Abstract
Genitourinary tuberculosis (GUTB) is a rare extrapulmonary manifestation of tuberculosis (TB). Various forms of presentation are described and in most cases the disease results in calcification, atrophy, or necrosis of the renal parenchyma. The kidney is not generally palpable except in cases of hydronephrosis due to an upper ureteric stricture. We present a case of GUTB presenting as inflammatory pseudotumor. This case was initially diagnosed as renal malignancy and managed accordingly. Histopathology confirmed the diagnosis of pseudotumoral renal TB.
Keywords: Extrapulmonary tuberculosis, genitourinary tuberculosis, pseudotumor, renal cell carcinoma
INTRODUCTION

Tuberculosis (TB) can involve any organ system in the body. Although pulmonary TB is the most common presentation, extrapulmonary TB is also an important clinical problem. Genitourinary tuberculosis (GUTB) complicates 3-4% of patients with pulmonary TB.[1,2] Hematogenous dissemination from an active site of infection results in GUTB. Initially metastatic lesions (tubercles) are formed in the kidneys. Macroscopic progression of the disease is often unilateral.[3] Usually, these lesions heal spontaneously or as a result of treatment. Patients present with dysuria and hematuria, which may be painless, flank pain, sterile pyuria, and recurrent urinary tract infection. In rare cases, acute presentation mimicking renal mass have also been described. Other uncommon presentations include the following: Nonhealing wounds, sinuses or fistulae, hemospermia and others.
CASE REPORT
A 34-year-old woman presented with 1-month history of intermittent right flank pain and occasional fever. Two-months earlier she had one episode of gross hematuria. Clinically, a ballotable and bimanually palpable vague lump was appreciated in right hypochondrium. She did not have any history of pulmonary TB in the past. A marginally elevated erythrocyte sedimentation rate was noted. Although urine culture was sterile, 10-12 pus cells were seen on microscopic urine examination. Chest X-ray was normal. Contrast-enhanced computed tomography (CECT) showed a heterogeneously enhancing lesion 8 × 7 cm in dimension with areas of necrosis, involving the right kidney with enlarged aortocaval and paraaortic lymph nodes [Figure 1a and b]. Right renal vein and inferior venacava were normal. She then underwent right radical nephrectomy [Figure 2]. Histopathology showed presence of acid-fast bacilli with multiple granulomas consistent with GUTB [Figure 3a and b]. Postoperatively we started oral antitubercular therapy. Patient recovered well, completed her antitubercular therapy, and after 1 year of follow-up she is free of TB.
Figure 1.
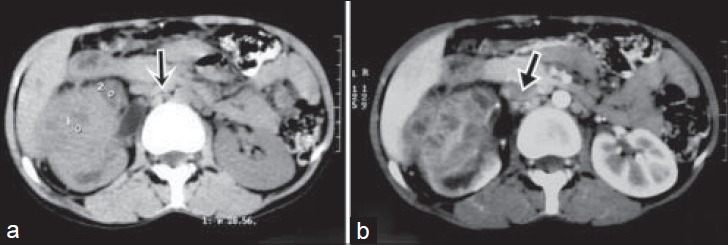
34-year-old woman with intermittent right flank pain diagnosed with genitourinary tuberculosis. (a) Computed tomography (CT) shows heterogeneous enhancing mass involving the upper and mid pole of the right kidney with aortocaval and paracaval lymphadenopathy(arrow) and (b) contrast enhanced CT scan of the abdomen show presence of rim enhancement with central necrosis in lymph nodes (arrow).
Figure 2.
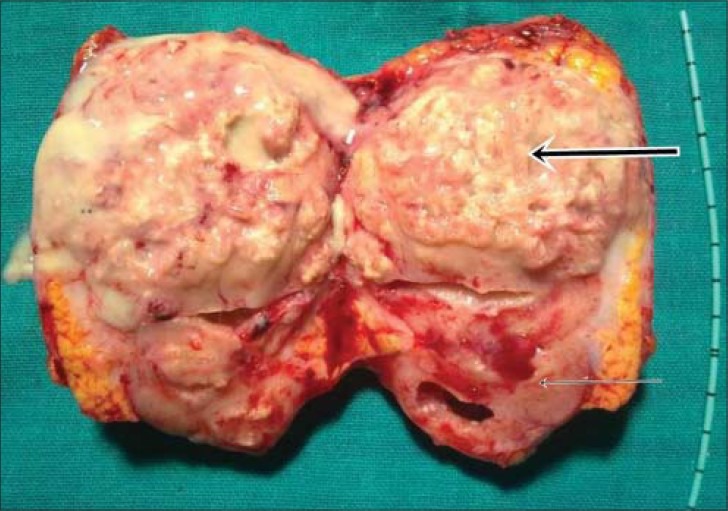
34-year-old woman with intermittent right flank pain diagnosed with genitourinary tuberculosis. Section removed during right side nephrectomy shows normal looking kidney (thin arrow and renal mass with pus around it (thick arrow).
Figure 3.
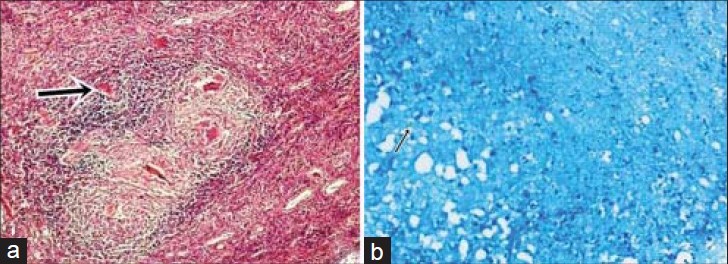
34-year-old woman with intermittent right flank pain diagnosed with genitourinary tuberculosis. Histopathology slides (a) stained with hematoxylin and eosin (×100) shows presence of multiple granulomas (thick arrow) and (b) stained with Ziehl-Neelsen stain (×100) shows presence of acid-fast bacilli (thin arrow).
DISCUSSION
TB is a common public health problem in endemic areas like India. It continues to be an important diagnostic problem because of its nonspecific clinical presentation and variable radiographic appearances that often mimic many other pathologic lesions. The first note of urogenital TB was made by Porter (1894). Later, Wildbolz (1937) suggested the term genitourinary TB. The term “Urogenital TB” is more logical because kidney TB, which is usually primary, is diagnosed more often than genital TB. Only 53% of patients with kidney TB had genital lesions, but in 61.9% patients with epididymorchitis and in 79.3% patients with TB of the prostate, a renal lesion could be diagnosed. In GUTB, the kidneys are the most common sites of infection and are infected through hematogenous spread of the bacilli, which then spread through the renal and genital tract. GUTB is the second most common form of extrapulmonary TB in countries with severe epidemic situations and the third most common form in regions with a low incidence of TB.[4]
GUTB usually presents with nonspecific symptoms and variable radiographic appearances. The diagnosis of TB on images of the urinary tract depends on the stage of the infection. Tubercular granulomas in the renal pyramids coalesce to form ulcers that discharge mycobacteria and pus in the urine. Untreated lesions enlarge and a tubercular abscess may form in the parenchyma. Later on, perinephric abscess is formed and the kidney is replaced by caseous material (“putty kidney”), which may become calcified (“cement kidney”) and nonfunctional leading to renal failure.[5] CT findings include focal caliectasis, hydronephrosis, calcifications, cortical thinning, and soft tissue masses.[6] Usually an enhancing renal mass is caused by renal cell carcinoma, metastasis, lymphoma, or an abscess.[7] GUTB rarely manifests as pseudotumors, which otherwise are usually due to hypertrophied column of Bertin, renal dysmorphism, or unusually shaped kidney.[8] In rare cases, urinary TB manifests as either single or multiple parenchymal nodules without urinary tract involvement. Patients with this form, known as the pseudotumoral type, present with variable-sized but well-defined parenchymal nodules on cross-sectional images.[9] Clinical and radiological findings mimic those of a renal cancer.[9,10] The lesion may simulate a renal hydatid cyst or a pseudotumoral xanthogranulomatous pyelonephritis.[10] Pseudotumoral GUTB end up undergoing a surgical removal and diagnosis is suspected intraoperatively or histopathologically. Surgery must be followed by antituberculous therapy. Pseudotumoral GUTB is extremely rare and may simulate renal cancer.
CONCLUSION
Pseudotumoral presentation of GUTB is very rare. Renal TB should be suspected when atypical renal masses are seen in patients from TB endemic areas. Preoperative fine-needle aspiration cytology (FNAC) can be considered in highly suspicious cases. Treatment includes surgery followed by antitubercular therapy. An early diagnosis can save the kidney.
Footnotes
Available FREE in open access from: http://www.clinicalimagingscience.org/text.asp?2014/4/1/26/133259
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Hemal AK. Genitourinary tuberculosis. In: Sharma SK, Mohan A, editors. Tuberculosis. New Delhi: Jaypee Brothers Medical Publishers; 2001. pp. 325–37. [Google Scholar]
- 2.National survey of notifications of tuberculosis in England and Wales in 1983. Medical Research Council Tuberculosis and Chest Diseases Unit. Br Med J (Clin Res Ed) 1985;291:658–61. doi: 10.1136/bmj.291.6496.658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kumar S. Female genital tuberculosis. In: Sharma SK, Mohan A, editors. Tuberculosis. New Delhi: Jaypee Brothers Medical Publishers; 2001. pp. 311–24. [Google Scholar]
- 4.Kulchavenya E, Kim CS, Bulanova O, Zhukova I. Male genital tuberculosis: Epidemiology and diagnostic. World J Urol. 2012;30:15–21. doi: 10.1007/s00345-011-0695-y. [DOI] [PubMed] [Google Scholar]
- 5.Lima NA, Vasconcelos CC, Filgueira PH, Kretzmann M, Sindeaux TA, Feitosa Neto B, et al. Review of genitourinary tuberculosis with focus on end-stage renal disease. Rev Inst Med Trop Sao Paulo. 2012;54:57–60. doi: 10.1590/s0036-46652012000100011. [DOI] [PubMed] [Google Scholar]
- 6.Das KM, Indudhara R, Vaidyanathan S. Sonographic features of genitourinary tuberculosis. AJR Am J Roentgenol. 1992;158:327–9. doi: 10.2214/ajr.158.2.1729792. [DOI] [PubMed] [Google Scholar]
- 7.Wein AJ, Kavoussi LR, Campbell MF. 10th ed. Philadelphia: WB Saunders; 2012. Campbell-Walsh Urology; pp. 1417–8. [Google Scholar]
- 8.Bhatt S, MacLennan G, Dogra V. Renal Pseudotumors. AJR Am J Roentgenol. 2007;188:1380–7. doi: 10.2214/AJR.06.0920. [DOI] [PubMed] [Google Scholar]
- 9.Njeh M, Jemni M, Abid R, Karray MS, el Ouakdi M, Ayed M. Renal tuberculosis with pseudotumoral form: Apropos of a case. J Urol (Paris) 1993;99:150–2. [PubMed] [Google Scholar]
- 10.Merran S. Diagnostic case: Pseudotumoral tuberculous pyelonephritis. J Radiol. 1995;76:1122–4. [PubMed] [Google Scholar]


