Abstract
Background
Circulatory system diseases are the first cause of death in Brazil.
Objective
To analyze the evolution of mortality caused by heart failure, by ischemic heart diseases and by ill-defined causes, as well as their possible relations, in Brazil and in the geoeconomic regions of the country (North, Northeast, Center-West, South and Southeast), from 1996 to 2011.
Methods
Data were obtained from DATASUS and death declaration records with codes I20 and I24 for acute ischemic diseases, I25 for chronic ischemic diseases, and I50 for heart failure, and codes in chapter XIII for ill-defined causes, according to geoeconomic regions of Brazil, from 1996 to 2011.
Results
Mortality rates due to heart failure declined in Brazil and its regions, except for the North and the Northeast. Mortality rates due to acute ischemic heart diseases increased in the North and Northeast regions, especially from 2005 on; they remained stable in the Center-West region; and decreased in the South and in the Southeast. Mortality due to chronic ischemic heart diseases decreased in Brazil and in the Center-West, South and Southeast regions, and had little variation in the North and in the Northeast. The highest mortality rates due to ill-defined causes occurred in the Northeast until 2005.
Conclusions
Mortality due to heart failure is decreasing in Brazil and in all of its geoeconomic regions. The temporal evolution of mortality caused by ischemic heart diseases was similar to that of heart failure. The decreasing number of deaths due to ill-defined causes may represent the improvement in the quality of information about mortality in Brazil. The evolution of acute ischemic heart diseases ranged according to regions, being possibly confused with the differential evolution of ill-defined causes.
Keywords: Heart Failure / mortality, Myocardial Ischemia / mortality, Epidemiology, Brazil
Introduction
Circulatory System Diseases (CSD) are the main causes of death in Brazil. In 2011, CSDs were responsible for 28.6% of the 1,170,498 deaths that occurred in the country. Ischemic Heart Diseases (IHD) and Heart Failure (HF) were responsible for 39.1% of the deaths caused by CSD1. In the past decades, especially in the South and Southeast regions, it has been possible to observe decreasing mortality due to CSD in Brazil2. The same behavior has been observed in Europe3. In 2008, in the United States, 32.8% of all 2,471,984 deaths were caused by CSD, whose mortality rate was of 244.8 per 100,000 inhabitants; however, from 1998 to 2008, these rates presented a 30.6% decrease4.
Mortality rates due to IHD in Brazil have presented decreasing tendency in the past decades. The analysis of a temporal series from 1981 to 2001 showed declining mortality rates due to IHD in the South and Southeast regions, being stable in the Center-West region and increasing in the Northeast5. Mortality rates due to IHD in Brazil and in the metropolitan region of São Paulo (RMSP), in a more recent period (from 1990 to 2009), revealed the maintenance of the progressive decline observed earlier, in all of the analyzed age groups and in both sexes. The decreasing mortality rates caused by IHD were higher in RMSP than in Brazil as a whole2. This behavior was also observed in CSD, including the IHD, in the States of Rio de Janeiro, São Paulo and Rio Grande do Sul, where mortality rates declined from 1980 to 20066.
National data about the behavior of mortality due to HF are scarce. Most publications about the magnitude of HF as a cause of death in Brazil derive from cohort studies7,8 and from analyses concerning hospital mortality9. According to death records in Rio de Janeiro, São Paulo and Rio Grande do Sul, specific mortality rates due to HF in these States, both for men and women, declined in all ages, except for individuals aged 80 years old or more10.
Goldacre et al11, in England, analyzed the population of Oxford, from 1979 to 2003, and concluded that mortality rates due to HF and IHD had similar declining rates11. Murdoch et al12 studied HF in Scotland, from 1979 to 1992, and besides the observation of declining mortality, they also noticed that 30 to 40% of deaths attributed to IHD may have been related to HF, which demonstrates the correlation of these two conditions.
Mortality statistics is the most useful way to analyze the health status of a population and to plan the necessary health promotion actions. The quality of information about causes of death, therefore, is essential. One of the indicators used to assess the quality of these data is the proportion of deaths attributed to Ill-Defined Causes (IDC). This indicator not only qualifies information, but it also points to the proper analysis of mortality. In Brazil, in 2003, IDC was codified as a basic cause of death in 13.3% of all deaths, and the highest percentages were in the North and the Northeast regions, with 25.9% and 21.1%, respectively13.
The objective of this study was to analyze the evolution of mortality caused by HF, IHD and IDC and their possible relations, in Brazil and according to its geographic regions, from 1996 to 2011.
Methods
The death declarations (DD) records of each Brazilian state, from 1996 to 2011, were obtained from the website of the Unified Health System Information System (DATASUS) (http://tabnet.datasus.gov.br/cgi/sim/dados/cid10_indice.htm#dados, which was accessed in November, 2013. Afterwards, records from DDs of the five regions in Brazil were obtained by the sum of States that compose each region.
Populations in census years were also obtained in the DATASUS website (http://www2.datasus.gov.br/DATASUS/index.php?area=0206&VObj=http://tabnet.datasus.gov.br/cgi/deftohtm.exe?ibge/cnv/pop, which was accessed in November, 2013, by age groups (younger than 1 year old, from 1 to 4 years old, from 5 to 9, from 10 to 14, from 15 to 19, and after that, with 10 year intervals, up to the age of 80). However, the census estimates provided by the Brazilian Institute of Geography and Statistics (IBGE) were not used due to the change of methods adopted after 2007, which caused abrupt and unlikely inflexions in all age groups. These inflexions could lead to disturbances in mortality rate estimates. The populations of inter-census years were obtained by the estimates in each age group, with the arithmetic progression method14.
Computed DD records used the mortality classification of the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (CID-10), in order to codify causes of death. We selected records with codes I20 to I24 for acute IHD, I25 for chronic IHD, I50 for HF and codes in chapter XIII for IDC. The considered cause of death was the one codified as the basic cause of death, according to rules in CID-1015.
The annual mortality rates in Brazil and its geographic regions were calculated, caused by acute IHD, chronic IHD, HF and IDC, per 100 thousand inhabitants, with crude and direct standardized methods, according to the referred age groups. The pattern was the age distribution of the Brazilian population in 2000. These rates were distributed in graphs of annual temporal series for each selected group of causes of death in Brazil and its regions.
The statistical software Stata, version 1216, was used to calculate mortality rates and to elaborate the graphs.
Results
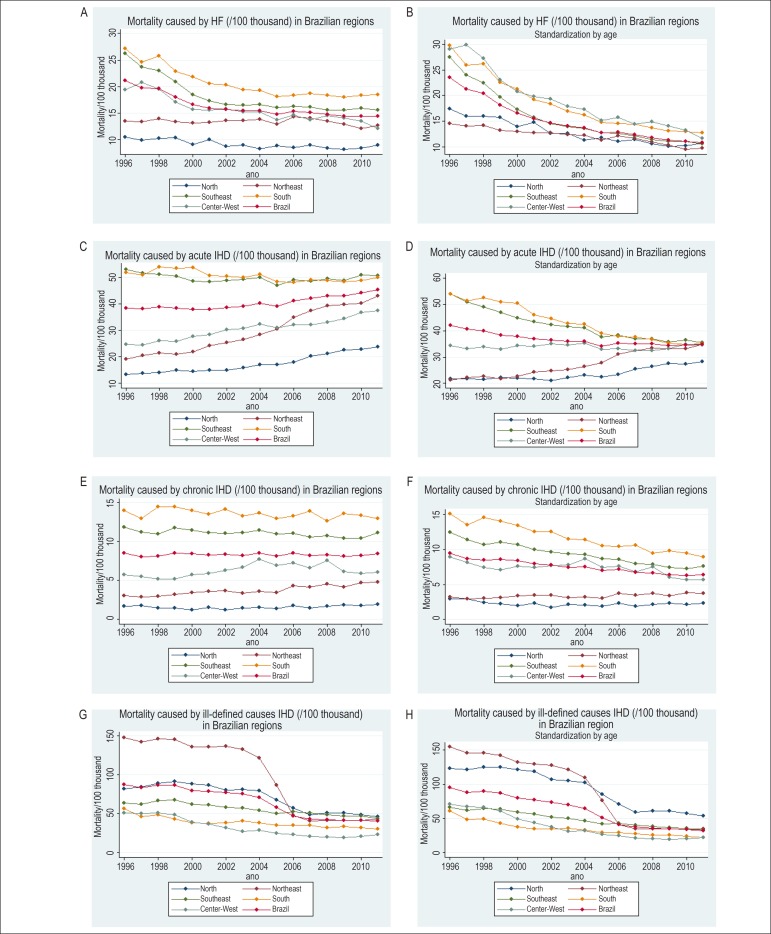
Crude mortality rates caused by HF declined in Brazil and in almost all of its regions, except for the Northeast (Figure 1A). When we observe the standardized rates, this decline is more evident, even in the Northeast, and differences between geographic regions decrease, especially in more recent periods (Figure 1B). In Brazil, the reduced mortality from the first to the last year of the temporal series was of 32.1% in crude rates, and 54.0% in standardized rates (Table 1). The highest crude mortality rates due to HF for the whole period were observed in the South and in the Southeast. However, after considering age distribution, the Center-West presented the highest rates for almost the entire period, and the South was very close (Figure 1B).
Figure 1.
(A) Crude mortality due to heart failure (HF), per 100 thousand, in Brazilian regions, from 1996 to 2011. (B) Standardized mortality due to heart failure, per 100 thousand, in Brazilian regions, from 1996 to 2011 – direct standardization method, according to age groups of DATASUS (pattern: Brazil 2000). (C) Crude mortality due to acute ischemic heart diseases (IHD), per 100 thousand, in Brazilian regions, from 1996 to 2011. (D) Standardized mortality due to acute ischemic heart diseases, per 100 thousand, in Brazilian regions, from 1996 to 2011 – direct standardization method, according to age groups of DATASUS (pattern: Brazil 2000). (E) Crude mortality due to chronic ischemic heart diseases, per 100 thousand, in Brazilian regions, from 1996 to 2011. (F) Standardized mortality due to chronic ischemic heart diseases, per 100 thousand, in Brazilian regions, from 1996 to 2011 – direct standardization method, according to age groups of DATASUS (pattern: Brazil 2000). (G) Crude mortality due to ill-defined causes, per 100 thousand, in Brazilian regions, from 1996 to 2011. (H) Standardized mortality due to ill-defined causes, per 100 thousand, in Brazilian regions, from 1996 to 2011 – direct standardization method, according to age groups of DATASUS (pattern: Brazil 2000).
Table 1.
Crude and standardized mortality* per 100 thousand, due to selected causes - Brazil, 1996-2011
| Year | Heart failure | Acute ischemic heart diseases | Chronic ischemic heart diseases | Ill-defined causes | ||||
|---|---|---|---|---|---|---|---|---|
| Crude | Standardized | Crude | Standardized | Crude | Standardized | Crude | Standardized | |
| 1996 | 21.2 | 23.5 | 38.5 | 42.0 | 8.5 | 9.5 | 87.5 | 85.1 |
| 1997 | 19.7 | 21.2 | 38.0 | 40.5 | 8.0 | 8.6 | 83.1 | 88.3 |
| 1998 | 19.5 | 20.5 | 38.3 | 39.9 | 8.1 | 8.5 | 86.3 | 89.7 |
| 1999 | 17.7 | 18.2 | 37.6 | 38.4 | 8.4 | 8.6 | 85.1 | 86.7 |
| 2000 | 16.6 | 16.6 | 37.8 | 37.8 | 8.4 | 8.4 | 79.9 | 79.9 |
| 2001 | 16.0 | 15.5 | 37.9 | 36.8 | 8.3 | 8.0 | 79.0 | 76.9 |
| 2002 | 15.7 | 14.7 | 38.5 | 36.3 | 8.3 | 7.8 | 77.1 | 73.2 |
| 2003 | 15.4 | 14.1 | 39.0 | 35.9 | 8.2 | 7.5 | 75.8 | 70.2 |
| 2004 | 15.5 | 13.7 | 40.2 | 36.0 | 8.5 | 7.6 | 71.2 | 64.4 |
| 2005 | 14.7 | 12.7 | 39.0 | 34.1 | 8.1 | 7.0 | 57.9 | 51.2 |
| 2006 | 15.3 | 12.9 | 41.2 | 35.2 | 8.5 | 7.2 | 46.9 | 40.7 |
| 2007 | 15.2 | 12.4 | 41.9 | 35.0 | 8.2 | 6.8 | 43.5 | 37.0 |
| 2008 | 14.8 | 11.8 | 43.0 | 35.1 | 8.3 | 6.7 | 42.4 | 35.5 |
| 2009 | 14.5 | 11.3 | 43.0 | 34.4 | 8.1 | 6.4 | 41.9 | 34.4 |
| 2010 | 14.4 | 11.0 | 44.2 | 34.6 | 8.2 | 6.3 | 41.7 | 33.6 |
| 2011 | 14.4 | 10.8 | 45.2 | 34.7 | 8.5 | 6.4 | 40.6 | 32.1 |
Source of data: deaths - SUS Information System (DATASUS); population - Brazilian Institute of Geography and Statistics (count of 1996, census of 2000 and 2010 and linear estimation).
Direct standardization method, according to age groups in DATASUS - Standard: Brazil, year 2000.
In Figure 1C, referring to crude mortality rates caused by acute IHD, it is possible to observe an increasing tendency in the North, Northeast and Center-West regions. From the first to the last year of the series, there was an increase of 77.6% in the North; 124.0% in the Northeast; and 52.4% in the Center-West (Tables 2 to 4).There was a discrete declining tendency in the South and in the Southeast. In the composition of regions, rates in Brazil presented increasing tendency from 2005 on.
Table 2.
Crude and standardized mortality* per 100 thousand, due to selected causes - North region, 1996-2011
| Year | Heart failure | Acute ischemic heart diseases | Chronic ischemic heart diseases | Ill-defined causes | ||||
|---|---|---|---|---|---|---|---|---|
| Crude | Standardized | Crude | Standardized | Crude | Standardized | Crude | Standardized | |
| 1996 | 10.5 | 17.4 | 13.4 | 21.7 | 1.7 | 2.9 | 82.6 | 122.6 |
| 1997 | 9.9 | 16.0 | 13.7 | 21.6 | 1.8 | 2.9 | 84.0 | 121.4 |
| 1998 | 10.1 | 16.0 | 13.8 | 21.4 | 1.5 | 2.4 | 87.5 | 124.7 |
| 1999 | 10.1 | 15.8 | 14.5 | 22.3 | 1.4 | 2.2 | 88.7 | 124.7 |
| 2000 | 9.2 | 13.9 | 14.5 | 22.0 | 1.2 | 1.9 | 88.3 | 121.3 |
| 2001 | 10.1 | 14.8 | 15.0 | 21.8 | 1.5 | 2.3 | 87.1 | 118.3 |
| 2002 | 8.8 | 12.6 | 14.9 | 21.1 | 1.2 | 1.7 | 80.6 | 106.5 |
| 2003 | 9.1 | 12.6 | 16.0 | 22.1 | 1.5 | 2.1 | 81.1 | 105.3 |
| 2004 | 8.3 | 11.3 | 17.1 | 23.1 | 1.5 | 2.1 | 80.0 | 102.4 |
| 2005 | 8.9 | 11.8 | 17.0 | 22.4 | 1.4 | 1.9 | 67.5 | 85.1 |
| 2006 | 8.5 | 11.1 | 18.1 | 23.3 | 1.8 | 2.4 | 57.2 | 70.8 |
| 2007 | 9.0 | 11.5 | 20.2 | 25.5 | 1.5 | 1.9 | 48.4 | 59.0 |
| 2008 | 8.5 | 10.6 | 21.3 | 26.4 | 1.7 | 2.2 | 50.8 | 61.1 |
| 2009 | 8.2 | 10.1 | 22.7 | 27.6 | 1.9 | 2.3 | 50.9 | 60.5 |
| 2010 | 8.4 | 10.2 | 22.8 | 27.4 | 1.8 | 2.2 | 48.7 | 57.1 |
| 2011 | 9.0 | 10.8 | 23.8 | 28.2 | 1.9 | 2.3 | 46.2 | 53.7 |
Source of data: deaths - SUS Information System (DATASUS); population - Brazilian Institute of Geography and Statistics (count of 1996, census of 2000 and 2010 and linear estimation).
Direct standardization method, according to age groups in DATASUS - Standard: Brazil, year 2000.
Table 4.
Crude and standardized mortality* per 100 thousand, due to selected causes - Center-West region 1996-2011
| Year | Heart failure | Acute ischemic heart diseases | Chronic ischemic heart diseases | Ill-defined causes | ||||
|---|---|---|---|---|---|---|---|---|
| Crude | Standardized | Crude | Standardized | Crude | Standardized | Crude | Standardized | |
| 1996 | 19.4 | 29.0 | 24.6 | 34.3 | 5.8 | 8.9 | 50.9 | 70.5 |
| 1997 | 20.8 | 29.8 | 24.5 | 33.2 | 5.5 | 8.1 | 50.3 | 67.0 |
| 1998 | 19.4 | 27.2 | 25.9 | 33.8 | 5.2 | 7.4 | 51.1 | 66.3 |
| 1999 | 16.8 | 23.1 | 25.6 | 32.8 | 5.2 | 7.1 | 48.4 | 60.0 |
| 2000 | 15.7 | 20.7 | 27.6 | 34.3 | 5.7 | 7.6 | 39.6 | 49.2 |
| 2001 | 15.6 | 19.8 | 28.4 | 34.1 | 5.9 | 7.4 | 36.8 | 44.1 |
| 2002 | 15.8 | 19.3 | 30.2 | 35.1 | 6.3 | 7.7 | 31.7 | 37.1 |
| 2003 | 15.3 | 17.9 | 30.8 | 34.7 | 6.7 | 7.8 | 27.2 | 30.7 |
| 2004 | 15.2 | 17.3 | 32.4 | 35.3 | 7.8 | 8.7 | 28.8 | 31.7 |
| 2005 | 13.8 | 15.2 | 30.9 | 32.9 | 6.9 | 7.5 | 24.9 | 26.7 |
| 2006 | 14.7 | 15.8 | 32.2 | 33.2 | 7.3 | 7.6 | 23.5 | 24.6 |
| 2007 | 13.8 | 14.5 | 32.1 | 32.4 | 6.6 | 6.8 | 20.7 | 21.1 |
| 2008 | 14.6 | 14.9 | 32.9 | 32.5 | 7.6 | 7.6 | 20.2 | 20.3 |
| 2009 | 14.1 | 14.1 | 34.3 | 33.1 | 6.1 | 6.0 | 19.2 | 18.9 |
| 2010 | 13.6 | 13.3 | 36.7 | 34.7 | 5.9 | 5.7 | 20.7 | 19.9 |
| 2011 | 12.2 | 11.7 | 37.5 | 34.7 | 6.1 | 5.7 | 23.0 | 21.9 |
Source of data: deaths - SUS Information System (DATASUS); population - Brazilian Institute of Geography and Statistics (count of 1996, census of 2000 and 2010 and linear estimation).
Direct standardization method, according to age groups in DATASUS - Standard: Brazil, year 2000.
Mortality rates due to acute IHD, when standardized by age, as demonstrated in Figure 1D, increased in the North and Northeast regions, especially from 2005 on. These rates remained stable in the Center-West region. In the South and Southeast regions, rates declined throughout the period. In Brazil, these rates declined throughout the period - and a bit less from 2005 on. From the first to the last year, there was a decrease of 34.2% in the Southeast region (Table 5), 35.2% in the South (Table 6), while, in Brazil, it was of 17.3% (Table 1).
Table 5.
Crude and standardized mortality* per 100 thousand, due to selected causes - Southeast Region, 1996-2011
| Year | Heart failure | Acute ischemic heart diseases | Chronic ischemic heart diseases | Ill-defined causes | ||||
|---|---|---|---|---|---|---|---|---|
| Crude | Standardized | Crude | Standardized | Crude | Standardized | Crude | Standardized | |
| 1996 | 26.3 | 27.5 | 53.1 | 54.0 | 11.8 | 12.5 | 64.3 | 65.9 |
| 1997 | 23.6 | 24.0 | 51.5 | 51.0 | 11.2 | 11.4 | 61.7 | 61.8 |
| 1998 | 22.8 | 22.5 | 50.6 | 48.9 | 10.9 | 10.8 | 66.2 | 64.8 |
| 1999 | 20.5 | 19.7 | 49.5 | 46.8 | 11.6 | 11.1 | 66.6 | 63.9 |
| 2000 | 18.5 | 17.4 | 48.5 | 44.9 | 11.4 | 10.7 | 62.5 | 58.8 |
| 2001 | 17.4 | 15.7 | 48.3 | 43.3 | 11.2 | 10.1 | 61.3 | 56.0 |
| 2002 | 16.6 | 14.5 | 48.6 | 42.3 | 11.1 | 9.6 | 58.1 | 51.7 |
| 2003 | 16.5 | 13.9 | 49.2 | 41.6 | 11.2 | 9.4 | 57.3 | 49.7 |
| 2004 | 16.6 | 13.6 | 49.8 | 41.0 | 11.4 | 9.3 | 54.6 | 46.0 |
| 2005 | 16.0 | 12.7 | 47.0 | 37.6 | 11.0 | 8.7 | 50.5 | 41.7 |
| 2006 | 16.3 | 12.6 | 49.0 | 38.3 | 11.1 | 8.6 | 52.3 | 42.3 |
| 2007 | 16.1 | 12.1 | 48.5 | 37.0 | 10.6 | 8.0 | 51.0 | 40.3 |
| 2008 | 15.6 | 11.4 | 49.5 | 36.9 | 10.7 | 7.9 | 48.7 | 37.9 |
| 2009 | 15.6 | 11.1 | 48.8 | 35.7 | 10.4 | 7.5 | 47.4 | 36.0 |
| 2010 | 16.0 | 11.1 | 50.9 | 36.4 | 10.4 | 7.3 | 47.3 | 35.3 |
| 2011 | 15.6 | 10.7 | 50.7 | 35.5 | 11.1 | 7.6 | 44.3 | 32.5 |
Source of data: deaths - SUS Information System (DATASUS); population - Brazilian Institute of Geography and Statistics (count of 1996, census of 2000 and 2010 and linear estimation).
Direct standardization method, according to age groups in DATASUS - Standard: Brazil, year 2000.
Table 6.
Crude and standardized mortality* per 100 thousand, due to selected causes - South Region, 1996-2011
| Year | Heart failure | Acute ischemic heart diseases | Chronic ischemic heart diseases | Ill-defined causes | ||||
|---|---|---|---|---|---|---|---|---|
| Crude | Standardized | Crude | Standardized | Crude | Standardized | Crude | Standardized | |
| 1996 | 27.2 | 29.7 | 51.9 | 53.9 | 14.0 | 15.1 | 56.8 | 60.5 |
| 1997 | 24.6 | 25.9 | 50.9 | 51.4 | 13.0 | 13.5 | 46.6 | 48.2 |
| 1998 | 25.6 | 26.2 | 53.5 | 52.6 | 14.4 | 14.6 | 48.4 | 49.0 |
| 1999 | 22.7 | 22.6 | 52.9 | 50.8 | 14.3 | 14.1 | 42.8 | 42.3 |
| 2000 | 21.9 | 21.2 | 53.7 | 50.4 | 14.0 | 13.4 | 38.3 | 37.1 |
| 2001 | 20.5 | 19.2 | 50.6 | 46.0 | 13.5 | 12.5 | 37.5 | 35.1 |
| 2002 | 20.4 | 18.4 | 50.5 | 44.5 | 14.1 | 12.6 | 38.3 | 34.7 |
| 2003 | 19.4 | 16.9 | 49.9 | 42.6 | 13.3 | 11.5 | 40.7 | 35.9 |
| 2004 | 19.3 | 16.3 | 51.2 | 42.5 | 13.7 | 11.4 | 38.7 | 33.1 |
| 2005 | 18.1 | 14.8 | 48.3 | 39.0 | 13.0 | 10.5 | 35.2 | 29.4 |
| 2006 | 18.3 | 14.5 | 48.0 | 37.8 | 13.3 | 10.4 | 35.6 | 29.0 |
| 2007 | 18.7 | 14.4 | 48.9 | 37.5 | 13.9 | 10.6 | 35.0 | 27.9 |
| 2008 | 18.4 | 13.7 | 48.8 | 36.6 | 12.7 | 9.4 | 32.3 | 25.2 |
| 2009 | 18.0 | 13.1 | 48.3 | 35.3 | 13.6 | 9.9 | 33.3 | 25.3 |
| 2010 | 18.3 | 13.0 | 48.6 | 34.7 | 13.4 | 9.5 | 31.9 | 23.8 |
| 2011 | 18.4 | 12.8 | 50.0 | 34.9 | 13.0 | 9.0 | 30.4 | 22.3 |
Source of data: deaths - SUS Information System (DATASUS); population - Brazilian Institute of Geography and Statistics (count of 1996, census of 2000 and 2010 and linear estimation).
Direct standardization method, according to age groups in DATASUS - Standard: Brazil, year 2000.
Crude mortality rates due to chronic IHD, which can be seen in Figure 1E, were stable in Brazil and in most regions, except for the Northeast, which had a 3.0 rate per 100 thousand inhabitants in 1996, and 4.8 in 2011, which represented a 60% increase (Table 3).
Table 3.
Crude and standardized mortality* per 100 thousand, due to selected causes - Northeast Region, 1996-2011
| Year | Heart failure | Acute ischemic heart diseases | Chronic ischemic heart diseases | Ill-defined causes | ||||
|---|---|---|---|---|---|---|---|---|
| Crude | Standardized | Crude | Standardized | Crude | Standardized | Crude | Standardized | |
| 1996 | 13.6 | 14.5 | 19.2 | 21.3 | 3.0 | 3.2 | 148.1 | 154.7 |
| 1997 | 13.4 | 14.0 | 20.5 | 22.3 | 2.9 | 3.0 | 142.1 | 145.7 |
| 1998 | 13.8 | 14.2 | 21.3 | 22.7 | 3.0 | 3.1 | 144.8 | 145.7 |
| 1999 | 13.2 | 13.2 | 20.7 | 21.6 | 3.1 | 3.2 | 143.1 | 141.6 |
| 2000 | 13.2 | 13.0 | 22.0 | 22.6 | 3.5 | 3.4 | 135.8 | 132.4 |
| 2001 | 13.2 | 12.7 | 24.2 | 24.2 | 3.6 | 3.4 | 135.8 | 129.6 |
| 2002 | 13.7 | 12.8 | 25.4 | 24.8 | 3.6 | 3.4 | 136.6 | 127.7 |
| 2003 | 13.6 | 12.4 | 26.4 | 25.2 | 3.4 | 3.1 | 132.7 | 121.4 |
| 2004 | 13.8 | 12.3 | 28.3 | 26.4 | 3.6 | 3.2 | 121.7 | 109.3 |
| 2005 | 13.0 | 11.3 | 30.4 | 27.7 | 3.4 | 3.0 | 86.8 | 76.4 |
| 2006 | 14.4 | 12.2 | 34.9 | 31.1 | 4.3 | 3.7 | 47.6 | 41.3 |
| 2007 | 14.1 | 11.7 | 37.3 | 32.5 | 4.2 | 3.5 | 41.1 | 35.0 |
| 2008 | 13.5 | 11.0 | 39.2 | 33.2 | 4.5 | 3.8 | 41.5 | 34.8 |
| 2009 | 13.0 | 10.4 | 39.7 | 33.5 | 4.2 | 3.4 | 41.3 | 34.3 |
| 2010 | 12.2 | 9.5 | 40.2 | 33.1 | 4.7 | 3.8 | 41.8 | 34.0 |
| 2011 | 12.8 | 9.8 | 43.0 | 34.7 | 4.8 | 3.8 | 43.4 | 34.6 |
Source of data: deaths - SUS Information System (DATASUS); population - Brazilian Institute of Geography and Statistics (count of 1996, census of 2000 and 2010 and linear estimation).
Direct standardization method, according to age groups in DATASUS - Standard: Brazil, year 2000.
In Figure F, it is possible to observe that standardized mortality rates due to chronic IHD decreased in Brazil and in the Center-West, South and Southeast regions, with little variation in the North and Northeast regions. In Brazil, in 1996, the rate was of 9.5 per 100 thousand inhabitants, while, in 2011, it was 32.6% lower (Table 1).
Mortality rates due to IDC, presented in Figure 1G, declined in all regions. In the North and Northeast regions, this decline was more present from 2004 on. In these regions, from the first to the last year of the period, declines were of 71 and 44%, respectively.
The highest mortality rates due to IDC, both crude and standardized, occurred in the Northeast until 2004. From that point on, the North and the Southeast regions were leaders in these rates (Figures 1G and 1H).
Discussion
Mortality rates due to HF declined in Brazil throughout the analyzed period. Despite the different rates between geographic regions in the country, all of them presented declining numbers (Figures 1A and 1B). The highest crude rates occurred in the South and the Southeast regions, probably because the population in these States is older in relation to the others. That would also explain the decreasing differences observed between regions and the increasing rates in the Center-West region, when these are standardized by age. In the last years of the analyzed series (2011), the differences between standardized rates, which revealed the effect of differences in age, were the lowest in the period.
The decreasing mortality rates due to HF in this study were in accordance with other results published in the few studies about the subject that were conducted in Brazil10,17,18, in which mortality due to HF was also analyzed in DDs.
The same has been observed in other countries. Najafi et al19 analyzed mortality due to HF in Australia, from 1997 to 2003, and found declining rates. They conclude that this fact is related to changes in diagnosis or in the codification of causes of death, thus reflecting changes in HF epidemiology19. In the United States, mortality due to HF was also declining. From 1993 to 2003, the number of deaths due to HF increased 20.5%, and even so, the mortality rate decreased in 2.0%20.
Laribi et al21 studied mortality rates due to HF in seven countries of Europe, and concluded that these numbers reduced 40% in the period between 1987 and 2008. The mean age of death due to HF increased, both for men and women. The authors still consider that these results may be related to improvements in the treatment in the past 20 years21.
Fonarow et al22 assessed the impact of the main treatments tested in several clinical trials, which are recommended by the guidelines of the two largest American societies of cardiology, would have on mortality by HF. Six recommended therapeutic prescriptions estimated that the potential increase of lives saved a year could range between 9.6 and 31.5%22.
In Holland, even with the increasing prescription of drugs to treat HF, no improvement was observed in the prognosis of the first year after hospital discharge after hospitalizations due to HF, when comparing the periods of 1998-2002 and 2003-2007. However, the prescription of renin-angiotensin-Aldosterone system inhibitors and beta blockers was not higher than 60% in the second period of this series23.
In this study, mortality caused by acute IHD presented different behaviors, depending on the region. As with HF, the highest rates were concentrated in the South and in the Southeast, and the lowest ones, in the North and in the Northeast (Figures 1C and 1D). Rates in the South and in the Southeast presented decreasing tendency, especially when standardized; the ones in the North and Northeast region tended to increase throughout the period, mostly after 2005. In 2011, the mortality strength of acute IHD, despite the differences of age structure, was practically the same in all regions, except for the North. However, since the growth tendency remained in this region, soon enough the mortality strength of acute IHD in the North will reach the same levels of the other regions.
It is possible to speculate that the decreasing differences are not explained by changes in patterns of deaths caused by acute IHD between the regions, but instead, by changes in the way DDs are filled out. And that is because, in the middle of the studied period, around 2005, the number of ill-defined or undetermined causes of death in DDs decreased notably in the North and Northeast regions. Therefore, it is possible that most declarations that previously contained ill-defined causes changed into acute IHD as the cause of death (Figures 1C, 1D, 1G e 1H).
As in acute IHD, the South and the Southeast regions also had the highest mortality rates due to chronic IHD, and the North and the Northeast, the lowest ones (Figures 1E e 1F). However, in this group of IHD, the decrease observed in strength mortality in the South and in the Southeast, after the exclusion of age differences, can make regional differences minimum in the future.
Mortality rates due to acute and chronic IHD in Brazil, as a whole, are a weighed composition of regional rates. Therefore, if the latter are heterogeneous, the global rate of the country does not sum up what happened in any part of the territory throughout the period (Figures 1C e 1D e Table 1).
The regional differences concerning the mortality behavior due to IHD in Brazil reported here have been published before. A temporal series5 from 1981 to 2001 demonstrated the declining mortality rates due to IHD in the South and Southeast regions, being stable in the Center-West region and higher in the Northeast region. The authors, Souza et al5 related the declining tendency of circulatory diseases to the probable improvement in the control of risk factors, such as smoking, dyslipidemias, diabetes and systemic arterial hypertension. The control of these factors, the primary and secondary prevention, would be more adequate in more developed regions, and it could explain the observed regional differences5.
In a series from 1990 to 2009, it was also possible to observe declining mortality rates due to IHD. The mortality due to this condition in RMSP was higher than the numbers in Brazil, however, it also presented a stronger decreasing tendency than in the country, both among men (36.2% vs. 23,5%) and women (44.5% vs. 29.5%)2.
Soares et al6 analyzed mortality due to all causes and caused by CSD, IHD and Cerebrovascular Diseases (CVDs), from 1980 to 2006, in Rio de Janeiro, in Rio Grande do Sul and in São Paulo, and found decreasing mortality rates due to all groups of causes. The decreasing mortality due to all causes was mostly attributed to the relevant decline in mortality by CSD. The authors speculated that these results may be a result of the slower decrease of mortality due to infectious diseases and of the improved life conditions of the population6.
In a more recent publication, these authors reinforce the validity of this hypothesis by studying the evolution of socioeconomic indicators and cardiovascular mortality in the same three Brazilian states. There was a strong correlation between the decreasing child mortality rates, the increasing Gross Domestic Product (GPD) per capita and the increasing schooling with the reduced mortality due to CSD, IHD and CVDs in adults of the studied series of 1980 to 200824.
One of the indicators of quality concerning the death records is the proportion of causes of death codified as ill-defined ones13. In Brazil, the proportion of deaths due to IDC was around 20%, from 1970 to 1986. After 1987, this proportion declined progressively, reaching 15%, in 2996, and being still unsatisfactory in 2003, with 13.3%13.
A study about death reclassification due to IDC in DDs, in the late 1990s, in the State of Rio de Janeiro, found that the CSD were the most likely causes of death. Proportional mortality due to CSD was higher in reclassified ill-defined causes, according to information obtained by the Authorization Forms for Hospital Admission25. Therefore, it is possible that the increasing levels of death rates due to acute IHD, which is an important component of CSD, has occurred together with the decline in death rates due to IDC, observed in the North and in the Northeast.
In this study, we observed a decreasing tendency in mortality caused by IDC in all of the Brazilian regions, however, with major variation (Figures 1G and 1H). The Northeast and North regions, in this order, presented the highest rates throughout the years, however, the decline of these rates was more present after 2004, especially in the Northeast. However, the Southeast region, which presents more economic progress and has the largest population contingent, still has high levels of mortality caused by IDC in the last years of the series.
We can speculate that the temporal evolution of mortality rates due to chronic IHD and HF are similar in the South, Southeast, and Center-West regions. At the same time, in the North and the Northeast, deaths caused by IDC and acute and chronic IHD and HF competed, which made it difficult to assess the evolution of each of the groups of defined causes and their relations. Therefore, it was possible to observe in the region of Oxford, in England, from 1979 to 200311, that the decreasing mortality rates due to acute and chronic IHD was not followed by the increasing mortality due to HF - this could only be observed in the South of Brazil in the studied period. In the other regions, flows and high levels of deaths due to IDC disturb the analysis of the combined evolution of IHD and HF.
This main limiting factor for this study was the quality of information about cause of death, which depended on the diagnosis of the causes and the proper filling out of the DD; the use of the basic cause of death to analyze mortality can also be a limiting factor. For some conditions, such as HF, mortality can be underestimated, when we do not use the multiple cause analysis, which contemplates all causes mentioned in the DD10,26,27.
Conclusion
Mortality caused by heart failure has been declining in Brazil consistently for all major geoeconomic regions. Mortality due to acute ischemic heart disease declined in the South and the Southeast regions, but remained stable in the Center-West and increased in the North and Northeast regions. The behavior of mortality due to chronic ischemic heart diseases was similar with that of heart failure. The decline observed in deaths due to ill-defined causes may represent an improvement in the quality of information about mortality in Brazil. For the proper planning of public health policies that aim at decreasing the mortality due to circulatory system diseases, the observed regional differences must be considered.
Footnotes
Author contributions
Conception and design of the research, Acquisition of data, Analysis and interpretation of the data, Statistical analysis, Writing of the manuscript and Critical revision of the manuscript for intellectual content: Gaui EN, Oliveira GMM, Klein CH.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Sources of Funding
There were no external funding sources for this study.
Study Association
This article is part of the thesis of Doctoral submitted by Eduardo Nagib Gaui, from Universidade Federal do Rio de Janeiro.
References
- 1.Ministério da Saúde. Secretaria Executiva. Datasus [Acesso em 2013 nov 20];Informações de Saúde. Estatísticas vitais. Disponível em: http://www.datasus.gov.br.
- 2.Mansur AP, Favarato D. Mortalidade por doenças cardiovasculares no Brasil e na Região Metropolitana de São Paulo: atualização 2011. Arq Bras Cardiol. 2012;99(2):755–761. doi: 10.1590/s0066-782x2012005000061. [DOI] [PubMed] [Google Scholar]
- 3.Helis E, Augustincic L, Steiner S, Chen L, Turton P, Fodor JG. Time trends in cardiovascular and all-cause mortality in the "old" and "new" European Union countries. Eur J Cardiovasc Prev Rehabil. 2011;18(3):347–359. doi: 10.1177/1741826710389361. [DOI] [PubMed] [Google Scholar]
- 4.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Heart disease and stroke statistics- 2012 update: a report from American Heart Association. Circulation. 2012;125(1):e2–e220. doi: 10.1161/CIR.0b013e31823ac046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Souza MF, Alencar AP, Malta DC, Moura L, Mansur AP. Análise de séries temporais da mortalidade por doenças isquêmicas do coração e cerebrovasculares, nas cinco regiões do Brasil, no período de 1981 a 2001. Arq Bras Cardiol. 2006;87(6):735–740. [Google Scholar]
- 6.Soares GP, Brum JD, Oliveira GM, Klein CH, Silva NA. Mortalidade por todas as causas e por doenças cardiovasculares em três estados do Brasil, 1980 a 2006. Rev Panam Salud Publica. 2010;28(4):258–266. doi: 10.1590/s1020-49892010001000004. [DOI] [PubMed] [Google Scholar]
- 7.Rassi S, Barreto CP, Porto CC, Pereira CR, Calaça BW, Rassi DC. Sobrevida e fatores prognósticos na insuficiência cardíaca sistólica com início recente dos sintomas. Arq Bras Cardiol. 2005;84(4):309–313. doi: 10.1590/s0066-782x2005000400007. [DOI] [PubMed] [Google Scholar]
- 8.Latado AL, Passos LC, Braga JC, Santos A, Guedes R, Moura SS, et al. Preditores de letalidade hospitalar em pacientes com insuficiência cardíaca avançada. Arq Bras Cardiol. 2006;87(2):185–192. doi: 10.1590/s0066-782x2006001500018. [DOI] [PubMed] [Google Scholar]
- 9.Albanesi FM., Filho Indicadores de doença cardiovascular no estado do Rio de Janeiro com relevo para a insuficiência cardíaca. Rev SOCERJ. 2004;17(4):264–269. [Google Scholar]
- 10.Gaui EN, Klein CH, Oliveira GM. Mortalidade por insuficiência cardíaca: análise ampliada e tendência temporal em três estados do Brasil. Arq Bras Cardiol. 2010;94(1):55–61. doi: 10.1590/s0066-782x2010000100010. [DOI] [PubMed] [Google Scholar]
- 11.Goldacre MJ, Mant D, Duncan M, Griffith M. Mortality from heart failure in an English population, 1979-2003: study of death certification. J Epidemiol Community Health. 2005;59(9):782–784. doi: 10.1136/jech.2004.028951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murdoch DR, Love MP, Robb TA, McDonagh TA, Davie AP, Ford I, et al. Importance of heart failure as a cause of death: changing contribution to overall mortality and coronary heart disease mortality in Scotland 1979-1992. Eur Heart J. 1998;19(12):1829–1835. doi: 10.1053/euhj.1998.1269. [DOI] [PubMed] [Google Scholar]
- 13.Santo AH. Causas mal definidas de morte e óbitos sem assistência. Rev Assoc Med Bras. 2008;54(1):23–28. doi: 10.1590/s0104-42302008000100016. [DOI] [PubMed] [Google Scholar]
- 14.Laurenti R, Mello Jorge MH, Lebrão ML, Gotlieb SLD. Estatísticas de Saúde. São Paulo: EPU; 2005. [Google Scholar]
- 15.Organização Mundial de Saúde . Classificação estatística internacional de doenças e problemas relacionados à saúde. São Paulo: EDUSP; 1997. [Google Scholar]
- 16.Stata 8.2 statistics/data analysis. Special Edition. Statacorp 4905 Lakeway Drive College Station; Texas, USA: 2005. [Google Scholar]
- 17.Latado AL, Passos LC, Guedes R, Santos AB, Andrade M, Moura S. Tendência da mortalidade por insuficiência cardíaca em Salvador, Bahia, Brasil. Arq Bras Cardiol. 2005;85:327–332. doi: 10.1590/s0066-782x2005001800005. [DOI] [PubMed] [Google Scholar]
- 18.Gaui EN, Klein CH, Oliveira GM. Mortalidade por insuficiência cardíaca como causa básica ou contribuinte de óbito em três estados brasileiros, de 1999 a 2004. Rev SOCERJ. 2008;21(3):129–137. [Google Scholar]
- 19.Najafi F, Dobson AJ, Jamrozik K. Is mortality from heart failure increasing in Austrália? An analysis of official data on mortality for 1997-2003. Bull World Health Organ. 2006;84(9):722–728. doi: 10.2471/blt.06.031286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thom T, Haase N, Rosamond W, Howard VJ, Rumsfeld J, Manolio T, et al. Heart disease and stroke statistics - 2006 update: a report from American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2006;113(6):e85–159. doi: 10.1161/CIRCULATIONAHA.105.171600. [DOI] [PubMed] [Google Scholar]
- 21.Laribi S, Aouba A, Nikolaou M, Lassus J, Cohen-Solal A, Plaisance P, et al. Trends in death attributed to heart failure over the past two decades in Europe. Eur J Heart Fail. 2012;14(3):234–239. doi: 10.1093/eurjhf/hfr182. [DOI] [PubMed] [Google Scholar]
- 22.Fonarow GC, Yancy CW, Hernandez AF, Peterson ED, Spertus JA, Heindenreich PA. Potential impact of optimal implementation of evidence-based heart failure therapies on mortality. Am Heart J. 2011;161(6):1024–1030. doi: 10.1016/j.ahj.2011.01.027. [DOI] [PubMed] [Google Scholar]
- 23.de Peuter OR, Lip GY, Souverein PC, Klungel OH, de Boer A, Büller HR, et al. Time-trends in treatment and cardiovascular events in patients with heart failure: a pharmacosurveillance study. Eur J Heart Fail. 2011;13(5):489–495. doi: 10.1093/eurjhf/hfq228. [DOI] [PubMed] [Google Scholar]
- 24.Soares GP, Brum JD, Oliveira GM, Klein CH, Souza e Silva NA. Evolução de indicadores socioeconômicos e da mortalidade cardiovascular em três estados do Brasil. Arq Bras Cardiol. 2013;100(2):147–156. doi: 10.5935/abc.20130028. [DOI] [PubMed] [Google Scholar]
- 25.Teixeira CS, Klein CH, Block KV. Reclassificação dos grupos de causas prováveis de óbitos de causa mal definida, com base nas Autorizações de Internação Hospitalar no Sistema Único de Saúde, Estado do Rio de Janeiro, Brasil. Cad Saúde Pública. 2006;22(6):1315–1324. doi: 10.1590/s0102-311x2006000600020. [DOI] [PubMed] [Google Scholar]
- 26.Santo AH. Potencial epidemiológico da utilização das causas múltiplas de morte por meio de suas menções nas declarações de óbito, Brasil, 2003. Rev Panam Salud Publica. 2007;22(3):178–186. doi: 10.1590/s1020-49892007000800004. [DOI] [PubMed] [Google Scholar]
- 27.Engelfriet PM, Hoogenveen RT, Boshuizen HC, van Baal PH. To die with or from heart failure: a difference that counts. Eur J Heart Fail. 2011;13(4):377–383. doi: 10.1093/eurjhf/hfq223. [DOI] [PubMed] [Google Scholar]