Abstract
Background and objectives
More than 40% of elderly hemodialysis patients experience one or more accidental falls within a 1-year period. Such falls are associated with higher mortality. The objectives of this study were to assess whether falls are also common in elderly patients established on peritoneal dialysis and evaluate if patients with falls have a higher risk of mortality than patients who do not experience a fall.
Design, setting, participants, & measurements
Using a prospective cohort study design, patients ages≥65 years on chronic peritoneal dialysis from April 2002 to April 2003 at the University Health Network were recruited. Patients were followed biweekly, and falls occurring within the first 15 months were recorded. Outcome data were collected until death, study end (July 31, 2012), transplantation, or transfer to another dialysis center.
Results
Seventy-four of seventy-six potential patients were recruited, assessed at baseline, and followed biweekly for falls; 40 of 74 (54%) peritoneal dialysis patients experienced 89 falls (adjusted mean fall rate, 1.7 falls per patient-year; 95% confidence interval, 1.0 to 2.7). Patients with falls were more likely to have had previous falls, be more recently initiated onto dialysis, be men, be older, and have higher comorbidity. Twenty-eight patients died during the follow-up period. After adjustment for known risk factors, each successive fall was associated with a 1.62-fold higher mortality (hazard ratio, 1.62; 95% confidence interval, 1.29 to 2.02; P<0.001).
Conclusions
Accidental falls are common in the peritoneal dialysis population and often go unrecognized. Falls were associated with higher mortality risk. Because fall interventions are effective in other populations, screening peritoneal dialysis patients for falls may be a simple measure of clinical importance.
Keywords: dialysis, end stage kidney disease, geriatric nephrology, peritoneal dialysis
Introduction
Geriatric issues are becoming increasingly prevalent within the field of nephrology, because the absolute number of individuals ages 65 years or more undergoing chronic dialysis therapy continues to rise. One of the most common and concerning phenomena associated with aging is accidental falls. Falls account for 85% of seniors’ injury-related hospitalizations in Canada and are associated with long hospital stays, functional decline, long-term care admission, and mortality (1–3). Even falls that do not result in injury are associated with a loss of confidence and predict a reduction in activity level and reduced ability to care for oneself (2,4,5). Patients maintained on chronic dialysis are, by virtue of the high rates of multimorbidity, polypharmacy, muscular dysfunction, and cognitive deficits, at higher risk of falls, with data suggesting falls rates of 1.2–1.6 per person-year among patients treated with hemodialysis (HD) (6–9). As seen in nonrenal geriatric studies, patients stable on HD who experience one or more falls are at approximately 2-fold higher risk of death (after adjustment for known mortality risk factors) than patients who do not fall (10).
Little information on the fall rate and consequences of falls are available for patients stable on peritoneal dialysis (PD) therapy. We hypothesized that, given the previously shown high burden of geriatric syndromes among older patients with CKD, falls would be common and that, as seen in data from nonrenal geriatric populations, falls would be associated with a higher risk of death.
Materials and Methods
Using a prospective cohort study design, all ESRD patients≥65 years undergoing chronic PD treatment at the University Health Network were approached to participate in the study. Patients were excluded if they were unable or unwilling to provide informed consent or if they resided in a long-term institutional setting. Willing participants provided written informed consent to participate in the study. Recruitment and baseline assessments were conducted during the period from April 9, 2002, to April 9, 2003, by a research study nurse using standardized protocols. These protocols have been previously reported in detail (6). In brief, the medical history, including cause of ESRD and comorbid conditions, was abstracted from the clinical and electronic chart records. Comorbid illnesses included illnesses associated with aging (including documented osteoporosis, joint deforming arthritis, Parkinson’s disease, macular degeneration or cataracts, and a history of falls within the previous 12 months) and illnesses traditionally associated with renal disease (including hypertension, diabetes, cardiac disease, and cerebrovascular disease). A full medication history, dialysis history, and laboratory history (hemoglobin, serum albumin, serum calcium, and serum phosphate levels) were recorded for each subject. Three consecutive values of each laboratory test, taken at 1-month intervals, were averaged. Participants were also asked to undergo a comprehensive baseline assessment using validated tools measuring functional independence (Barthel Index [11] and Lawton–Brody [12] scales), functional mobility (timed up-and-go test [13]), and cognitive status (Mini Mental Status Examination [14]). The timed up-and-go test is a test of balance, mobility, and gait. Participants are asked to rise from the seated position in a chair (with arms), walk 3 m, turn around, and return to a seated position in the chair. The time taken to complete the task is noted. Participants are encouraged to wear their regular footwear and use a walking aid if needed. Completion of the task is timed in seconds, and scores<10 seconds are considered normal. Participants with scores between 10 and 15 seconds were considered as having slowed mobility, and participants with scores>15 seconds were considered as having impaired mobility (15,16).
Patients (and/or caregivers) were contacted in person or by telephone at biweekly intervals for the next 15 months (last date of follow-up was July 2004), and all falls were recorded prospectively using a standardized method (17). A fall was defined as an event that resulted in a person coming to rest inadvertently on the ground or other lower level (17). Participants were considered to be fallers if they sustained one or more falls during the biweekly fall observation period. Patient outcome was followed until death or study end (July 31, 2012) (Figure 1). Death, kidney transplantation, and facility transfer dates were confirmed using data from the local Toronto Area Dialysis Registry, which is a prospectively maintained dialysis registry for all patients on RRT within the Toronto region. Ethics approval was granted by the University Health Network Research Ethics Board.
Figure 1.
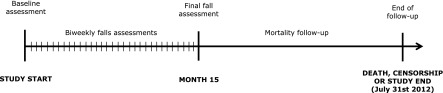
Study timeline and design.
Demographic data were summarized using mean and SD or median and quartiles for continuous variables and percentages for categorical data. There were five ways that follow-up on a patient could end: (1) death, (2) loss to follow-up, (3) kidney transplant, (4) transfer to another dialysis facility, or (5) renal recovery. In the analysis of fall rates, follow-up ended at the earliest of any these ways. A crude fall rate was calculated as the total number of falls divided by the total follow-up across patients. A Poisson regression with lognormal random effects was used to model heterogeneity between participants in fall rates. The number of falls was the outcome, and patient follow-up time was used to create an offset. The overall rate was estimated in an intercept-only model, and age at dialysis, sex, number of comorbidities, history of previous falls, cognitive impairment, and number of medications were included in a multivariable model to identify their influence on the rate of falls. In the survival analyses of risk factors for death, follow-up began at the start of the study, and patients were censored when follow-up ended for reasons other than death. It was assumed that patients who, at baseline, reported a fall within 1 year of recruitment were fallers, whereas patients who did not have or did not recall having a fall within 12 months before recruitment were considered nonfallers at the start of the study. During the biweekly follow-up, study participants could switch from the no falls group to the falls group if they experienced a fall. At the end of the fall follow-up period (15 months), participants remained within the group that they had been in until study end or death. Among participants with a fall, time at risk before a fall was allocated to the nonfaller group, and time at risk after the fall was allocated to the faller group. Nonfallers remained in the nonfaller group throughout the study. We also created a time-dependent variable for the cumulative number of falls that a patient had experienced. A graphical presentation of the survival of fallers versus nonfallers was made using an adaptation of the Kaplan–Meier product-limit estimator. We ran separate univariate Cox proportional hazards models for the binary fall–no fall variable and the cumulative number of falls variable as well as a multivariable model that adjusted for known risk factors for death in this population. To limit model overfitting, the risk factors included in the model were the number of comorbidities and age at the time of dialysis initiation. The effects of diabetes, serum albumin, and dialysis vintage were evaluated by assessing the change in the estimated hazard ratio by the univariate addition of each variable to the model. The proportionality of hazards over time was assessed for all variables.
All survival analyses were performed using the survival package in the R statistical software (version 3.0.1; R-Core Development Group, R Foundation of Vienna, Vienna, Austria). A significance level of 0.05 was used in all analyses.
Results
Of 76 potential participants, 74 (97%) agreed to participate. Patients had a mean age of 76.2±7.5 years and were on dialysis for a median of 22 months (quartiles=11–58) at the time of study entry (Table 1). Most patients were maintained on chronic ambulatory PD with four exchanges per day, with only 28 of 74 (38%) patients being treated with cycler therapy. Membrane characteristics were available in only a subset of patients and showed that 13 of 17 patients had low average transporter status. Fifty-seven patients did not have peritoneal equilibration test results within a 12-month period or had experienced peritonitis in the intervening period. Baseline functional characteristics are shown in Table 2. Over the fall follow-up period, 40 (54%) patients fell at least one time, with a total of 89 falls occurring. Forty-five percent of participants who fell had only one fall during the study follow-up period. Another 11 (27.5%) patients had two falls, whereas the remaining patients had three or more falls (median number of falls was two). The crude fall rate was 1.25 per patient-year, and the estimated mean per-patient fall rate was 1.7 per patient-year (95% confidence interval, 1.0 to 2.7). The most common activity during which a fall occurred was walking indoors (51%) followed by walking outdoors (12%) and sitting down from a standing position (11%). The majority of falls that occurred (87%) were either noninjurious or caused minor reported trauma (cuts, bruises, or scrapes). Five (6%) falls resulted in a fracture (n=1 for hip, pelvis, and rib; n=2 for other), and five (6%) falls caused patient-reported trauma to the head, with four falls reportedly leading to a loss of consciousness; 21 (24%) falls resulted in an emergency room visit, whereas 12 (14%) falls led to hospitalization within 24 hours of the fall.
Table 1.
Baseline demographic and medical characteristics
| Variable | All Patients (n=74) | Fallers (n=40) | Nonfallers (n=34) | P Value |
|---|---|---|---|---|
| Demographics | ||||
| Mean (SD) age, yr | 76.2 (7.5) | 77.5 (7.7) | 74.7 (7.2) | 0.11 |
| Mean (SD) age at dialysis initiation, yr | 73.2 (9.0) | 75.0 (8.6) | 71.1 (9.0) | 0.14 |
| Men | 41 (55%) | 24 (60%) | 17 (50%) | |
| Lives alone | 13 (18%) | 9 (23%) | 4 (12%) | 0.48 |
| Medical history | ||||
| Incident patient | 5 (7%) | 3 (8%) | 2 (6%) | >0.99 |
| Median (interquartile range) dialysis duration, mo | 22 (11–58) | 19 (8–56) | 29 (14–63) | 0.38 |
| Comorbidities | ||||
| Hypertension | 66 (89%) | 33 (83%) | 33 (97%) | 0.06 |
| Cerebrovascular disease | 12 (16%) | 9 (23%) | 3 (9%) | 0.13 |
| Diabetes | 24 (32%) | 17 (43%) | 7 (21%) | 0.05 |
| Cardiovascular disease | 43 (58%) | 20 (50%) | 23 (67%) | 0.64 |
| History of previous fracture(s) | 11 (15%) | 10 (25%) | 1 (3%) | 0.01 |
| Visual impairment | 50 (68%) | 31 (78%) | 19 (56%) | 0.08 |
| Depression | 12 (16%) | 8 (20%) | 4 (12%) | 0.53 |
| Cognitive impairment | 1 (2%) | 0 (0%) | 1 (3%) | 0.46 |
| Laboratory values | ||||
| Mean (SD) hemoglobin (n=73), mg/dl | 11.8±1.4 | 11.7±1.5 | 11.8±0.96 | 0.96 |
| Mean (SD) albumin, mg/dl | 3.51±0.41 | 3.40±0.45 | 3.64±0.03 | 0.03 |
| Mean (SD) calcium, mg/dl | 9.14±0.82 | 9.15±0.72 | 9.14±0.88 | 0.88 |
| Mean (SD) phosphate, mg/dl | 4.34±0.94 | 4.33±1.09 | 4.34±0.87 | 0.87 |
| Mean (SD) predialysis systolic BP | 132±16 | 132±17 | 133±15 | 0.97 |
| Medications | ||||
| Mean (SD) total medications | 10.9 (3.7) | 11.0 (3.7) | 10.8 (3.7) | 0.59 |
| Mean (SD) total hypotensive medications | 2.1 (1.4) | 1.95 (1.2) | 2.24 (1.5) | 0.44 |
Table 2.
Baseline functional characteristics
| Variable | All Patients (n=74) | Fallers (n=40) | Nonfallers (n=34) |
|---|---|---|---|
| One or more falls in previous 12 mo | 31 (42%) | 19 (48%) | 12 (35%) |
| One or more disabilities in basic activities of daily living | 47 (64%) | 31 (77%) | 16 (47%) |
| One or more disabilities in instrumental activities of daily living | 66 (89%) | 37 (92%) | 29 (85%) |
| Timed up-and-go test attempted | 60 (81%) | 31 (78%) | 29 (85%) |
| Timed up-and-go test time(s) | 11.0±2.4 | 11.7±2.6 | 10.2±2.0 |
| Mini Mental State Examination<24 (n=73) | 26 (35%) | 15 (38%) | 11 (32%) |
Patients with falls were more likely to be men, be older age, have higher comorbidity, and be more recently initiated onto dialysis. Patients were also more likely to have reported a fall in the previous 1 year and have a documented history of fractures and visual impairment (Table 1). Patients with falls had a higher baseline burden of functional dependence in one or more daily activities compared with nonfallers. No relationship between fall risk and BP was seen (Figure 2). Twenty-six (36%) of seventy-three individuals who completed the Mini Mental Status Examination met the criteria for cognitive impairment (a score<24), with no observable differences in cognitive status between fallers and nonfallers. Baseline laboratory values and medications seemed similar in both faller and nonfaller groups (Table 1).
Figure 2.
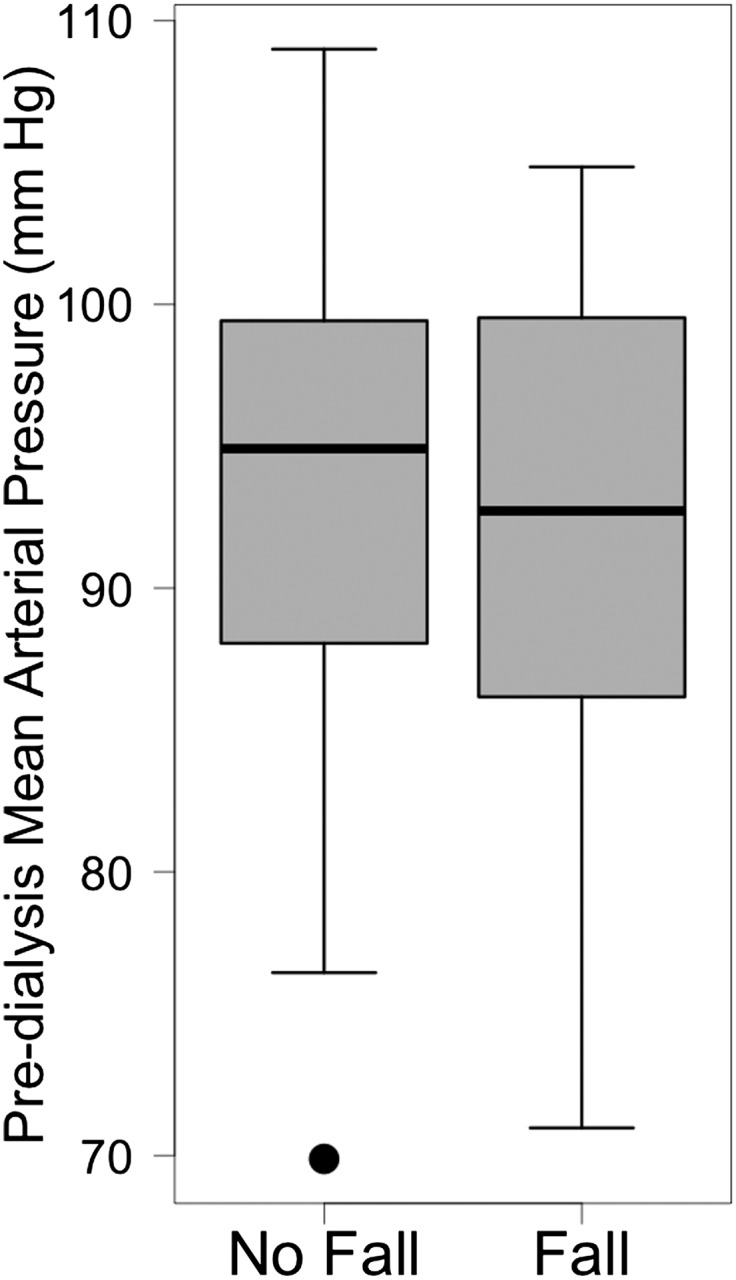
Box plot showing the distribution of BP readings is similar in both fallers and nonfallers. The whiskers extend to the largest or smallest nonoutlying value, where an outlier is defined to be 1.5× interquartile range above or below the limits of the box.
In multivariable random effects Poisson regression, the only factor significantly associated with higher falls risk was a history of previous falls (rate ratio [RR], 2.37; 95% confidence interval [95% CI], 0.98 to 5.70; P=0.05). Men and higher comorbidity were associated with nonstatistically significant increases in risk of falls (Table 3).
Table 3.
Multivariable random effects Poisson regression analysis looking at factors associated with higher fall risk
| Variable | Rate Ratio (95% Confidence Interval) | P Value |
|---|---|---|
| Body mass index (per 5 points) | 1.00 (0.64 to 1.57) | >0.99 |
| Age entry (per decade) | 0.96 (0.49 to 1.89) | 0.91 |
| Women | 0.69 (0.29 to 1.66) | 0.41 |
| Number of medications | 0.93 (0.69 to 1.26) | 0.64 |
| Mean arterial pressure (per 5 mmHg) | 0.90 (0.68 to 1.19) | 0.44 |
| Number of comorbid conditions (doubling) | 1.41 (0.55 to 3.6) | 0.47 |
| FAS (per 10 points) | 0.99 (0.72 to 1.38) | 0.97 |
| Fall in the previous 1 yr | 2.37 (0.98 to 5.70) | 0.05 |
FAS, functional activity score.
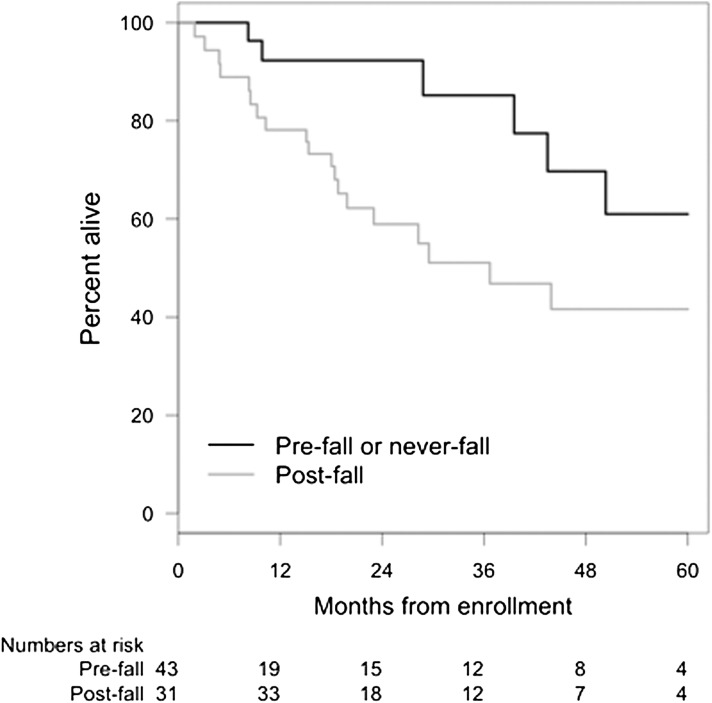
Patients were followed for survival for a median of 20.4 months (interquartile range=9.4–43.2 months; range=0.3–88.8 months). A total of 28 patients died during the follow-up period (median time to death=1.6 years). In unadjusted analysis, patients who had one or more falls were at a significantly higher risk of death compared with nonfallers (hazard ratio [HR], 2.19; 95% CI, 1.00 to 4.76; P=0.05). Using a reduced model and adjusting for the strongest known predictors of mortality (age at the start of dialysis and number of comorbidities), the number of fall events remained a significant predictor of death (HR, 1.62; 95% CI, 1.29 to 2.02; P<0.001) (Figure 3, Table 4). The HR estimate remained robust with the addition of the variables diabetes, albumin, and dialysis vintage to the model. This result was true in both unadjusted (HR per fall, 1.68; 95% CI, 1.31 to 2.16; P<0.001) and adjusted analyses (HR per fall, 1.62).
Figure 3.
Survival plot showing higher survival in patients who experienced no falls (black line) compared with those with one or more falls (gray line). Patients who reported a fall in 12 months before study recruitment were considered fallers at the start of the study. During the period of biweekly follow-up, participants could switch from the no falls group to the falls group if they experienced a fall. However, at the end of the fall follow-up period (15 months), participants remained within the group that they had been in until death or study end.
Table 4.
Multivariable analysis showing a higher mortality risk per fall event after adjustment for known predictors of death
| Variable | Hazard Ratio (95% Confidence Interval) | Significance Level |
|---|---|---|
| Fall event | 1.62 (1.29 to 2.02) | <0.001 |
| Age at cohort entry (per decade) | 1.06 (1.00 to 1.12) | 0.04 |
| Number of comorbidities | 1.13 (0.94 to 1.36) | 0.19 |
Factors introduced at baseline include the number of comorbidities and age at time of dialysis initiation. Concordance statistic=0.71.
Discussion
This study is one of the first prospective studies to examine the significance of accidental falls and their association with mortality among elderly individuals maintained on PD. More than one half of the study sample had at least one fall during the 1-year fall observation period. Fall rates were similar to the rates reported in HD populations (1.2–1.6 per person-year) (7,8) but almost two times the rates observed in large cohort studies of community-dwelling elderly populations (18,19).
Among the strengths of our study are the high rate of recruitment, the use of prospective methodology, and a biweekly approach to falls measurements to minimize the risk of recall bias. We also have robust long-term mortality follow-up, with patients being followed at least 8 years after the falls assessment period had ended. Polypharmacy (defined as four or more daily medications), sedating or other drugs affecting the neurologic system, and diuretics have been found to increase the risk of falls in older individuals (20). We were unable to show any association between medications (either the number or type) and falls, likely because of the widespread use of polypharmacy (the median number of drugs used was 10) and the small study sample size. Similarly, no significant association was found between BP and fall risk, possibly because of the wide range of BP readings seen in both patients who did and did not experience falls.
The strongest independent risk factor for falls was a history of one or more falls in the previous 1 year. This finding aligns with previous data in the geriatric literature (20–22). Notably, most of the patients who fell during the falls observation period fell more than one time. Previous literature has suggested that older individuals who experience recurrent falls are at greater risk of future adverse outcomes compared with nonfallers and one-time fallers (22). Routine clinical questioning about previous falls may, thus, be a key strategy to identify at-risk individuals, and therefore, preventive interventions can be introduced.
We observed a strong association between falls and higher mortality that persisted even after adjustment for known mortality risk factors, such as age and serum albumin. Dialysis patients are known to be at higher risk of fractures (23,24), which are also associated with an higher risk of death. Although it is possible to postulate that the increase in mortality risk is a direct consequence of the injuries incurred, the majority of falls in this study seemed to be noninjurious, with less than one quarter resulting in a hospital visit. It therefore is more likely that falls are a marker of increased frailty and/or general ill health. In CKD, the higher fracture risk is, in part, believed to be attributable to the presence of metabolic bone disease and may be related to low vitamin D3 levels. The rate of injurious falls (i.e., falls with documented injuries) seen in our study and in several other studies was, however, not higher than that seen in the general population. Boudville et al. (25) have shown that a low 25-hydroxyvitamin D3 level is also associated with markers of higher fall risk, such as impaired timed up-and-go and high scores on the fall efficacy score. This finding suggests that strategies, such as administration of exogenous 25-hydroxyvitamin D3 together with exercise programs targeting improving balance and muscle strength to reduce the risk of falls, require additional evaluation.
Unfortunately, longitudinal data on functional changes were not measured as part of this study. However, the observation that successive falls are associated with incremental risk of mortality also suggests that the falls may precipitate a reduced activity level because of the fear of falling syndrome, which in turn, increases the risk of dependence, hospitalization, and death. Given the increasing availability of assisted PD services in recent years across a variety of centers in North America and Europe, we speculate that it is likely that the fall rate seen in our data is an underestimation rather than overestimation of the burden of falls. Multidisciplinary falls prevention programs have been shown to be effective in preventing falls within various populations of at-risk older adults, but together with inpatient geriatric rehabilitation programs, they have not been well studied in the older dialysis patient population and may deserve additional attention and study.
The observation that patients at higher risk of falls were more likely to have recently started onto dialysis and the observed relationship between falls and higher mortality suggest that the study design has inadvertently led to a bias to a lower observed fall rate than actually occurred. Additionally, any misclassification of individuals who had experienced a fall before or after the 18-month falls assessment period as nonfallers would likely lead to an underestimation of the true association between falls and mortality. This finding suggests that the inclusion of a question about accidental falls during clinic assessments or the inclusion of a record of the cumulative number of falls occurring may have some clinical use in the assessment of patients undergoing chronic dialysis therapy.
In conclusion, we report a high burden of falls within the older population of patients on dialysis and an independent positive association between falls and mortality risk. Future studies are needed to determine whether screening and prevention programs are effective for reducing falls in the elderly dialysis population.
Disclosures
S.V.J. has received an honorarium from Amgen for giving Grand rounds at an academic institution within the past 12 months. There are no other disclosures.
Acknowledgments
Funding was from Physicians Services Incorporated Foundation.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Tinetti ME, Williams CS: The effect of falls and fall injuries on functioning in community-dwelling older persons. J Gerontol A Biol Sci Med Sci 53: M112–M119, 1998 [DOI] [PubMed] [Google Scholar]
- 2.Tinetti ME, Williams CS: Falls, injuries due to falls, and the risk of admission to a nursing home. N Engl J Med 337: 1279–1284, 1997 [DOI] [PubMed] [Google Scholar]
- 3.Sattin RW, Lambert Huber DA, DeVito CA, Rodriguez JG, Ros A, Bacchelli S, Stevens JA, Waxweiler RJ: The incidence of fall injury events among the elderly in a defined population. Am J Epidemiol 131: 1028–1037, 1990 [DOI] [PubMed] [Google Scholar]
- 4.Vellas B, Cayla F, Bocquet H, de Pemille F, Albarede JL: Prospective study of restriction of activity in old people after falls. Age Ageing 16: 189–193, 1987 [DOI] [PubMed] [Google Scholar]
- 5.Vellas BJ, Wayne SJ, Romero LJ, Baumgartner RN, Garry PJ: Fear of falling and restriction of mobility in elderly fallers. Age Ageing 26: 189–193, 1997 [DOI] [PubMed] [Google Scholar]
- 6.Cook WL, Jassal SV: Prevalence of falls among seniors maintained on hemodialysis. Int Urol Nephrol 37: 649–652, 2005 [DOI] [PubMed] [Google Scholar]
- 7.Desmet C, Beguin C, Swine C, Jadoul M, Université Catholique de Louvain Collaborative Group : Falls in hemodialysis patients: Prospective study of incidence, risk factors, and complications. Am J Kidney Dis 45: 148–153, 2005 [DOI] [PubMed] [Google Scholar]
- 8.Cook WL, Tomlinson G, Donaldson M, Markowitz SN, Naglie G, Sobolev B, Jassal SV: Falls and fall-related injuries in older dialysis patients. Clin J Am Soc Nephrol 1: 1197–1204, 2006 [DOI] [PubMed] [Google Scholar]
- 9.Abdel-Rahman EM, Yan G, Turgut F, Balogun RA: Long-term morbidity and mortality related to falls in hemodialysis patients: Role of age and gender - a pilot study. Nephron Clin Pract 118: c278–c284, 2011 [DOI] [PubMed] [Google Scholar]
- 10.Li M, Tomlinson G, Naglie G, Cook WL, Jassal SV: Geriatric comorbidities, such as falls, confer an independent mortality risk to elderly dialysis patients. Nephrol Dial Transplant 23: 1396–1400, 2008 [DOI] [PubMed] [Google Scholar]
- 11.Mahoney FI, Barthel DW: Functional evaluation: The Barthel index. Md State Med J 14: 61–65, 1965 [PubMed] [Google Scholar]
- 12.Lawton MP, Brody EM: Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 9: 179–186, 1969 [PubMed] [Google Scholar]
- 13.Podsiadlo D, Richardson S: The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J Am Geriatr Soc 39: 142–148, 1991 [DOI] [PubMed] [Google Scholar]
- 14.Folstein MF, Folstein SE, McHugh PR: “Mini-mental state.” A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12: 189–198, 1975 [DOI] [PubMed] [Google Scholar]
- 15.Botolfsen P, Helbostad JL, Moe-Nilssen R, Wall JC: Reliability and concurrent validity of the Expanded Timed Up-and-Go test in older people with impaired mobility. Physiother Res Int 13: 94–106, 2008 [DOI] [PubMed] [Google Scholar]
- 16.Deathe AB, Miller WC: The L test of functional mobility: Measurement properties of a modified version of the timed “up & go” test designed for people with lower-limb amputations. Phys Ther 85: 626–635, 2005 [PubMed] [Google Scholar]
- 17.Hakim RM: Reducing early mortality in hemodialysis patients. Curr Opin Nephrol Hypertens 17: 595–599, 2008 [DOI] [PubMed] [Google Scholar]
- 18.O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S: Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. Am J Epidemiol 137: 342–354, 1993 [DOI] [PubMed] [Google Scholar]
- 19.Campbell AJ, Borrie MJ, Spears GF: Risk factors for falls in a community-based prospective study of people 70 years and older. J Gerontol 44: M112–M117, 1989 [DOI] [PubMed] [Google Scholar]
- 20.Tromp AM, Pluijm SM, Smit JH, Deeg DJ, Bouter LM, Lips P: Fall-risk screening test: A prospective study on predictors for falls in community-dwelling elderly. J Clin Epidemiol 54: 837–844, 2001 [DOI] [PubMed] [Google Scholar]
- 21.Stalenhoef PA, Diederiks JP, Knottnerus JA, Kester AD, Crebolder HF: A risk model for the prediction of recurrent falls in community-dwelling elderly: A prospective cohort study. J Clin Epidemiol 55: 1088–1094, 2002 [DOI] [PubMed] [Google Scholar]
- 22.Pluijm SM, Smit JH, Tromp EA, Stel VS, Deeg DJ, Bouter LM, Lips P: A risk profile for identifying community-dwelling elderly with a high risk of recurrent falling: Results of a 3-year prospective study. Osteoporos Int 17: 417–425, 2006 [DOI] [PubMed] [Google Scholar]
- 23.Coco M, Rush H: Increased incidence of hip fractures in dialysis patients with low serum parathyroid hormone. Am J Kidney Dis 36: 1115–1121, 2000 [DOI] [PubMed] [Google Scholar]
- 24.Alem AM, Sherrard DJ, Gillen DL, Weiss NS, Beresford SA, Heckbert SR, Wong C, Stehman-Breen C: Increased risk of hip fracture among patients with end-stage renal disease. Kidney Int 58: 396–399, 2000 [DOI] [PubMed] [Google Scholar]
- 25.Boudville N, Inderjeeth C, Elder GJ, Glendenning P: Association between 25-hydroxyvitamin D, somatic muscle weakness and falls risk in end-stage renal failure. Clin Endocrinol (Oxf) 73: 299–304, 2010 [DOI] [PubMed] [Google Scholar]