Abstract
Objectives
To investigate the effects of a multifaceted implementation strategy on behaviour, behavioural determinants, knowledge and awareness of healthcare workers regarding the use of recommendations to prevent hand eczema.
Methods
The Hands4U study is a randomised controlled trial. A total of 48 departments (n=1649 workers) were randomly allocated to the multifaceted implementation strategy or the control group (minimal implementation strategy). Within the departments designated to the multifaceted implementation strategy, participatory working groups were set up to enhance the implementation of the recommendations for hand eczema. In addition, working group members were trained to become role models, and an education session was given within the department. Outcome measures were awareness, knowledge, receiving information, behaviour and behavioural determinants. Data were collected at baseline, with a 3- and 6-month follow-up.
Results
Statistically significant effects were found after 6 months for awareness (OR 6.30; 95% CI 3.41 to 11.63), knowledge (B 0.74; 95% CI 0.54 to 0.95), receiving information (OR 9.81; 95% CI 5.60 to 17.18), washing hands (B −0.40; 95% −0.51 to −0.29), use of moisturiser (B 0.29; 95% CI 0.20 to 0.38), cotton under gloves (OR 3.94; 95% CI 2.04 to 7.60) and the overall compliance measure (B 0.14; 95% CI 0.02 to 0.26), as a result of the multifaceted implementation strategy. No effects were found for behavioural determinants.
Conclusions
The multifaceted implementation strategy can be used in healthcare settings to enhance the implementation of recommendations for the prevention of hand eczema.
Trial registration number
NTR2812.
Keywords: randomized controlled trial, implementation
What this paper adds.
Evidence based recommendations are available for the prevention of hand eczema in healthcare workers, but these are not implemented well into daily practice.
The multifaceted implementation strategy used in this study proved to be effective on behaviour related to the compliance of recommendations for the prevention of hand eczema.
The multifaceted implementation strategy was effective for knowledge and awareness related to hand eczema prevention.
The strategy can be used in practice to enhance implementation of recommendations for the prevention of hand eczema among healthcare workers.
Background
In the Netherlands, many healthcare workers report symptoms related to hand eczema.1 This is not surprising since hand eczema is one of the most prevalent occupational disease.2 Risk factors for developing this condition are—among others—exposure to water and detergents, and wearing occlusive gloves: irritants which are handled frequently by healthcare workers during their work.3–5
According to a review by Agner and Held,6 the prevention of hand eczema in an occupational setting should focus on the reduction of risk factors, as well as on the use of skin protection measures, like the use of moisturisers and cotton under gloves.6 In the Netherlands, the Netherlands Society of Occupational Medicine (NVAB) used the aforementioned as a starting point to develop a guideline containing recommendations to reduce occupational hand eczema.7 Unfortunately, many new guidelines do not reach the target group or are not implemented into daily practice.8 Therefore, we developed a multifaceted implementation strategy with the aim of implementing the recommendations from the NVAB guideline in order to prevent hand eczema among healthcare workers in the Netherlands.9 We evaluated this strategy in the Hands4U study, a two-armed randomised controlled trial (RCT) among healthcare workers.
A change in behaviour is often the most important goal of an implementation strategy.10 In the present study, a change in behaviour of the healthcare workers towards the use of the NVAB recommendations is used as a measure for implementation of the NVAB guideline. A commonly used model for explaining behaviour is the attitude, social influence and self-efficacy (ASE) model.11 The determinants, attitude, social influence and self-efficacy, influence the intention to perform the desired behaviour.12 13 The intention to perform the behaviour is the strongest predictor for actually performing the behaviour.14 Apart from these behavioural determinants, there are also barriers that can negatively influence implementation, such as a lack of knowledge or a lack of awareness.15 16 To be able to implement the NVAB guideline, it is thus necessary to change the behavioural determinants and reduce barriers related to implementation.
The primary aim of this study was to investigate the effects of the multifaceted implementation strategy on (1) behaviour of healthcare workers regarding the use of the recommendations to prevent hand eczema; (2) attitude, social influence, self-efficacy and intention to perform the desired behaviour (the use of the recommendations); and (3) knowledge and awareness among the healthcare workers, and the information they received on the prevention of hand eczema.
Methods
Study design
In this RCT, workers belonging to the department allocated to the intervention group received the multifaceted implementation strategy; departments allocated to the control group received a minimal implementation strategy. Data on the outcome measures were assessed at baseline and 6 months after baseline. Data on behaviour of the healthcare workers were also collected at 3 months after baseline. The data collection started in April 2011.9
The study protocol was approved by the Medical Ethics Committee of the VU University Medical Center in Amsterdam. As departments were included as a whole, this committee decided that participants did not have to sign an informed consent.
Study population
Participants for this study were recruited from three university hospitals, one academic centre for dentistry, two general hospitals and two nursing homes from different parts of the Netherlands. We included only departments where irritants were handled (eg, frequent hand washing, wearing gloves, handling food). In total, 48 departments participated in the Hands4U study. Inclusion criteria for workers at those departments were: (1) employed at one of the participating hospitals; (2) able to fill out Dutch questionnaires; (3) aged between 18 and 64 years; and (4) working for at least 8 h a week. Exclusion criterion was not handling irritants like water, disinfectants and gloves.
Randomisation, stratification and blinding
Randomisation of the intervention and control group took place at department level to avoid contamination between healthcare workers within departments. We used prestratification to establish equal groups at the department level, concerning risk for hand eczema and whether workers had contact with patients. Risk categorisation was determined by an occupational physician. Randomisation was performed in strata of two by an independent researcher based on the sequence of inclusion. The randomisation was performed before the baseline measurement. Workers were not informed about the outcome of the randomisation and the design of the study. However, all participants were informed about the goal of the study (the prevention of hand eczema in healthcare workers) via a letter and a leaflet. It was impossible to blind researchers, occupational nurses and department managers. Detailed information about the randomisation, stratification and blinding have been described previously.9
Intervention group: multifaceted implementation strategy
The intervention group received the multifaceted implementation strategy, which consisted of several components, including a leaflet containing the recommendations derived from the NVAB guideline to prevent and reduce hand eczema.9 17 A detailed description of this implementation strategy can be found elsewhere.9
The participatory working groups
The participatory working groups were the central part of the multifaceted implementation strategy. One working group was formed at each intervention department and was guided by a trained occupational nurse. The goal of the working group was to identify problems with adherence to the recommendations, find solutions for these problems and implement the solutions within their department.
Role model training
Working group members received training to become role models—the so-called ‘Dermacoaches’—for their colleagues. The Dermacoaches stimulated and motivated their colleagues to be aware of risk-behaviour during work and they tried to decrease problems with adherence to the recommendations within their department. Role model training was given by a trained occupational nurse.
The education programme
The goal of the education programme—a 20 min session—was to inform all workers about the risk of hand eczema and to train them in the actual use of individual preventive measures according to the NVAB guideline. During this education session, the workers received a bag containing a moisturiser, two flacons of disinfectant and one pair of cotton under gloves. Afterwards, key messages (reminders) were placed at relevant places within the department. If necessary, the education session was given several times to reach as many workers as possible.
Control group
The workers in the control group received a minimal implementation strategy consisting of the same leaflet as the intervention group.
Data collection
The baseline questionnaire was sent to all workers in participating departments who handled irritants. The departments were recruited between April 2011 and May 2012. A maximum of two reminders was sent to enhance overall response. After baseline, only the participants who had filled out the baseline questionnaire received the follow-up questionnaires at 3 and 6 months.
Outcome measures
Hand eczema preventive behaviour
The behaviour of the healthcare workers regarding the use of the NVAB recommendations was measured using a partly modified version of the Nordic Occupational Skin Questionnaire-2002 (NOSQ-2002).18 19 These modifications were necessary since the questions had to be in accordance with the specific work environment of the healthcare workers. Below, we describe, per question, whether we modified the specific question and, if so, how we modified the question.
First, we used original question E8 from the NOSQ-2002, without modification, as a measure for the frequency of hand washing per day: ‘How many times a day do you wash your hands during a usual working day? (1: 0–5 times; 2: 6–10 times; 3: 11–20 times; 4: more than 20 times).’
Second, we measured the frequency of disinfectant use. As the NOSQ-2002 did not include a question for this behaviour, we constructed a new question based on question E8 to ask about the frequency of using disinfectant: ‘How many times a day do you use disinfectant during a usual working day? (1: 0–5 times; 2: 6–10 times; 3: 11–20 times; 4: more than 20 times).’
Third, we modified question E1 of the NOSQ-2002 to measure the average duration of wearing gloves per day. The original question consists of two questions. We constructed a single question out of the two original questions: ‘How many hours do you wear gloves during a usual working day?’
Fourth, we constructed four questions to measure the use of moisturisers, body lotion, wearing jewellery and cotton under gloves. We based these questions on question E1 of the NOSQ-2002. An example of one of these newly constructed questions is: ‘Do you use cotton under gloves during your work? (0: no, never; 1: yes, once in a while; 2: yes, daily).’ Due to the distribution of the answers, we decided to dichotomise the following questions: body lotion and wearing jewellery (0: yes daily/yes, once in a while; 1; no, never) and cotton under gloves (0: no, never; 1: yes, daily/yes, once in while).
Fifth, we measured exposure to wet work by means of the original question E5 from the NOSQ-2002 (‘What are you doing or handling in your work at present?’). However, we changed the term ‘wet work’ into ‘Activities where your hands become wet or moist’. We also added an answer category (‘never’), creating the following answer categories: 1: never; 2: less than ½ h; 3: ½ – 2 h; 4: more than 2 h.
All the questions, except the question on wet work, were assessed every 3 months. The question on exposure to wet work was measured at baseline and after 6 months only.
Compliance measure
To be able to determine compliance to the NVAB guideline, we constructed a compliance measure. We based this measure on the recommendations of the NVAB guideline and the cut-off points mentioned in this guideline.7 We created a sum score, ranging from 0 to 5, in which a respondent received one point for each of the following behaviours: (1) performing wet work for less than 2 h a day; (2) washing the hands less than 20 times a day; (3) not using body lotion; (4) not wearing jewellery during work; and (5) using a moisturiser at least six times a day. This score was created for baseline and for the 6-month mark. For the other behavioural determinants related to the NVAB guideline, such as the use of cotton under gloves and the use of disinfectant, no cut-off points were given in the guideline and therefore they were not included in the compliance measure.
Behavioural determinants
Attitude, social influence, self-efficacy and intention of the ASE model were assessed at baseline and after 6 months. The questions were based on two other studies using this model20 21 and were measured on a 5-point Likert scale. Each determinant was measured by two questions (1: totally disagree; 5: totally agree). We calculated the mean of the two questions, thereby creating a continuous score ranging from 1.0 to 5.0. The Cronbach's α for social influence, self-efficacy and intention were between 0.71 and 0.79. For attitude, the Cronbach's α was too low (0.37) to create one scale. Therefore, the two questions for attitude were analysed separately. One question asked if the respondent considered it important to protect her/his hands during work. The other question asked if the respondent was content with the possibilities he/she had at work to protect his/her hands. Both questions were dichotomised (0: (totally) disagree/neutral; 1: (totally) agree) because of the distribution of the answers to the questions.
Knowledge and awareness
The questionnaire incorporated seven questions on knowledge concerning the recommendations of the prevention of hand eczema. Every participant received 1 point for each correct answer to a question, creating a continuous scale ranging from 0 to 7. An example of a question was: ‘If you wear gloves for longer than 10 min, you should also wear cotton under gloves (yes/no)’.
One question was used to assess awareness. Awareness was operationalised as whether the healthcare workers talked with their colleagues about hand eczema. Awareness was measured by means of a 4-point Likert scale. This question was dichotomised due to the distribution of the answers (0: (totally) disagree; 1: (totally) agree). Knowledge and awareness were assessed at baseline and after 6 months.
Information
We determined whether the healthcare workers received information on the prevention of hand eczema by one dichotomous question. This question was present in the baseline questionnaire and the questionnaire at 6 months.
Covariates
At baseline we assessed age (years), gender (male/female), education level, number of working hours per week, having patient-related tasks (yes/no), psychosocial work characteristics and (symptoms of) hand eczema. Low or middle education was operationalised as: primary school, middle education, basic vocational education, secondary vocational education and high-school degree. Higher education was operationalised as: higher vocational education or university degree.
Psychosocial work characteristics were measured by means of a Dutch version of Karasek's Job Content Questionnaire containing the following constructs: decision authority and coworker support.22 For each construct, we calculated the mean scores of the questions belonging to that construct.
Further, hand eczema was measured using questions D1 (‘Have you ever had hand eczema?’), D2 (‘Have you ever had eczema on your wrists or forearms?’) and D5 (‘When did you last have eczema on your hands, wrists and forearms?’ (I have it just now; not just now, but within the past 3 months; between 3–12 months ago; more than 12 months ago)) from the NOSQ-2002.18 19 Hand eczema at baseline was defined as having hand eczema in the past 3 months.
To assess symptoms related to hand eczema we included a questionnaire from NVAB about the occurrence of specific symptoms related to hand eczema in the past 3 months:7 ‘Did you have one of the following complaints on your hands or fingers in the past 3 months?’ The questionnaire contained the following symptoms: vesicles on palms, back of hands or side of fingers (yes/no); red and swollen hands or fingers (yes/no); red papules on hands or fingers (yes/no); scaling on hands or fingers (yes/no); itchy hands or fingers (yes/no); hands or fingers with fissures (yes/no). We defined the presence of hand eczema symptoms as having at least one symptom related to hand eczema in the past 3 months.
Statistical analyses
Linear and logistic multilevel analyses were performed to evaluate the effects of the multifaceted implementation strategy. Due to the nature and the distribution, the ordinal outcome variables were analysed with linear multilevel analyses. Since these variables were normally distributed, we consider this as a valid method.
The dependent (outcome) variables related to behaviour were: washing hands, use of disinfectant, wet work, use of moisturiser, wearing gloves, use of body lotion, wearing jewellery, wearing cotton under gloves and compliance to the guideline. The dependent variables related to behavioural determinants were: attitude, social influence, self-efficacy and intention. Other dependent variables were: knowledge, awareness and receiving information. The independent (explanatory) variable was the division of the participants in the intervention or the control group (reference category: control group).
All analyses were adjusted for the baseline values of the particular outcome variable. For the outcome variables measured at 3 and 6 months, we used a four level structure (repeated measures; worker; department; hospital), while for the outcome variables measured only at 6 months a three level structure was used (worker; department; hospital).
For each outcome measure, both crude and adjusted analyses were performed. In the adjusted analyses, all covariates were added to the model.
The outcome measure, ‘wearing gloves’ (hours/day), was analysed only for the subgroup of participants who performed wet work at baseline. This was necessary as the recommendation for gloves is twofold: wear gloves when performing wet work, but do not wear gloves when performing dry work.
In this study, we considered a p value lower than 0.05 as statistically significant. All multilevel analyses were performed with MLwiN 2.18 and the other analyses in IBM SPSS Statistics V.20.0.
Results
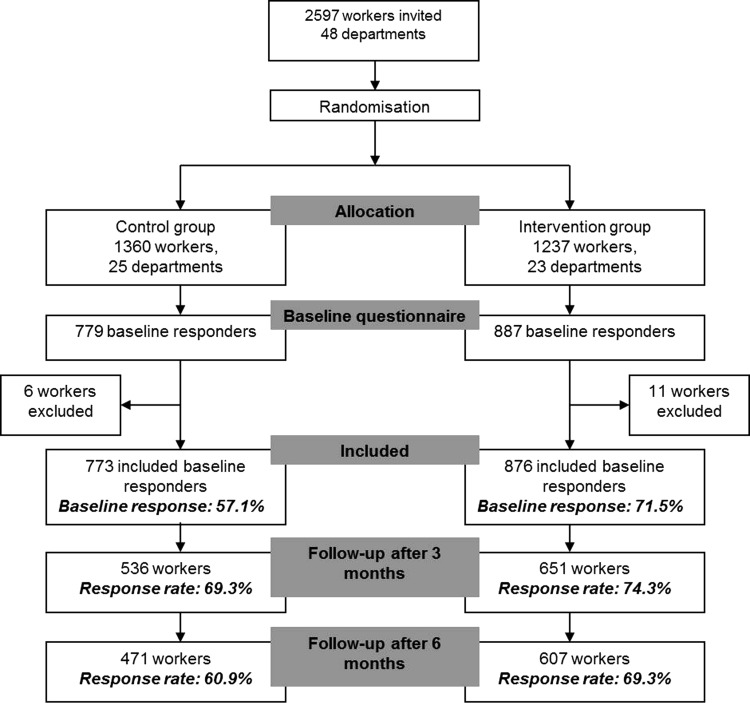
Figure 1 presents the flow of participants during this trial. We invited 2597 healthcare workers to participate in the study; of those invited, 1666 responded to the questionnaire (64.2%). Of the 1666 respondents, we excluded 17 participants: seven because they worked less than 8 h a week and 10 because they did not handle irritants. In total, we included 1649 participants, who received the follow-up questionnaires. A total of 1187 participants responded to the second questionnaire (72.0%) 3 months after baseline and 1078 responded to the third questionnaire 6 months after baseline (65.4%).
Figure 1.
Flow chart of participants during the phases of the trial.
At the follow-up measurements there was a non-response of 28%–35%. The non-responders at 6 months had a lower education level, were 1.5 years younger and worked 1 year shorter at their current job compared with the baseline values.
Table 1 shows the baseline characteristics for the control and intervention groups, table 2 shows descriptive information of the outcome measures, and table 3 shows the effects of the intervention.
Table 1 .
Baseline characteristics
| Variable | Total (n) | Control group (n=773) | Intervention group (n=876) |
|---|---|---|---|
| Female, n (%) | 1641 | 603 (78.3) | 683 (78.4) |
| Education*, n (%) | 1640 | ||
| Low/middle | 372 (48.3) | 371 (42.6) | |
| High | 398 (51.7) | 499 (57.4) | |
| Patient-related task, n (%) | 1641 | 626 (81.2) | 604 (69.4) |
| Hand eczema at baseline, n (%) | 1649 | 80 (10.3) | 64 (7.3) |
| Symptoms related to hand eczema at baseline, n (%) | 1635 | 359 (46.7) | 361 (41.6) |
| Age, mean (SD) | 1635 | 40.8 (11.3) | 40.7 (11.5) |
| Working hours per week, mean (SD) | 1636 | 30.2 (8.8) | 29.8 (8.1) |
| Colleague support, mean (SD) | 1600 | 3.1 (0.4) | 3.1 (0.4) |
| Decision authority, mean (SD) | 1605 | 2.8 (0.5) | 2.8 (0.4) |
*Low/middle education=primary school, middle education, basic vocational education, secondary vocational education, high-school degree; high education=higher vocational education or university degree.
Table 2 .
Descriptive statistics for the outcome measures: barriers for implementation, behavioural determinants and behaviour
| Variable | Scale | Baseline | 3 months | 6 months | |||
|---|---|---|---|---|---|---|---|
| Control (n=773) | Intervention (n=876) | Control (n=536) | Intervention (n=651) | Control (n=471) | Intervention (n=607) | ||
| Barriers for implementation | |||||||
| Awareness ((totally) agree), n (%) | – | 91 (12.2) | 98 (11.5) | – | – | 48 (12.5) | 127 (27.6) |
| Receiving information (yes), n (%) | – | 183 (24.5) | 262 (30.6) | – | – | 152 (39.6) | 353 (76.7) |
| Knowledge, mean (SD) | 0–7 | 5.0 (1.2) | 5.1 (1.2) | – | – | 5.3 (1.3) | 6.2 (1.0) |
| Behavioural determinants | |||||||
| Attitude: Important to protect hands ((totally) agree), n (%) | – | 691 (90.9) | 804 (92.9) | – | – | 351 (90.9) | 426 (92.0) |
| Attitude: Content with protective measures ((totally) agree), n (%) | – | 494 (65.2) | 595 (68.8) | – | – | 283 (73.5) | 358 (77.3) |
| Social influence, mean (SD) | 1.0–5.0 | 2.5 (1.0) | 2.5 (1.0) | – | – | 2.5 (1.0) | 2.5 (0.9) |
| Self-efficacy, mean (SD) | 1.0–5.0 | 3.5 (0.9) | 3.5 (0.9) | – | – | 3.6 (0.9) | 3.7 (0.8) |
| Intention, mean (SD) | 1.0–5.0 | 3.9 (0.8) | 3.9 (0.8) | – | – | 3.9 (0.9) | 4.0 (0.7) |
| Behaviour | |||||||
| Washing hands, mean (SD) | 1–4 | 2.5 (1.0) | 2.3 (1.0) | 2.4 (0.9) | 1.9 (0.8) | 2.5 (0.9) | 2.0 (0.9) |
| Use of disinfectant, mean (SD) | 1–4 | 2.6 (1.1) | 2.7 (1.1) | 2.6 (1.1) | 2.6 (1.1) | 2.6 (1.1) | 2.7 (1.1) |
| Wet work, mean (SD) | 1–4 | 2.8 (0.9) | 2.6 (0.9) | – | – | 2.8 (0.8) | 2.6 (0.8) |
| Use of moisturiser, mean (SD) | 0–2 | 0.9 (0.7) | 0.9 (0.7) | 0.8 (0.7) | 1.0 (0.7) | 0.9 (0.7) | 1.1 (0.7) |
| Wearing gloves (hours/day), mean (SD) | – | 2.3 (1.9) | 2.2 (1.8) | 2.2 (1.7) | 1.9 (1.6) | 2.3 (1.8) | 2.0 (1.7) |
| Use of body lotion (no, never), n (%) | – | 636 (85.8) | 765 (89.8) | 489 (92.1) | 607 (94.0) | 406 (88.3) | 555 (93.4) |
| Wearing jewellery (no, never), n (%) | – | 526 (85.8) | 706 (83.7) | 480 (90.4) | 551 (85.3) | 420 (91.5) | 503 (84.7) |
| Wearing cotton under gloves (once in a while/daily), n (%) | – | 19 (2.6) | 16 (1.9) | 10 (1.9) | 13 (2.0) | 14 (3.0) | 53 (8.8) |
| Compliance to guideline, mean (SD) | 0–5 | 3.4 (0.8) | 3.4 (0.7) | – | – | 3.5 (0.7) | 3.6 (0.6) |
Table 3.
Intervention effects after 12 months of follow-up for barriers for implementation, behavioural determinants and behaviour in the intervention group compared with the control group (reference group)
| Crude* | Adjusted† | |
|---|---|---|
| Outcome variables | B/OR (95% CI) | B/OR (95% CI) |
| Barriers for implementation | ||
| Awareness ((totally) agree) (OR, 95% CI) | 5.43 (2.96 to 9.97) | 6.30 (3.41 to 11.63) |
| Knowledge (B, 95% CI) | 0.72 (0.49 to 0.96) | 0.74 (0.54 to 0.95) |
| Receiving information (yes) (OR, 95% CI) | 9.20 (5.31 to 15.92) | 9.81 (5.60 to 17.18) |
| Behavioural determinants | ||
| Attitude: Important to protect hands ((totally) agree) (OR, 95% CI) | 1.08 (0.57 to 2.07) | 1.12 (0.57 to 2.22) |
| Attitude: Content with protective measures ((totally) agree) (OR, 95% CI) | 1.37 (0.85 to 2.20) | 1.37 (0.84 to 2.26) |
| Social influence (B, 95% CI) | 0.02 (−0.13 to 0.17) | 0.03 (−0.14 to 0.19) |
| Self-efficacy (B, 95% CI) | 0.03 (−0.08 to 0.15) | 0.04 (−0.07 to 0.15) |
| Intention (B, 95% CI) | 0.03 (−0.10 to 0.16) | 0.02 (−0.11 to 0.15) |
| Behaviour | ||
| Washing hands (B, 95% CI) | −0.41 (−0.52 to −0.29) | −0.40 (−0.51 to −0.29) |
| Wet work (B, 95% CI) | −0.07 (−0.19 to 0.05) | −0.08 (−0.18 to 0.03) |
| Use of moisturiser (B, 95% CI) | 0.27 (0.18 to 0.37) | 0.29 (0.20 to 0.38) |
| Use of disinfectant (B, 95% CI) | 0.04 (−0.09 to 0.17) | 0.05 (−0.06 to 0.16) |
| Wearing gloves (B, 95% CI) | −0.21 (−0.56 to 0.15) | −0.22 (−0.60 to 0.15) |
| Use of body lotion (no, never) (OR, 95% CI) | 1.21 (0.72 to 2.01) | 1.07 (0.64 to 1.79) |
| Wearing jewellery (no, never) (OR, 95% CI) | 1.06 (0.55 to 2.02) | 1.03 (0.54 to 1.97) |
| Wearing cotton under gloves (once in a while/daily) (OR, 95% CI) | 3.68 (1.97 to 6.88) | 3.94 (2.04 to 7.60) |
| Compliance to guideline (B, 95% CI) | 0.15 (0.03 to 0.28) | 0.14 (0.02 to 0.26) |
*Adjusted for the baseline value of the particular outcome variable.
†Adjusted for baseline values of: age, gender, education level, number of working hours per week, having patient-related tasks, decision authority, coworker support, symptoms of hand eczema and hand eczema. B, beta.
Barriers for implementation
At baseline, 11.5% of the participants in the intervention and 12.2% of the control group agreed that they talked with colleagues about hand eczema (awareness), and 24.5% (control) to 30.6% (intervention) indicated that they received information on hand eczema (see table 2). The baseline values for knowledge were quite high: 5.0 (control) to 5.1 (intervention) on a scale from 0 to 7. After 6 months, the intervention group was 6.30 times more likely (95% CI 3.41 to 11.63) than the control group to agree that they talked about hand eczema with their colleagues (awareness), and the intervention group was 9.81 times more likely (95% CI 5.60 to 17.18) to report that they received information on hand eczema compared with the control group (table 3). In addition, after 6 months the intervention group scored 0.74 points higher (95% CI 0.54 to 0.95) on knowledge compared with the control group. All these effects were statistically significant.
Behavioural determinants
The baseline values for attitude (important to protecting the hands), self-efficacy and intention were already high at baseline for both the intervention and the control groups (table 2). No statistically significant intervention effects were found for the behavioural determinants from the ASE model (table 3).
Behaviour
Washing hands, the use of disinfectant, wet work and using moisturisers had baseline values around or a bit above average on their scale, in both the intervention and control groups. Gloves were used more than 2 h a day in both groups. Only a small percentage of the control and intervention groups used cotton under gloves at baseline. The majority of workers in both groups indicated that they never used body lotion and never wore jewellery at work (see table 2).
The intervention group reported a lower frequency of hand washing (B −0.40; 95% −0.51; −0.29), more frequent use of a moisturiser (B 0.29; 95% CI 0.20 to 0.38) and they scored 0.14 points higher on the compliance measure (95% CI 0.02 to 0.26) after 6 months compared with the control group (table 3). In addition, the intervention group was 3.94 times more likely (95% CI 2.04 to 7.60) to report wearing cotton under gloves after 6 months compared with the control group. All these effects were statistically significant. No statistically significant effects were found for the other behaviours (use of disinfectant, wet work, wearing gloves, use of body lotion and wearing jewellery).
Discussion
The aim of the present paper was to evaluate a multifaceted implementation strategy for the prevention of hand eczema on several outcome measures related to behaviour and barriers for implementation. The strategy showed statistically significant effects for behaviour (washing hands, use of moisturiser, cotton under gloves and compliance to the NVAB guideline), knowledge on (the prevention of) hand eczema, awareness and receiving information. The strategy, however, had no effect on the behavioural determinants and the behavioural outcome measures: use of disinfectant, wet work, wearing gloves, use of body lotion and wearing jewellery.
Interpretation of the findings
A surprising finding of our study was that the intervention was effective for behaviour, but not for the behavioural determinants. This could be explained by the finding that the intention to perform the behaviour was already high at baseline. The reason why workers had not already changed their behaviour could be explained by barriers that stand between intention and behaviour. It is therefore necessary to identify these barriers and find ways to overcome them.23 This was partly demonstrated in the present study by the finding of statistically significant effects for two barriers for implementation (knowledge and awareness), as a result of the implementation strategy. Fleuren et al15 defined several barriers and facilitators for implementation. We targeted each component of our strategy to at least one of these barriers or facilitators,9 as will be discussed below.
First, the education session was added because Grol argued in his overview study on implementation strategies24 that educational strategies improve knowledge and skills. Our education session was targeted at enhancing the knowledge, awareness, attitude and skills (eg, self-efficacy) of the healthcare workers, of which only attitude and self-efficacy did not show an effect.
Second, the participatory working groups were incorporated in the strategy to reduce barriers for implementation. This approach has shown to be a promising tool for implementation.10 A study among slaughterhouse workers—that aimed to reduce hand eczema—also used a participatory approach combined with education25 and they too accomplished a behavioural change in favour of the use of preventive measures. The power of this method, which is derived from participatory ergonomics, is that workers are involved in the planning and controlling of their own working activities and have the power to influence these processes.26 In our study, the working group gained support for the implementation of the recommendations at their departments and they warranted that the most important barriers for the specific departments were tackled.
The role models in our study were aimed at improving social influence. However, there was no effect on social influence. The reason for this finding, despite the fact that the baseline value was quite low, can be twofold. First, the role models perhaps did not perform their tasks. On the other hand, the role models might have influenced other factors than social influence.
Our multifaceted implementation strategy focused on four important recommendations: that is, the use of disinfectant instead of water and soap; the use of moisturiser; the use of gloves while performing wet work; and the use of cotton under gloves while wearing gloves. Of these four recommendations, an effect was accomplished for three of them including on the overall compliance to the recommendations. In general, we could therefore conclude that our strategy was effective in implementing the NVAB recommendations. However, not every aspect of behaviour was influenced by the implementation strategy. There could be multiple reasons for this finding. First, the reason why there was no effect on the use of gloves in workers performing wet work could be due to the mixed message of this recommendation. On the one hand, healthcare workers were advised to wear gloves when performing wet work; on the other, they were instructed to wear gloves no longer than necessary. For reducing wet work, we did not focus on diminishing wet work, rather we focused on diminishing exposure to wet work by means of wearing gloves. For the measurement of the use of disinfectant, it might have been difficult to measure an increase in its use as the question was categorical with ‘more than 20 times a day’ as the highest category. Participants who were in the highest category at baseline might have used more disinfectant after 6 months, but due to the answer categories this increase could not be detected. Further, the baseline values for not using body lotion and not wearing jewellery (desirable behaviour according to the recommendations) were already high at baseline, leaving little room for improvement.
For hand washing and using a moisturiser, the effects were presented as β's. One might wonder how relevant these effects are as they seem rather small. However, the answer categories for, for instance, hand washing were very broad. An effect of 1 point for hand washing indicates a shift from one category to the next, for instance, a shift from washing the hands 11–20 times a day to 6–10 times a day.
Strengths and limitations
This is the first RCT that evaluated a strategy to implement recommendations for the prevention of hand eczema in the Netherlands and that also looked into behavioural determinants. To our knowledge, there are no other studies on the primary prevention of hand eczema that studied these determinants. Another strength of our study is the randomisation at the department level, which minimised the risk for contamination between workers between the intervention and control groups.
A limitation of our study is the use of self-reported questionnaires to measure behaviour. This could have led to an underestimation—or more probably—an overestimation of the effect as the participants were all aware of the goal of the study. Further, at every follow-up measurement there was a non-response of 20%. The baseline values of the non-responders at 6 months were different from the baseline values of the total population for education, age and working years. These differences were considered to be small, but they could nonetheless have biased our results. Other research also showed that people with a lower education level tend to respond less to questionnaires compared with people with a higher educational level.27 This might introduce bias as participants with a lower educational level might also respond differently to our implementation strategy compared with participants with a higher educational level. A final limitation relates to the use of the ASE model. We detected no effects on these determinants. However, we used only two questions per determinant. It is questionable whether this was sufficient.
Implications for practice and research
As the multifaceted strategy seems to be effective for behaviour, the strategy can be used in practice to alter healthcare workers' behaviour towards a more preventive behaviour in relation to hand eczema. However, there are some aspects that need further research.
We would recommend studying the function of role models more thoroughly. Role models have been shown to be very important in a hospital setting, for instance, for the compliance to hand hygiene protocols.28 However, many of these role models were role models by nature. In our study, we appointed role model tasks to healthcare workers without knowledge about whether their colleagues considered them to be a role model before the study started. It would therefore be interesting to study whether appointed role models can have the same effect as natural role models. Also, the training of the role models might not have been sufficient enough to establish working group members as role models within their department. More intensive training of the role models might therefore enhance their influence. Another point for research would be to investigate whether each component of the multifaceted implementation strategy contributed to the implementation of the NVAB guideline. By selecting the most effective components, the components of the strategy could be reduced and as a result it would be less time consuming and less expensive.
Conclusions
The multifaceted implementation strategy showed an effect on knowledge, awareness and behaviour related to the prevention of hand eczema—but not on the behavioural determinants. As behaviour was the most important outcome measure related to the implementation of the recommendations for hand eczema, our strategy can be used in healthcare settings to enhance the implementation of these recommendations.
Footnotes
Contributors: All authors contributed to the writing of this paper. They all approved the final manuscript. EWCM is the principle researcher and is responsible for the data collection. CRLB coordinated the study. JWRT supervised the statistical analyses. CRLB, JWRT, PJC, JWJG, FHWJ and JRA supervised the study.
Funding: This study is supported by a grant from The Netherlands Organisation for Health Research and Development (ZONMW).
Competing interests: None.
Ethics approval: Medical Ethics Committee of the VU University Medical Center.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.van der Meer EWC, Boot CRL, van der Gulden JWJ, et al. Hand eczema among health care professionals in the Netherlands: prevalence, absenteeism and presenteeism. Contact Dermatitis 2013;69:164–71 [DOI] [PubMed] [Google Scholar]
- 2.Diepgen TL. Occupational skin-disease data in Europe. Int Arch Occup Environ Health 2003;76:331–8 [DOI] [PubMed] [Google Scholar]
- 3.Nicholson PJ, Llewellyn D, English JS. Evidence-based guidelines for the prevention, identification and management of occupational contact dermatitis and urticaria. Contact Dermatitis 2010;63:177–86 [DOI] [PubMed] [Google Scholar]
- 4.Ramsing DW, Agner T. Effect of glove occlusion on human skin (II). Long-term experimental exposure. Contact Dermatitis 1996;34:258–62 [DOI] [PubMed] [Google Scholar]
- 5.Thyssen JP, Johansen JD, Linneberg A, et al. The epidemiology of hand eczema in the general population – prevalence and main findings. Contact Dermatitis 2010;62:75–87 [DOI] [PubMed] [Google Scholar]
- 6.Agner T, Held E. Skin protection programmes. Contact Dermatitis 2002;46:253–6 [DOI] [PubMed] [Google Scholar]
- 7.Jungbauer FHW, Piebenga WP, ten Berge EE, et al. NVAB-richtlijn: Preventie Contacteczeem [NVAB-guideline: Prevention of Contact Dermatitis], 2006
- 8.Grol R. Implementation of evidence and guidelines in clinical practice: a new field of research? Int J Qual Health Care 2000;12:455–6 [DOI] [PubMed] [Google Scholar]
- 9.van der Meer EWC, Boot CRL, Jungbauer FHW, et al. Hands4U: A multifaceted strategy to implement guideline-based recommendations to prevent hand eczema in health care workers: design of a randomised controlled trial and (cost) effectiveness evaluation. BMC Public Health 2011;11:669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van der Molen HF, Sluiter JK, Hulshof CTJ, et al. Effectiveness of measures and implementation strategies in reducing physical work demands due to manual handling at work. Scand J Work Environ Health 2005;31:75–87 [PubMed] [Google Scholar]
- 11.de Vries H, Dijkstra M, Kuhlman P. Self-efficacy: the third factor besides attitude and subjective norm as a predictor of behavioural intentions. Health Educ Res 1988;3:273–82 [Google Scholar]
- 12.Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall, 1986 [Google Scholar]
- 13.Fishbein M, Azjen I. Formation of intentions Belief, attitude, intention, and behavior: an introduction to theory and research. Addison-Wesley Publishing Company, 1975 [Google Scholar]
- 14.Fishbein M, Azjen I. Prediction of behaviour Belief, attitude, intention, and behaviour: an introduction to theory and research. Addison-Wesley Publishing Company, 1975 [Google Scholar]
- 15.Fleuren M, Wiefferink K, Paulussen T. Determinants of innovation within health care organizations. Int J Qual Health Care 2004;16:107–23 [DOI] [PubMed] [Google Scholar]
- 16.Grol R, Wensing M. What drives change? Barriers to and incentives for achieving evidence-based practice. Med J Aust 2004;180:57–60 [DOI] [PubMed] [Google Scholar]
- 17.van der Meer EWC, Boot CRL, Jungbauer FHW, et al. Implementation of recommendations for hand eczema through a multifaceted strategy. A process evaluation among health care workers. Acta Derm Venereol 2014, [Accepted for publication]. [DOI] [PubMed] [Google Scholar]
- 18.Flyvholm MA, Susitaival P, Meding B. Nordic occupational skin questionnaire—NOSQ-2002 Nordiq questionnaire for surveying work related skin diseases on hand and forearms and relevant exposures. Copenhagen: Nordic Council of Ministers, 2002: 1–186 [Google Scholar]
- 19.Susitaival P, Flyvholm MA, Meding B. Nordic occupational skin questionnaire (NOSQ-2002): a new tool for surveying occupational skin diseases and exposure. Contact Dermatitis 2003;49:70–6 [DOI] [PubMed] [Google Scholar]
- 20.Driessen MT, Anema JR, Proper KI, et al. Stay@Work: Participatory Ergonomics to prevent low back and neck pain among workers: design of a randomised controlled trial to evaluate the (cost-) effectiveness. BMC Musculoskelet Disord 2008;9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vyth EL, Steenhuis IHM, Heymans MW, et al. Influence of placement of a nutrition logo on cafeteria menu items on lunchtime food Choices at Dutch work sites. J Am Diet Assoc 2011;111:131–6 [DOI] [PubMed] [Google Scholar]
- 22.Karasek R, Brisson C, Kawakami N, et al. The job content questionnaire: an instrument for international comparative assessments for psychosocial job characteristics. Journal of Occupational Psychology 1998:322–55 [DOI] [PubMed] [Google Scholar]
- 23.Erasmus V, Kuperus MN, Richardus JH, et al. Improving hand hygiene behaviour in nurses using action planning: a pilot study in the intensive care unit and surgical ward. J Hosp Infect 2010;76:161–4 [DOI] [PubMed] [Google Scholar]
- 24.Grol R. Implementing guidelines in general practice care. Quality in Health Care 1992;1:184–91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Flyvholm MA, Mygind K, Sell L, et al. A randomised controlled intervention study on prevention of work related skin problems among gut cleaners in swine slaughterhouses. Occup Environ Med 2005;62:642–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wilson JR, Corlett EN. Evaluation of human work: a practical ergonomics methodology. London: Taylor and Francis, 1995: 1071–96 [Google Scholar]
- 27.Ekman A, Dickman PW, Klint A, et al. Feasibility of using web-based questionnaires in large population-based epidemiological studies. Eur J Epidemiol 2006;21:103–11 [DOI] [PubMed] [Google Scholar]
- 28.Erasmus V, Brouwer W, van Beeck EF, et al. A qualitative exploration of reasons for poor hand hygiene among hospital workers: lack of positive role models and of convincing evidence that hand hygiene prevents cross-infection. Infect Control Hosp Epidemiol 2009;30:415–19 [DOI] [PubMed] [Google Scholar]