Abstract
Aim
To determine the efficacy of 2.0 mg aflibercept in the management of patients with recalcitrant exudative age-related macular degeneration (AMD).
Methods
In this prospective, open-label, single-arm clinical trial, patients were seen monthly and given mandatory 2.0 mg aflibercept at baseline, months 1, 2 and 4. Pro re nata (PRN) retreatment at months 3 and 5 was performed upon evidence of disease on spectral domain-optical coherence tomography (SD-OCT). End point at month 6: mean change in Early Treatment Diabetic Retinopathy Study best corrected visual acuity (ETDRS BCVA) and central subfield thickness (CST), mean number of aflibercept injections, percentage of PRN injections required, patients with no fluid on SD-OCT and patients losing >15 letters.
Results
At baseline, 46 patients with a mean of 42 prior antivascular endothelial growth factor-A (anti-VEGF) intravitreal treatments had a mean of 74.2 letters (Snellen equivalent 20/32) and mean CST of 347 µm. ETDRS letters remained stable throughout the trial; at month 6, mean BCVA change was +0.2 letters (range −10 to +13, p=0.71). Anatomically, mean CST improved significantly from baseline at each study visit including −23.6 µm at month 1 and −27.3 µm at month 6 (p=0.018). Seventy-one of 90 (79%) possible PRN injections were required and a mean of 5.6 aflibercept injections out of the maximum six were administered. Ten of 45 (22%) patients had no retinal fluid on SD-OCT at month 6. No patient lost >15 letters.
Conclusions
Aflibercept 2.0 mg treatment maintained mean visual acuity improvements previously achieved with high-dose 2.0-mg ranibizumab injections in recalcitrant wet AMD patients. Aflibercept 2.0 mg treatment led to significant anatomic improvement and was required monthly in most patients.
Clinical Trials Registration
FDA IND#12462. NCT 01543568.
Trial Details
IND 12462, NCT 01543568 http://clinicaltrials.gov/show/NCT01543568.
Keywords: Retina, Clinical Trial, Macula, Degeneration, Neovascularisation
Introduction
Neovascular age-related macular degeneration (AMD) is a leading cause of vision loss around the world.1 Pharmaceutical agents that block vascular endothelial growth factor-A (VEGF) have revolutionised the management of neovascular AMD and most exudative retinal diseases. Nevertheless, many eyes treated with monthly dosing of ranibizumab (Lucentis, Genentech, South San Francisco, California, USA),2 3 bevacizumab (Avastin, Genentech, South San Francisco, California, USA),4 or aflibercept (Eylea, Regeneron, Tarrytown, New Jersey)5 manifest recalcitrant fluid. For example, in the CATT trial (Comparison of AMD Treatment Trial), despite monthly treatment with anti-VEGF agents for 2 years, 51.5% of patients treated with ranibuzumab and 67.4% of patients given bevacizumab showed evidence of persistent fluid on time-domain optical coherence tomography (OCT).4 Similarly, in the VIEW1 and VIEW2 trials (VEGF Trap-Eye: Investigation of Efficacy and Safety in Wet AMD), between 27.6% and 32.3% of patients had evidence of persistent intraretinal or subretinal fluid at the primary end-point of 1 year despite 2.0 mg aflibercept treatment.5 Such residual intraretinal or subretinal fluid likely limits optimal visual improvement,6 and patients with recalcitrant wet AMD represent a substantial clinical burden.
Evidence suggests that some of these patients may benefit from a higher dose of anti-VEGF medication or switching to a different pharmacologic agent. The SAVE trial (Super-dose Anti-VEGF (SAVE) Trial: 2.0 mg Intravitreal Ranibizumab for Recalcitrant Neovascular Age-Related Macular Degeneration) demonstrated significant visual and anatomic gains in recalcitrant wet AMD eyes at both 1 and 2 years of treatment.7 8 However, pro re nata (PRN) retreatments were required at almost every monthly visit in these aggressive wet AMD eyes, and retinal fluid was still present in 70% (45/64) of patients at the end of 2 years.8
The current study aimed to determine if 2.0 mg aflibercept could maintain or even improve upon the visual acuity and anatomic gains of the SAVE trial for these well-characterised recalcitrant exudative AMD eyes.
Materials and methods
This study was a prospective, multicentre, open-label, single-arm clinical trial (aflibercepT for subjects with exudative AMD who were incomplete responders to mUltiple Ranibizumab anti-VEGF injections (TURF trial); Food and Drug Administration (FDA) Investigational New Drug #12462). Inclusion criteria were that only patients who completed the 2-year, prospective SAVE trial (NCT01025232) in which recalcitrant wet AMD eyes were treated with 2.0 mg ranibizumab7–9 were eligible. TURF sample size was determined by enrolling all consenting patients who enrolled directly into TURF immediately following completion of the SAVE trial. There was a protocol-mandated 28-day minimum ‘wash-out’ before enrolment in the TURF study in which patients could not have received any anti-VEGF medication. No patient had received prior aflibercept treatment. Exclusion criteria included significant subretinal fibrosis or geographic atrophy involving the fovea.
After obtaining institutional review board (IRB) approval of the study protocol and consent, appropriate patients seen at Retina Consultants of Houston were identified, provided with informed consent documents, and enrolled. Data was collected at Retina Consultants of Houston in the Texas Medical Center (6560 Fannin, Suite 750, Houston, Texas) and in The Woodlands, Texas (17350 St Luke's Way, Suite 120).
At all study visits, subjects underwent best corrected Early Treatment Diabetic Retinopathy Study best corrected visual acuity (ETDRS BCVA) and comprehensive ophthalmic examination including applanation tonometry, slit-lamp evaluation and dilated binocular indirect ophthalmoscopy. Fundus photography and fluorescein angiography were performed at baseline, month 3 and month 6. Spectral domain OCT (SD-OCT) was performed at each visit using the Heidelberg Spectralis HRA+OCT (Spectralis; Heidelberg Engineering, Heidelberg, Germany). All patients received 0.05 mL open-label intravitreal injections of 2.0 mg aflibercept administered every 28 days for the first 3 months (baseline, month 1 and month 2), one mandatory dose at month 4 and, as needed, doses at months 3 and 5. PRN retreatments at months 3 and 5 were performed in the presence of intraretinal or subretinal fluid on SD-OCT or if BCVA decreased >5 letters from the previous visit.
Sterile surgical technique was applied for each intravitreal injection. Patients self-administered topical antimicrobials four times daily for 3 days prior to treatment. After topical anaesthesia, the periocular skin, eyelid and eyelashes were treated with 10% povidone iodine swabs, and 5% povidone iodine ophthalmic solution was applied to the conjunctival surface. Following intravitreal injection, finger-counting testing was performed and indirect ophthalmoscopy was performed to confirm central retinal artery perfusion.
Key outcome measures included mean change in ETDRS BCVA from baseline, mean change in central subfield thickness (CST), mean number of 2.0 mg intravitreal aflibercept injections administered, percentage of PRN injections required, percentage of patients with no intraretinal, subretinal, or subretinal pigment epithelial (RPE) fluid on SD-OCT at month 6 and percentage of patients who lost >15 letters BCVA. All SD-OCT segmentations were manually confirmed and corrected as needed to follow the internal limiting membrane and Bruch's membrane prior to computation of SD-OCT change maps and CST (MEM, CCW). Statistical comparisons were performed with paired Student t tests where appropriate.
Results
Patient characteristics
Forty-six patients enrolled directly from the SAVE trial into the TURF trial between April and September 2012.7–9 Baseline demographics and clinical findings are described in table 1. Forty-five of 46 (98%) patients completed the 6-month trial. At baseline, patients had received a mean of 42 (range 19–67) prior anti-VEGF intravitreal treatments including a mean of 21 (range 13–24) prior 2.0 mg ranibizumab treatments out of a maximum 24 during the immediately preceding 24 months of the SAVE trial. Median time from prior anti-VEGF treatment to the first aflibercept treatment was 28 days (mean 33.3, range 28 to 68 days).
Table 1.
Baseline patient demographics
| Baseline demographics | |
|---|---|
| Patients | 46 |
| Sex (male/female) | 22/24 |
| Age m(r) | 77.8 (55–95) |
| Prior anti-VEGF injections m(r) | 42 (19–67) |
| 2.0 mg ranibizumab injections m(r) | 21 (13–24) |
| Washout period in days m(r) | 33 (28–68) |
| ETDRS BCVA m(r) | 74.2 (41–92) |
| Snellen equivalent (r) | (20/100–20/16) |
| SD OCT CST μm m(r) | 347 (188–565) |
| Intraretinal fluid n(%) | 17 (37) |
| Subretinal fluid n(%) | 21 (46) |
| Sub-RPE fluid n(%) | 18 (39) |
| No intraretinal, subretinal, or Sub-RPE fluid n(%) | 8 (17) |
anti-VEGF, anti-vascular endothelial growth factor-A; CST, central subfield thickness; ETDRS BCVA, Early Treatment Diabetic Retinopathy Study best corrected visual acuity; m, mean; OCT, optical coherence tomography; r, range; sub-RPE, subretinal pigment epithelial.
Visual outcomes
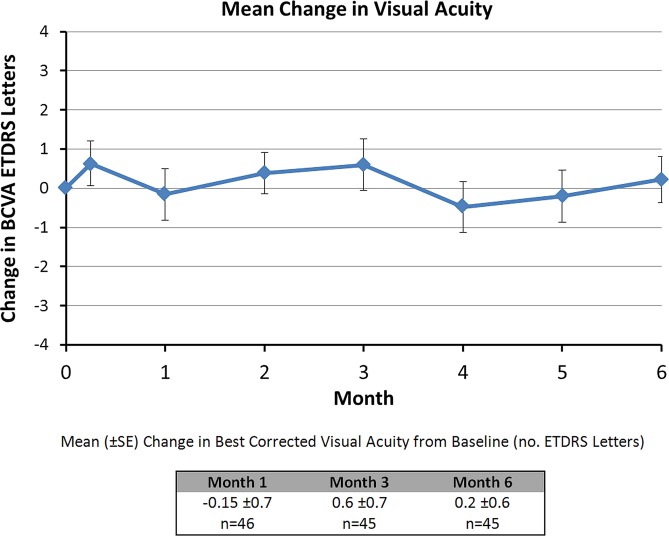
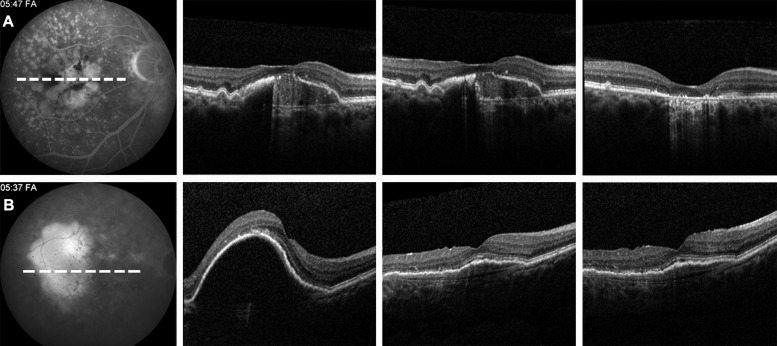
At enrolment, mean BCVA was 74.2 ETDRS letters (Snellen equivalent 20/32, range 41–91, 20/100–20/16). BCVA remained stable throughout the 6-month trial with no significant fluctuation; at month 6, mean change was +0.2 ETDRS letters (range −10 to +13, p=0.71) (figure 1). At 6 months, 4 eyes (9%) improved by ≥5 ETDRS letters and 1 eye (2%) improved by ≥10 ETDRS letters, gaining 13 letters within the first month of treatment; PRN retreatment was required at both PRN visits in 3 of 4 of these patients, while 1 patient received neither PRN retreatment. At month 6, 4 eyes (9%) lost ≥5 letters or more with 1 eye (2%) receiving neither PRN retreatment and losing 10 letters associated with collapse of a pigment epithelial detachment (PED) and progression of geographic atrophy (figure 2A); PRN retreatment was required at both PRN visits in 2 of 4 of these patients, and 2 patients received neither PRN retreatment. No patient lost >15 letters BCVA.
Figure 1 .
Change in mean best-corrected visual acuity (best corrected visual acuity (BCVA); Early Treatment Diabetic Retinopathy Study (ETDRS) letters) over 6 months with standard error (SE) bars.
Figure 2 .
Case examples. Baseline late-phase fluorescein angiograms (FA) with associated spectral domain optical coherence tomography (SD-OCT) orientations (white dashed line) followed by sequential SD-OCT images at baseline (left), 1 month (centre) and 6 months (right). (A) flattening of pigment epithelial detachment (PED) from baseline associated with retinal pigment epithelial and outer retinal atrophy. (B) flattening of PED with residual subretinal fluid under the fovea at month 6.
Anatomic outcomes
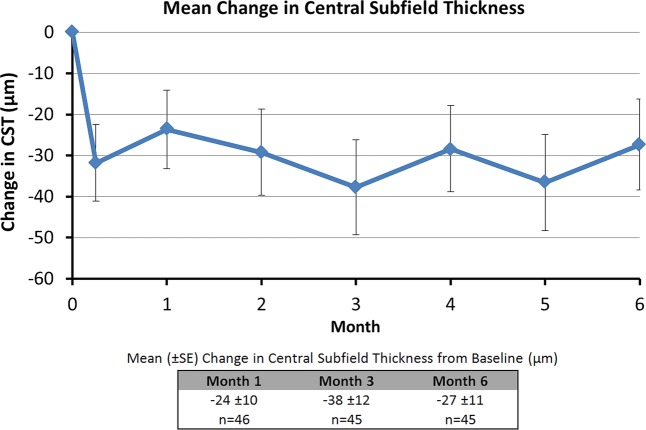
At enrolment, mean CST was 347 μm (range 188–565 µm). Mean CST improved significantly from baseline at all study visits including −23.6 µm at month 1 (−5%, range −384 to +32 µm), and −27.3 µm at month 6 (−6%, range −381 to +59 µm, p=0.018) (figure 3).
Figure 3 .
Change in central subfield thickness (spectral domain optical coherence tomography (SD-OCT)) over 6 months with standard error (SE) bars. Central subfield thickness was evaluated monthly as well as 7 days after the first aflibercept treatment.
CST decreased >10% in 9 of 46 patients (19.6%) at month 3, and in 7 of 45 patients (15.6%) at month 6. For these eyes, the mean decrease in CST at month 6 was −149 µm (−31%, range −48 to −381 µm). Of the 7 patients with CST decrease >10% at month 6, 4 had complete, or near complete, resolution of PED (figure 2B); 94% of the decrease in CST in these patients was realised within the first 2 months of aflibercept treatment. At month 3, no patient gained >10% CST, but at month 6, 2 patients gained >10% CST, gaining either significant subretinal (60 µm) or intraretinal (92 µm) fluid after not receiving a PRN injection.
In total, 71 of 90 (79%) possible PRN injections were administered and a mean of 5.6 aflibercept injections out of the minimum 4 and maximum 6 total injections were administered. PRN retreatment was required at both PRN visits in 33 of 46 (72%) patients due to SD-OCT findings, and neither of the PRN injections were given in 8 of 46 (17%) patients. At months 3 and 6, 17 (37%) and 10 (22%) patients had no intraretinal, subretinal, or sub-RPE fluid, respectively.
Adverse events
Ocular and systemic adverse events are reported in table 2. There were no cases of endophthalmitis, intraocular inflammation, new subretinal haemorrhage, or traumatic cataract. In total, three patients were noted to have increased geographic atrophy (3/46, 7%). No systemic arterial thromboembolic events were identified. One (1/46, 2%) patient died at month 5 related to complications of acute onset leukaemia.
Table 2 .
Ocular and serious systemic adverse events (AEs)
| Ocular adverse event (%) | |
| Patients with ocular AEs | 6 (13) |
| Cataract progression | 3 (7) |
| Geographic atrophy progression | 3 (7) |
| Serious adverse events (%) | |
| Patients with SAEs | 9 (20) |
| Total SAEs | 11 (24) |
| Death | 1 (2) |
| Atrial fibrillation | 1 (2) |
| Squamous cell carcinoma | 2 (4) |
| Upper respiratory tract infection | 5 (11) |
| Urinary tract infection | 2 (4) |
Discussion
Eyes with recalcitrant exudative AMD are a substantial clinical burden, representing approximately a quarter to one-third of all new wet AMD eyes. In such patients, 2.0 mg ranibizumab, a fourfold higher dose than the FDA approved 0.5 mg dose for wet AMD management, appears capable of additional anatomic and visual benefit based on the SAVE trial outcomes at month 3, year 1 and year 2,7–9 as well as the LAST study (evaLuation of high-dose rAnibizumab (2.0 mg) in the management of AMD in patients with perSistent/recurrenT macular fluid).10 In the HARBOR study, 2.0 mg ranibizumab demonstrated no clinical advantage over the 0.5 mg ranibizumab dosing in treatment naive eyes11 and Genentech discontinued further development and clinical trials of the 2.0 mg dose. As the SAVE cohort had demonstrated sustained clinical benefit from the higher dose, we were reticent to switch these patients back to 0.5 mg ranibizumab. With FDA approval of aflibercept for therapeutic use, the TURF trial was designed to assess if the anatomic and BCVA gains could be maintained with this alternative pharmacologic agent. The TURF trial consisted entirely of patients exiting the SAVE trial, and demonstrates that commercially available 2.0 mg aflibercept treatment maintained the mean visual gains attained with 2.0 mg ranibizumab treatment and led to significant mean anatomic improvement. These anatomic gains were primarily driven by a minority of patients (20%, 9 of 45), many with dramatic flattening of PED. Despite no mean change in BCVA including all TURF patients, one patient gained 13 ETDRS letters within 1 month of aflibercept initiation, a patient who required both PRN retreatments.
The FDA approved labelling for aflibercept use in the management of wet AMD includes two options: 2 mg every 8 weeks after 3 initial monthly doses or 2 mg monthly. While both treatment regimens led to clinically equivalent mean visual outcomes in treatment-naive patients, there is evidence that continued monthly therapy after the first 3 monthly doses translates into better visual outcomes in some patients, particularly those with recalcitrant exudative disease activity. For example, when eyes with persistent macular oedema during each of the first 4 visits in VIEW1 and VIEW2 were considered, continued monthly aflibercept achieved superior outcomes compared with every 8-week dosing.12 The current TURF trial employed every other month dosing after the first 3-monthly doses, but was designed to permit PRN dosing at the intervening months. Supporting the observation that aflibercept does not maintain maximal retinal deturgesence for 2 months in many patients, and indicative of the recalcitrant exudative nature of the study eyes in TURF, 72% of eyes required retreatment at both PRN visits, and 79% of PRN retreatments were required. Furthermore, the only two patients who experienced a >10% gain in CST during the TURF trial both did not receive a PRN treatment the month prior.
In the treatment-naive eyes included in the VIEW1 and VIEW2 trials, aflibercept and ranibizumab treatment resulted in clinically equivalent visual outcomes.5 While both pharmacologic agents neutralise VEGF-A, aflibercept has a distinct mechanism of action and also inhibits VEGF-B and placental growth factor.13 As such, eyes with recalcitrant exudative AMD may respond differently to these medications. Indeed, many analyses have recently reported positive anatomic benefit, and in some cases visual benefit, with aflibercept in recalcitrant wet AMD eyes previously treated with ranbizumab or bevacizumab.14–18
The strength of this study is its prospective design involving a well-defined patient cohort who had received rigorous previous treatment with anti-VEGF therapies, as well as its standardised treatment and follow-up intervals. The limitations of this trial include the lack of a control group, relatively small sample size, and the limited duration of 6 months.
This study provides evidence that aflibercept treatment may be anatomically valuable in some recalcitrant exudative AMD eyes, while maintaining prior visual gains. Such value may be apparent relatively quickly after initiation of aflibercept treatment. However, a substantial majority of the patients in this prospective trial required monthly aflibercept dosing to achieve maximal anatomic and visual benefit. Longer-term data will be valuable to guide the ongoing management of patients with recalcitrant wet AMD.
Footnotes
Contributors: CCW: concept, design, PI, writing of the manuscript (guarantor); DMB: concept, design, revision of the manuscript; MEM: data collection, analysis, writing of the manuscript. DEC: data collection, analysis, writing of the manuscript.
Funding: Research grant from Regeneron Pharmaceuticals. The funding organisation had no role in the design or conduct of this research.
Competing interests: Yes. ICMJE conflicts of interest forms have been attached.
Ethics approval: Sterling IRB.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Jager RD, Mieler WF, Miller JW. Age-related macular degeneration. N Engl J Med 2008;358:2606–17 [DOI] [PubMed] [Google Scholar]
- 2.Brown DM, Kaiser PK, Michels M, et al. Ranibizumab versus verteporfin for neovascular age-related macular degeneration. N Engl J Med 2006;355:1432–44 [DOI] [PubMed] [Google Scholar]
- 3.Rosenfeld PJ, Brown DM, Heier JS, et al. Ranibizumab for neovascular age-related macular degeneration. N Engl J Med 2006;355:1419–31 [DOI] [PubMed] [Google Scholar]
- 4.Martin DF, Maguire MG, Fine SL, et al. Ranibizumab and Bevacizumab for treatment of Neovascular age-related macular degeneration: two-year results. Ophthalmology 2012;119:1388–98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heier JS, Brown DM, Chong V, et al. Intravitreal Aflibercept (VEGF Trap-Eye) in Wet Age-related Macular Degeneration. Ophthalmology 2012;119:2537–48 [DOI] [PubMed] [Google Scholar]
- 6.Brown DM, Tuomi L, Shapiro H. Anatomical measures as predictors of visual outcomes in ranibizumab-treated eyes with neovascular age-related macular degeneration. Retina 2013;33:23–34 [DOI] [PubMed] [Google Scholar]
- 7.Wykoff CC, Brown DM, Chen E, et al. SAVE (Super-dose Anti-VEGF) trial: 2.0 mg Ranibizumab for recalcitrant Neovascular age-related macular degeneration: 1-Year results. Ophthalmic Surg Lasers Imaging Retin 2013;44:121–6 [DOI] [PubMed] [Google Scholar]
- 8.Wykoff CC, Brown DM, Croft DE, et al. Two year SAVE outcomes: 2.0 mg ranibizumab for recalcitrant neovascular AMD. Ophthalmology 2013;120:1945–6 e1941 [DOI] [PubMed] [Google Scholar]
- 9.Brown DM, Chen E, Mariani A, et al. Super-dose anti-VEGF (SAVE) trial: 2.0 mg intravitreal ranibizumab for recalcitrant neovascular macular degeneration-primary end point. Ophthalmology 2013;120:349–54 [DOI] [PubMed] [Google Scholar]
- 10.Fung AT, Kumar N, Vance SK, et al. Pilot study to evaluate the role of high-dose ranibizumab 2.0 mg in the management of neovascular age-related macular degeneration in patients with persistent/recurrent macular fluid <30 days following treatment with intravitreal anti-VEGF therapy (the LAST Study). Eye (Lond) 2012;26:1181–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Busbee BG, Ho AC, Brown DM, et al. Twelve-month efficacy and safety of 0.5 mg or 2.0 mg ranibizumab in patients with subfoveal neovascular age-related macular degeneration. Ophthalmology 2013;120:1046–56 [DOI] [PubMed] [Google Scholar]
- 12.Jaffe G. The Effect of Early, Persistent Fluid on Subsequent Visual Acuity in the VIEW 1 and VIEW 2 Studies of Neovascular AMD. American Societey of Retina Specialists Toronto, Canada, August 25th. 2013
- 13.Nguyen QD, Shah SM, Browning DJ, et al. A phase I study of intravitreal vascular endothelial growth factor trap-eye in patients with neovascular age-related macular degeneration. Ophthalmology 2009;116:2141–8 e2141. [DOI] [PubMed] [Google Scholar]
- 14.Chang AA, Li H, Broadhead GK, et al. Intravitreal aflibercept for treatment-resistant neovascular age-related macular degeneration. Ophthalmology 2014;121:188–92 [DOI] [PubMed] [Google Scholar]
- 15.Bakall B, Folk JC, Boldt HC, et al. Aflibercept therapy for exudative age-related macular degeneration resistant to bevacizumab and ranibizumab. Am J Ophthalmol 2013;156:15–22 [DOI] [PubMed] [Google Scholar]
- 16.Yonekawa Y, Andreoli C, Miller JB, et al. Conversion to aflibercept for chronic refractory or recurrent neovacular age-related macular degeneration. Am J Ophthalmol 2013;156:29–35 [DOI] [PubMed] [Google Scholar]
- 17.Cho H, Shah CP, Weber M, et al. Aflibercept for exudative AMD with persistent fluid on ranibizumab and/or bevacizumab. Br J Ophthalmol 2013;97:1032–5 [DOI] [PubMed] [Google Scholar]
- 18.Schachat AP. Switching anti-vascular endothelial growth factor therapy for neovascular age-related macular degeneration. American J Ophthalmol 2013;156:1–2 e1 [DOI] [PubMed] [Google Scholar]