Abstract
Background and objectives
Retinal abnormalities may be associated with changes in the renal vasculature. This study assessed the association between retinopathy and progression of kidney disease in participants of the Chronic Renal Insufficiency Cohort (CRIC) study.
Design, setting, participants, & measurements
This was a prospective study in which patients with CKD enrolled in CRIC had nonmydriatic fundus photographs of both eyes. All CRIC participants in six clinical sites in which fundus cameras were deployed were offered participation. Photographs were reviewed at a reading center. The presence and severity of retinopathy and vessel calibers were assessed using standard protocols by graders masked to clinical information. The associations of retinal features with changes in eGFR and the need for RRT (ESRD) were assessed.
Results
Retinal images and renal progression outcomes were obtained from 1852 of the 2605 participants (71.1%) approached. During follow-up (median 2.3 years), 152 participants (8.2%) developed ESRD. Presence and severity of retinopathy at baseline were strongly associated with the risk of subsequent progression to ESRD and reductions in eGFR in unadjusted analyses. For example, participants with retinopathy were 4.4 times (95% confidence interval [95% CI], 3.12 to 6.31) more likely to develop ESRD than those without retinopathy (P<0.001). However, this association was not statistically significant after adjustment for initial eGFR and 24-hour proteinuria. Venular and arteriolar diameter calibers were not associated with ESRD or eGFR decline. The results showed a nonlinear relationship between mean ratio of arteriole/vein calibers and the risk of progression to ESRD; participants within the fourth arteriole/vein ratio quartile were 3.11 times (95% CI, 1.51 to 6.40) more likely to develop ESRD than those in the first quartile (P<0.001).
Conclusions
The presence and severity of retinopathy were not associated with ESRD and decline in eGFR after taking into account established risk factors.
Keywords: chronic renal insufficiency, clinical epidemiology, epidemiology, outcomes, ESRD, kidney disease
Introduction
Retinal vasculopathy or retinopathy can be readily observed and documented by fundus photography. Retinal vascular abnormalities including vascular diameter changes may reflect broader vascular pathologic changes in the kidneys, heart, and other organs. Consequently, retinal images may supplement other diagnostic and prognostic information regarding kidney disease.
CKD is associated with substantial morbidity (1), including eye disease (2,3). We previously reported a strong independent, cross-sectional association between the severity of retinopathy and the level of kidney dysfunction (4). Previous population studies have shown associations between baseline retinopathy and progression of CKD (5,6).The purpose of this Retinopathy in Chronic Renal Insufficiency (RCRIC) study was to extend these observations by evaluating the relationship between retinal vascular changes and renal disease progression among the well characterized participants enrolled in the Chronic Renal Insufficiency Cohort (CRIC) study, a multicenter, long-term observational, prospective study in patients with CKD (7,8).
Materials and Methods
Study Design
A detailed description of the CRIC study (7,8) and the methodology used to obtain and interpret retinal images were previously reported (4). All CRIC participants from six CRIC clinical sites in which six fundus cameras were deployed were offered participation in our study. A total of 2605 participants in the CRIC study were offered participation in our ancillary RCRIC study. Among these, 1936 participants had baseline fundus photographs taken from June 2006 to May 2008. This study adhered to the tenets of the Declaration of Helsinki and was approved by the institutional review boards of the participating institutions. All participants provided written consent.
Trained nonophthalmic personnel took photographs of participants without pharmacologic dilation of the pupils. A Canon CR-DGI Non-Mydriatic Retinal Camera (Canon Inc, Tokyo, Japan) was used to obtain 45° digital, color fundus photographs. A set of two images, one centered on the macula and the other on the optic disc, was obtained from each eye. A participant was considered eligible for analysis if either the disc or macula photographs of one eye could be evaluated.
Retinopathy and Vessel Caliber Assessment Protocols
Digital fundus photographs were assessed by trained graders and a retinal specialist at a central reading site. Readers were unaware of the participant’s clinical and demographic information. Fundus pathology including retinopathy (attributed to diabetes, hypertension, or other) and measurement of the diameter of the major retinal vessels were assessed. Because the readers were unaware of the diabetic or hypertensive status of the participants, retinopathy was evaluated without assumption of cause.
The Atherosclerosis Risk in Communities (ARIC) study fundus photographic protocol (9) and the Early Treatment of Diabetic Retinopathy (ETDRS) grading protocols (10) were used to grade retinopathy caused by diabetes, hypertension, and other conditions. The Multi-Ethnic Study of Atherosclerosis protocol was used for the evaluation of macular edema (11). These grading protocols were previously used in persons with and without diabetes (12). The following evaluations of digital photographs were done by a single masked reader using standard protocols with standardized photographic field definitions.
Semiquantitative Grading of Retinopathy.
The following retinal abnormalities were graded by referring to standard photographs: microaneurysms, retinal hemorrhages, hemorrhages and/or microaneurysms, retinal hemorrhage type (flame or blot), drusen, hard exudates, cotton-wool patches or soft exudates, intraretinal microvascular abnormalities, new vessels on or within 1 disc–diameters of the disc or elsewhere, fibrous proliferation, and scars from previous pan retinal photocoagulation.
From these diverse retinal abnormalities, an overall ETDRS retinopathy severity score was assigned for each eye (5). The score, which is derived from the presence and severity of the above-mentioned abnormalities, is on an ordinal scale and is not a continuous variable. Scores were classified as normal (<14), very mild nonproliferative retinopathy (NPR; 14–20), NPR (35–53), and proliferative retinopathy (PR; >60). The score for the eye with more advanced retinopathy was used as the score of the participant; when photographs of only one eye were available, the score for that eye was used. A total of 116 participants (6%) had photographs that could not be graded for either eye. Among them, 38 participants had photographs in which no features could be detected. The remaining 78 participants had photographs that were ungraded because of poor image quality from underexposure or lack of focus, and although some mild retinopathy features were present, an accurate grading could not be assigned because more advanced and subtle retinopathy features were not discernible.
Intragrader agreement for the EDTRS retinopathy score was assessed in a random sample of 200 participants. The weighted κ value for ETDRS scores was 0.77 (95% confidence interval [95% CI], 0.67 to 0.88), a value similar to the reproducibility previously reported (10).
Semiautomated Quantitative Measurement of Vascular Diameters.
Image processor measurements of vascular arteriolar and venular calibers were performed according to the ARIC study protocol (9), using interactive vessel analysis software developed at the University of Wisconsin. Graders overlaid a grid centered on the disc to establish the distance from the optic nerve. Vessels were measured within an annulus spanning 0.5–1 disc diameter from the edge of the disc. Graders identified major arterioles and venules and chose segments most suitable for measurement according to the vessel’s sharpness and straightness. The diameters of up to six arterioles and six venules were averaged (9).
Renal Outcomes
We used three approaches to characterize CKD progression. The first was incident ESRD, defined as the initiation of chronic dialysis therapy or kidney transplantation. Ascertainment of ESRD in the CRIC study was supplemented by linkage with the US Renal Data System. The second approach utilized the slope of change of eGFR, in which eGFR was calculated using a CRIC internal GFR estimating equation derived from iothalamate125 clearance testing that incorporated information on serum creatinine, serum cystatin C, age, sex, and race (13,14). We also used a composite of ESRD and 50% decline in eGFR; however, because the results were very similar, we did not include them. These approaches used data through December 2011.
Statistical Analyses
A log transformation was applied to the values for 24-hour urine protein because the distribution was highly skewed. For the association between baseline retinopathy and incidence of ESRD, we used Cox proportional hazards models to estimate hazard ratios (HRs), their 95% CIs, associated P values, and the unadjusted cumulative incidence rates at 2 years. For the association between baseline retinopathy and CKD progression over time, we used linear mixed models of eGFR change (slope of change). Analyses were performed including all participants and for subgroups based on the presence of diabetes.
To investigate the associations of baseline retinopathy with risk of ESRD and eGFR slope, we used the following four statistical models: unadjusted, adjusted by baseline variables (age, systolic BP, race, body mass index [BMI], smoking, diabetes, and clinical site) plus baseline log-transformed 24-hour urine protein, adjusted by baseline variables plus baseline eGFR, and adjusted by baseline variables plus baseline log-transformed 24-hour urine protein plus baseline eGFR.
Retinopathy was included either as a dichotomous covariate (yes or no) or as a categorical covariate reflecting retinopathy severity (no retinopathy, mild NPR, NPR, or PR). Ungradable retinopathy was a separate category.
Vessel caliber measurements were modeled both as continuous and unordered categorical variables grouped into quartiles. We applied the strategies to covariate adjustment for analyzing the association of retinal vessel calibers with renal outcomes. A statistical test of interaction of retinopathy with diabetes was assessed separately. All statistical analyses were performed with Statistcal Analysis System V9.3 software (SAS Institute Inc, Cary, NC), and P<0.05 was considered statistically significant.
Results
Among 1936 participants who had baseline retinal photographs, 1852 participants with follow-up outcome measures available for analysis (1847 for ESRD and 1665 for eGFR) were included in the study. The median age was 62 years (range, 22–77 years), and 50.6% of participants were white, 43.6% were black, 54.1% were men, and 875 (47.2%) had diabetes. At baseline, there were 1221 participants (65.9%) with no retinopathy, 133 (7.2%) with mild NPR, 227 (12.3%) with NPR, 166 (9.0%) with PR, and the remaining 105 (5.7%) were not assessed as a result of poor image quality. Table 1 shows participants’ characteristics.
Table 1.
Characteristics of participants by retinopathy status
| Characteristic | Retinopathy Status | P Valuea | ||||
|---|---|---|---|---|---|---|
| No NPR | Mild NPR | NPR | PR | Ungradable | ||
| Participants | 1221 (66) | 133 (7) | 227 (12) | 166 (9) | 105 (6) | n/a |
| Men | 638 (52) | 78 (59) | 133 (59) | 99 (60) | 54 (51) | 0.14 |
| Race | ||||||
| White | 697 (57) | 51 (38) | 85 (37) | 70 (42) | 34 (32) | <0.001 |
| Black | 464 (38) | 68 (51) | 127 (56) | 86 (52) | 63 (60) | |
| Other | 60 (5) | 14 (11) | 15 (7) | 10 (6) | 8 (8) | |
| Ethnicity | ||||||
| Hispanic | 52 (4) | 3 (2) | 14 (6) | 15 (9) | 6 (6) | 0.04 |
| Smoking status | ||||||
| Nonsmoker | 586 (48) | 52 (39) | 89 (39) | 79 (48) | 39 (37) | 0.06 |
| Former smoker | 503 (41) | 60 (45) | 103 (45) | 68 (41) | 53 (50) | |
| Current smoker | 132 (11) | 21 (16) | 35 (15) | 19 (11) | 13 (12) | |
| Presence of comorbidities | ||||||
| Any cardiovascular disease | 335 (27) | 60 (45) | 101 (44) | 86 (52) | 56 (53) | <0.001 |
| Hypertension | 1027 (84) | 127 (95) | 216 (95) | 160 (96) | 100 (95) | <0.001 |
| Diabetes mellitus | 379 (31) | 64 (48) | 203 (89) | 156 (94) | 73 (70) | <0.001 |
| Mean age (yr) | 59.7 (11.0) | 59.8 (10.1) | 59.8 (10.4) | 58.4 (10.7) | 63.7 (9.5) | 0.002 |
| Mean BMI (kg/m2) | 31.1 (7.4) | 32.4 (8.2) | 33.1 (8.0) | 32.4 (7.1) | 32.8 (7.7) | <0.001 |
| Mean systolic BP (mmHg) | 123 (20) | 129 (21) | 135 (24) | 132 (24) | 133 (23) | <0.001 |
| Mean diastolic BP (mmHg) | 70 (12) | 73 (13) | 69 (13) | 67 (13) | 67 (13) | <0.001 |
| Mean eGFR (ml/min per 1.73 m2) | 47.8 (18.3) | 42.8 (19.3) | 38.0 (16.4) | 33.9 (14.6) | 38.6 (17.6) | <0.001 |
| Median 24-h urine protein (g/24 h) | 0.11 (0.06, 0.41) | 0.18 (0.07, 0.63) | 0.48 (0.10, 1.22) | 0.76 (0.19, 2.37) | 0.21 (0.08, 1.42) | <0.001b |
Data are presented as n (%), mean (SD), or median (25%, 75%) unless otherwise indicated. NPR, nonproliferative retinopathy; PR, proliferative retinopathy; BMI, body mass index.
Chi-squared test for categorical characteristics, ANOVA for continuous characteristics.
Based on the ANOVA for log-transformed value.
During the median follow-up of 2.3 years, 152 of 1847 participants (8.2%) developed ESRD (105 of 871 participants with diabetes [12.1%] and 47 of 976 participants without diabetes [4.8%]). Among participants with ≥2 eGFR measurements at or after photographic baseline (median number of eGFR measurements, 5), the mean slopes of eGFR were −0.53 ml/min per 1.73 m2 per year (95% CI, −0.68 to −0.39) overall and −1.0 (−1.2 to −0.8) and −0.14 (−0.32 to 0.04) in participants with and without diabetes, respectively. This eGFR slope is somewhat lower than the slope in the CRIC study because participants that had eye photographs were healthier than CRIC participants that did not get photographs (3).
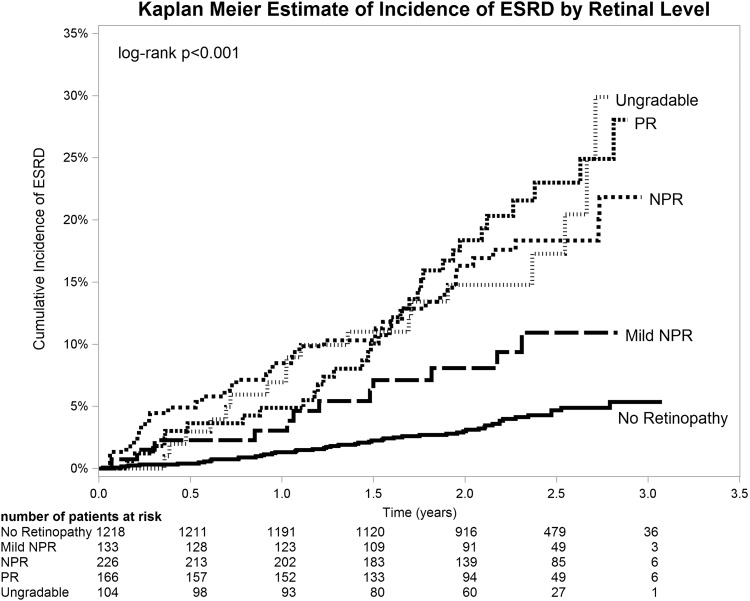
Among all participants, the presence of any retinopathy was associated with a significantly higher incidence of ESRD (14.9% versus 3.3%; P<0.001), and greater severity of retinopathy was associated with a higher incidence of ESRD (8.2% for mild NPR, 15.9% for NPR, 18.9% for PR; Figure 1, Table 2). This relationship remained significant after adjustment for known risk factors for CKD progression including age, systolic BP, race, diabetes mellitus, BMI, smoking and 24-hour urine protein (P=0.004; Table 2). Although the risk of ESRD was lower among participants without retinopathy and higher with more severe retinopathy in the unadjusted analyses, the multivariable analysis adjusting for the above risk factors showed that risk of ESRD was approximately 2-folder higher in participants with retinopathy regardless of the severity of retinopathy.
Figure 1.
Kaplan–Meier estimates of cumulative incidence of ESRD by retinal level. All estimates are plotted until <10 participants are left at risk. The actual number remaining at 3 years is reported in the table. NPR, nonproliferative retinopathy; PR, proliferative retinopathy.
Table 2.
The association of retinopathy with the incidence of ESRD
| Level | At Risk (n) | ESRD (%)a | Model 1 (Unadjusted) | Model 2 (Partially Adjusted) | Model 3 (Partially Adjusted) | Model 4 (Fully Adjusted) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| HR (95% CI) | P Value | HR (95% CI) | P Value | HR (95% CI) | P Value | HR (95% CI) | P Value | |||
| Any retinopathy | ||||||||||
| No retinopathy | 1218 | 3.3 | 1.00 | <0.001 | 1.00 | 0.003 | 1.00 | <0.001 | 1.00 | <0.001 |
| Retinopathy | 525 | 14.9 | 4.44 (3.12 to 6.31) | <0.001b | 1.98 (1.21 to 3.26) | 0.004b | 1.58 (1.00 to 2.50) | 0.049b | 1.26 (0.76 to 2.11) | 0.36b |
| Ungradable | 104 | 18.2 | 5.43 (3.22 to 9.16) | 3.03 (1.58 to 5.82) | 3.80 (2.19 to 6.58) | 3.19 (1.79 to 5.68) | ||||
| Retinal level | ||||||||||
| No retinopathy | 1218 | 3.3 | 1.00 | <0.001 | 1.00 | 0.01 | 1.00 | <0.001 | 1.00 | <0.001 |
| Mild NPR | 133 | 8.2 | 2.45 (1.30 to 4.63) | <0.001b | 1.99 (0.99 to 4.03) | 0.07b | 1.44 (0.71 to 2.94) | 0.10b | 1.27 (0.60 to 2.71) | 0.35b |
| NPR | 226 | 15.9 | 4.76 (3.11 to 7.27) | 1.96 (1.01 to 3.79) | 2.04 (1.14 to 3.65) | 1.61 (0.82 to 3.13) | ||||
| PR | 166 | 18.9 | 5.65 (3.65 to 8.76) | 2.00 (1.10 to 3.62) | 1.33 (0.75 to 2.36) | 1.04 (0.56 to 1.93) | ||||
| Ungradable | 104 | 18.2 | 5.43 (3.22 to 9.16) | 3.03 (1.56 to 5.87) | 3.85 (2.20 to 6.74) | 3.20 (1.77 to 5.77) | ||||
| Arteriole diameter, quartile (µm) | ||||||||||
| First (≤140) | 382 | 6.7 | 1.00 | 0.17 | 1.00 | 0.13 | 1.00 | 0.27 | 1.00 | 0.11 |
| Second (>140, ≤149) | 387 | 3.7 | 0.54 (0.30 to 0.99) | 0.44 (0.22 to 0.89) | 0.57 (0.28 to 1.16) | 0.64 (0.30 to 1.37) | ||||
| Third (>149, ≤159) | 383 | 6.7 | 1.00 (0.61 to 1.66) | 0.91 (0.51 to 1.62) | 1.08 (0.62 to 1.89) | 1.27 (0.67 to 2.37) | ||||
| Fourth (>159) | 389 | 5.5 | 0.82 (0.49 to 1.39) | 0.83 (0.46 to 1.48) | 1.12 (0.62 to 1.99) | 1.59 (0.86 to 2.93) | ||||
| Per-unit increase | 1541 | 5.7 | 0.99 (0.83 to 1.19) | 0.94 | 1.03 (0.85 to 1.25) | 0.76 | 0.99 (0.83 to 1.18) | 0.91 | 1.20 (0.97 to 1.49) | 0.09 |
| Venular diameter, quartile (µm) | ||||||||||
| First (≤204) | 392 | 7.0 | 1.00 | 0.13 | 1.00 | 0.10 | 1.00 | 0.53 | 1.00 | 0.73 |
| Second (>204, ≤219) | 389 | 3.5 | 0.50 (0.27 to 0.90) | 0.61 (0.31 to 1.21) | 0.70 (0.39 to 1.28) | 0.84 (0.42 to 1.67) | ||||
| Third (>219, ≤236) | 377 | 5.8 | 0.83 (0.50 to 1.38) | 0.55 (0.30 to 1.01) | 0.69 (0.38 to 1.27) | 0.68 (0.35 to 1.34) | ||||
| Fourth (>236) | 383 | 6.3 | 0.90 (0.55 to 1.50) | 0.52 (0.30 to 0.93) | 0.66 (0.34 to 1.29) | 0.80 (0.43 to 1.50) | ||||
| Per-unit increase | 1541 | 5.7 | 1.01 (0.84 to 1.21) | 0.95 | 0.88 (0.73 to 1.06) | 0.19 | 0.95 (0.79 to 1.14) | 0.57 | 0.91 (0.74 to 1.13) | 0.39 |
| Arteriolar/venular ratio, quartile | ||||||||||
| First (≤0.64) | 374 | 7.4 | 1.00 | 0.02 | 1.00 | <0.001 | 1.00 | 0.03 | 1.00 | <0.001 |
| Second (>0.64, ≤0.68) | 388 | 5.3 | 0.71 (0.42 to 1.20) | 1.15 (0.63 to 2.07) | 1.01 (0.53 to 1.91) | 1.25 (0.64 to 2.44) | ||||
| Third (>0.68, ≤0.73) | 388 | 3.0 | 0.40 (0.21 to 0.75) | 0.56 (0.26 to 1.20) | 0.71 (0.36 to 1.39) | 0.59 (0.27 to 1.28) | ||||
| Fourth (>0.73) | 391 | 7.2 | 0.98 (0.60 to 1.58) | 3.10 (1.73 to 5.57) | 1.80 (0.93 to 3.49) | 3.11 (1.51 to 6.40) | ||||
| Per-unit increase | 1541 | 5.7 | 0.95 (0.79 to 1.15) | 0.63 | 1.21 (0.98 to 1.49) | 0.07 | 1.06 (0.89 to 1.27) | 0.52 | 1.32 (1.03 to 1.70) | 0.03 |
Model 1 is unadjusted. Model 2 is adjusted for age, systolic BP, race, diabetes, BMI, smoking status, clinical site, and 24-hour urine protein. Model 3 is adjusted for age, systolic BP, race, diabetes, BMI, smoking status, clinical site, and eGFR. Model 4 is adjusted for age, systolic BP, race, diabetes, BMI, smoking status, clinical site, 24-hour urine protein, and eGFR. HR, hazard ratio; 95% CI, 95% confidence interval. .
Percentage of ESRD, 2-year cumulative incidence rate.
P value for comparison excluding ungradable photographs.
When the above multivariable analyses were further adjusted for baseline eGFR, the HRs associated with ESRD decreased and were not statistically significant when excluding the participants with ungradable photographs. Interestingly, participants with ungradable photographs had the highest HR of 3.2 for ESRD that remained statistically significant after multivariate adjustment.
The relationship between the presence of retinopathy and ESRD was consistent for participants with and without diabetes mellitus; the interaction between diabetes mellitus and presence of retinopathy on ESRD was not significant (P=0.24).
The presence and severity of retinopathy was associated with a significantly steeper decline in eGFR in the unadjusted analysis (P<0.001; Table 3). This relationship did not persist after adjustment for known risk factors including age, systolic BP, race, diabetes, BMI, smoking, 24-hour urine protein, and/or baseline eGFR.
Table 3.
The association of retinopathy with eGFR slope (ml/min per 1.73 m2 per year)
| Level | At Risk (n) | Model 1 (Unadjusted) | Model 2 (Partially Adjusted) | Model 3 (Partially Adjusted) | Model 4 (Fully Adjusted) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Slope Difference (95% CI) | P Value | Slope Difference (95% CI) | P Value | Slope Difference (95% CI) | P Value | Slope Difference (95% CI) | P Value | ||
| Any retinopathy | |||||||||
| No retinopathy | 1134 | 0 | <0.001 | 0 | 0.95 | 0 | 0.26 | 0 | 0.88 |
| Retinopathy | 442 | −0.93 (−1.27 to −0.59) | −0.04 (−0.38 to +0.31) | −0.27 (−0.64 to +0.10) | −0.01 (−0.36 to +0.33) | ||||
| Ungradable | 89 | −0.89 (−1.59 to −0.20) | −0.09 (−0.74 to +0.56) | −0.38 (−1.07 to +0.32) | −0.17 (−0.83 to +0.49) | ||||
| Retinal level | |||||||||
| No retinopathy | 1134 | 0 | <0.001 | 0 | 0.77 | 0 | 0.08 | 0 | 0.62 |
| Mild NPR | 116 | −0.50 (−1.07 to +0.08) | −0.07 (−0.61 to +0.46) | −0.05 (−0.63 to +0.52) | −0.05 (−0.59 to +0.50) | ||||
| NPR | 187 | −0.83 (−1.31 to −0.36) | 0.15 (−0.32 to +0.62) | −0.07 (−0.58 to +0.44) | 0.21 (−0.27 to +0.69) | ||||
| PR | 139 | −1.47 (−2.04 to −0.90) | −0.28 (−0.84 to +0.29) | −0.84 (−1.43 to -0.24) | −0.31 (−0.88 to +0.26) | ||||
| Ungradable | 89 | −0.89 (−1.58 to −0.20) | −0.09 (−0.74 to +0.56) | −0.39 (−1.08 to +0.31) | −0.17 (−0.83 to +0.49) | ||||
| Arteriole diameter, quartile (µm) | |||||||||
| First (≤140) | 350 | 0 | 0.54 | 0 | 0.61 | 0 | 0.64 | 0 | 0.58 |
| Second (>140, ≤149) | 359 | −0.01 (−0.45 to +0.43) | −0.03 (−0.43 to +0.37) | −0.09 (−0.53 to +0.34) | −0.03 (−0.44 to +0.38) | ||||
| Third (>149, ≤159) | 343 | 0.25 (−0.19 to +0.69) | 0.11 (−0.30 to +0.52) | 0.12 (−0.32 to +0.57) | 0.12 (−0.30 to +0.53) | ||||
| Fourth (>159) | 353 | −0.05 (−0.49 to +0.39) | −0.16 (−0.58 to +0.25) | −0.15 (−0.60 to +0.31) | −0.17 (−0.59 to +0.25) | ||||
| Venular diameter, quartile (µm) | |||||||||
| First (≤204) | 359 | 0 | 0.06 | 0 | 0.50 | 0 | 0.31 | 0 | 0.52 |
| Second (>204, ≤219) | 364 | 0.27 (−0.16 to +0.70) | 0.28 (−0.11 to +0.67) | 0.17 (−0.26 to +0.59) | 0.25 (−0.14 to +0.65) | ||||
| Third (>219, ≤236) | 339 | 0.14 (−0.29 to +0.58) | 0.25 (−0.16 to +0.66) | 0.23 (−0.21 to +0.67) | 0.27 (−0.15 to +0.68) | ||||
| Fourth (>236) | 343 | −0.32 (−0.77 to +0.12) | 0.16 (−0.28 to +0.59) | −0.16 (−0.63 to +0.31) | 0.12 (−0.32 to +0.56) | ||||
| Arteriolar/venular ratio | |||||||||
| First (≤0.64) | 337 | 0 | 0.01 | 0 | 0.06 | 0 | 0.03 | 0 | 0.04 |
| Second (>0.64, ≤0.68) | 347 | 0.74 (+0.30 to +1.19) | 0.24 (−0.17 to +0.65) | 0.59 (+0.15 to +1.03) | 0.27 (−0.15 to +0.69) | ||||
| Third (>0.68, ≤0.73) | 363 | 0.62 (+0.18 to +1.06) | 0.09 (−0.32 to +0.50) | 0.36 (−0.08 to +0.80) | 0.13 (−0.29 to +0.54) | ||||
| Fourth (>0.73) | 358 | 0.47 (+0.02 to +0.92) | −0.30 (−0.72 to +0.12) | 0.10 (−0.35 to +0.55) | −0.29 (−0.72 to +0.13) | ||||
Model 1 is unadjusted. Model 2 is adjusted for age, systolic BP, race, diabetes, BMI, smoking status, clinical site, and 24-hour urine protein. Model 3 is adjusted for age, systolic BP, race, diabetes, BMI, smoking status, clinical site, and eGFR. Model 4 is adjusted for age, systolic BP, race, diabetes, BMI, smoking status, clinical site, 24-hour urine protein, and eGFR.
Neither the mean calibers of retinal veins nor arterioles were significantly associated with progression to ESRD (Table 2). The arteriole/vein ratio, however, was significantly, nonlinearly associated with subsequent progression to ESRD (unadjusted P for overall difference is 0.02; P<0.001 when adjusted for baseline risk factors, 24-hour protein, and eGFR). The arteriole/vein ratio in the fourth quartile (those with the smaller venules and larger arterioles) was significantly associated with a higher risk of ESRD (HR, 3.11; 95% CI, 1.51 to 6.40) in the multivariate analysis (Table 2).
Neither the mean calibers of retinal veins nor arterioles were significantly associated with eGFR slope (Table 3) in the unadjusted or multivariable analysis. A larger arteriolar/venular ratio was associated with a steeper decline in eGFR, although this association was of borderline significance (overall P=0.04; Table 3).
Discussion
This is the first large-scale, long-term, prospective, multicenter study to examine in detail the association between retinopathy and kidney disease progression among individuals with established CKD. The results summarized in Table 1 and our previous report (5) show a cross-sectional association at baseline between retinopathy and decreased renal function. Our current results show a significant association between retinopathy and subsequent progression of kidney disease in unadjusted analyses, suggesting that retinovascular pathology may be a reflection of disease in other vascular beds, including the kidneys. When adjusted for baseline kidney function parameters such as eGFR and proteinuria in the multivariable analysis, the association between retinopathy and CKD progression waned. These results, therefore, suggest that both the retinopathy level and the presence of any retinopathy are associated with the progression of CKD but they do not provide additional prognostic information for kidney disease progression beyond that provided by 24-hour urine protein and eGFR.
Unexpectedly, the greatest risk of CKD progression was observed in persons whose retinal photographs could not be graded. A number of ocular and systemic conditions may be associated with ungradable fundus photographs. Decreased ocular media clarity by cataracts, corneal opacities, vitreous hemorrhage or retinal detachment, and poor pupillary dilation may cause poor photographic quality. In addition, severely ill patients are less likely to sit quietly and maintain fixation and this may in turn result in poor-quality photographs. Similar results were reported by another study showing that eyes with ungradable photographs have more eye pathology (10), suggesting that ungradable photography by itself may provide important information, and such information should not be disregarded.
No significant association was observed for both venular or arteriolar diameters and risk of CKD progression when each of these two measurements was analyzed separately. This is consistent with a previous population-based study (15). However, when we looked at the ratio between the arterioles and venules, the largest ratio (highest quartile) was statistically significantly associated with future progression of kidney disease (risk of ESRD and steeper eGFR decline) that remained significant after multivariate adjustment for baseline kidney function. This relationship was not linear; therefore, the interpretation of the per-unit increase for the arteriolar/venular ratio is unclear. Participants with the largest quartile of arteriolar/venular ratio, however, had a significantly higher risk of ESRD, as well as a steeper eGFR slope. In other words, participants with a combination of smaller venules and larger arterioles had the highest risk for kidney disease progression. The interpretation of these results is difficult because participants in the third quartile did not show increased risk of progression. These results need to be confirmed by future studies.
Smaller venules were shown to be associated with higher mean arterial BP and higher serum HDL cholesterol (16). Smoking, on the other hand, was reported to be associated with larger arterioles (17). All of these conditions are risk factors for the development of CKD. Both smaller arterioles and smaller venules were reported with advancing CKD (18).
Our study has some limitations, such as the short follow-up and the possibility that a lack of associations could be a result of the effect of competing risk such as death from cardiac and other comorbidities.
In summary, our study performed in a population of patients with CKD demonstrates that both the retinopathy level and presence of any retinopathy are strong risk factors for CKD outcomes, but they do not provide additional prognostic information beyond that offered by 24-hour urine protein and eGFR. Additional studies are needed to further understand the relationship between the large arteriolar venular ratio and progression of CKD.
Disclosures
R.R.T. is a consultant for Medtronic, Janssen, and Merck. J.C.L. received research funding from Amgen Inc.
Acknowledgments
This study was supported by a grant from the National Institutes of Health (NIH) (DK74151). The CRIC study was funded by a National Institute for Diabetes and Digestive and Kidney Diseases cooperative agreement (U01-DK060990, U01-DK060984, U01-DK061022, U01-DK061021, U01-DK061028, U01-DK060980, U01-DK060963, and U01-DK060902); Clinical and Translational Science Awards from the University of Pennsylvania (NIH/National Center for Advancing Translational Sciences UL1-TR000003) and University of Illinois at Chicago (UL1-RR029879); and grants from Johns Hopkins University (UL1-TR000424), University of Maryland General Clinical Research Center (M01RR-16500), Clinical and Translational Science Collaborative of Cleveland (UL1-TR000439), Michigan Institute for Clinical and Health Research (UL1-TR000433), Tulane University Translational Research in Hypertension and Renal Biology (P30-GM103337), Kaiser Permanente (NIH/National Center for Research Resources UCSF-CTSI UL1 RR-024131), Vivian S. Lasko Research Fund, Nina C. Mackall Trust, and Research to Prevent Blindness.
The CRIC study investigators include Lawrence J. Appel, Alan S. Go, Jiang He, and Akinlolu Ojo.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van Lente F, Levey AS: Prevalence of chronic kidney disease in the United States. JAMA 298: 2038–2047, 2007 [DOI] [PubMed] [Google Scholar]
- 2.Wong WW, Wong TT, Cheung CY, Sabanayagam C: Kidney and eye diseases: Common risk factors, etiological mechanisms, and pathways [published online ahead of print December 11, 2013]. Kidney Int 10.1038/ki.2013.491 [DOI] [PubMed] [Google Scholar]
- 3.Grunwald JE, Alexander J, Maguire M, Whittock R, Parker C, McWilliams K, Lo JC, Townsend R, Gadegbeku CA, Lash JP, Fink JC, Rahman M, Feldman H, Kusek J, Ojo A, CRIC Study Group : Prevalence of ocular fundus pathology in patients with chronic kidney disease. Clin J Am Soc Nephrol 5: 867–873, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grunwald JE, Alexander J, Ying GS, Maguire M, Daniel E, Whittock-Martin R, Parker C, McWilliams K, Lo JC, Go A, Townsend R, Gadegbeku CA, Lash JP, Fink JC, Rahman M, Feldman H, Kusek JW, Xie D, Jaar BG, CRIC Study Group : Retinopathy and chronic kidney disease in the Chronic Renal Insufficiency Cohort (CRIC) study. Arch Ophthalmol 130: 1136–1144, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wong TY, Coresh J, Klein R, Muntner P, Couper DJ, Sharrett AR, Klein BE, Heiss G, Hubbard LD, Duncan BB: Retinal microvascular abnormalities and renal dysfunction: The Atherosclerosis Risk in Communities study. J Am Soc Nephrol 15: 2469–2476, 2004 [DOI] [PubMed] [Google Scholar]
- 6.Edwards MS, Wilson DB, Craven TE, Stafford J, Fried LF, Wong TY, Klein R, Burke GL, Hansen KJ: Associations between retinal microvascular abnormalities and declining renal function in the elderly population: The Cardiovascular Health Study. Am J Kidney Dis 46: 214–224, 2005 [DOI] [PubMed] [Google Scholar]
- 7.Feldman HI, Appel LJ, Chertow GM, Cifelli D, Cizman B, Daugirdas J, Fink JC, Franklin-Becker ED, Go AS, Hamm LL, He J, Hostetter T, Hsu CY, Jamerson K, Joffe M, Kusek JW, Landis JR, Lash JP, Miller ER, Mohler ER, 3rd, Muntner P, Ojo AO, Rahman M, Townsend RR, Wright JT, Chronic Renal Insufficiency Cohort (CRIC) Study Investigators : The Chronic Renal Insufficiency Cohort (CRIC) Study: Design and Methods. J Am Soc Nephrol 14[Suppl 2]: S148–S153, 2003 [DOI] [PubMed] [Google Scholar]
- 8.Lash JP, Go AS, Appel LJ, He J, Ojo A, Rahman M, Townsend RR, Xie D, Cifelli D, Cohan J, Fink JC, Fischer MJ, Gadegbeku C, Hamm LL, Kusek JW, Landis JR, Narva A, Robinson N, Teal V, Feldman HI, Chronic Renal Insufficiency Cohort (CRIC) Study Group : Chronic Renal Insufficiency Cohort (CRIC) Study: Baseline characteristics and associations with kidney function. Clin J Am Soc Nephrol 4: 1302–1311, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hubbard LD, Brothers RJ, King WN, Clegg LX, Klein R, Cooper LS, Sharrett AR, Davis MD, Cai J, Atherosclerosis Risk in Communities Study Group : Methods for evaluation of retinal microvascular abnormalities associated with hypertension/sclerosis in the Atherosclerosis Risk in Communities Study. Ophthalmology 106: 2269–2280, 1999 [DOI] [PubMed] [Google Scholar]
- 10.Early Treatment Diabetic Retinopathy Study Research Group : Grading diabetic retinopathy from stereoscopic color fundus photographs—an extension of the modified Airlie House classification. ETDRS report number 10. Ophthalmology 98[Suppl]: 786–806, 1991 [PubMed] [Google Scholar]
- 11.Wong TY, Klein R, Islam FM, Cotch MF, Folsom AR, Klein BE, Sharrett AR, Shea S: Diabetic retinopathy in a multi-ethnic cohort in the United States. Am J Ophthalmol 141: 446–455, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Klein R, Klein BE, Moss SE, Wong TY: The relationship of retinopathy in persons without diabetes to the 15-year incidence of diabetes and hypertension: Beaver Dam Eye Study. Trans Am Ophthalmol Soc 104: 98–107, 2006 [PMC free article] [PubMed] [Google Scholar]
- 13.Dobre M, Yang W, Chen J, Drawz P, Hamm LL, Horwitz E, Hostetter T, Jaar B, Lora CM, Nessel L, Ojo A, Scialla J, Steigerwalt S, Teal V, Wolf M, Rahman M, CRIC Investigators Association of serum bicarbonate with risk of renal and cardiovascular outcomes in CKD: A report from the Chronic Renal Insufficiency Cohort (CRIC) study. Am J Kidney Dis 62: 670–678, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Anderson AH, Yang W, Hsu CY, Joffe MM, Leonard MB, Xie D, Chen J, Greene T, Jaar BG, Kao P, Kusek JW, Landis JR, Lash JP, Townsend RR, Weir MR, Feldman HI, CRIC Study Investigators : Estimating GFR among participants in the Chronic Renal Insufficiency Cohort (CRIC) Study. Am J Kidney Dis 60: 250–261, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sabanayagam C, Shankar A, Klein BE, Lee KE, Muntner P, Nieto FJ, Tsai MY, Cruickshanks KJ, Schubert CR, Brazy PC, Coresh J, Klein R: Bidirectional association of retinal vessel diameters and estimated GFR decline: The Beaver Dam CKD Study. Am J Kidney Dis 57: 682–691, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Myers CE, Klein R, Knudtson MD, Lee KE, Gangnon R, Wong TY, Klein BEK: Determinants of retinal venular diameter: the Beaver Dam Eye Study. Ophthalmology 119: 2563–2571, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Klein R, Myers CE, Knudtson MD, Lee KE, Gangnon R, Wong TY, Klein BEK: Relationship of blood pressure and other factors to serial retinal arteriolar diameter measurements over time: The Beaver Dam eye study. Arch Ophthalmol 130: 1019–1027, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ooi QL, Tow FK, Deva R, Alias MA, Kawasaki R, Wong TY, Mohamad N, Colville D, Hutchinson A, Savige J: The microvasculature in chronic kidney disease. Clin J Am Soc Nephrol 6: 1872–1878, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]