Abstract
Background:
Detection of hepatitis B virus (HBV) genomes without detectable hepatitis B surface antigen (HBs-Ag) is termed occult HBV infection (OHBV) that may be transmitted by blood transfusion or organ transplantation and has acute reactivation when an immunosuppressive status like human immunodeficiency virus (HIV) infection occurs. We aimed to evaluate OHBV in HIV-infected patients with isolated antibodies to hepatitis B core antigen (anti-HBc) in Isfahan, Iran.
Materials and Methods:
In a cross-sectional study during August-September 2011, serum samples from HIV-infected patients who attended Isfahan Consultation Center for Behavioral Diseases were tested for HBs-Ag and anti-HBc using ELISA method. HBV-deoxyribonucleic acid (DNA) was detected and quantified in plasma of HBs-Ag negative/anti-HBc positive subjects by real-time polymerase chain reaction.
Results:
From 64 HIV-positive individuals, 12 (18%) patients were HBs-Ag negative/anti-HBc positive, and from those 3 (25%) had detectable HBV-DNA in their plasma.
Conclusion:
It seems that occult HBV might be assessed and be treated in HIV-infected patients.
Keywords: Hepatitis B, hepatitis B core antigen, human immunodeficiency virus
INTRODUCTION
Hepatitis B virus (HBV) is a serious global health problem with 2 billion people infected, from which 350 million suffer from chronic hepatitis B worldwide.[1] For the long time, hepatitis B surface antigen (HBs-Ag) positivity has been the classic carrier state; however, it is demonstrated that HBV replication may persist for years in the livers of HBs-Ag negative patients after they have recovered from acute HBV infection.[2,3] Occult HBV infection (OBI) is defined as the presence of HBV-deoxyribonucleic acid (DNA) in individuals who test negative for HBs-Ag and is more frequent in patients positive for the antibody to hepatitis B core antigen (anti-HBc).[4] The state of suppression of viral replication and gene expression typical of the occult HBV status, leads to a severe and sometimes even fulminant hepatitis B[5] which is an event is usually observed in immunosuppressed patients like human immunodeficiency virus (HIV)–infected ones. In fact, these patients may show a reaction of the viral replication because of the fault of the immunological control which leads to cytotoxic T lymphocytes-medical hepatocyte injury and development of hepatitis.[6] Exposure to HBV infection is common among HIV-infected patients because of shared routes of transmission, and serologic markers of prior or active HBV infection are identified in up to 68% of HIV patients.[3]
Conflicting data are reported on the prevalence of occult HBV infection in HIV settings, and the published data for occult HBV prevalence in patients with HIV infection ranges from 0% to 89.5% in the world.[7] In a study by Neau et al., it was recommended to test all HIV-infected persons for both HBs-Ag and anti-HBc and if either is positive, to test for HBV-DNA.[8] In a study in Iran 85% of HIV-infected patients with positive ‘anti-HBc alone’ were reported to be HBV viremic.[9] As there was no more study in Iran, we aimed to determine the frequency of occult HBV infection among a sample of HBs-Ag−/anti-HBc+ HIV-infected subjects in Isfahan-Iran.
MATERIALS AND METHODS
In a cross-sectional study during August-September 2011, all the HIV-infected patients who attended Isfahan Consultation Center for Behavioral Diseases on a voluntary basis after obtaining informed consent, enrolled in this study regardless of clinical stage of infection, sex or HIV transmission category. The project was approved by the Ethical Committee of Isfahan University of Medical Sciences (research project number: 389301).
The subjects had laboratory confirmed HIV by Western blot and completed a checklist that collected demographic data at enrollment. From each patient, a serum sample was obtained and was stored at −70°C. Clinical and therapeutic data were retrieved from the database of Isfahan Consultation Center for Behavioral Diseases.
Immunologic evaluation for HBs-Ag was performed using enzyme immunoassay test kit (Diapro-Milano-Italy), in accordance with manufacture's specification. Those samples that were negative for HBs-Ag were tested for total anti-HBc by enzyme immunoassay (Diapro-Milano-Italy), and for those that were positive for anti-HBc, HBV-DNA test was done. DNA was extracted from 200 μl of serum using high pure viral Nucleic Acid kit (Roche, Germany). For detection of HBV genomes, samples were assessed by Taqman real-time polymerase chain reaction in the Rotor-Gene Q (QIAGEN. Germany). Analytical studies yielded a limit of detection of 10 IU/ml.
RESULTS
Of 64 HIV-infected patients evaluated in the study, we identified 58 HBs-Ag negative and of them, 12 (20.7%) were anti-HBc positive. HIV acquisition was unknown.
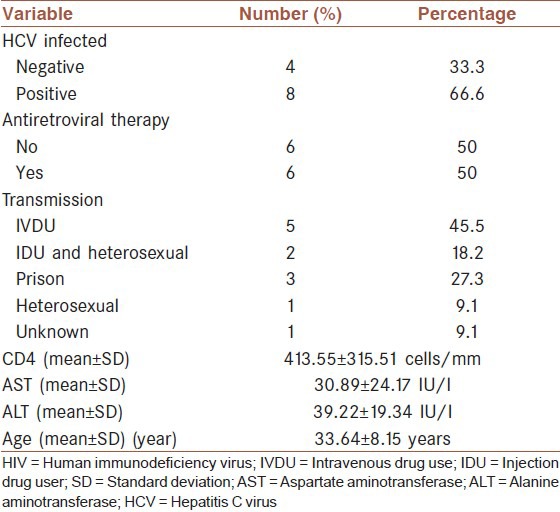
After testing for HBV-DNA, 3 (25%) subjects identified with occult HBV. The plasma HBV-DNA load in the three patients was 357, 536, and 267857 IU/ml. All of them were male and co-infected with hepatitis C virus (HCV). Subjects with and without occult HBV infections were similar with regard to age, use of antiretroviral therapy, CD4 count, aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels, co-infection with HCV, and routes of HIV transmission. Table 1 presents the clinical and demographic characteristics of these patients.
Table 1.
Baseline characteristics of HIV+ subjects with isolated hepatitis B core antibody (n= 12)
DISCUSSION
In this study, isolated anti-HBc was detected in 18.75% of the HIV-infected subjects from whom 25% had occult HBV infection. The frequency of isolated anti-HBc in HIV-infected patients is not similar in different studies.[10,11] About 50% of cases with OHBV infection have been reported to be positive for anti-HBc.[12] The prevalence of occult HBV in HIV-infected patients in previous studies varies from 0% to 89.5% in the world which may be due to the diverse prevalence of hepatitis B and HIV infections in different geographical regions and the sensitivity of the technique used to detect the HBV-DNA.[6,7]
There are some reports in Iran as well. In a study which was carried out in Tehran, Iran, 20.75% of HIV-infected patients had isolated anti-HBc, and HBV-DNA was detected in 13.6% of them.[13] In another study in Tehran, Iran, HBV-DNA was detected in 12 out of 40 (30%) high-risk patients, including HIV-infected and hemodialysis patients with anti-HBc alone.[14] It is demonstrated that, the mortality rate is 19 times higher in co-infected patients than in HIV mono-infected individuals and an increased risk of liver-related morbidity and mortality among HIV-HBV co-infected patients have been indicated.[15]
Prior studies among HIV-infected patients found that occult HBV increased the frequency of transaminitis and hepatic flares.[16] We evaluated ALT and AST levels, which are biochemical markers of liver injury. We did not find any correlation between HBV-DNA detection in the plasma and these parameters which may be due to small sample size.
In our study, all of the OHBV patients were HCV infected, which is important. Occult hepatitis B, particularly in HCV-infected subjects may play a role in accelerating the progression of liver disease.[17] Furthermore, patients with chronic hepatitis C and OHBV infection have more frequently lack of response to interferon treatment, and a higher risk of developing hepatocellular carcinoma than those with chronic HCV alone.[18]
On the other hand, in patients co-infected with hepatitis and HIV, more sever and end-stage liver disease is declared.[19] Approximately 20% of HIV-infected patients in the world have chronic hepatitis C infection and HCV has emerged as an important cause of morbidity and mortality in these patients.[15]
It is concluded that occult HBV might be regularly assessed in HIV-infected population. Our study limited by small sample size which is due to problems in HIV patient's selection.
AUTHORS’ CONTRIBUTION
All authors have contributed in designing and conducting the study. KT and BA collected the data and AJ and FKh did the analysis. All authors have assisted in preparation of the first draft of the manuscript or revising it critically for important intellectual content. All authors have read and approved the content of the manuscript and are accountable for all aspects of the work.
ACKNOWLEDGMENTS
The authors are grateful to Research Council of Isfahan University of Medical Sciences for financial support of this study. Also they acknowledge Professor Mohsen Janghorbani for his contribution in preparation of the manuscript.
Footnotes
Source of Support: The authors are gratefully acknowledged to Research Council of Isfahan University of Medical Sciences for financial support of this study.
Conflict of Interest: None declared.
REFERENCES
- 1.Lavanchy D. Hepatitis B virus epidemiology, disease burden, treatment, and current and emerging prevention and control measures. J Viral Hepat. 2004;11:97–107. doi: 10.1046/j.1365-2893.2003.00487.x. [DOI] [PubMed] [Google Scholar]
- 2.Mason AL, Xu L, Guo L, Kuhns M, Perrillo RP. Molecular basis for persistent hepatitis B virus infection in the liver after clearance of serum hepatitis B surface antigen. Hepatology. 1998;27:1736–42. doi: 10.1002/hep.510270638. [DOI] [PubMed] [Google Scholar]
- 3.Raimondo G, Pollicino T, Cacciola I, Squadrito G. Occult hepatitis B virus infection. J Hepatol. 2007;46:160–70. doi: 10.1016/j.jhep.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 4.Núñez M, Ríos P, Pérez-Olmeda M, Soriano V. Lack of ‘occult’ hepatitis B virus infection in HIV-infected patients. AIDS. 2002;16:2099–101. doi: 10.1097/00002030-200210180-00024. [DOI] [PubMed] [Google Scholar]
- 5.Mphahlele MJ, Lukhwareni A, Burnett RJ, Moropeng LM, Ngobeni JM. High risk of occult hepatitis B virus infection in HIV-positive patients from South Africa. J Clin Virol. 2006;35:14–20. doi: 10.1016/j.jcv.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 6.Santos EA, Yoshida CF, Rolla VC, Mendes JM, Vieira IF, Arabe J, et al. Frequent occult hepatitis B virus infection in patients infected with human immunodeficiency virus type 1. Eur J Clin Microbiol Infect Dis. 2003;22:92–8. doi: 10.1007/s10096-002-0868-0. [DOI] [PubMed] [Google Scholar]
- 7.Lok AS, McMahon BJ. Chronic hepatitis B: Update 2009. Hepatology. 2009;50:661–2. doi: 10.1002/hep.23190. [DOI] [PubMed] [Google Scholar]
- 8.Neau D, Winnock M, Jouvencel AC, Faure M, Castéra L, Legrand E, et al. Occult hepatitis B virus infection in HIV-infected patients with isolated antibodies to hepatitis B core antigen: Aquitaine cohort, 2002-2003. Clin Infect Dis. 2005;40:750–3. doi: 10.1086/427882. [DOI] [PubMed] [Google Scholar]
- 9.Sharifi-Mood B, Sanei-Moghaddam E, Ghasem-Zadeh I, Khosravi S. Occult Hepatitis B virus Infection among anti-HBc only positive individuals in the Southeast of Iran in high prevalence of HBV infection region. Iran Red Crescent Med J. 2009;11:90–2. [Google Scholar]
- 10.Grob P, Jilg W, Bornhak H, Gerken G, Gerlich W, Günther S, et al. Serological pattern “anti-HBc alone”: Report on a workshop. J Med Virol. 2000;62:450–5. doi: 10.1002/1096-9071(200012)62:4<450::aid-jmv9>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 11.Gandhi RT, Wurcel A, Lee H, McGovern B, Boczanowski M, Gerwin R, et al. Isolated antibody to hepatitis B core antigen in human immunodeficiency virus type-1-infected individuals. Clin Infect Dis. 2003;36:1602–5. doi: 10.1086/375084. [DOI] [PubMed] [Google Scholar]
- 12.Hollinger FB, Sood G. Occult hepatitis B virus infection: A covert operation. J Viral Hepat. 2010;17:1–15. doi: 10.1111/j.1365-2893.2009.01245.x. [DOI] [PubMed] [Google Scholar]
- 13.Azadmanesh K, Mohraz M, Aghakhani A, Edalat R, Jam S, Eslamifar A, et al. Occult hepatitis B virus infection in HIV-infected patients with isolated hepatitis B core antibody. Intervirology. 2008;51:270–4. doi: 10.1159/000160217. [DOI] [PubMed] [Google Scholar]
- 14.Ramezani A, Banifazl M, Eslamifar A, Aghakhani A. Serological pattern of anti-HBc alone infers occult hepatitis B virus infection in high-risk individuals in Iran. J Infect Dev Ctries. 2010;4:658–61. doi: 10.3855/jidc.728. [DOI] [PubMed] [Google Scholar]
- 15.Ramezani A, Banifazl M, Mohraz M, Rasoolinejad M, Aghakhani A. Occult hepatitis B virus infection: A major concern in HIV-infected patients: Occult HBV in HIV. Hepat Mon. 2011;11:7–10. [PMC free article] [PubMed] [Google Scholar]
- 16.Filippini P, Coppola N, Pisapia R, Scolastico C, Marrocco C, Zaccariello A, et al. Impact of occult hepatitis B virus infection in HIV patients naive for antiretroviral therapy. AIDS. 2006;20:1253–60. doi: 10.1097/01.aids.0000232232.41877.2a. [DOI] [PubMed] [Google Scholar]
- 17.Sagnelli E, Coppola N, Scolastico C, Mogavero AR, Filippini P, Piccinino F. HCV genotype and “silent” HBV coinfection: Two main risk factors for a more severe liver disease. J Med Virol. 2001;64:350–5. doi: 10.1002/jmv.1057. [DOI] [PubMed] [Google Scholar]
- 18.Pollicino T, Squadrito G, Cerenzia G, Cacciola I, Raffa G, Craxi A, et al. Hepatitis B virus maintains its pro-oncogenic properties in the case of occult HBV infection. Gastroenterology. 2004;126:102–10. doi: 10.1053/j.gastro.2003.10.048. [DOI] [PubMed] [Google Scholar]
- 19.Thio CL. Management of chronic hepatitis B in the HIV-infected patient. AIDS Read. 2004;14:122–9. 133, 136-7. [PubMed] [Google Scholar]


