Abstract
We present a case of diverticular colitis of the ascending colon preceding the onset of ulcerative colitis. A 58-year-old man presented with positive faecal occult blood test. Colonoscopy disclosed diverticular colitis of the ascending colon. After a year's follow-up, typical ulcerative colitis developed and diverticular colitis improved. Diverticular colitis is a newly established disorder of chronic segmental mucosal inflammation affected by diverticular disease. There is increasing recognition of such cases with diverticular colitis preceding ulcerative colitis. There may be a possible pathogenic relationship between the two diseases.
Background
Diverticular colitis (DC) is a newly established disorder of chronic colitis. Only a small number of cases with DC have progressed to classical ulcerative colitis (UC). Moreover, this progression has been documented by endoscopy very rarely.
Case presentation
A 58-year-old man presented for positive faecal occult blood test. He had regular stool once daily and denied any symptoms. His medical history was unremarkable. On examination, there was no tenderness on the abdomen with normal bowel sounds. Routine laboratory tests were normal. Colonoscopy was then performed.
Investigations
Colonoscopy disclosed segmental inflammation of the ascending colon with multiple diverticula (figure 1). Patchy loss of vascular pattern, oedema, and hyperaemic mucosa over diverticula were presented (figure 2). Biopsies of the inflamed mucosa revealed lymphoplasmacytic inflammation with eosinophils and haemorrhage in the lamina propria and neutrophilic crypt abscesses (figure 3). The rectum (figure 4) and other segments of the colon were macroscopically normal. Stool culture was negative. A diagnosis of DC of the ascending colon was carried out. He had been followed conservatively until he presented haematochezia a year later. Repeated colonoscopy showed typical UC with rectosigmoid involvement (figure 5) and the improvement of known DC (figure 6). Stool culture was negative. The progression of DC to UC was then diagnosed.
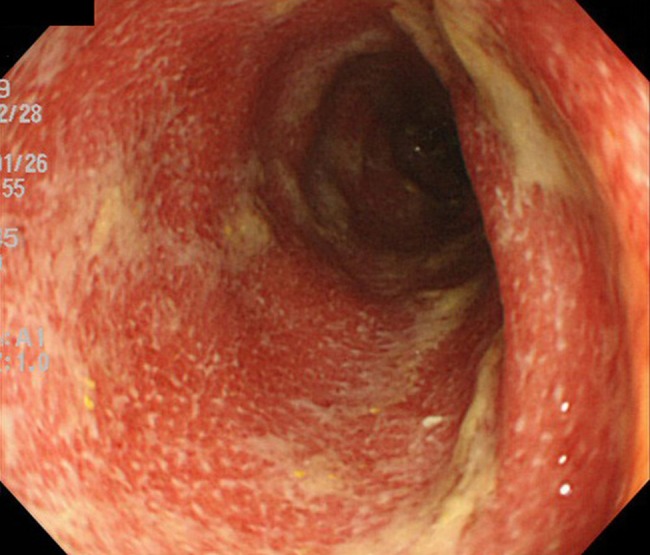
Figure 1.
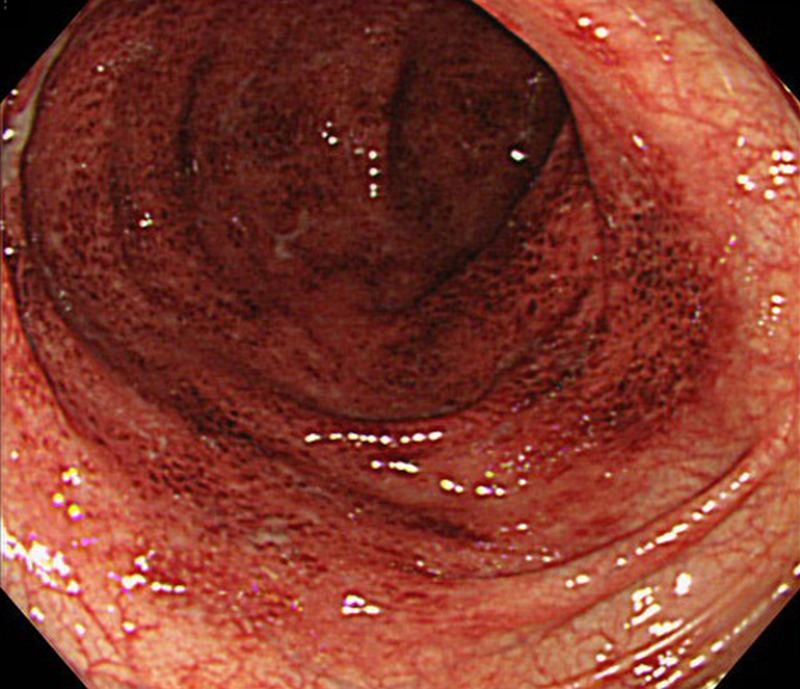
Colonoscopy showing segmental inflammation involving the ascending colon with multiple diverticula.
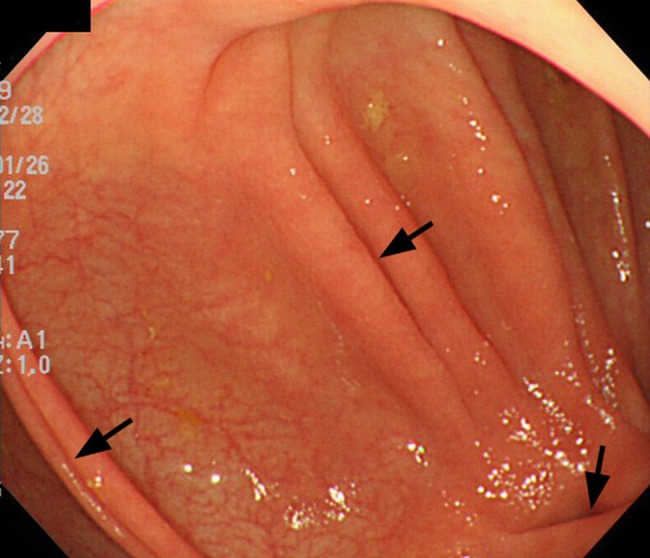
Figure 2.
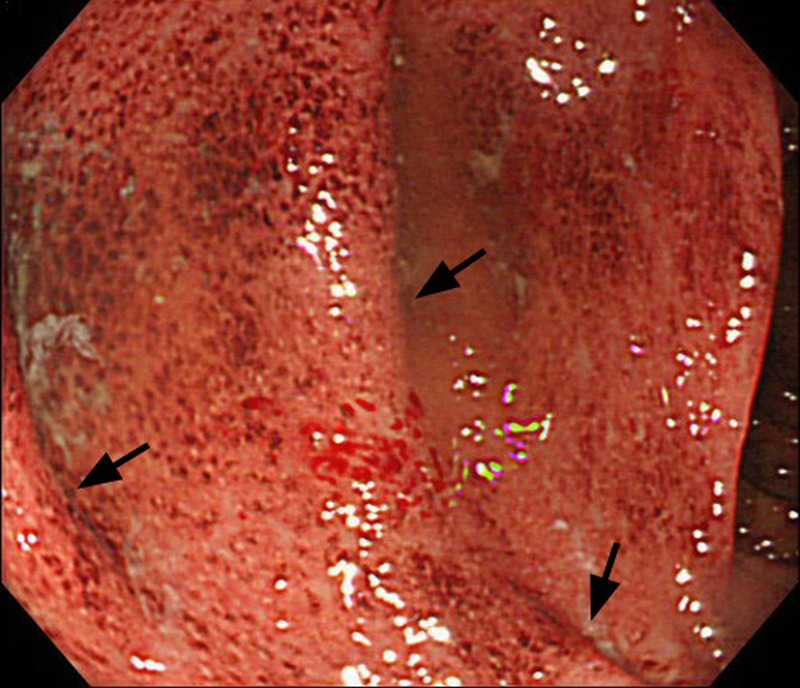
Colonoscopy showing patchy loss of vascular pattern, oedema and hyperaemic mucosa over diverticula (arrows).
Figure 3.
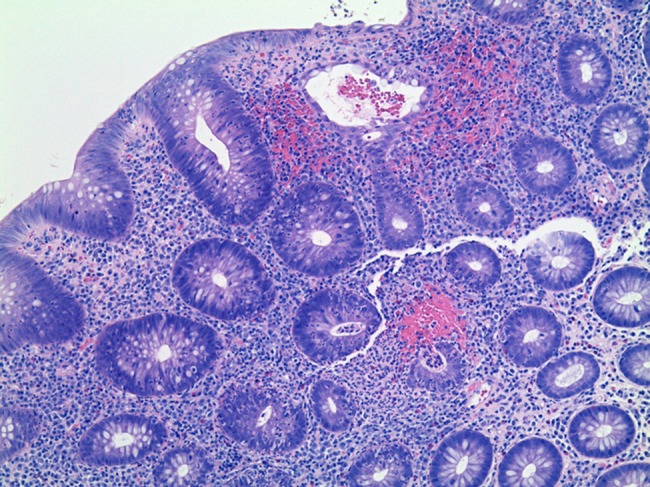
Histopathological picture of the inflamed mucosa showing lymphoplasmacytic inflammation with eosinophils and haemorrhage in the lamina propria and neutrophilic crypt abscesses (H&E, ×100, magnification).
Figure 4.
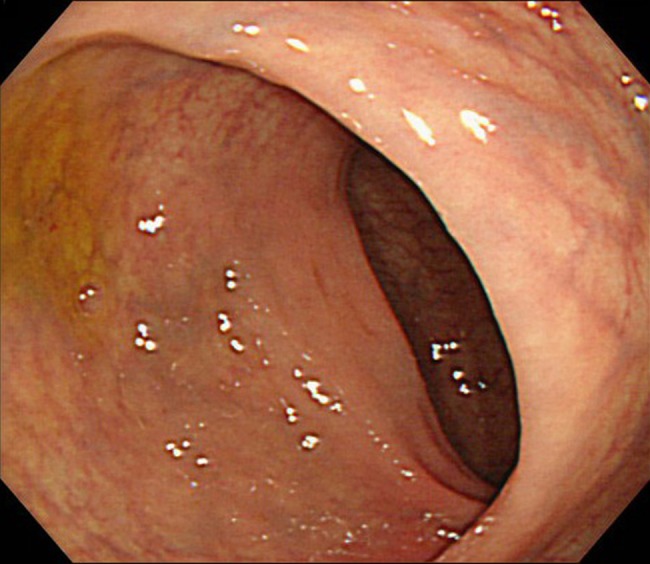
Colonoscopy showing the macroscopically normal rectum.
Figure 5.
Colonoscopy showing typical ulcerative colitis with rectosigmoid involvement.
Figure 6.
Colonoscopy showing the improvement of the known inflammation over the same diverticula (arrows) in the ascending colon.
Differential diagnosis
Diverticular colitis
Ulcerative colitis
Infectious colitis
Diverticulitis
Treatment
His symptoms and rectosigmoid inflammation of UC responded well to oral mesalazine.
Outcome and follow-up
Rectosigmoid UC has sometimes relapsed due to poor medication adherence.
Discussion
DC, also known as diverticular disease-associated colitis, or segmental colitis associated with diverticulosis, is a newly established disorder of chronic segmental mucosal inflammation affected by diverticular disease.1 More than 200 cases with DC have been reported worldwide.2 3 Although the pathogenesis has not been unveiled, multiple pathogenic factors including mucosal prolapse, faecal retention, mucosal ischaemia and mucosal compression by subserosal peridiverticulitis have been postulated.1 Although less than 20 cases with DC preceding UC have been reported,1 4 there is increasing recognition of such cases. It may shed new light on the pathogenesis of UC. Recent studies have revealed that appendiceal orifice inflammation (AOI) in certain cases has preceded development of UC presumably by priming lymphocytes at the appendix.5 6 As appendix and diverticulum have similar blind-ending structures with faecal stasis, it is speculated that diverticular inflammation of DC may also prime lymphocytes then trigger distal UC. In our first case with DC preceding UC,7 sigmoid inflammation of DC had lasted when UC developed. In the present case, however; the inflammation of DC resolved when UC appeared. It may suggest the existence of diverse phenotypes in DC. In conclusion, DC should be followed carefully as DC may precede the onset of UC.
Patient's perspective.
UC can be managed in remission with regular medication.
Learning points.
Diverticular colitis is a newly established disorder of chronic segmental mucosal inflammation affected by diverticular disease.
Although rare, diverticular colitis may precede the onset of conventional ulcerative colitis.
There may be a possible pathogenic relationship between diverticular colitis and ulcerative colitis.
Footnotes
Contributors: TM, AH and TK were involved in the treatment of the patient. TM wrote the manuscript. AH reviewed the manuscript. JF supervised the study.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Ludeman L, Shepherd NA. What is diverticular colitis? Pathology 2002;34:568–72 [DOI] [PubMed] [Google Scholar]
- 2.Mulhall AM, Mahid SS, Petras RE, et al. Diverticular disease associated with inflammatory bowel disease-like colitis: a systematic review. Dis Colon Rectum 2009;52:1072–9 [DOI] [PubMed] [Google Scholar]
- 3.Tursi A, Elisei W, Brandimarte G, et al. The endoscopic spectrum of segmental colitis associated with diverticulosis. Colorectal Dis 2010;12:464–70 [DOI] [PubMed] [Google Scholar]
- 4.Pereira MC. Diverticular disease-associated colitis: progression to severe chronic ulcerative colitis after sigmoid surgery. Gastrointest Endosc 1998;48:520–3 [DOI] [PubMed] [Google Scholar]
- 5.Park SH, Yang SK, Kim MJ, et al. Long term follow-up of appendiceal and distal right-sided colonic inflammation. Endoscopy 2012;44:95–8 [DOI] [PubMed] [Google Scholar]
- 6.Park SH, Loftus EV, Jr, Yang SK. Appendiceal skip inflammation and ulcerative colitis. Dig Dis Sci 2014. In press. doi: 10.1007/s10620-014-3129-z [DOI] [PubMed] [Google Scholar]
- 7.Hokama A, Kinjo F, Tomiyama R, et al. Progression of diverticular colitis to ulcerative colitis. Inflamm Bowel Dis 2005;11:618. [DOI] [PubMed] [Google Scholar]


