Abstract
A 29-year-old woman presented with symptoms of gradual, progressive, painless diminution of vision in both eyes for past 8–10 years. On examination, uncorrected visual acuity was 20/60 in the right eye and 20/126 in the left eye. Anterior segment examination was essentially normal except for a conical protrusion in the pupillary axis of the anterior lens capsule with a clear underlying lens. During surgery, central protruded fragile lens capsule was meticulously handled to create well-centered continuous curvilinear capsulorhexis by using paediatric rhexis forceps. Histopathology of excised capsule showed markedly thinned lens capsule with normal epithelium. Electron microscopy of the anterior lens capsule showed multiple linear and irregular zones of dehiscence. Few of these had fibrillar, irregular electron-dense material and vacuoles; and adjacent cells were irregular suggestive of Alport syndrome. Postoperative course was uneventful and visual acuity improved to 20/20 unaided. Clear lens extraction is an effective means of rehabilitating visually symptomatic anterior lenticonus of Alport syndrome.
Background
Alport syndrome is a rare disorder of the basement membrane due to mutations involving the coding for type IV collagen resulting in a defective synthesis of type IV collagen; characterised by progressive hereditary nephritis, sensorineural hearing loss and ocular abnormalities.1 Biomechanical properties of a normal capsule depend primarily on type IV collagen and other extracellular matrix constituents, such as collagen types I and III, laminin, and fibronectin.2 Defective type IV collagen eventually results in increased capsular fragility,thus leading to progressive forward bowing of capsule at its weakest point. It manifests as a slowly progressive deterioration of vision, resulting from high degree of lenticular myopia.3 We report the clinical and electron microscopic findings of anterior capsule in a case of bilateral anterior lenticonus of Alport syndrome.
Case presentation
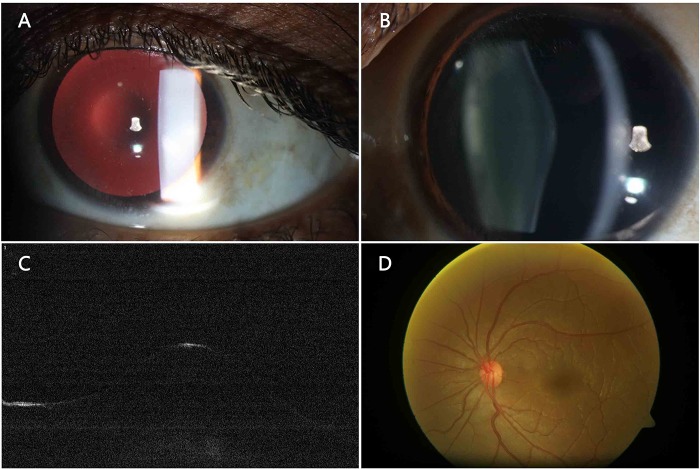
A 29-year-old woman presented with gradual, progressive, painless diminution in her vision in both eyes, more for distance than near for the past 8–10 years. There was a frequent change in spectacle prescription for the past 5 years. She also had recent onset of progressive hearing loss. Family history revealed second-degree parental consanguinity. Her parents were asymptomatic; however, her elder sibling was treated for similar ailment in the past. On examination, her uncorrected visual acuity was 20/60 in the right eye and 20/126 in the left eye. Refraction was −19.50−0.75/50° in OD and −20.00−1.75/180° in OS. Retinoscopy revealed a central oil droplet reflex (figure 1A). Anterior segment examination was essentially within normal limits except for conical protrusion in the anterior lens capsule with clear lens (figure 1B).
Figure 1.
Slit lamp photograph of the right eye showing (A) typical oil droplet reflection on retroillumination, (B) slit section of anterior capsule showing conical protrusion in the pupillary area, (C) anterior segment optical coherence tomography showing anterior conical protrusion of lens capsule, (D) fundus photographs showing few retinal flecks.
Investigations
Anterior segment optical coherence tomography (OCT, Carl Zeiss Meditec, Dublin, California, USA) was suggestive of the anterior lenticonus (figure 1C). Retinal examination revealed a few visually insignificant flecks in both the eyes (figure 1D). Pure tone audiometry revealed bilateral sensorineural deafness more for frequencies between 3000 and 4000 Hz. Urine analysis showed microscopic haematuria and proteinuria. Ultrasound abdomen picked up bilateral renal parenchymal disease. Her blood pressure was 110/80 mm Hg. Urine analysis reports of her father showed microscopic haematuria and red blood cells 4–5/high power field. Based on the corroborative findings, diagnosis of bilateral anterior lenticonus of Alport syndrome was made. For visual rehabilitation clear lens extraction with intraocular implantation was considered.
Treatment
Surgery was planned sequentially at an interval of 4 weeks between the eyes, under local anaesthesia. A preoperative biometry was performed. Two stab wounds at 10 and 2 o’clock were made and a 3 mm triplanar, superior clear corneal incision was placed. Anterior chamber was inflated with a cohesive viscoelastic agent (Healon OVD), Abbott Laboratories Inc, Illinois, USA) after staining the fragile anterior capsule with trypan blue, anterior capsule was meticulously handled in order to achieve central curvilinear capsulorhexis by using a 23 G capsulorhexis forceps (Indo-German Surgical Corporation, India; Video). The stripped off anterior capsule was sent for histological examination.
Outcome and follow-up
On the first postoperative day, the visual acuity improved to 20/20 with pinhole in both the eyes. Slit lamp biomicroscopy revealed in situ posterior chamber intraocular lens (figure 2A, B). Postoperative medications included topical prednisolone acetate 1% drops six times a day for the first week, tapered over the next 4 weeks and moxifloxacin 0.5% eye drops four times a day for the first 1 week. Postoperatively, her visual acuity was 20/30 improving to 20/20 p with −1.50 Cyl D@10° in the right eye whereas in order to give her a monocular near vision, left eye was kept slightly myopic, with a visual acuity of 20/50 improving to 20/25 p with −1.25 Sph D/−1.75 Cyl D @25° with unaided near vision of N6.
Figure 2.
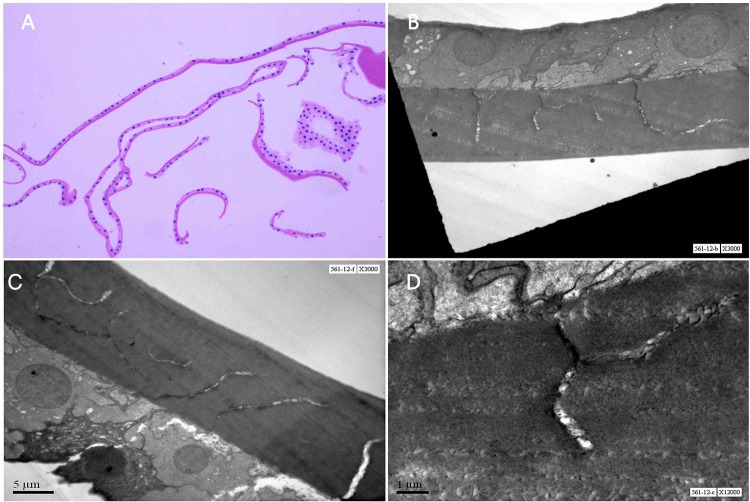
Histopathology of the excised anterior capsule. (A) Markedly thinned lens capsule with atrophic epithelium in central portion (H&E, ×100). (B) EM of anterior capsule showed multiple linear and irregular zones of capsular dehiscence in inner two-third of capsule. (C) A normal lens epithelium with thinned anterior lens capsule. (D) A few of this dehiscence had a fibrillar and irregular electron dense material and vacuoles.
Histopathology
Sections from the specimens showed markedly thinned lens capsule with normal epithelium in the central portion (figure 3A). Electron microscopy of anterior capsule showed multiple linear and irregular zones of capsular dehiscence. A few of these had fibrillar and irregular electron-dense material. The adjacent cells were irregular, highly suggestive of Alport syndrome (figure 3B–D).
Figure 3.
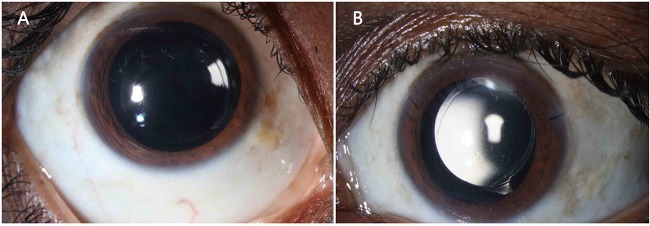
Postoperative (A) right eye and (B) left eye slit lamp images showing intra-ocular lens in situ.
Surgical video demonstrating the technique of capsulorhexis in case of anterior lenticonus.
Discussion
Alport syndrome is a group of basement membrane abnormality due to defective type IV collagen gene and has estimated prevalence of 1 case per 5000 people and 85% of patients have the X linked inheritance form, although there can be autosomal recessive (10%) or autosomal dominant (5%) inheritance. Men are affected more commonly and more severely. Nephritis with haematuria secondary to basement membrane disease of the glomeruli is the most life-threatening aspect of this disorder. Progressive sensorineural hearing loss beginning with high frequencies, most pronounced at a frequency of between 2000 and 8000 Hz, which makes it difficult to distinguish speech and gives increased sensitivity to loud noises, is characteristic. The most frequent ocular findings are progressive bilateral lenticonus and it occurs in approximately 25% of patients with X linked Alport syndrome,when present, it may be a pathognomonic feature.1–3 Lens capsule comprises a three-dimensional molecular meshwork made up primarily of type IV collagen and other extracellular matrix constituents, such as collagen types I and III, laminin and fibronectin.2 Each constituent is important to the biomechanical properties of the capsule. Mutation in the gene that codes for these constituents will result in capsule fragility leading to conical protrusion of the capsule at its weakest point and rarely can it get ruptured. Anterior lenticonus is more commonly seen than posterior, which leads to progressive lenticular myopia developing by the second decade as seen in our patient.4 5 In our case, axial length and corneal curvature were normal, which further substantiate that the myopia was lenticular in origin. The presence of retinal flecks in Alport syndrome is usually innocuous and does not lead to a decrease in vision. Although, there are several published reports of successful clear lens extraction for anterior lenticonus, capsulorhexis is technically difficult in view of highly fragile and elastic anterior capsule; hence it is extremely important to be very meticulous to prevent radial extension. All the intracapsular manoeuvers should be performed with utmost caution to avoid posterior capsular rupture. Acrylic intra-ocular lens with square edged designs were used to minimise capsular opacification.5 6
Histopathological examination of anterior lens capsule under electron microscope is a unique feature in our case. The anterior lens capsule was extremely thin, fragile with normal epithelium. Electron microscope study revealed multiple linear dehiscences in the inner 2/3 of capsule, containing fibrillar material and vacuoles. Studies have demonstrated similar changes on electron microscopic examination.7 In addition to the histological changes of the anterior capsule, the weakened structure is stressed during accommodation, as the anterior lens curvature becomes more convex centrally or rarely capsule may rupture.8–10 The combination of these factors might lead to linear dehiscence in the inner two-third of the anterior lens capsule, as seen in our patient.
In conclusion, though rare, symptomatic anterior lenticonus can be successfully managed by clear lens extraction with intraocular lens implantation, while a fragile lens capsule should be meticulously handled to prevent radial extension under appropriate anaesthesia. Timely recognition of systemic complications can minimise the irreversible damage. The EM demonstrates the fact that defective basement membrane would ultimately result in forward protrusion of lens capsule due to dehiscence.
Learning points.
Alport syndrome is a rare genetic disorder characterised by progressive hereditary nephritis with haematuria secondary to basement membrane disease of the glomeruli is the life-threatening component of this disease.
Bilateral lenticonus is a common presenting clinical sign and seen in ≅1/4th of patients with X linked inheritance, when present, it may be a pathognomonic feature.
Capsulorhexis is technically difficult in view of highly fragile and elastic anterior capsule; hence, it is extremely important to be very meticulous to avoid radial extension.
Electron microscope showed multiple linear dehiscences in the inner two-third of capsule, perhaps as result of progressive bowing of anterior capsule during accommodation would have resulted in microruptures within in fragile capsule.
Timely recognition of this rare clinical condition can lessen life-threatening systemic complications.
Acknowledgments
Photography: SBN chary Ddigital editing: Katheek K Histopathology technical support: B Sreedhar Rao, GC Naidu. Dr Partho Bakshi for logistics in the working of the case.
Footnotes
Contributors: MR involved in the design and conduct of the study; SK involved in the data collection and preparation; KM involved in the histopathology reporting; MR, SC were involved in the management, analysis, and interpretation; SC and MR Other were involved in the critical preparation, review, or approval of the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Colville D, Savige J, Morfis M, et al. Ocular manifestations of autosomal recessive Alport syndrome. Ophthalmic Genet 1997;18:119–28 [DOI] [PubMed] [Google Scholar]
- 2.Kohno T, Sorgente N, Ishibashi T, et al. Immunofluorescent studies of fibronectin and laminin in the human eye’. Invest Ophthalmol Vis Sci 1987;28:506–14 [PubMed] [Google Scholar]
- 3.Seymenoglu G, Baser EF. Ocular manifestations and surgical results in patients with Alport syndrome. J Cataract Refract Surg 2009;35:1302–6 [DOI] [PubMed] [Google Scholar]
- 4.Liu YB, Tan SJ, Sun ZY, et al. Clear lens phacoemulsification with continuous curvilinear capsulorhexis and foldable intraocular lens implantation for the treatment of a patient with bilateral anterior lenticonus due to Alport syndrome. J Int Med Res 2008;36:1440–4 [DOI] [PubMed] [Google Scholar]
- 5.Gupta A, Ramesh Babu K, Srinivasan R, et al. Clear lens extraction in Alport syndrome with combined anterior and posterior lenticonus or ruptured anterior lens capsule. J Cataract Refract Surg 2011;37:2075–8 [DOI] [PubMed] [Google Scholar]
- 6.Zare MA, Rajabi MT, Nili-Ahmadabadi M, et al. Phacoemulsification and intraocular lens implantation in Alport syndrome with anterior lenticonus. J Cataract Refract Surg 2007;33:1127–30 [DOI] [PubMed] [Google Scholar]
- 7.Choi Jh, Na Ks, Bae Sh, et al. Anterior lens capsule abnormalities in Alport syndrome. Korean J Ophthalmol 2005;19:84–9 [DOI] [PubMed] [Google Scholar]
- 8.Wilson ME, Jr, Trivedi RH, Biber JM, et al. Anterior capsule rupture and subsequent cataract formation in Alport syndrome. J AAPOS 2006;10:182–3 [DOI] [PubMed] [Google Scholar]
- 9.Olitsky SE, Waz WR, Wilson ME. Rupture of the anterior lens capsule in Alport syndrome. J AAPOS 1999;3:381–2 [DOI] [PubMed] [Google Scholar]
- 10.Chaurasia S, Garg P. Bilateral spontaneous rupture of the anterior capsule. J Cataract Refract Surg 2008;34:1413–15 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Surgical video demonstrating the technique of capsulorhexis in case of anterior lenticonus.