Abstract
Objective:To investigate and compare the effects of superelastic nickel–titanium and multistranded stainless steel archwires on pain during the initial phase of orthodontic treatment.
Design:A double-blind two-arm parallel design stratified randomized clinical trial.
Setting:A single centre in India between December 2010 and June 2012. A total of 96 participants (48 male and 48 females; 14.1±2.1 years old) were randomized (stratified on age, sex and initial crowding) to superelastic nickel–titanium or multistranded stainless steel archwire groups using a computer-generated allocation sequence.
Methods:We compared 0.016-inch superelastic nickel–titanium and 0.0175-inch multistranded stainless steel wires in 0.022-inch slot (Roth prescription) preadjusted edgewise appliances. The follow-up period was 14 days. Outcome was assessed with a visual analogue scale at baseline and 32 pre-specified follow-up points. Data was analyzed using mixed-effects model analysis.
Results:One participant was lost to follow up and 10 were excluded from the analysis due to bond failure or incomplete questionnaire answers. Ultimately, 85 participants (42 males and 43 females; 14.1±2.0 years old) were analysed for the final results. No statistically significant difference was found for overall pain [F value = 2.65, degrees of freedom (df) = 92.6; P = 0.1071]. However, compared to multistranded stainless steel wires, pain in subjects with superelastic nickel–titanium archwires was significantly greater at 12 h (t = 2.34; P = 0.0193), as well as at day 1 in the morning (t = 2.21, P = 0.0273), afternoon (t = 2.11, P = 0.0346) and at bedtime (t = 2.03, P = 0.042).
Conclusion:For overall pain, there was no statistically significant difference between the two wires. However, subjects with superelastic nickel–titanium archwires had a significantly higher pain at peak level.
Keywords: Orthodontic pain, initial archwires, alignment
Introduction
Orthodontic force application leads to periodontal ligament tissue injury and the initiation of acute inflammatory processes. Subsequent production of pro-inflammatory mediators such as prostaglandins, substance P and cytokines plays an important role in the mediation of orthodontic pain.1 Therefore, it is recommended that light force should be used during orthodontic treatment to minimize tissue damage and subsequent pain and discomfort.2–5 Multistranded stainless steel and nickel–titanium (NiTi) alloy archwires are commonly used during the initial levelling and aligning phase of fixed orthodontic treatment because these wires are closest to fulfilling the ideal requirements of an initial archwire.6
Previous authors have failed to demonstrate a significant difference in the aligning capabilities of superelastic nickel–titanium and multistranded stainless steel archwires.7,8 These findings have been confirmed by recent clinical9 and laboratory10 studies using a pre-adjusted edgewise appliance (0.022-inch slot) system during alignment of the mandibular anterior segment. These studies9,10 highlight the fact that superelastic nickel titanium wires are not superior to multistranded stainless steel, even in the mandibular anterior segment where small inter-bracket widths decrease the relative length of the archwire, which might be expected to favour superelastic nickel titanium archwires.8
Besides clinical efficiency, another important consideration for initial arch wire selection should be minimal pain and discomfort because the prevalence of pain during the initial phase of fixed orthodontic treatment is high.11,12 Surprisingly, this important topic has been largely ignored in clinical practice as well as research, as evidenced by the scarcity of publications. In the last 20 years, no study has compared these two archwire types for pain, though the effect of bracket design on pain during the initial phase of fixed orthodontic treatmenthas been investigated.13,14 Only one clinical trial15 published in 1992 compared superelastic nickel titanium and multistranded stainless wires for orthodontic pain. However, it is unclear whether their sample size was based on priori power analysis and whether groups were appropriately balanced for demographic and clinical characteristics. As pain is a subjective response, it can be significantly influenced by several factors, including age15 and sex16 and clinical characteristics such as orthodontic force level.17 The degree of crowding has a direct effect on inter-bracket distance, which can significantly influence deactivation forces of initial archwires.18
Therefore, the present study was designed as a stratified (age, sex and initial crowding) randomized clinical trial to investigate and compare the effects of superelastic nickel titanium and multistranded stainless steel archwires on orthodontic pain over a period of 2 weeks.
Material and methods
We conducted a single-centre, double-blind, parallel two-arm (1∶1 allocation ratio) stratified randomized controlled trial in India between December 2010 and June 2012. A total of 96 participants met all inclusion criteria and were enrolled in the study after providing written informed consent. The study protocol was approved by a local ethics review committee of the Indian Medical Association in Jalandhar, Punjab, India on 20 December 2010.
Inclusion criteria were: (1) 11- to -17-year-old male and females who required fixed orthodontic treatment; (2) moderate-to-severe crowding (4–9 mm) in the mandibular anterior segment that was not severe enough to prevent bracket engagement, patients with severe crowding related to one or two teeth (such as blocked out lateral incisors) were not included; (3) eruption of all mandibular anterior teeth; (4) no history of medical problems/medication that could influence pain perception; and (5) informed and witnessed consent from the minor participant and their parent/guardian.
Exclusion criteria were: (1) presence of a severe deep bite that could affect bracket placement on the mandibular anterior teeth; (2) malocclusion correction required treatment procedures other than continuous arch wire mechanics; (3) participants taking pain medications for chronic pain; (4) participants with a positive history of dental pain or pain in the orofacial region; (5) a medical condition that precluded the use of a fixed orthodontic appliance (e.g. allergy to nickel, recent history of epileptic seizure or physician’s consent could not be obtained, etc.).
Initial crowding assessment was done by using Little’s Irregularity index.19 Decisions regarding extraction, as and when required, were based on comprehensive diagnosis and treatment planning. After extractions, participants were scheduled for appointments at least 2-week post-extraction to allow a standardized minimum healing time since one of the prerequisites before trial initiation was that participants should be pain free.
On the first day of orthodontic treatment but before the bonding procedure, booklets containing the pain assessment scale and written instructions were provided to participants for the baseline pain assessment. Verbal instructions and guidance during the baseline assessment were provided to familiarize the participants with the pain assessment procedure. For all participants, the bonding procedure and initial wire placement were carried out between 10 and 11 o’ clock in the morning, though on different days. This was to ensure that the follow-up time points for pain assessment were the same.
Preadjusted Edgewise Appliances (PEA) with 0.022×0.028-inch slot twin brackets (Roth prescription, Gemini Metal Brackets; 3M Unitek Corporation, Monrovia, CA, USA) were bonded directly to the mandibular dentition using light-cure composite resin (Transbond XT; 3M Unitek Corporation). We employed either 0.0175-inch multistranded stainless steel (Six-stranded, Unitek™ Coaxial Wire; 3M Unitek Corporation) or 0.016-inch superelastic nickel–titanium (austenitic active, preformed ovoid, superelastic arch wire; 3M Unitek Corporation) as interventions. Only the mandibular arch was bonded until the completion of the study. Intervention and follow-up were done by the first and second authors, who are both qualified orthodontists. After initial arch wire placement, participants were discharged with the booklets containing the pain assessment scale and written instructions. Participants were requested to report back after 14 days (follow-up period), unless they experienced an emergency, such as mucosal injury or damage to the appliance.
Outcome was assessed by using the Visual Analogue Scale (VAS), which is a 100-mm long horizontal line where one end corresponds to ‘no pain’ and the other end indicates ‘worst pain possible’.20 The VAS is a valid and reliable scale for pain assessment.21 Pain was assessed at baseline and at 32 pre-specified follow-up (post-wire placement) time points.
Although the literature shows that there are varying pain perceptions during different dental occlusal positions, we decided to assess pain only at the rest position because participants showed a reluctance to record multiple measurements during the pilot study. Assessing pain at the rest position, while touching the front teeth, and while touching the back teeth triples the number of pain assessments at each time point, which could make patients unenthusiastic and, therefore, could affect cooperation during the trial, especially in one that has multiple time points.
Participants marked a line across the scale corresponding to perceived pain at each time point. The mark was measured from the left margin of the line to the nearest millimetre to quantify the pain and recorded a VAS score in mm. The VAS score was measured by trained dental assistants (blinded to the study) using a manual 0.1-mm calibrated Vernier caliper (manual type). The first and second authors measured 20 randomly selected VAS scales, independently, and the intraclass correlation coefficient of 0.95 suggested excellent reproducibility and reliability.
For pain relief, participants were allowed to take any over-the-counter analgesic. However, participants were asked to record pain (VAS score) before taking the medication in order to minimize the effect of the analgesic on the pain recording. No restriction was imposed regarding the timing or frequency of analgesic consumption. It is quite possible that analgesic consumption, especially before recording the pain, could lead to bias in pain assessment. However, it is unethical to ask the participant not to take medication or to control the timing or frequency of analgesic consumption.
Sample size was based on power analysis (Stata/SE 10.0 software, College Station, TX, USA) for a repeated measure design with 1 baseline and 32 follow-up repeated measurements (r = 0.15) to detect a 3-mm (SD 10 for each group, Cohen’s effect size 0.3) mean difference on a 100-mm VAS. The sample size determining assumptions, such as effect size and correlation coefficient (r) between follow-up repeated measurement, were based on pilot study results. We determined that 42 participants per group (84 in total) were required to achieve 90% power with a significance level of 0.05. Considering possible drop out of 10–15% during follow-up, it was decided to enrol at least 95 participants.
The randomization schedule was prepared by using ralloc procedure (Stata/SE 10.0 software) to enrol 96 participants into superelastic nickel titanium and multistranded stainless steel groups using stratified block (size 4) randomization. A statistician generated the random allocation sequence, and the dental assistant helped enrol and conceal participant allocation using the opaque sealed envelope method. The stratification factors for randomization were age, sex, and initial crowding (moderate 4–6 mm, severe >6–9 mm). Age groups 11–14 and 14–17 years were selected because these represent preadolescent and adolescent age groups, respectively.22
Statistical analysis
Data was analysed with SAS 9.2 software (SAS Institute Inc., Cary, NC, USA) Demographic and clinical characteristics, including frequency, arithmetic mean and standard deviation calculated using descriptive statistics.
Mixed model analysis (PROC MIXED) was employed to analyse repeated measure data (VAS score) by using the Restricted Maximum Likelihood method of estimation.23 Both random and repeated statements were used to model the variance and covariance structures, respectively. Random intercept was used with Unstructured variance matrix for random effects, whereas SP(POW) (spatial power law) covariance structure was used for repeated measures. To fit a time-series-type covariance structure for unequally spaced longitudinal repeated measurements in which the correlations between follow-up measurements change rapidly as a function of time, the spatial structures such as SP(POW) (spatial power law), SP(GAU) (Gaussian) and SP(SPH) (spherical) are appropriate for modelling covariance structures.23 These covariance structures were evaluated, and the best-fitting model was selected based on log likelihood ratio test and Akaike’s information criterion (AIC), AIC small sample corrected and Bayesian information criterion (smaller is better). The SP(POW) structure was the best fitting covariance structure, which is a direct generalization of the Autoregressive First Order AR (1) covariance structure for equally spaced data.23 The Tukey-Kramer method was used to adjust P-values of Pairwise Comparisons of LS-Means (LS-Means), as recommended by Westfall et al.24 for unbalanced design. The null hypotheses were tested at a significance level of 0.05.
Results
Out of 168 participants assessed for eligibility, 96 met the inclusion criteria and enrolled in the trial. One participant was lost to follow up, and 10 were excluded from the analysis due to bond failure or incomplete questionnaires. Therefore, a total of 85 participants (42 males and 43 females; mean age 14.1±2.0 years) were included in the analysis as shown in the CONSORT flow diagram (Figure 1). Numbers analysed and the demographic/clinical characteristics are shown in Table 1. VAS score data (mean, SD) are shown in Table 2. Figure 2 shows the mean profile plots of VAS scores.
Figure 1.
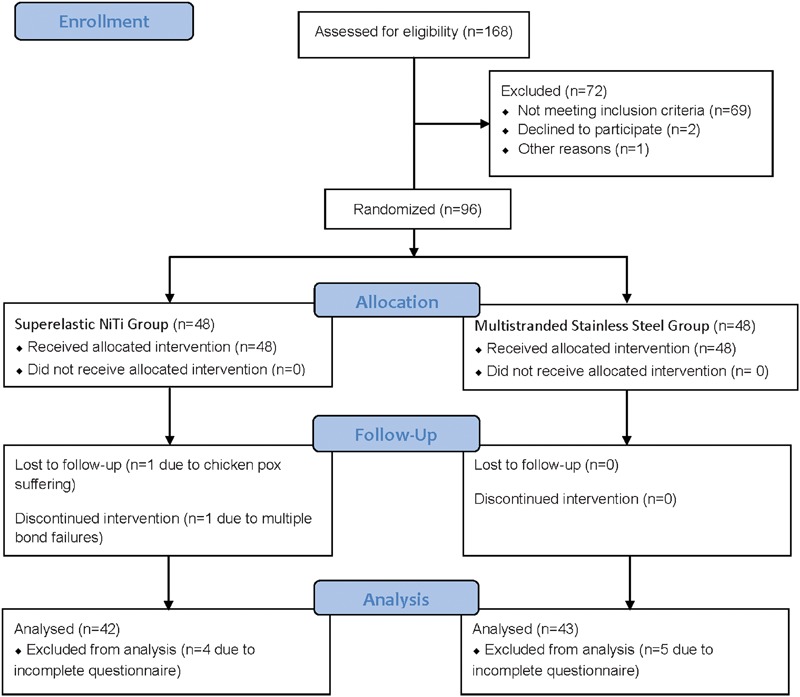
CONSORT flow diagram
Table 1. Baseline demographic and clinical characterstics data.*.
| Superelastic NiTi (n = 42) | Multistranded stainless steel (n = 43) | ||
| Age (years) | 14.2 (1.9) | 13.9 (2.0) | |
| Sex | Male | 21 (50%) | 21 (48.8%) |
| Female | 21 (50%) | 22 (51.2%) | |
| Initial crowding (mm) | 6.5 (1.3) | 6.6 (1.4) | |
| Extractions | No | 18 (42.9%) | 17 (39.6%) |
| Yes | 24 (57.1%) | 26 (60.4%) |
Data numbers (%) or means (SD).
Table 2. Vas scores* at each time point.
| Group | |||||
| Superelastic NiTi (n = 42) | Multistranded stainless Steel (n = 43) | ||||
| Time point | Description | Mean | Standard deviation | Mean | Standard deviation |
| 0 | Baseline | 0 | 0 | 0 | 0 |
| 1 | 1 h | 5.0 | 3.0 | 3.7 | 2.1 |
| 2 | 2 h | 6.1 | 3.0 | 4.2 | 2.2 |
| 3 | 4 h | 8.6 | 4.0 | 8.4 | 4.3 |
| 4 | 6 h | 14.6 | 7.0 | 12.7 | 6.0 |
| 5 | 12 h | 27.0 | 9.1 | 24.4 | 10.8 |
| 6 | Day 1 morning | 28.8 | 11.0 | 26.4 | 9.0 |
| 7 | Day 1 afternoon | 27.8 | 9.1 | 25.4 | 8.6 |
| 8 | Day 1 bedtime | 27.5 | 11.2 | 25.2 | 8.2 |
| 9 | Day 2 morning | 24.6 | 10.4 | 23.0 | 5.8 |
| 10 | Day 2 afternoon | 22.2 | 9.6 | 21.6 | 6.0 |
| 11 | Day 2 bedtime | 20.6 | 10.2 | 20.3 | 6.5 |
| 12 | Day 3 morning | 18.3 | 9.2 | 17.9 | 6.3 |
| 13 | Day 3 afternoon | 16.1 | 8.2 | 16.5 | 5.7 |
| 14 | Day 3 bedtime | 15.6 | 7.6 | 15.0 | 3.5 |
| 15 | Day 4 morning | 14.2 | 6.8 | 12.9 | 2.5 |
| 16 | Day 4 afternoon | 12.9 | 4.6 | 11.6 | 2.0 |
| 17 | Day 4 bedtime | 11.3 | 5.3 | 10.1 | 3.1 |
| 18 | Day 5 morning | 9.8 | 4.3 | 8.5 | 3.0 |
| 19 | Day 5 afternoon | 8.3 | 4.6 | 7.1 | 2.5 |
| 20 | Day 5 bedtime | 6.4 | 3.3 | 5.9 | 2.3 |
| 21 | Day 6 morning | 5.5 | 3.4 | 4.9 | 2.5 |
| 22 | Day 6 afternoon | 4.9 | 2.5 | 4.4 | 1.8 |
| 23 | Day 6 bedtime | 4.4 | 1.6 | 3.7 | 1.5 |
| 24 | Day 7 morning | 3.5 | 1.5 | 3.2 | 1.3 |
| 25 | Day 7 afternoon | 2.7 | 0.9 | 2.9 | 0.8 |
| 26 | Day 7 bedtime | 2.3 | 0.9 | 2.5 | 0.8 |
| 27 | Day 10 morning | 2.5 | 1.2 | 2.1 | 1.1 |
| 28 | Day 10 afternoon | 2.3 | 1.3 | 2.0 | 1.1 |
| 29 | Day 10 bedtime | 2.2 | 0.8 | 1.9 | 1.0 |
| 30 | Day 14 morning | 2.1 | 0.9 | 1.8 | 0.9 |
| 31 | Day 14 afternoon | 1.8 | 1.1 | 1.7 | 1.2 |
| 32 | Day 14 bedtime | 1.8 | 0.6 | 1.5 | 0.7 |
Figure 2.
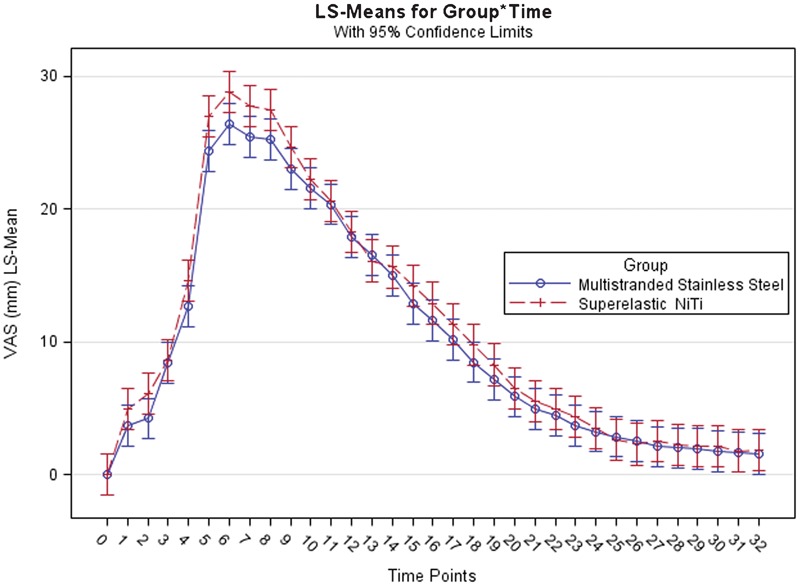
Least Square Means (LS-Means) profile plot of VAS scores (please refer to Table 2 for the description of time points)
The results of the mixed effect model analysis are shown in Table 3. Time had the most significant effect on pain (F value = 146.63, df = 2501, P<0.0001). There was no statistically significant difference between superelastic nickel–titanium and multistranded stainless steel wires for mean average VAS score across all time points (F value = 2.65, df = 92.6, P = 0.1071). However, the significant interaction between Group and Time (F value = 1.57, df = 2501, P = 0.0226) highlights the fact that the difference for VAS score between superelastic nickel–titanium and multistranded stainless steel wires was not insignificant across all the time points. This implies that there was a significant difference between these two wires for pain during the trial period.
Table 3. Effect of superelastic NiTi versus multistranded stainless steel wires on orthodontic pain.*.
| Effect | Numerator DF† | Denominator DF* | F value | Pr>F |
| Group | 1 | 92.63 | 2.65 | 0.1071 |
| Time | 32 | 2501 | 146.63 | <0.0001 |
| Group×Time | 32 | 2501 | 1.57 | 0.0226 |
Type III tests of fixed effects.
Kenward Roger Degree of Freedom.
The results of pairwise comparisons for VAS score at each time point are shown in Table 4. The significant differences (P<0.05) are highlighted in bold italics. Compared to multistranded stainless steel, the pain produced by superelastic nickel–titanium wires was significantly greater at 12 h (t = 2.34, P = 0.0193) and on the morning (t = 2.21, P = 0.0273), afternoon (t = 2.11, P = 0.0346) and bedtime (t = 2.03, P = 0.042) of day 1. These findings correspond to the LS-Means profile plot shown in Figure 2.
Table 4. Pairwise comparisons of superelastic NiTi versus multistranded stainless steel wires for effect on pain at each time point.
| Time | Group* | Estimate | SE† | DF‡ | t value | P¶ | 95% confidence interval | ||
| Lower | Upper | ||||||||
| Baseline | Multistranded | Superelastic | −1.81E-13 | 1.1125 | 1047 | 0 | 1 | −2.1815 | 2.1815 |
| 1 h | Multistranded | Superelastic | −1.3053 | 1.1125 | 1047 | −1.17 | 0.2408 | −3.4868 | 0.8762 |
| 2 h | Multistranded | Superelastic | −1.8545 | 1.1125 | 1047 | −1.67 | 0.0956 | −4.036 | 0.327 |
| 4 h | Multistranded | Superelastic | −0.245 | 1.1125 | 1047 | −0.22 | 0.8257 | −2.4266 | 1.9365 |
| 6 h | Multistranded | Superelastic | −1.9599 | 1.1125 | 1047 | −1.76 | 0.0782 | −4.1415 | 0.2216 |
| 12 h | Multistranded | Superelastic | −2.6041 | 1.1125 | 1047 | −2.34 | 0.0193 | −4.7856 | −0.4226 |
| Day 1 morning | Multistranded | Superelastic | −2.4572 | 1.1125 | 1047 | −2.21 | 0.0273 | −4.6387 | −0.2757 |
| Day 1 afternoon | Multistranded | Superelastic | −2.3516 | 1.1125 | 1047 | −2.11 | 0.0346 | −4.5331 | −0.1701 |
| Day 1 bedtime | Multistranded | Superelastic | −2.263 | 1.1125 | 1047 | −2.03 | 0.042 | −4.4445 | −0.08149 |
| Day 2 morning | Multistranded | Superelastic | −1.6196 | 1.1125 | 1047 | −1.46 | 0.1456 | −3.8011 | 0.5619 |
| Day 2 afternoon | Multistranded | Superelastic | −0.6327 | 1.1125 | 1047 | −0.57 | 0.5696 | −2.8142 | 1.5488 |
| Day 2 bedtime | Multistranded | Superelastic | −0.2781 | 1.1125 | 1047 | −0.25 | 0.8026 | −2.4597 | 1.9034 |
| Day 3 morning | Multistranded | Superelastic | −0.3784 | 1.1125 | 1047 | −0.34 | 0.7338 | −2.5599 | 1.8031 |
| Day 3 afternoon | Multistranded | Superelastic | 0.4317 | 1.1125 | 1047 | 0.39 | 0.698 | −1.7498 | 2.6132 |
| Day 3 bedtime | Multistranded | Superelastic | −0.6619 | 1.1125 | 1047 | −0.59 | 0.5519 | −2.8434 | 1.5196 |
| Day 4 morning | Multistranded | Superelastic | −1.2825 | 1.1125 | 1047 | −1.15 | 0.2491 | −3.4641 | 0.899 |
| Day 4 afternoon | Multistranded | Superelastic | −1.3367 | 1.1125 | 1047 | −1.2 | 0.2297 | −3.5182 | 0.8448 |
| Day 4 bedtime | Multistranded | Superelastic | −1.2189 | 1.1125 | 1047 | −1.1 | 0.2733 | −3.4005 | 0.9626 |
| Day 5 morning | Multistranded | Superelastic | −1.3085 | 1.1125 | 1047 | −1.18 | 0.2396 | −3.49 | 0.873 |
| Day 5 afternoon | Multistranded | Superelastic | −1.1344 | 1.1125 | 1047 | −1.02 | 0.308 | −3.3159 | 1.0472 |
| Day 5 bedtime | Multistranded | Superelastic | −0.5856 | 1.1125 | 1047 | −0.53 | 0.5987 | −2.7671 | 1.596 |
| Day 6 morning | Multistranded | Superelastic | −0.5915 | 1.1125 | 1047 | −0.53 | 0.595 | −2.773 | 1.59 |
| Day 6 afternoon | Multistranded | Superelastic | −0.4731 | 1.1125 | 1047 | −0.43 | 0.6707 | −2.6546 | 1.7084 |
| Day 6 bedtime | Multistranded | Superelastic | −0.6648 | 1.1125 | 1047 | −0.6 | 0.5502 | −2.8464 | 1.5167 |
| Day 7 morning | Multistranded | Superelastic | −0.2239 | 1.1125 | 1047 | −0.2 | 0.8405 | −2.4054 | 1.9576 |
| Day 7 afternoon | Multistranded | Superelastic | 0.2017 | 1.1125 | 1047 | 0.18 | 0.8561 | −1.9798 | 2.3833 |
| Day 7 bedtime | Multistranded | Superelastic | 0.2182 | 1.1125 | 1047 | 0.2 | 0.8445 | −1.9633 | 2.3998 |
| Day 10 morning | Multistranded | Superelastic | −0.4228 | 1.1125 | 1047 | −0.38 | 0.7039 | −2.6044 | 1.7587 |
| Day 10 afternoon | Multistranded | Superelastic | −0.2619 | 1.1125 | 1047 | −0.24 | 0.8139 | −2.4434 | 1.9196 |
| Day 10 bedtime | Multistranded | Superelastic | −0.2209 | 1.1125 | 1047 | −0.2 | 0.8426 | −2.4024 | 1.9606 |
| Day 14 morning | Multistranded | Superelastic | −0.3202 | 1.1125 | 1047 | −0.29 | 0.7735 | −2.5017 | 1.8613 |
| Day 14 afternoon | Multistranded | Superelastic | −0.1038 | 1.1125 | 1047 | −0.09 | 0.9257 | −2.2853 | 2.0777 |
| Day 14 bedtime | Multistranded | Superelastic | −0.2903 | 1.1125 | 1047 | −0.26 | 0.7941 | −2.4718 | 1.8912 |
Multistranded: multistranded stainless steel; superelastic: superelastic NiTi.
Standard error.
Kenwardroger Degree of Freedom.
Significance level P<0.05.
Throughout the study, no harm was done to the participants in terms of pain experienced, which was similar to what it would have been if participants were not part of the study. Decisions regarding extraction were based on comprehensive diagnosis and treatment planning. There was no effect on total duration of treatment because the most recent clinical study concluded that both wire types are equally efficient with a PEA.9
Discussion
In this clinical trial, orthodontic pain began 1 h after initial arch wire placement, reached a peak on the morning of day 1 (24 h), and gradually decreased thereafter. However, even after 14 days, the mean VAS score did not reach zero (Figure 2). There was no statistical significant difference between superelastic nickel–titanium and multistranded stainless steel wire for overall pain during the entire study. However, compared to multistranded stainless steel wire, subjects who received superelastic nickel–titanium wire reported greater pain at peak from 12 h after placement to bedtime on day 1.
The observed trend of pain perhaps reflect the underlying biological responses to orthodontic force application. Interleukin-1beta (IL-1beta) is the first mediator to regulate bone remodelling in response to orthodontic force, and it also plays a significant role in orthodontic pain by inducing the secretion of pain-producing pro-inflammatory mediators.1,25 A recent study17 demonstrated that the IL-1beta concentration increases after 1 h of orthodontic force application, peaks after 24 h, and subsequently declines approximately to baseline in 1-week to 1-month time period. In another study,26 the concentration of IL-1beta declined to normal only towards the end of the 3-week study period. These findings could explain the pain trend observed in the present trial, where pain started 1 h after initial arch wire placement, peaked after 24 h, then began to decline. However, pain did not decrease to baseline (zero), even after 2 weeks of force application.
The findings of our trial both support and refute results from a previous clinical trial investigating pain during initial orthodontic tooth alignment with fixed appliances.15 The results are in accordance in that we did not find a statistically significant difference between the two wires for overall pain experience. However, the pain trend showed some interesting differences. The previous study15 reported that from days 2 to 5, there was less pain associated with the superelastic nickel–titanium wire. However, subjects who received this wire in the present investigation did not report less pain at any assessment (Figure 2). Furthermore, the previous study reported no significant difference in pain between the two wires during the entire study. However, the subjects in the current work reported that superelastic nickel–titanium wires produced greater pain, especially at peak plateau from 12 h to bedtime of day 1 (Table 4 and Figure 2).
These differences between the previous report15 and our trial could be explained by the fact that different arch wire material and dimensions were used in these studies. The previous study compared 0.014-inch superelastic nickel–titanium and 0.015-inch, three-stranded Twistflex multistranded stainless steel wires. In contrast, we compared 0.016-inch superelastic nickel–titanium and 0.0175-inch, six-stranded, coaxial wire (five strands wrapped around a core wire). The variations in the wire dimensions and multistranded wire design can influence the force they deliver.
Although there is great variation in force values with different nickel–titanium wires of the same diameter, in general an increase in superelastic nickel–titanium wire diameter from 0.014 to 0.016 inch increases the force level by 50%.27 In comparison, an increase in multistranded wire diameter from 0.015 to 0.0175 inch only increases the force by 20–30%.28 Therefore, the increase in superelastic nickel–titanium diameter from 0.014 to 0.016 inch might have resulted in a substantial (50%) increase in force level compared to only a 20–30% increase for multistranded wires with an increase in diameter from 0.015 to 0.0175 inch. Furthermore, the 20–30% increase in force level for the multistranded wire could have been negated to some extent because coaxial wires deliver less force than twisted wires,28 and the increase in the number of strands (from three strands to six strands) makes multistranded wires more flexible and lessens the force.29
There is much controversy regarding the question of whether light versus heavy forces have any effect on orthodontic tooth movement and associated pain. Various histological studies and clinical trials suggest that light forces are capable of producing efficient tooth movement with less tissue damage and subsequent pain, whereas heavy forces cause greater periodontal compression and thus more pain.2–5 However, few authors reported that application of heavier forces per unit area increases the rate of biological response,30 and there are no statistically significant correlations among the initial tooth positions, applied force levels and experienced pain.31
However, one of the most recent studies carried out to examine the relationship between amount of force (heavy versus low) concluded that application of heavy force does not significantly enhance the rate of tooth movement, but compared to light force, it does produce significantly greater pain at the peak level of pain, i.e. 24 h after force application.17 The study further concluded that the effect of heavy forces on orthodontic pain was due to significantly greater increase in IL-1beta concentration as compared to light forces. Perhaps this could explain the difference with regard to pain among superelastic nickel–titanium wire and multistranded stainless steel wires at the peak level observed in the present trial. The average plateau force produced by the 0.016-inch superelastic nickel–titanium is around 133 g of force over a deflection of 4 mm.27 At a similar deflection of 3 mm, the force produced by 0.0175-inch six-stranded coaxial multistranded stainless steel wire is around 95 g.28 The greater force level associated with superelastic nickel–titanium wire 27–29 could have resulted in increased concentrations of IL-1beta at peak level, which could cause increased pain. Since there was a plateau of peak-level pain, it is quite possible that the concentration of IL-1beta might have been higher from 12 h to bedtime on day 1. Unfortunately, the previous study17 examined IL-1beta concentrations at 1 h, 24 h, 1 week, and so on; therefore, further studies are required to explore the precise relationships among orthodontic force level, IL-1beta concentration and orthodontic pain.
We compared the two most commonly used initial archwires in moderate-to-severe crowding conditions that are commonly encountered during orthodontic treatment. Therefore, our findings can be generalized to most settings involving the levelling and alignment phase of fixed orthodontic treatment. Furthermore, robust conclusions can be drawn from the results because the sample size was based on the priori power analysis, randomization was stratified on known confounding factors, the longitudinal data were comprised of a large number of repeated measures; and the statistical analysis involved a mixed-effect model analysis that considered the correlated nature of data and inter-individual variations in the form of random effects.
The weaknesses and limitations of this study mostly pertain to the non-consideration of a few factors that could have influenced the outcome. Although an attempt was made to control all such factors (age, sex and initial crowding), psychological factors such as anxiety/depression and hormonal fluctuation in females during menstruation cycle were not taken into account and could have influenced the outcome of the trial. Furthermore, ‘as and when required’ use of analgesics could have also affected the results. Future studies should take into account all such factors that can influence pain perception.
During the initial levelling and aligning phase of fixed orthodontic treatment, the initial wire should exert light continuous forces to facilitate the most efficient tooth movement with the least possible tissue damage and pain. Because recent clinical9 and laboratory10 studies have concluded that both wire types are equally efficient, the wire choice could be selected based on patient pain and discomfort. Our study, perhaps for the first time, demonstrates that during the peak level of pain, multistranded stainless steel wire produces significantly less pain compared to superelastic nickel–titanium archwires. Therefore, multistranded stainless steel wires can be an important and viable alternative to superelastic nickel–titanium during the initial levelling and aligning phase of fixed orthodontic treatment because pain produced by these wires at the peak level is less than that produced by superelastic nickel–titanium.
Conclusion
During the peak level of pain following the placement of an initial aligning archwire (12 h to day 1 bedtime), subjects with superelastic nickel–titanium wire reported significantly greater pain compared to those with multistranded stainless steel. However, there was no statistically significant difference between these archwires for mean average pain across all time points.
References
- 1.Giannopoulou C, Dudic A, Kiliaridis S. Pain discomfort and crevicular fluid changes induced by orthodontic elastic separators in children. J Pain. 2006;7:367–76. doi: 10.1016/j.jpain.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 2.Reitan K. Some factors determining the evaluation of forces in orthodontics. Am J Orthod. 1957;43:32–45. [Google Scholar]
- 3.Weinstein S. Minimum forces in tooth movement. Am J Orthod. 1967;53:881–903. doi: 10.1016/0002-9416(67)90163-7. [DOI] [PubMed] [Google Scholar]
- 4.Storey E, Smith R. Force in orthodontics and its relation to tooth movement. Aust J Dent. 1952;56:11–18. [Google Scholar]
- 5.Gianelly A A, Goldman H M, (eds.). Tooth Movement. Biological Basis of Orthodontics. Philadelphia, PA: Lea and Febiger; 1971, 116–204. [Google Scholar]
- 6.Quintao CC, Cal-Neto JP, Menezes LM, Elia CN. Force-deflection properties of initial orthodontic archwires. World J Orthod. 2009;10:29–32. [PubMed] [Google Scholar]
- 7.Jones ML, Staniford H, Chan C. Comparison of superelastic NiTi and multistranded stainless steel wires in initial alignment. J Clin Orthod. 1990;24:611–13. [PubMed] [Google Scholar]
- 8.Evans TJ, Jones ML, Newcombe RG. Clinical comparison and performance perspective of three aligning arch wires. Am J Orthod Dentofacial Orthop. 1998;114:32–39. doi: 10.1016/s0889-5406(98)70234-3. [DOI] [PubMed] [Google Scholar]
- 9.Sandhu SS, Shetty VS, Mogra S, Varghese J, Sandhu J, Sandhu JS. Efficiency, behavior, and clinical properties of superelastic NiTi versus multistranded stainless steel wires. Angle Orthod. 2012;82:915–21. doi: 10.2319/100311-622.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Badran SA, Orr JF, Stevenson M, Burden DJ. Photo-elastic stress analysis of initial alignment archwires. Eur J Orthod. 2003;25:117–25. doi: 10.1093/ejo/25.2.117. [DOI] [PubMed] [Google Scholar]
- 11.Erdinc AM, Dincer B. Perception of pain during orthodontic treatment with fixed appliances. Eur J Orthod. 2004;26:79–85. doi: 10.1093/ejo/26.1.79. [DOI] [PubMed] [Google Scholar]
- 12.Scheurer PA, Firestone AR, Burgin WB. Perception of pain as a result of orthodontic treatment with fixed appliances. Eur J Orthod. 1996;18:349–57. doi: 10.1093/ejo/18.4.349. [DOI] [PubMed] [Google Scholar]
- 13.Scott P, Sherriff M, Dibiase AT, Cobourne MT. Perception of discomfort during initial orthodontic tooth alignment using a self-ligating or conventional bracket system: a randomized clinical trial. Eur J Orthod. 2008;30:227–32. doi: 10.1093/ejo/cjm131. [DOI] [PubMed] [Google Scholar]
- 14.Pringle AM, Petrie A, Cunningham SJ, McKnight M. Prospective randomized clinical trial to compare pain levels associated with 2 orthodontic fixed bracket systems. Am J Orthod Dentofacial Orthop. 2009;136:160–67. doi: 10.1016/j.ajodo.2007.08.032. [DOI] [PubMed] [Google Scholar]
- 15.Jones M, Chan C. The pain and discomfort experienced during orthodontic treatment: A randomized controlled clinical trial of two initial aligning arch wires. Am J Orthod Dentofacial Orthop. 1992;102:373–81. doi: 10.1016/0889-5406(92)70054-e. [DOI] [PubMed] [Google Scholar]
- 16.Bergius M, Berggren U, Kiliaridis S. Experience of pain during an orthodontic procedure. Eur J Oral Sci. 2002;110:92–98. doi: 10.1034/j.1600-0722.2002.11193.x. [DOI] [PubMed] [Google Scholar]
- 17.Luppanapornlarp S, Kajii TS, Surarit R, Iida J. Interleukin-1beta levels, pain intensity, and tooth movement using two different magnitudes of continuous orthodontic force. Eur J Orthod. 2010;32:596–601. doi: 10.1093/ejo/cjp158. [DOI] [PubMed] [Google Scholar]
- 18.Schumacher HA, Bourauel C, Drescher D. The deactivation behavior and effectiveness of different orthodontic leveling arches — a dynamic analysis of the force. Fortschr Kieferorthop. 1992;53:273–85. doi: 10.1007/BF02325076. [DOI] [PubMed] [Google Scholar]
- 19.Little RM. The irregularity index: a quantitative score of mandibular anterior alignment. Am J Orthod. 1975;68:554–63. doi: 10.1016/0002-9416(75)90086-x. [DOI] [PubMed] [Google Scholar]
- 20.Huskisson EC. Visual analogue scales. In Melzack R (ed.). Pain measurement and assessment. New York Raven Press, 1983, 33–37. [Google Scholar]
- 21.Breivik H, Borchgrevink PC, Allen SM, et al. Assessment of pain. Br J Anaesth. 2008;101:17–24. doi: 10.1093/bja/aen103. [DOI] [PubMed] [Google Scholar]
- 22.Corsaro WA. The Sociology of Childhood, 2nd Edn. Thousand Oaks, CA: SAGE Publications, 2004, 191 and 24. [Google Scholar]
- 23.Littell RC, George AM, Walter WS, Russell DW, Oliver S. 2006. SAS® for Mixed Models, 2nd Edn. Cary, NC: SAS Publishing. [Google Scholar]
- 24.Westfall PH, Tobias RD, Wolfinger RD. 2011. Multiple comparisons and multiple tests using SAS, 2nd Edn. Cary, NC: SAS Publishing. [Google Scholar]
- 25.Davidovitch Z, Nicolay O, Ngan P, Shanfeld J. Neurotransmitters, cytokines and the control of alveolar bone remodeling in orthodontics. Dent Clin North Am. 1988;32:411–35. [PubMed] [Google Scholar]
- 26.Lee KJ, Park YC, Yu HS, Choi SH, Yoo YJ. Effects of continuous and interrupted orthodontic force on interleukin-1beta and prostaglandin E2 production in gingival crevicular fluid. Am J Orthod Dentofacial Orthop. 2004;125:168–77. doi: 10.1016/j.ajodo.2003.03.006. [DOI] [PubMed] [Google Scholar]
- 27.Lombardol L, Marafioti M, Stefanonif F, Mollica F, Siciliani G. Load deflection characteristics and force level of nickel titanium initial archwires. Angle Orthod. 2012;82:507–21. doi: 10.2319/032511-213.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Taneja P, Duncanson MG, Khajotia SS, Nanda RS. Deactivation force-deflection behavior of multistranded stainless steel wires. Am J Orthod Dentofacial Orthop. 2003;124:61–68. doi: 10.1016/s0889-5406(03)00309-3. [DOI] [PubMed] [Google Scholar]
- 29.Kusy RP, Dilley GJ. Elastic modulus of a triple-stranded stainless steel archwire via three and four point bending. J Dent Res. 1984;63:1232–40. doi: 10.1177/00220345840630101401. [DOI] [PubMed] [Google Scholar]
- 30.Hixon EH, Aitikian H, Callow G, McDonald H, Tacy RJ. Optimal force, differential force, and anchorage. Am J Orthod. 1969;55:437–51. doi: 10.1016/0002-9416(69)90083-9. [DOI] [PubMed] [Google Scholar]
- 31.Jones ML, Richmond S. Initial tooth movement: force application and pain — a relationship? Am J Orthod. 1985;88:111–16. doi: 10.1016/0002-9416(85)90234-9. [DOI] [PubMed] [Google Scholar]


