Abstract
Background and objectives
Hyperlipidemia is common in patients with CKD. The objective of this study was to evaluate whether measures of plasma lipids and lipoproteins predict progression of kidney disease in patients with CKD.
Design, setting, participants, & measurements
Prospective cohort study in adults (n=3939) with CKD aged 21–74 years recruited between 2003 and 2008 and followed for a median of 4.1 years. At baseline, total cholesterol, triglycerides, very-low-density lipoprotein cholesterol (VLDL-C), LDL cholesterol (LDL-C), HDL cholesterol (HDL-C), apoA-I , apoB, and lipoprotein(a) [Lp(a)] were measured. The outcomes were composite end point of ESRD or 50% decline in eGFR from baseline (rate of change of GFR).
Results
Mean age of the study population was 58.2 years, and the mean GFR was 44.9 ml/min per 1.73 m2; 48% of patients had diabetes. None of the lipid or lipoprotein measures was independently associated with risk of the composite end point or rate of change in GFR. However, there were significant (P=0.01) interactions by level of proteinuria. In participants with proteinuria<0.2 g/d, 1-SD higher LDL-C was associated with a 26% lower risk of the renal end point (hazard ratio [HR], 0.74; 95% confidence interval [95% CI], 0.59 to 0.92; P=0.01), and 1-SD higher total cholesterol was associated with a 23% lower risk of the renal end point (HR, 0.77; 95% CI, 0.62 to 0.96; P=0.02). In participants with proteinuria>0.2 g/d, neither LDL-C (HR, 0.98; 95% CI, 0.98 to 1.05) nor total cholesterol levels were associated with renal outcomes. Treatment with statins was reported in 55% of patients and was differential across lipid categories.
Conclusions
In this large cohort of patients with CKD, total cholesterol, triglycerides, VLDL-C, LDL-C, HDL-C, apoA-I, apoB, and Lp(a) were not independently associated with progression of kidney disease. There was an inverse relationship between LDL-C and total cholesterol levels and kidney disease outcomes in patients with low levels of proteinuria.
Keywords: lipids, chronic kidney disease, progression of chronic renal failure
Introduction
Dyslipidemia is common among patients with CKD (1) and is characterized by elevated plasma triglycerides and VLDL cholesterol (VLDL-C) and reduced HDL cholesterol (HDL-C) concentrations (2). Animal studies have shown development and progression of kidney damage in the setting of hyperlipidemia with increased glomerulosclerosis and tubulointerstitial damage (3–6). In epidemiologic studies, the presence of dyslipidemia was associated with a higher risk of development of incident CKD in the general population (7–9). The association between dyslipidemia and progression of established kidney disease is not consistent in studies of diabetic (10) and nondiabetic (11–15) participants. These inconsistent findings may have resulted from the relatively small number of patients, low event rates, and concurrent lipid-lowering therapy. In addition, analyses of data from large, interventional studies on the effects of lipid-lowering agents have not shown a consistent benefit on progression of kidney disease (16,17). Therefore, the role of dyslipidemia as a predictor or mediator of decline in renal function in patients with CKD is unclear.
The objective of this study was to evaluate whether measures of plasma lipids and lipoproteins predict progression of kidney disease, as defined by rate of change in eGFR, significant declines in eGFR, and development of ESRD in a multicenter cohort of patients with CKD. We hypothesized that baseline lipid and lipoprotein measures are independently associated with kidney disease outcomes.
Materials and Methods
The design, methods, and baseline characteristics of the Chronic Renal Insufficiency Cohort (CRIC) study population have been published (18,19). Briefly, CRIC is a prospective observational study of patients with mild-to-moderate kidney disease that was established by the National Institute of Diabetes and Digestive and Kidney Diseases to examine risk factors for kidney and cardiovascular disease progression in CKD. A total of 3939 participants aged 21–74 years were enrolled from seven clinical centers throughout the United States (Ann Arbor, MI; Baltimore, MD; Chicago, IL; Cleveland, OH; New Orleans, LA; Philadelphia, PA; and Oakland, CA) between June 2003 and September 2008. The CRIC protocol was approved by the local institutional review board at each of the clinical centers, and all participants provided written informed consent. CRIC participants have been followed and seen annually for study visits until death or withdrawal of informed consent.
Inclusion in the CRIC study was based on age-specific eGFRs as follows: eGFR of 20–70 ml/min per 1.73 m2 for patients age 21–44 years, 20–60 ml/min per 1.73 m2 for patients age 45–64 years, and 20–50 ml/min per 1.73 m2 for patients age 65–74 years. Major exclusion criteria were polycystic kidney disease, additional primary renal diseases requiring active immunosuppression, and significant coexisting illnesses likely to affect survival as previously published (18). All participants completed a baseline visit, during which sociodemographic characteristics, medical history, lifestyle behaviors, current medications, and anthropomorphic measurements were recorded. BP measurements were obtained using a standardized protocol and calibrated sphygmomanometers. In addition, plasma and urine samples were collected for measurement of study variables. History of cardiovascular disease (congestive heart failure, myocardial infarction/prior revascularization, peripheral vascular disease) was collected from the medical history questionnaire completed at the baseline visit.
Hypertension was defined as systolic BP≥140 mmHg, diastolic BP≥90 mmHg, or self-reported use of antihypertensive medications. Diabetes was defined as a fasting glucose≥126 mg/dl, random glucose≥200 mg/dl, or use of insulin or other antidiabetic medication. Serum creatinine was measured at the University of Pennsylvania laboratory and standardized to isotope-dilution mass spectrometry reference values (20). The eGFR was calculated using the CRIC equation (21). Plasma lipids and lipoproteins were measured using standard laboratory assays; triglycerides, total cholesterol, and HDL-C were measured by spectrophotometry; VLDL-C and LDL-C were directly measured after separation by ultracentrifugation (β quantification), and apoA-I, apoB, and lipoprotein(a) [Lp(a)] were measured using immunoturbidimetric assays. The blood sample was obtained in a fasting state in 96% of patients. The malnutrition/inflammation complex was defined by body mass index<23 kg/m2, C-reactive protein≥10 mg/L, albumin<3.6 g/dl, or IL-6>3.09 pg/ml (22).
The kidney disease outcomes evaluated in this paper are rate of eGFR decline per year and incidence of 50% decline in eGFR from baseline or development ESRD. Serum creatinine measurements to calculate slope of eGFR over time were obtained at annual visits.
Statistical Analyses
Demographic information and other baseline variables were described using mean±SD or median and interquartile range, when appropriate, for continuous variables and frequency and proportion for categorical variables. The lipid variable distributions across baseline eGFR categories were compared using ANOVA for total cholesterol, LDL-C, HDL-C, apoA-I, and apoB and Wilcoxon rank-sum test for VLDL-C, triglycerides, and Lp(a). Because of their skewed distributions, VLDL-C, triglycerides, and Lp(a) were log transformed in all subsequent analyses.
To identify risk factors for progression of kidney disease, we conducted two sets of analyses: failure time analysis and repeated eGFR analysis. In failure time analysis, Cox proportional hazards models were fit using a composite renal end point of ESRD or 50% decline in eGFR from baseline as the primary end point (23). Patients were censored at the end of the follow-up time period (March 31, 2011), loss to follow-up, or death. We started with the unadjusted analysis showing the association between each of the lipoprotein variables and outcome in terms of hazards ratios (HRs) per 1-SD increase of the variable, followed by the multivariable models adjusting for the following baseline covariates: age, race/ethnicity, sex, systolic and diastolic BP, statin use, diabetes, smoking, 24-hour urine total protein excretion, body mass index, alcohol use, baseline eGFR, and clinical site. Stratified analyses were performed in subgroups defined by baseline diabetic status, statin use, malnutrition/inflammation complex, eGFR, and 24-hour urine total protein excretion level. Formal tests of interaction for each lipoprotein predictor were done by including the two-way interaction terms between the lipoprotein variable and all other covariates in the model. In the analyses of repeated eGFR measures, we estimated the associations between each lipoprotein measure with the slope of eGFR decline over the follow-up period using linear mixed effects models with both random intercept and slope terms (24). Parameter estimates were reported as the slope difference per 1-SD increase of the lipoprotein variable. In the multivariable adjusted model, we adjusted for the same covariates as were in the survival analysis (SAS 9.3; SAS Institute, Cary, NC).
Results
Baseline characteristics of the study population are described in Table 1.The mean age of the study population was 58.2 years; 55% of patients were male and 42% were non-Hispanic black. Most patients (86%) had a history of hypertension, and slightly less than half (48%) were diabetic. Treatment with statins was reported in 55% of patients; in addition, 13% of patients reported use of lipid-lowering therapy other than statins. There were several differences in baseline characteristics between patients in the low and high total cholesterol strata. Patients with low total cholesterol were older; were more likely to be men, be white, and have hypertension, diabetes, or prior cardiovascular disease; to be receiving statins and have a lower GFR and BP; and to be receiving an angiotensin-converting enzyme inhibitor.
Table 1.
Clinical and demographic characteristics of the Chronic Renal Insufficiency Cohort study population stratified by quartiles of baseline total cholesterol
| Characteristic | All (n=3939) | Quartiles of Total Cholesterol at Baseline | P Value for Trend | |||
|---|---|---|---|---|---|---|
| ≤152 mg/dl (n=1003) | >152 to ≤178 mg/dl (n=972) | >178 to ≤209 mg/dl (n=993) | >209 mg/dl (n=958) | |||
| Age (yr) | 58.2±11.0 | 59.4±10.7 | 59.0±10.6 | 57.9±11.1 | 56.3±11.4 | <0.001 |
| Women, n (%) | 1778 (45.1) | 331 (33.0) | 424 (43.6) | 476 (47.9) | 540 (56.4) | <0.001 |
| Race/ethnicity, n (%) | ||||||
| Non-Hispanic black | 1650 (41.9) | 378 (37.7) | 415 (42.7) | 423 (42.6) | 425 (44.4) | 0.02 |
| Non-Hispanic white | 1638 (41.6) | 453 (45.2) | 410 (42.2) | 415 (41.8) | 358 (37.4) | |
| Hispanic | 497 (12.6) | 125 (12.5) | 113 (11.6) | 118 (11.9) | 139 (14.5) | |
| Other | 154 (3.91) | 47 (4.7) | 34 (3.5) | 37 (3.7) | 36 (3.8) | |
| Hypertension, n (%) | 3391 (86.1) | 885 (88.2) | 855 (88) | 834 (84) | 806 (84.1) | 0.001 |
| Diabetes, n (%) | 1908 (48.4) | 601 (59.9) | 500 (51.4) | 409 (41.2) | 394 (41.1) | <0.001 |
| History of myocardial infarction/prior revascularization, n (%) | 862 (21.9) | 332 (33.1) | 228 (23.5) | 162 (16.3) | 137 (14.3) | <0.001 |
| History of congestive heart failure, n (%) | 382 (9.70) | 134 (13.4) | 106 (10.9) | 70 (7) | 68 (7.1) | <0.001 |
| History of peripheral vascular disease, n (%) | 262 (6.65) | 85 (8.5) | 67 (6.9) | 61 (6.1) | 47 (4.9) | 0.001 |
| Current smoker, n (%) | 517 (13.1) | 136 (13.6) | 114 (11.7) | 128 (12.9) | 135 (14.1) | 0.58 |
| Systolic BP (mmHg) | 128.5±22.2 | 127.0±21.62 | 127.2±21.03 | 128.5±22.05 | 131.5±23.79 | <0.001 |
| Diastolic BP (mmHg) | 71.5±12.8 | 69.2±12.55 | 69.5±12.40 | 72.7±12.83 | 74.9±12.62 | <0.001 |
| Body mass index (kg/m2) | 32.1±7.8 | 32.2±7.61 | 32.9±8.52 | 31.6±7.41 | 31.7±7.63 | 0.02 |
| ACE inhibitor or ARB, n (%) | 2689 (68.8) | 736 (73.7) | 714 (74) | 640 (64.8) | 592 (62.6) | <0.001 |
| Statins, n (%) | 2153 (55.0) | 742 (74.3) | 612 (63.4) | 479 (48.5) | 314 (33.2) | <0.001 |
| Lipid-lowering medications other than statins, n (%) | 527 (13.5) | 188 (18.8) | 130 (13.5) | 98 (9.9) | 109 (11.5) | <0.001 |
| eGFR (ml/min per 1.73 m2) | 44.9 (16.8) | 43.4 (16.06) | 44.3 (17.02) | 46.8 (17.11) | 45.2 (17.04) | 0.001 |
| Serum creatinine (mg/dl) | 1.7 (0.6) | 1.79 (0.54) | 1.76 (0.61) | 1.69 (0.57) | 1.73 (0.59) | 0.001 |
| 24-hr urine protein (g/24 hr) | 0.18 (0.07–0.91) | 0.20 (0.08–0.75) | 0.17 (0.07–0.82) | 0.14 (0.07–0.78) | 0.23 (0.07–1.66) | 0.001 |
| Hemoglobin (g/dl) | 12.6±1.8 | 12.4±1.84 | 12.5±1.73 | 12.8±1.76 | 12.8±1.74 | <0.001 |
| Hemoglobin A1c (%) | 6.7±1.6 | 6.7±1.46 | 6.7±1.51 | 6.5±1.53 | 6.7±1.74 | 0.1 |
| Glucose (mg/dl) | 115.4±51.7 | 116.8±53.0 | 114.7±45.2 | 114.7±52.2 | 115.6±55.8 | 0.61 |
| C-reactive protein (mg/L) | 2.57 (1.05–6.51) | 2.40 (0.96–6.24) | 2.63 (1.08–6.42) | 2.53 (1.02–6.47) | 2.69 (1.16–6.77) | 0.03 |
| Serum albumin (g/dl) | 3.9±0.5 | 3.89±0.43 | 3.95±0.42 | 3.96±0.47 | 3.94±0.57 | 0.01 |
| IL-6 (pg/ml) | 1.90 (1.17–3.15) | 2.19 (1.31–3.82) | 1.91 (1.19–3.22) | 1.78 (1.09–2.95) | 1.80 (1.08–2.83) | 0.002 |
| Malnutrition/inflammation (%)a | 1819 (46.6) | 493 (49.5) | 427 (44.3) | 449 (45.5) | 437 (46.1) | 0.2 |
Values expressed with a plus/minus sign are the mean±SD. Values with ranges are the median (interquartile range). ACE, angiotensin-converting enzyme; ARB, angiotensin-receptor blocker.
As defined by body mass index<23 kg/m2, C-reactive protein≥10 mg/L, albumin<3.6 g/dl, or IL-6>3.09 pg/ml.
At baseline, in cross-sectional analyses, low eGFR was associated with lower LDL-C, HDL-C, and Apo A1 and higher VLDL-C and triglycerides and Lp(a) (Table 2).
Table 2.
Lipoproteins stratified by baseline eGFR in the Chronic Renal Insufficiency Cohort study
| Lipoprotein | Overall (n=3939) | eGFR<30 ml/min per 1.73 m2 (n=806) | eGFR 30 to <40 ml/min per 1.73 m2 (n=902) | eGFR 40 to <50 ml/min per 1.73 m2 (n=859) | eGFR 50 to <60 ml/min per 1.73 m2 (n=668) | eGFR≥60 ml/min per 1.73 m2 (n=702) | P Value |
|---|---|---|---|---|---|---|---|
| Total cholesterol (mg/dl) | 183.7±45.6 | 182.9±52.9 | 182.6±44.5 | 183.5±46.2 | 183.2±43.0 | 186.6±39.1 | 0.45 |
| LDL cholesterol (mg/dl) | 102.7±35.6 | 99.1±38.9 | 100.3±34.6 | 102.3±36.2 | 104.6±34.2 | 108.6±32.4 | <0.001 |
| HDL cholesterol (mg/dl) | 47.5±15.5 | 45.2±14.6 | 47.0±15.5 | 47.2±14.9 | 47.9±15.4 | 50.8±16.7 | <0.001 |
| VLDL cholesterol (mg/dl) | 27 (17–42) | 31 (19–47) | 30 (19–43) | 29 (17–43) | 25 (15–39) | 22 (13–35) | <0.001 |
| Triglycerides (mg/dl) | 128.5 (89–186) | 139 (100–205) | 135 (94–196) | 133 (92–193) | 120 (84–177) | 109 (79–156) | <0.001 |
| Lp(a) (mg/dl) | 24.5 (9–59) | 31.3 (12–69) | 26.45 (9–63) | 23.35 (8–64) | 23 (8–53) | 18.3 (7–46) | <0.001 |
| ApoA-I | 136.7±29.6 | 132.4±28.7 | 136.7±30.9 | 136.2±29.3 | 137.1±28.6 | 141.6±29.4 | <0.001 |
| ApoB | 84.2±24.6 | 85.1±28.0 | 83.8±24.0 | 83.9±24.6 | 83.9±23.5 | 84.5±22.3 | 0.82 |
Values expressed with a plus/minus sign are the mean±SD. Values expressed with ranges are the median (interquartile range). Lp(a), lipoprotein(a).
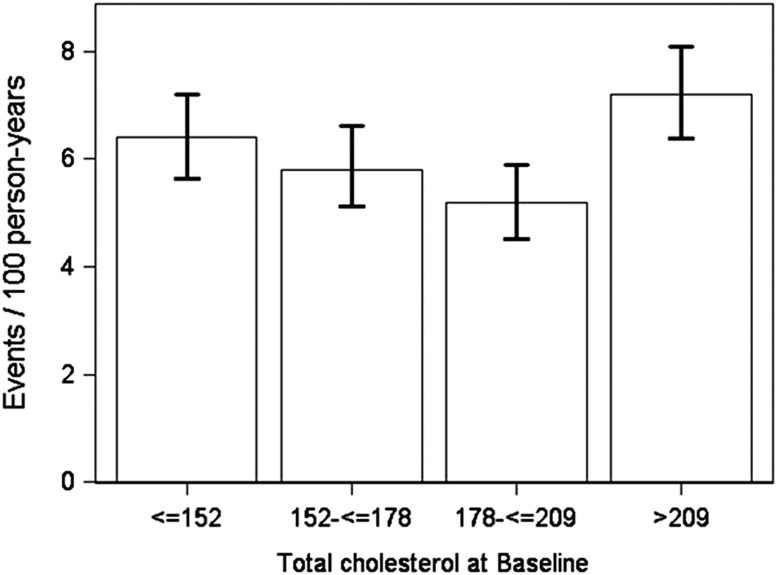
During the median follow-up of 4.1 years, 752 patients (4.7 per 100 patient years) reached ESRD, and 986 patients (6.1 per 100 patient-years) reached the combined end point of ESRD or 50% decline in GFR. The mean rate of change of GFR for the study population was −1.5 ml/min per 1.73 m2/ per year. Figure 1 shows the crude event rates for the combined end point of ESRD or 50% decline in eGFR by quartiles of total cholesterol.
Figure 1.
Crude event rates for ESRD or 50% decline in GFR stratified by quartiles of total cholesterol (mg/dl) at baseline. The error bars delineate the 95% confidence interval.
The associations of lipoproteins and the composite kidney end point (unadjusted and adjusted) are presented in Table 3. Although there was an association in unadjusted models, after adjustment for covariates, total cholesterol, LDL-C, HDL-C, triglycerides, apoA-I, apoB, and Lp(a) levels were not independently predictive of the renal end point. The possibility of a nonlinear relationship between total cholesterol and outcomes was explored by adding a higher-order term in the model; the adjusted HR remained similar (0.95; P=0.23). Additional adjustment for albumin, IL-6, and history of cardiovascular disease did not change the association between lipid variables and outcomes (Supplemental Table 1). Analyses accounting for death as a competing risk also did not change the association between lipid variable and outcomes (Supplemental Table 2).
Table 3.
Associations between baseline lipoproteins and the composite end point of ESRD or 50% decline in GFR in the Chronic Renal Insufficiency Cohort study
| Lipoprotein | Unadjusted | Adjusteda | ||
|---|---|---|---|---|
| Hazard Ratiob (95% CI) | P Value | Hazard Ratiob (95% CI) | P Value | |
| Total cholesterol | 1.15 (1.08 to 1.23) | <0.01 | 1.00 (0.93 to 1.07) | 0.98 |
| LDL cholesterol | 1.01 (0.95 to 1.08) | 0.68 | 0.95 (0.89 to 1.02) | 0.14 |
| HDL cholesterol | 0.87 (0.81 to 0.93) | <0.01 | 1.00 (0.92 to 1.08) | 0.95 |
| VLDL cholesterolc | 1.33 (1.25 to 1.42) | <0.01 | 1.06 (0.99 to 1.14) | 0.11 |
| Triglyceridesc | 1.26 (1.19 to 1.34) | <0.01 | 1.05 (0.97 to 1.12) | 0.21 |
| Lp(a)c | 1.26 (1.18 to 1.35) | <0.01 | 1.07 (0.99 to 1.15) | 0.09 |
| ApoA-I | 0.93 (0.87 to 1.00) | 0.04 | 1.01 (0.93 to 1.10) | 0.75 |
| ApoB | 1.23 (1.15 to 1.30) | <0.01 | 1.00 (0.94 to 1.07) | 0.95 |
Lp(a), lipoprotein(a).
Model adjusted for age, race, sex, diabetes, BP, statin use at baseline, smoking, 24-hour urine protein excretion, body mass index, clinical center, alcohol use, and baseline eGFR.
Hazard ratios reported as per 1-SD change in independent variable.
Values were log transformed.
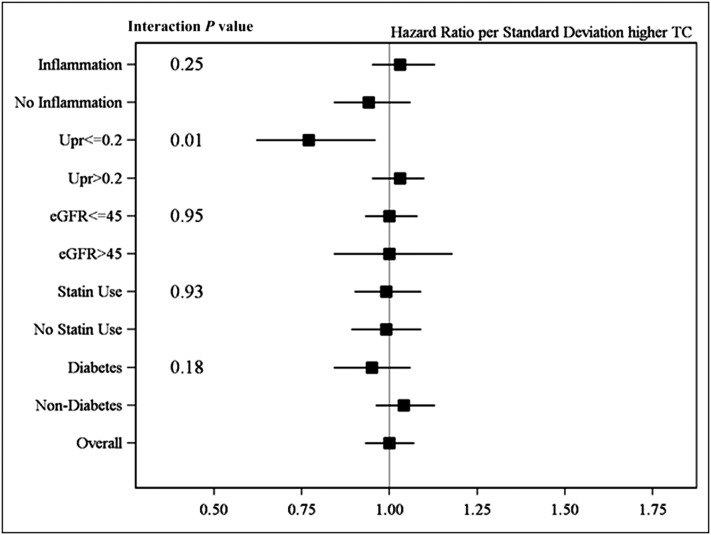
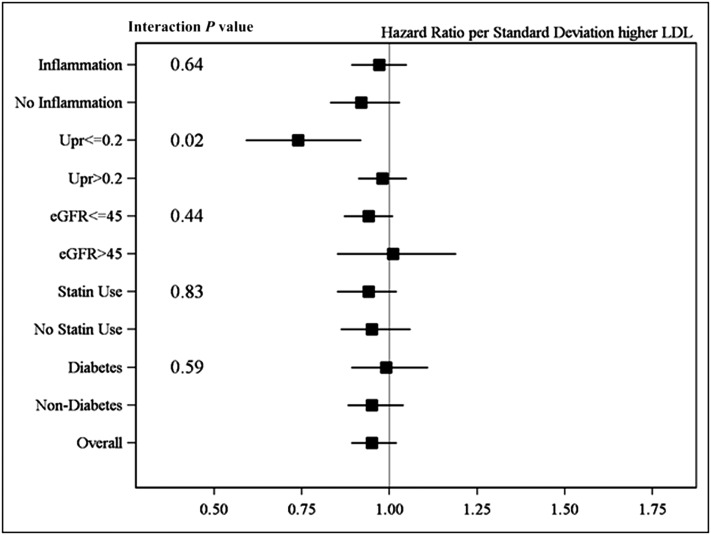
Subgroup analyses examined the relationships of lipoprotein measures and renal outcomes stratified by proteinuria, diabetes, statin use, presence of malnutrition/inflammation, and eGFR. The association between LDL and renal outcomes was significantly different according to level of proteinuria (interaction P=0.01). In participants with low levels of proteinuria (<0.2 g total protein/d; n=1916), a 1-SD higher LDL-C was associated with a 26% lower risk of the composite renal end point (HR, 0.74; 95% confidence interval [95% CI], 0.59 to 0.92; P=0.01) (Figure 2). In participants with higher levels of proteinuria (>0.2 g total protein/d), there was no significant association (HR, 0.96; P=0.26). Similarly, the association between total cholesterol and renal outcomes differed according to level of proteinuria (P for interaction =0.01) (Figure 3). One SD higher total cholesterol was associated with a 23% lower risk of the composite renal end point (HR, 0.77; 95% CI, 0.62 to 0.96; P=0.02) in participants with proteinuria<0.2 g/d, whereas there was no significant association between total cholesterol and outcomes in patients with proteinuria>0.2 g/d. The associations between all lipoproteins and renal outcomes were consistent across subgroups of diabetes, statin use, presence of malnutrition/inflammation, and eGFR (Figures 2 and 3, Supplemental Figures 1–6).
Figure 2.
Hazards ratios for renal outcome (ESRD or 50% decline in GFR) per 1-SD increase in total cholesterol (TC) in subgroups of inflammation/malnutrition, proteinuria, eGFR, statin use, and diabetes. Model adjusted for age, race, sex, diabetes, BP, statin use at baseline, smoking, 24-hour urine protein (UPr) excretion, body mass index, clinical center, alcohol use, and baseline eGFR. The error bars delineate the 95% confidence interval.
Figure 3.
Hazard ratios for renal outcome (ESRD or 50% decline in GFR) per 1-SD increase in LDL cholesterol in subgroups of inflammation/malnutrition, proteinuria, eGFR, statin use, and diabetes. Model adjusted for age, race, sex, diabetes, BP, statin use at baseline, smoking, 24-hour urine protein (UPr) excretion, body mass index, clinical center, alcohol use, baseline eGFR. The error bars delineate the 95% confidence interval.
To explore the unexpected association between high LDL-C and lower risk of renal outcomes in patients with lower levels of proteinuria, we stratified baseline characteristics by level of proteinuria (Supplemental Table 3). Baseline characteristics significantly differed betweenin participants with low (<0.2 g/d) and those with high (>0.2 g/d) levels of proteinuria. Given the higher use of statins in the low proteinuria group, analyses were further stratified by the use of statins and level of proteinuria. In participants with proteinuria<0.2 g/d who were receiving statin therapy, higher LDL-C (HR, 0.59; 95% CI, 0.43 to 0.82) and total cholesterol (HR, 0.67; 95% CI, 0.49 to 0.92) were associated with lower risk of the composite renal outcome. This association was attenuated and not statistically significant in participants with proteinuria<0.2 g/d who were not receiving statin therapy (HR, 0.89 and 0.87 for LDL-C and total cholesterol, respectively; P>0.05). Finally, within the subgroup of patients with lower levels of proteinuria, there were several differences in baselines characteristics upon stratification by baseline total cholesterol (Supplemental Table 4).
The association between baseline lipoproteins and rate of change of GFR over time is presented in Table 4. Although several lipoproteins were predictive of rate of change of GFR in unadjusted analyses, none of the measures was independently predictive after adjustment for other factors that may influence rate of change of GFR. This was consistent when variables were stratified by proteinuria level at baseline (Table 5). Three-way interactions between statin use, proteinuria, and LDL (P=0.61) and total cholesterol (P=0.71) were not statistically significant.
Table 4.
Associations between baseline lipoproteins and the rate of GFR decline in the Chronic Renal Insufficiency Cohort study
| Lipoprotein | Unadjusted | Adjusteda | ||
|---|---|---|---|---|
| Slope Differenceb per 1 SD Higher of Lipoprotein Variable (95% CI) | P Value | Slope Differenceb per 1 SD Higher of Lipoprotein Variable (95% CI) | P Value | |
| Total cholesterol | −0.20 (−0.32 to -0.08) | <0.01 | −0.00 (−0.12 to 0.11) | 0.94 |
| LDL cholesterol | −0.07 (−0.18 to 0.05) | 0.26 | 0.03 (−0.08 to 0.14) | 0.56 |
| HDL cholesterol | 0.10 (−0.01 to 0.21) | 0.06 | −0.03 (−0.14 to 0.08) | 0.57 |
| VLDL cholesterolc | −0.25 (−0.36 to -0.14) | <0.01 | 0.01 (−0.09 to 0.11) | 0.80 |
| Triglyceridesc | −0.21 (−0.32 to -0.09) | <0.01 | 0.05 (−0.06 to 0.15) | 0.39 |
| Lp(a)c | −0.19 (−0.30 to -0.08) | <0.01 | 0.01 (−0.10 to 0.12) | 0.84 |
| ApoA-I | 0.05 (−0.06 to 0.16) | 0.37 | 0.03 (−0.09 to 0.14) | 0.66 |
| ApoB | −0.23 (−0.35 to -0.11) | <0.01 | 0.06 (−0.05 to 0.17) | 0.30 |
Lp(a), lipoprotein(a).
Model adjusted for age, race, sex, diabetes, BP, statin use at baseline, smoking, 24-hour urine protein excretion, body mass index, clinical center, alcohol use, and baseline eGFR per 1-SD change in independent variable.
Slope difference in ml/min per 1.73 m2 per year; a negative slope difference indicates a faster decline in GFR.
Values were log transformed.
Table 5.
Associations between baseline lipoprotein measures and the rate of eGFR decline stratified by proteinuria at baseline in the Chronic Renal Insufficiency Cohort study
| Lipoprotein | 24-hr Urinary Protein≤0.2 g/d | 24-hr Urinary Protein>0.2 g/d | ||
|---|---|---|---|---|
| Slope Differenceb per 1 SD Higher of Lipoprotein Variable (95% CI) | P Value | Slope Differenceb per 1 SD Higher of Lipoprotein Variable (95% CI) | P Value | |
| Total cholesterol | 0.10 (−0.05 to 0.25) | 0.19 | −0.12 (−0.29 to 0.06) | 0.19 |
| LDL cholesterol | 0.11 (−0.04 to 0.25) | 0.15 | −0.03 (−0.20 to 0.13) | 0.68 |
| HDL cholesterol | −0.01 (−0.14 to 0.12) | 0.86 | −0.05 (−0.24 to 0.14) | 0.59 |
| VLDL cholesterolb | 0.06 (−0.06 to 0.19) | 0.34 | −0.06 (−0.23 to 0.10) | 0.46 |
| Triglyceridesb | 0.09 (−0.04 to 0.22) | 0.19 | −0.02 (−0.18 to 0.15) | 0.84 |
| Lp(a)b | 0.04 (−0.09 to 0.17) | 0.52 | −0.03 (−0.21 to 0.15) | 0.73 |
| ApoA-I | 0.07 (−0.06 to 0.21) | 0.29 | −0.04 (−0.23 to 0.15) | 0.70 |
| ApoB | 0.15 (0.01 to 0.29) | 0.03 | −0.04 (−0.22 to 0.13) | 0.61 |
Lp(a), lipoprotein(a).
Model adjusted for age, race, sex, diabetes, BP, statin use at baseline, smoking, 24-hour urine protein excretion, body mass index, clinical center, alcohol use, and baseline eGFR per 1-SD change in independent variable. Slope difference in ml/min per 1.73 m2 per year; a negative slope difference indicates a faster decline in GFR.
Values were log transformed.
Discussion
In this large cohort of patients with CKD, total cholesterol, triglycerides, VLDL-C, LDL-C, HDL-C, apoA-I, and apoB were not independently associated with progression of kidney disease. There was a borderline association between high Lp(a) levels and renal outcomes. However, there was a significant interaction by proteinuria. In patients with proteinuria<0.2 g/d, higher LDL-C and total cholesterol levels were associated with lower risk of kidney disease outcomes, whereas there was no significant association of LDL-C or total cholesterol levels and kidney disease outcomes in patients with proteinuria>0.2 g/d.
Dyslipidemia is common in patients with CKD and is characterized by elevated plasma triglyceride and VLDL-C levels and diminished plasma HDL-C concentrations (25). This pattern in the lipid profile was also seen at baseline in CRIC study participants (26). The association of LDL-C and its major protein apoB with kidney outcomes has been inconsistent in previous studies. In studies of patients with CKD (12) and without CKD (8), LDL-C and ApoB were significantly associated with a more rapid decline in renal function. Our study found no statistically significant association between LDL-C or apoB and CKD progression in the overall CRIC population, consistent with the Modification of Diet in Renal Disease and Atherosclerosis Research in Communities (ARIC) studies, as well as the Study of Heart and Renal Protection (SHARP) clinical trial, where statin/ezetimibe therapy was not associated with reduction in progression of kidney disease (9,11,27,28) However, total and LDL-C cholesterol levels were inversely associated with progression of kidney disease in patients with low levels of proteinuria, particularly those receiving statin therapy. The factors underlying this seemingly paradoxical relationship are unclear; participants in the lower cholesterol quartiles had more risk factors for progression and were more likely to be taking statins, perhaps reflecting a higher vascular risk. Although the relationship remained strong after adjustment for relevant covariates in multivariate analyses, it is possible that some residual confounding may contribute to this finding. In addition, there may be unmeasured factors contributing to confounding that cannot be accounted for in the analyses. This is supported by the significant differences in risk factor profile within the low proteinuria subgroup when stratified by baseline cholesterol, as noted in Supplemental Table 4. Another possibility is that because proteinuria is such a robust risk factor for progression of kidney disease, it may overwhelm the effect of other risk factors. In addition, as seen in Supplemental Table 3, patients with higher levels of proteinuria are more likely to have other risk factors for progression of CKD. In the absence of significant proteinuria, the relationship between LDL-C and outcomes may be easier to detect. Lastly, we evaluated the presence of malnutrition/inflammation as a confounder; in the setting of ESRD, a seemingly paradoxical relationship is seen between cholesterol levels and mortality. However, in the absence of malnutrition/inflammation, high cholesterol levels are associated with higher rates of mortality (22). In our study, results were consistent when stratified by malnutrition/inflammation, suggesting that the relationship between LDL-C cholesterol and progression of CKD is not confounded by the presence of malnutrition/inflammation. Of note, there was no relationship between total and LDL cholesterol levels and rate of change in GFR in the low proteinuria group (Table 5). This may relate to the overall slow decline in GFR in patients with lower levels of proteinuria with less power to detect an association; in addition, as shown in the African American Study of Kidney Disease and Hypertension study, nonlinear, abrupt declines in GFR are not uncommon in individual patients (29). This may contribute to why an association was seen between LDL and total cholesterol and clinical renal outcomes, but not with rate of decline in GFR.
Studies of the relationship between triglyceride levels and CKD progression have also been inconsistent. In the ARIC study, high triglycerides were associated with a rise in serum creatinine (9). Similarly, in a cohort of patients with IgA nephropathy, hypertriglyceridemia was independently associated with a 20% increase in serum creatinine levels above baseline (30). However, other studies have failed to show an association between triglycerides and progression of CKD (11,12). Our results, in the largest prospective study to date, demonstrate that VLDL-C and triglycerides are not independently predictive of progression of kidney disease.
Previous longitudinal studies evaluating HDL-C and apoA-I levels as predictors of decline in kidney function have been inconsistent; some studies have shown that low HDL-C and apoA-I levels were associated with a faster rate of progression of kidney disease (7–9,29), while others have not (12). In our study, neither HDL-C nor apoA-I levels were associated with kidney disease outcomes.
Although Lp(a) is a predictor of atherosclerotic cardiovascular disease in the general population, whether it predicts progression of kidney disease is not known (31). Lp(a) levels are known to increase early during the course of CKD and become more pronounced with increased severity of the disease (32,33), although some studies show a stronger association of Lp(a) with proteinuria than with GFR (34). In a prospective study in patients with type 2 diabetes who have overt proteinuria, an elevated Lp(a) level was an independent risk factor for the progression of diabetic nephropathy (35). In our study, Lp(a) levels were higher in patients with lower GFR and strongly predicted renal outcomes in unadjusted analyses. However, after adjustment for other known risk factors for progression, the association of Lp(a), even among the subpopulation with diabetes, was markedly attenuated and was not statistically significant. This suggests that effects of Lp(a) seen in previous studies may be confounded by other coexistent risk factors, but does not rule out a smaller association between Lp(a) levels and outcomes of kidney disease progression.
Our study makes an important contribution to the literature; as the largest study of the association between dyslipidemia and kidney disease progression in patients with CKD, it demonstrated that the lipids and lipoproteins measured in these analyses do not independently predict progression of kidney disease in the setting of CKD. Because they were obtained from an epidemiologic study, these data cannot directly address mechanisms of disease progression. Therefore, they do not rule out the role of dyslipidemia in progression of kidney disease; however, they do suggest that these effects may be mediated through other pathways and highlight the need for novel markers of lipid metabolism in the patients with CKD.
Our study has several strengths. The large sample size and availability of detailed, high-quality information on comorbidity and other risk factors in the CRIC study allowed for robust multivariate analyses to ascertain independent associations between lipoprotein measures and outcomes. In addition, the large proportion of minority and diabetic patients helps overcome the shortcomings of previous studies and enhances the generalizability of the findings. Our study also has important limitations. Most patients were receiving statins or other lipid-lowering therapy, which typically decreases total cholesterol, LDL-C, and, to a lesser extent, triglycerides. Statin use was more common in patients in the lowest quartile than the higher quartiles of cholesterol. Despite this limitation, the stratified analyses by baseline statin use were consistent with overall results. This study did not evaluate novel measures of lipoproteins measured by nuclear magnetic resonance spectroscopy (such as plasma apoC-III) that have been associated in cross-sectional studies with kidney function (37). The current analysis also did not assess whether dyslipidemia contributes to the high risk of cardiovascular disease seen in CKD, but future reports from the CRIC study will do so. Finally, it is possible that some of the seemingly paradoxical findings may simply relate to chance given the multiple comparisons performed in the analyses.
In summary, in this large cohort of patients with CKD, we report that total cholesterol, triglycerides, Lp(a), VLDL-C, LDL-C, HDL, apoA-I, and apoB were not independently associated with progression of kidney disease. We report an inverse relationship between LDL-C and total cholesterol levels and kidney disease outcomes in patients with low levels of proteinuria. Further research is needed to replicate these findings in other cohorts and to evaluate the pathophysiologic basis and implications of this seemingly paradoxical association.
Disclosures
None.
Supplementary Material
Acknowledgments
The CRIC study was funded under a cooperative agreement from National Institute of Diabetes and Digestive and Kidney Diseases (U01-DK060990, U01-DK060984, U01-DK061022, U01-DK061021, U01-DK061028, U01-DK060980, U01-DK060963, and U01-DK060902). In addition, this work was supported in part by the Perelman School of Medicine at the University of Pennsylvania Clinical and Translational Science Award National Institutes of Health (NIH)/National Center for Advancing Translational Sciences UL1-TR000003, Johns Hopkins University UL1-TR000424, University of Maryland GCRC M01-RR16500, Clinical and Translational Science Collaborative of Cleveland, UL1-TR000439 from the National Center for Advancing Translational Sciences component of the NIH and NIH roadmap for Medical Research, Michigan Institute for Clinical and Health Research UL1-TR000433, University of Illinois at Chicago CTSA UL1-RR029879, Tulane University Translational Research in Hypertension and Renal Biology P30-GM103337, Kaiser Permanente NIH/National Center for Research Resources UCSF-CTSI UL1-RR024131.
The study sponsor (National Institute of Diabetes and Digestive and Kidney Diseases) was involved in study design, interpretation of data, writing the report, and the decision to submit the report for publication.
The CRIC study investigators also include Harold I. Feldman, Alan S. Go, James P. Lash, Akinlolu Ojo, Raymond R. Townsend, and John Kusek.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.09320913/-/DCSupplemental.
References
- 1.Kaysen GA: New insights into lipid metabolism in chronic kidney disease. J Ren Nutr 21: 120–123, 2011 [DOI] [PubMed] [Google Scholar]
- 2.Vaziri ND: Lipotoxicity and impaired high density lipoprotein-mediated reverse cholesterol transport in chronic kidney disease. J Ren Nutr 20[Suppl]: S35–S43, 2010 [DOI] [PubMed] [Google Scholar]
- 3.Kasiske BL, O’Donnell MP, Cleary MP, Keane WF: Treatment of hyperlipidemia reduces glomerular injury in obese Zucker rats. Kidney Int 33: 667–672, 1988 [DOI] [PubMed] [Google Scholar]
- 4.Kasiske BL, O’Donnell MP, Cleary MP, Keane WF: Effects of reduced renal mass on tissue lipids and renal injury in hyperlipidemic rats. Kidney Int 35: 40–47, 1989 [DOI] [PubMed] [Google Scholar]
- 5.Kasiske BL, O’Donnell MP, Schmitz PG, Kim Y, Keane WF: Renal injury of diet-induced hypercholesterolemia in rats. Kidney Int 37: 880–891, 1990 [DOI] [PubMed] [Google Scholar]
- 6.Kasiske BL, O’Donnell MP, Keane WF: The Zucker rat model of obesity, insulin resistance, hyperlipidemia, and renal injury. Hypertension 19[Suppl]: I110–I115, 1992 [DOI] [PubMed] [Google Scholar]
- 7.Fox CS, Larson MG, Leip EP, Culleton B, Wilson PW, Levy D: Predictors of new-onset kidney disease in a community-based population. JAMA 291: 844–850, 2004 [DOI] [PubMed] [Google Scholar]
- 8.Schaeffner ES, Kurth T, Curhan GC, Glynn RJ, Rexrode KM, Baigent C, Buring JE, Gaziano JM: Cholesterol and the risk of renal dysfunction in apparently healthy men. J Am Soc Nephrol 14: 2084–2091, 2003 [DOI] [PubMed] [Google Scholar]
- 9.Muntner P, Coresh J, Smith JC, Eckfeldt J, Klag MJ: Plasma lipids and risk of developing renal dysfunction: The Atherosclerosis Risk in Communities study. Kidney Int 58: 293–301, 2000 [DOI] [PubMed] [Google Scholar]
- 10.Hadjadj S, Duly-Bouhanick B, Bekherraz A, BrIdoux F, Gallois Y, Mauco G, Ebran J, Marre M: Serum triglycerides are a predictive factor for the development and the progression of renal and retinal complications in patients with type 1 diabetes. Diabetes Metab 30: 43–51, 2004 [DOI] [PubMed] [Google Scholar]
- 11.Chawla V, Greene T, Beck GJ, Kusek JW, Collins AJ, Sarnak MJ, Menon V: Hyperlipidemia and long-term outcomes in nondiabetic chronic kidney disease. Clin J Am Soc Nephrol 5: 1582–1587, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Samuelsson O, Mulec H, Knight-Gibson C, Attman PO, Kron B, Larsson R, Weiss L, Wedel H, Alaupovic P: Lipoprotein abnormalities are associated with increased rate of progression of human chronic renal insufficiency. Nephrol Dial Transplant 12: 1908–1915, 1997 [DOI] [PubMed] [Google Scholar]
- 13.Kaysen GA: Lipid and lipoprotein metabolism in chronic kidney disease. J Ren Nutr 19: 73–77, 2009 [DOI] [PubMed] [Google Scholar]
- 14.Kaysen GA: Disorders in high-density metabolism with insulin resistance and chronic kidney disease. J Ren Nutr 17: 4–8, 2007 [DOI] [PubMed] [Google Scholar]
- 15.Dalrymple LS, Kaysen GA: The effect of lipoproteins on the development and progression of renal disease. Am J Nephrol 28: 723–731, 2008 [DOI] [PubMed] [Google Scholar]
- 16.Navaneethan SD, Pansini F, Perkovic V, Manno C, Pellegrini F, Johnson DW, Craig JC, Strippoli GFM: HMG CoA reductase inhibitors (statins) for people with chronic kidney disease not requiring dialysis. Cochrane Database Syst Rev CD007784, 2009 [DOI] [PubMed]
- 17.Rahman M, Baimbridge C, Davis BR, Barzilay J, Basile JN, Henriquez MA, Huml A, Kopyt N, Louis GT, Pressel SL, Rosendorff C, Sastrasinh S, Stanford C, ALLHAT Collaborative Research Group : Progression of kidney disease in moderately hypercholesterolemic, hypertensive patients randomized to pravastatin versus usual care: A report from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Am J Kidney Dis 52: 412–424, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Feldman HI, Appel LJ, Chertow GM, Cifelli D, Cizman B, Daugirdas J, Fink JC, Franklin-Becker ED, Go AS, Hamm LL, He J, Hostetter T, Hsu CY, Jamerson K, Joffe M, Kusek JW, Landis JR, Lash JP, Miller ER, Mohler ER, 3rd, Muntner P, Ojo AO, Rahman M, Townsend RR, Wright JT, Chronic Renal Insufficiency Cohort (CRIC) Study Investigators : The Chronic Renal Insufficiency Cohort (CRIC) Study: Design and methods. J Am Soc Nephrol 14[Suppl 2]: S148–S153, 2003 [DOI] [PubMed] [Google Scholar]
- 19.Lash JP, Go AS, Appel LJ, He J, Ojo A, Rahman M, Townsend RR, Xie D, Cifelli D, Cohan J, Fink JC, Fischer MJ, Gadegbeku C, Hamm LL, Kusek JW, Landis JR, Narva A, Robinson N, Teal V, Feldman HI, Chronic Renal Insufficiency Cohort (CRIC) Study Group : Chronic Renal Insufficiency Cohort (CRIC) Study: Baseline characteristics and associations with kidney function. Clin J Am Soc Nephrol 4: 1302–1311, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Joffe M, Hsu CY, Feldman HI, Weir M, Landis JR, Hamm LL, Chronic Renal Insufficiency Cohort (CRIC) Study Group : Variability of creatinine measurements in clinical laboratories: Results from the CRIC study. Am J Nephrol 31: 426–434, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Anderson AH, Yang W, Hsu CY, Joffe MM, Leonard MB, Xie D, Chen J, Greene T, Jaar BG, Kao P, Kusek JW, Landis JR, Lash JP, Townsend RR, Weir MR, Feldman HI, CRIC Study Investigators : Estimating GFR among participants in the Chronic Renal Insufficiency Cohort (CRIC) Study. Am J Kidney Dis 60: 250–261, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu Y, Coresh J, Eustace JA, Longenecker JC, Jaar B, Fink NE, Tracy RP, Powe NR, Klag MJ: Association between cholesterol level and mortality in dialysis patients: role of inflammation and malnutrition. JAMA 291: 451–459, 2004 [DOI] [PubMed] [Google Scholar]
- 23.Cox DR: Regression models and life-tables. J R Stat Soc B 34: 187–220, 2011 [Google Scholar]
- 24.Laird NM, Ware JH: Random-effects models for longitudinal data. Biometrics 38: 963–974, 1982 [PubMed] [Google Scholar]
- 25.Vaziri ND, Norris K: Lipid disorders and their relevance to outcomes in chronic kidney disease. Blood Purif 31: 189–196, 2011 [DOI] [PubMed] [Google Scholar]
- 26.Lee PH, Chang HY, Tung CW, Hsu YC, Lei CC, Chang HH, Yang HF, Lu LC, Jong MC, Chen CY, Fang KY, Chao YS, Shih YH, Lin CL: Hypertriglyceridemia: An independent risk factor of chronic kidney disease in Taiwanese adults. Am J Med Sci 338: 185–189, 2009 [DOI] [PubMed] [Google Scholar]
- 27.Baigent C, Landray MJ, Reith C, Emberson J, Wheeler DC, Tomson C, Wanner C, Krane V, Cass A, Craig J, Neal B, Jiang L, Hooi LS, Levin A, Agodoa L, Gaziano M, Kasiske B, Walker R, Massy ZA, Feldt-Rasmussen B, Krairittichai U, Ophascharoensuk V, Fellström B, Holdaas H, Tesar V, Wiecek A, Grobbee D, de Zeeuw D, Grönhagen-Riska C, Dasgupta T, Lewis D, Herrington W, Mafham M, Majoni W, Wallendszus K, Grimm R, Pedersen T, Tobert J, Armitage J, Baxter A, Bray C, Chen Y, Chen Z, Hill M, Knott C, Parish S, Simpson D, Sleight P, Young A, Collins R, SHARP Investigators : The effects of lowering LDL cholesterol with simvastatin plus ezetimibe in patients with chronic kidney disease (Study of Heart and Renal Protection): A randomised placebo-controlled trial. Lancet 377: 2181–2192, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hunsicker LG, Adler S, Caggiula A, England BK, Greene T, Kusek JW, Rogers NL, Teschan PE: Predictors of the progression of renal disease in the Modification of Diet in Renal Disease Study. Kidney Int 51: 1908–1919, 1997 [DOI] [PubMed] [Google Scholar]
- 29.Li L, Astor BC, Lewis J, Hu B, Appel LJ, Lipkowitz MS, Toto RD, Wang X, Wright JT, Jr, Greene TH: Longitudinal progression trajectory of GFR among patients with CKD. Am J Kidney Dis 59: 504–512, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Syrjänen J, Mustonen J, Pasternack A: Hypertriglyceridaemia and hyperuricaemia are risk factors for progression of IgA nephropathy. Nephrol Dial Transplant 15: 34–42, 2000 [DOI] [PubMed] [Google Scholar]
- 31.Erqou S, Kaptoge S, Perry PL, Di Angelantonio E, Thompson A, White IR, Marcovina SM, Collins R, Thompson SG, Danesh J, Emerging Risk Factors Collaboration : Lipoprotein(a) concentration and the risk of coronary heart disease, stroke, and nonvascular mortality. JAMA 302: 412–423, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kronenberg F: Epidemiology, pathophysiology and therapeutic implications of lipoprotein(a) in kidney disease. Expert Rev Cardiovasc Ther 2: 729–743, 2004 [DOI] [PubMed] [Google Scholar]
- 33.Sechi LA, Zingaro L, De Carli S, Sechi G, Catena C, Falleti E, Dell’Anna E, Bartoli E: Increased serum lipoprotein(a) levels in patients with early renal failure. Ann Intern Med 129: 457–461, 1998 [DOI] [PubMed] [Google Scholar]
- 34.Uhlig K, Wang SR, Beck GJ, Kusek JW, Marcovina SM, Greene T, Levey AS, Sarnak MJ: Factors associated with lipoprotein(a) in chronic kidney disease. Am J Kidney Dis 45: 28–38, 2005 [DOI] [PubMed] [Google Scholar]
- 35.Song KH, Ko SH, Kim HW, Ahn YB, Lee JM, Son HS, Yoon KH, Cha BY, Lee KW, Son HY: Prospective study of lipoprotein(a) as a risk factor for deteriorating renal function in type 2 diabetic patients with overt proteinuria. Diabetes Care 28: 1718–1723, 2005 [DOI] [PubMed] [Google Scholar]
- 36.Al-Shahrouri HZ, Ramirez P, Fanti P, Abboud H, Lorenzo C, Haffner S: NMR identifies atherogenic lipoprotein abnormalities in early diabetic nephropathy that are unrecognized by conventional analysis. Clin Nephrol 73: 180–189, 2010 [DOI] [PubMed] [Google Scholar]
- 37.Ooi EM, Chan DT, Watts GF, Chan DC, Ng TW, Dogra GK, Irish AB, Barrett PH: Plasma apolipoprotein C-III metabolism in patients with chronic kidney disease. J Lipid Res 52: 794–800, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.