disease Prevention and Control (CDC) Vaccine Safety Data Link, the Food and Drug Administration's (FDA) Mini-Sentinel, the National Institutes of Health (NIH) Health Care Systems Research Collaboratory, two components of a national research infrastructure emerged.3–8 These comprise clinical data research networks (CDRNs) based on the electronic health records and other electronic sources of very large populations receiving healthcare within integrated or networked delivery systems9 and patient-powered research networks (PPRNs) built by communities of motivated patients, forming partnerships with researchers.10 CDRN and PPRN brief communications included in this special focus issue provide further information about these networks.
In December 2013, PCORI's board of governors funded 11 CDRNs and 18 PPRNs for a period of 18 months starting in March 2014 that together form PCORnet (http://www.pcornet.org). Each CDRN is committed to building a large patient cohort with comprehensive, longitudinal electronic clinical data; developing policies for data standardization, shared governance, efficient use of clinical information for multicenter studies, stringent attention to data security and patient privacy, and robust, scalable centralized research support tools; and building the capacity to participate successfully in multi-network randomized trials and observational studies. Each CDRN is a collaboration of health systems that include among others academic health centers, community hospitals, health plans, inpatient and outpatient hospitals and providers, federally qualified health centers, veterans’ administration clinics, pediatric hospitals and providers, integrated delivery systems, private electronic health record companies, and a regional health information exchange (table 1).
Table 1.
Clinical data research networks
| Clinical Data Research Network (CDRN) name | Lead organization |
|---|---|
| Accelerating Data Value Across a National Community Health Center Network (ADVANCE) | Oregon Community Health Information Network |
| Chicago Area Patient Centered Outcomes Research Network (CAPriCORN) | The Chicago Community Trust |
| Great Plains Collaborative | University of Kansas Medical Center |
| Kaiser Permanente and Strategic Partners Patient Outcomes Research to Advance Learning (PORTAL) | Kaiser Foundation Research Institute |
| Louisiana CDRN | Louisiana Public Health Institute |
| Mid-South CDRN | Vanderbilt University |
| A National Pediatric Learning Health System (PEDSNet) | The Children's Hospital of Philadelphia |
| New York City clinical data research networks (NYC-CDRN) | Weill Medical College of Cornell University |
| Patient-oriented SCAlable National Network for Effectiveness Research (pSCANNER) | University of California, San Diego |
| A P2aTH Towards a Learning Health System in the Mid-Atlantic Region (P2aTH) | University of Pittsburgh |
| Scalable Collaborative Infrastructure for a Learning Healthcare System (SCILHS) | Harvard University |
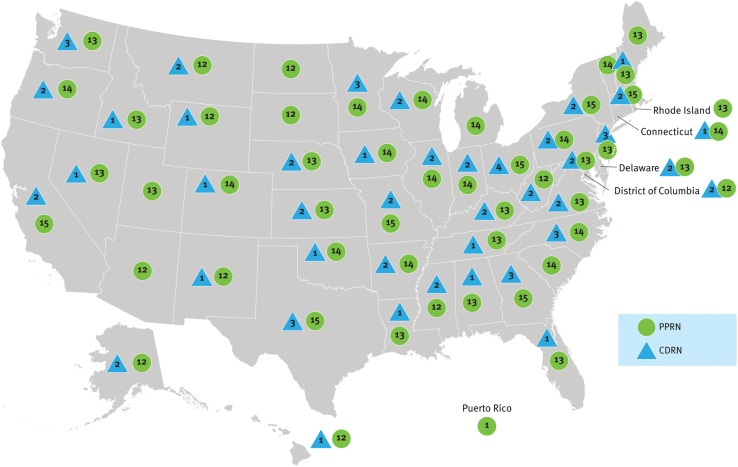
Each PPRN consists of patients, caregivers, or families, who are linked by the experience of a shared condition (table 2). An important commitment of these patient-based networks is to collect and curate data from at least 80% of their membership. The PPRNs are also expected to expand the number of patients in their network; to collect standardized patient data; and, when necessary, for the purposes of research, engage patients to participate in interventional research and in building, using, and governing their networks. The organizational set-up of PPRNs is diverse, as exemplified by the number of different partnership models that link patient foundations and associations with academic research centers. The CDRNs and PPRNs are geographically diverse, with patients in 50 states (figure 1).
Table 2.
Patient powered research networks
| Patient-Powered Research Network (PPRN) name | Condition |
|---|---|
| Adrenoleukodystrophy (ALD) Connect | ALD |
| American BRCA Outcomes and Utilization of Testing PPRN (ABOUT Network) | Hereditary breast and ovarian cancer |
| ARthritis patient Partnership With comparative Effectiveness Researchers (AR-PoWER PPRN) | Arthritis (rheumatoid arthritis, spondyloarthritis), musculoskeletal disorders (osteoporosis), and inflammatory conditions (psoriasis) |
| Chronic Obstructive Pulmonary Disease (COPD) Patient Powered Research Network | COPD |
| Collaborative Patient-Centered Rare Epilepsy Network (REN) | Aicardi syndrome, Lennox–Gastaut syndrome, Phelan–McDermid syndrome, hypothalamic hamartoma, Dravet syndrome, and tuberous sclerosis |
| Community-Engaged Network for All (CENA) | Alström syndrome, dyskeratosis congenita, Gaucher disease, hepatitis, inflammatory breast cancer, Joubert syndrome, Klinefelter syndrome and associated conditions, metachromatic leukodystrophy, Pseudoxanthoma elasticum (PXE), psoriasis |
| Crohn's and Colitis Foundation of America (CCFA) Partners PPRN | Inflammatory bowel disease (Crohn's disease and ulcerative colitis) |
| Duchenne Connect Patient-Report Registry Infrastructure Project | Duchenne and Becker muscular dystrophy |
| Health eheart alliance: a PPRN focused on cardiovascular health | Cardiovascular health |
| ImproveCareNow: a learning health system for children with Crohn's disease and ulcerative colitis | Pediatric Crohn's disease and ulcerative colitis |
| Mood PPRN | Major depressive disorder and bipolar disorder |
| A multiple sclerosis PPRN | Multiple sclerosis |
| NephCure Kidney Network for patients with nephrotic syndrome | Primary nephrotic syndrome (focal segmental glomerulosclerosis, minimal change disease, and membranous nephropathy) |
| The Patients, Advocates and Rheumatology Teams Network for Research and Service (PARTNERS) Consortium | Juvenile rheumatic disease |
| Phelan-McDermid Syndrome Data Network | Phelan–McDermid syndrome |
| Primary Immunodeficiency Patient Research Connection (PI-Connect) | Primary immunodeficiency diseases |
| Sleep Apnea-Patient Centered Outcomes Network (SA-PCON) | Sleep apnea |
| The Vasculitis Patient Powered Research Network | Vasculitis |
Figure 1.
Map of clinical data research networks (CDRN) and patient-powered research networks (PPRN) across the USA.
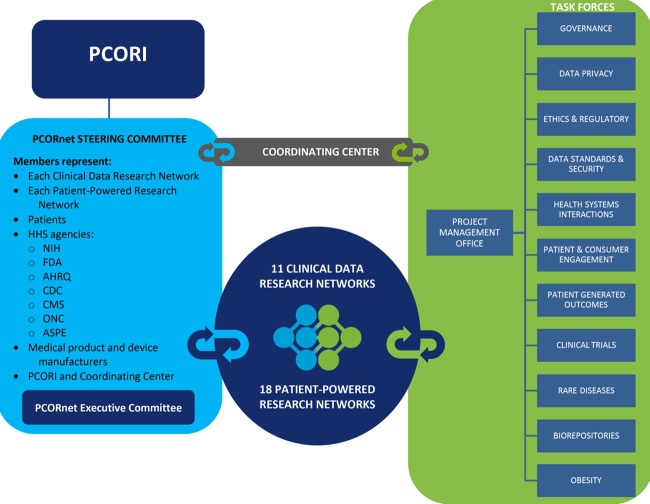
A coordinating center co-led by the Harvard Pilgrim Health Care Institute and Duke University (contract awarded in September 2013) provides technical and logistical expertise and assistance to awardees. It has established 11 task forces (figure 2), whose members are nominated from the CDRNs and PPRNs and whose role is to develop policies, operations, and products to support the development of PCORnet. A steering committee, subject to the oversight of PCORI, guides members of PCORnet and advises PCORI leadership (figure 2). Final approval of all policies, activities, and recommendations resides with the PCORI leadership.
Figure 2.
Organizational structure of PCORnet. AHRQ, Agency for Healthcare Research and Quality; ASPE, Assistant Secretary for Planning and Evaluation; CDC, US Centers for Disease Prevention and Control; CMS, Centers for Medicare and Medicaid Services; FDA, Food and Drug Administration; NIH, National Institutes of Health; ONC, Office of the National Coordinator for Health Information Technology; PCORI, Patient-Centered Outcomes Research Institute.
PCORnet distributed data research network
PCORnet is being developed as a distributed research network (DRN) that facilitates multi-site, observational and interventional research across the CDRNs, PPRNs, and other interested contributors, while minimizing the transfer of individual-level clinical data outside of the system where care is received. PCORnet's unique vision is to create a network that supports the CDRN and PPRN internal network development while creating a mechanism to facilitate research across these networks. Advantages of conducting research across multiple networks of PCORnet comprise greater sample size and power, the ability to study effects of practice pattern and treatment variation, the inclusion of diverse populations, and the possibility of supporting analyses that assess heterogeneity of treatment effect.
The distributed network will enable research studies to be conducted, while allowing each participating organization to maintain physical and operational control over their data. This structure lowers institutional barriers to participation and ensures availability of local experts who can interpret the data.11 12 The Data Standards, Security and Network Infrastructure (DSSNI) task force will identify minimal data standards and technical specifications for data standardization across CDRNs and PPRNs and develop an approach to cross-network querying that meets the security, patient privacy, institutional confidentiality, and governance needs of the network participants.13
The distributed querying approach allows simple and complex analyses to be executed behind institutional firewalls, thereby eliminating or minimizing the release of protected health information. Instead, only the minimum information needed to answer a specific question is transferred to the person making a request. Increasingly, even complex multi-site analyses can be accomplished without transfer of private health information by use of privacy preserving regression techniques.14 15
As part of their PCORnet participation, each CDRN will develop an analyzable research dataset (to be specified by the DSSNI task force) that supports complex distributed analyses. After 18 months, this dataset should contain data on one million patients and the CDRN will be able to regularly complete queries against the dataset using the secure PCORnet DRN tools. An example of the type of observational studies that might be supported by the DRN is a comparison of the outcomes of ischemic and hemorrhagic stroke in adults with atrial fibrillation who are new users of dabigatran or warfarin.16 The PCORnet DRN tools will be developed by input from the relevant task forces, including DSSNI, Governance, and Data Privacy during the first 18-month phase of funding (starting March 2014). The DSSNI task force will develop a PCORnet common data model (CDM) to support the development of analyzable research datasets that will permit efficient distributed analyses. The PPRNs aim in 18 months to have the ability to build a standardized clinical database with relevant clinical and patient-reported outcomes data from at least 80% of their membership. Overall, implementation of the PCORnet DRN networking and querying capabilities will prioritize rapid development, testing, use, and feedback learning cycles. This process will enable experimentation in networking approaches, demonstrate approaches to secure network operations, and identify potential barriers as early as possible.
PCORnet and patient-centeredness
Over the 18-month funding phase, each CDRN and PPRN will develop effective patient-engagement strategies at the level of their networks. These strategies will involve ensuring that patients have a central role in collecting data for the generation of new knowledge for patients with their condition, as well as in participating in the governance of the network, prioritizing research questions, and disseminating results.10 At the CDRN level, patient engagement strategies require developing approaches to inform patients who are members of the systems of the existence and function of the research network, to involve patients in generating research questions, and in including patients in the governance associated with the development and uses of the network.9
Challenges
Rapidly building a new national resource to facilitate large-scale, patient-centered CER will face a number of technical, regulatory, and organizational challenges.
Technical challenges, first, include successfully completing the capture of relevant longitudinal clinical data, a requirement for all CER studies. Since most electronic health record systems typically do not have information on care provided outside their health system, both CDRNs and PPRNs will need to explore approaches to dealing with this problem.17 Second, in order to achieve multi-institutional querying, PCORnet will have to deal with data harmonization.18 This will require understanding the context in which the data were collected, the various clinical and other terminologies in use, and changes in local systems and national standards (such as those associated with the Centers for Medicare and Medicaid's ‘meaningful use’ regulation) that affect the data. This should be done without requiring a change in the way the routine medical care data are collected, and will require data harmonization.19 20 PCORnet has chosen to develop a CDM, derived from the Mini-Sentinel CDM to enable efficient cross-networking querying.21 Third, the collection, harmonization, and use of a wide range of potential patient-reported data (eg, personal and family medical histories, use of remote monitoring devices, etc) for research is a nascent field,22 yet promises to empower patients to provide data that more fully describe their experience of, and preferences for, the treatment and management of their condition. In the absence of a standardized ontology or lexicon for a large number of these data elements, the ability to routinely include this information in analyzable research datasets will be explored in this first phase of PCORnet's development but will probably occur fully in later phases.
In addition to technical challenges, PCORnet will need to examine ethical and regulatory oversight. Many patients, advocates, and researchers describe the research oversight system as cumbersome, inefficient, and expensive.23–25 PCORnet will need to deal with problems associated with the design of appropriate clinical studies, informing prospective participants, and obtaining permissions in a manner that protects human rights while supporting the acknowledged need for more research to provide patients and clinical decision-makers with more reliable evidence.26 Areas of interest that PCORnet will explore through its task forces include central institutional review boards or internet-facilitated shared review systems, and, centralized support for enrolling subjects and obtaining their consent. Because of the scale and complexity of the types of research envisaged, PCORnet will be challenged to develop streamlined approaches to the structure and function of the network and its projects while maintaining sound ethics and regulatory compliance.
PCORnet will be faced with the organizational challenges associated with the rapid development of a national resource with a heterogeneous group of CDRNs and PPRNs of varying size, populations served, health systems included and many other characteristics. Although this diversity among awardees was both predictable and desirable, one area in which the diversity of networks was quickly apparent was the divergent approaches used for data management. Nevertheless, each CDRN and PPRN will be challenged with balancing the demands of their local networks, research cultures, and areas of particular expertise with the requirements of participating in a national research resource. This will require them to agree rapidly on a common approach to data interoperability and to the conduct of joint analyses.
PCORnet's success and long-term sustainability will also depend on communicating with health system leaders and providing them with evidence of the benefits of conducting high-quality, efficient research as part of the routine delivery of care. Securing the commitment of delivery systems’ leaders, health system administrators, and clinicians will require considerable strategy and effort by all PCORnet stakeholders. Finally, and importantly, PCORnet is committed to supporting patient engagement across the networks and will need to deal with the challenges of successfully supporting a variety of governance structures that fully ensure that patients are involved in setting policies for PCORnet and for their own networks, determining strategic direction, and prioritizing research questions.27
PCORnet will be open to external data partners, researchers, and funders
The PCORnet DRN will be open to external data and research affiliates willing to participate in research studies alongside the PCORI-funded CDRNs and PPRNs. Of particular note, PCORnet's distributed networking platform is shared by the FDA Mini-Sentinel program, the NIH Health Care Systems Research Collaboratory and other networks such as the HMO Research Network.3 6 7 Any organization that is part of these networks can make itself visible to the others and choose to receive queries from any of them. PCORI's vision is for the PCORnet DRN to be available for use by researchers not directly affiliated with PCORnet CDRNs and PPRNs through collaborative arrangements. The proposed governance models and mechanisms for these types of collaboration will be developed during the initial 18-month funding phase, which started in March 2014.
Conclusion
The first phase of building PCORnet will span 18 months. At the end of this time, we hope that a functional research network that can support both observational and interventional research will have emerged. We also expect a new model for efficiency and affordability in clinical research, made possible both by investments in, and use of, this evolving data infrastructure, and the involvement of host healthcare systems, clinicians, and patients together with researchers. Although PCORnet will need to continue to grow and improve its data resources and capabilities, a measure of success will be the willingness of external research funders, both public and private, to fund research studies using PCORnet.
Footnotes
Contributors: All authors have edited this manuscript and contributed portions of the text to its original version. RLF drafted the first version of the manuscript. LHC, RMC, RP, JVS, and JSB all edited and reviewed the manuscript. RLF is the guarantor of the manuscript.
Competing interests: RLF and JVS are employees of the Patient Centered Outcomes Research Institute and did not receive external support for this work. LHC, RMC, RP, and JSB are supported by the Patient-Centered Outcomes Research Center, contract No P12202013-499A for the PCORnet Coordinating Center.
Provenance and peer review: Commissioned; externally peer reviewed.
References
- 1.Institute of Medicine (U.S.). Committee on comparative effectiveness research prioritization. Initial national priorities for comparative effectiveness research. Washington, DC: National Academies Press, 2009 [Google Scholar]
- 2.PCORI. National workshop report: advancing the use of electronic data in patient-centered outcomes research. Washington, DC: PCORI, 2013 [Google Scholar]
- 3.Vogt TM, Elston-Lafata J, Tolsma D, et al. The role of research in integrated healthcare systems: the HMO Research Network. Am J Manag Care 2004;10:643–8 [PubMed] [Google Scholar]
- 4.EDM Forum. Building the Electronic Clinical Data Infrastructure to Improve Patient Outcomes: CER Project Profiles. Issue Briefs and Reports: Academy Health, 2012
- 5.Baggs J, Gee J, Lewis E, et al. The Vaccine Safety Datalink: a model for monitoring immunization safety. Pediatrics 2011;127(Suppl 1):S45–53 [DOI] [PubMed] [Google Scholar]
- 6.Behrman RE, Benner JS, Brown JS, et al. Developing the Sentinel System—a national resource for evidence development. N Engl J Med 2011;364:498–9 [DOI] [PubMed] [Google Scholar]
- 7.National Institutes of Health. NIH Health Care Systems Research Collaboratory. 2014. https://http://www.nihcollaboratory.org/Pages/default.aspx
- 8.Selby JV, Krumholz HM, Kuntz RE, et al. Network news: powering clinical research. Sci Transl Med 2013;5:182fs13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.The Patient Centered Outcomes Research Institute (PCORI). The national patient-centered clinical research network: Clinical Data Research Networks (CDRN)—phase one. Washington, DC: PCORI, 2013 [Google Scholar]
- 10.The Patient Centered Outcomes Research Institute (PCORI). The national patient-centered clinical research network: Patient-Powered Research Networks (PPRN)—phase one. Revised edn Washington, DC: PCORI, 2013 [Google Scholar]
- 11.Brown JS, Holmes JH, Shah K, et al. Distributed health data networks: a practical and preferred approach to multi-institutional evaluations of comparative effectiveness, safety, and quality of care. Med Care 2010;48(6 Suppl):S45–51 [DOI] [PubMed] [Google Scholar]
- 12.Curtis LH, Weiner MG, Boudreau DM, et al. Design considerations, architecture, and use of the Mini-Sentinel distributed data system. Pharmacoepidemiol Drug Saf 2012;21(Suppl 1):23–31 [DOI] [PubMed] [Google Scholar]
- 13.Brown J, Syat B, Lane K, et al. Blueprint for a distributed research network to conduct population studies and safety surveillance. Effective Health Care Research Report Rockville, MD: Agency for Healthcare Research and Quality (AHRQ), 2010 [Google Scholar]
- 14.Toh S, Gagne JJ, Rassen JA, et al. Confounding adjustment in comparative effectiveness research conducted within distributed research networks. Med Care 2013;51(8 Suppl 3):S4–10 [DOI] [PubMed] [Google Scholar]
- 15.Toh S, Reichman ME, Houstoun M, et al. Multivariable confounding adjustment in distributed data networks without sharing of patient-level data. Pharmacoepidemiol Drug Saf 2013;22:1171–7 [DOI] [PubMed] [Google Scholar]
- 16.Go AS, Singer D, Cheetham TC, et al. A protocol for assessment of Dabigatran: Mini-Sentinal (US Food and Drug Administration), 2013
- 17.Hersh WR, Weiner MG, Embi PJ, et al. Caveats for the use of operational electronic health record data in comparative effectiveness research. Med Care 2013; 51(8 Suppl 3):S30–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ogunyemi OI, Meeker D, Kim HE, et al. Identifying appropriate reference data models for comparative effectiveness research (CER) studies based on data from clinical information systems. Med Care 2013;51(8 Suppl 3):S45–52 [DOI] [PubMed] [Google Scholar]
- 19.Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med 2010;363:501–4 [DOI] [PubMed] [Google Scholar]
- 20.Institute of Medicine. Data harmonization for patient-centered clinical research—a workshop. 2014
- 21.PCORnet. PCORnet common data model specification. Version 1.0 Washington, DC: PCORI, 2014 [Google Scholar]
- 22.Abernethy AP, Herndon JE, II, Wheeler JL, et al. Improving health care efficiency and quality using tablet personal computers to collect research-quality, patient-reported data. Health Serv Res 2008;43:1975–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sung NS, Crowley WF, Jr, Genel M, et al. Central challenges facing the national clinical research enterprise. JAMA 2003;289:1278–87 [DOI] [PubMed] [Google Scholar]
- 24.Trinidad SB, Fullerton SM, Ludman EJ, et al. Research ethics. Research practice and participant preferences: the growing gulf. Science 2011;331:287–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Solomon MZ, Bonham AC. Ethical oversight of research on patient care. Hastings Cent Rep 2013;S1:pp S2–3. 10.1002/hast.132 [DOI] [PubMed] [Google Scholar]
- 26.Platt R, Kass NE, McGraw D. Ethics, regulation, and comparative effectiveness research: time for a change. JAMA 2014. Published Online First: Epub Date. 10.1001/jama.2014.2144 [DOI] [PubMed] [Google Scholar]
- 27.PPRN Consortium, Daughtery S, Whaba S, et al. PPRNs consortium. PCORI patient-powered research networks: building capacity for conducting patient-centered clinical outcomes research. J Am Med Inform Assoc 2014;21:583–6. [DOI] [PMC free article] [PubMed] [Google Scholar]