Abstract
Background
The radial access provides a lower risk of bleeding and vascular complications related to the puncture site in comparison to the femoral access. Recent studies have suggested a reduction in mortality associated with the radial access in patients with acute myocardial infarction undergoing percutaneous coronary intervention.
Objective
To compare the occurrence of adverse cardiovascular ischemic and hemorrhagic events in patients undergoing primary angioplasty according to the type of arterial access route.
Methods
From August 2010 to December 2011, 588 patients undergoing primary percutaneous coronary intervention during acute ST-segment elevation myocardial infarction were assessed; they were recruited from 47 centers participating in the ACCEPT registry. Patients were grouped and compared according to the arterial access used for the procedure.
Results
The mean age was 61.8 years; 75% were males and 24% had diabetes mellitus. There was no difference between groups as regards the procedure success rate, as well as regards the occurrence of death, reinfarction, or stroke at six months of follow-up. Severe bleeding was reported in 1.1% of the sample analyzed, with no statistical difference related to the access used.
Conclusions
The femoral and radial accesses are equally safe and effective for the performance of primary percutaneous coronary intervention. The low rate of cardiovascular events and of hemorrhagic complications reflects the quality of the participating centers and the operators expertise with the use of both techniques.
Keywords: Myocardial infarction, Percutaneous coronary interventions, Femoral artery / surgery, Radial artery / surgery
Introduction
The growing interest for the radial access as a strategy for the reduction of hemorrhagic complications in percutaneous coronary intervention (PCI) confirms the impact of severe bleeding as a determinant of a poorer prognosis in invasively stratified patients with acute coronary syndrome (ACS)1-3. Bleeding events related to the arterial access are the most frequent among patients undergoing coronary procedures and are independently associated with increased one-year mortality4. Recent reviews of guidelines dedicated to this subject suggest the option of the radial access as preferable to the femoral access, as long as employed by operators both experienced and familiar with the technique5,6.
Patients with ST-segment elevation acute myocardial infarction (AMI) undergoing primary PCI - commonly treated with aggressive adjunctive antithrombotic drug therapy, comprise the clinical group for which the benefits from the radial technique are more expressive7. However, many of the centers involved in randomized trials comparing the access routes in this scenario are known to adopt the radial technique as the first option in their procedures, thus representing a potential selection bias of these analyses.
The Acute Coronary Syndrome Clinical Practice Registry (ACCEPT) is a nationwide Brazilian case series that aims to provide a panorama of the demographic profile and of the occurrence of severe clinical endpoints in patients with ACS. The objective of the present analysis is to compare the six-month follow-up occurrence of severe adverse cardiovascular ischemic and hemorrhagic events among patients included in this registry and undergoing primary PCI, according to the arterial access used in the procedure.
Methods
The ACCEPT rationale, methodology, organization and registry committees have already been described elsewhere8,9. In sum, it is a prospective, voluntary, multicenter study conceived and managed by the Brazilian Society of Cardiology (Sociedade Brasileira de Cardiologia - SBC), logistically structured in the first semester of 2010, with patient data collection starting from August 2010. For this purpose, 47 investigation centers were gathered in order to reach the largest possible territorial area representing all the Brazilian federative regions, including public hospital care centers (Single Health System), health maintenance organizations, or private health care centers. These centers were selected using two criteria: by inviting qualified institutions and by actively searching for new centers, using the SBC's website to offer the opportunity to participate. The inclusion criteria were the presence of a research ethics committee (REC), ability to follow up the patients for up to one year, and presence of patients fitting the clinical scope of this registry.
All centers were given training on the protocol and the electronic system, whether in the classroom or by telephone, supported by the coordination team. Quality control of the study data was measured by different strategies, such as the use of an electronic form dedicated to the collection of clinical variables, central control of the variables collected, attendance monitoring in the five centers with the largest number of patients recruited, and random raffle of 20% of the centers for attendance monitoring. The protocol was approved by the REC of Hospital do Coração de São Paulo and, subsequently, each participating center had its local approval. All patients gave written informed consent to participate, and the clinical study was carried out according to the principles of the current review of the Declaration of Helsinki, the Guidelines of Good Clinical Practices, and Resolution 196/96.
In the present analysis, we assessed patients with ST-segment elevation AMI undergoing primary PCI, grouped according to the arterial access used, whether femoral or radial. The clinical endpoints analyzed were cardiovascular mortality, reinfarction, stroke, and severe bleeding. The occurrence of the clinical endpoints mentioned was checked after hospital admission and at 180 days. In compliance with the Bleeding Academic Research Consortium (BARC) classification10 , severe bleeding was defined as that of type 3, subdivided into (3a) - bleeding plus hemoglobin drop ≥ 3 and < 5 g/dL, or red blood cell transfusion; (3b) - bleeding with hemoglobin drop ≥ 5 g/dL, or cardiac tamponade, or bleeding requiring surgical intervention for control; (3c) - intracranial hemorrhage or subcategories confirmed by autopsy, imaging studies or lumbar puncture, or intraocular bleed compromising vision. Also, type 5 subdivided into (5a) - probable fatal bleeding, and (5b), definite fatal bleeding.
Continuous variables with skewed and normal distribution were described as median and mean ± standard deviation, respectively. Categorical variables were described as absolute and relative frequencies. Proportions were compared between two independent groups using Fisher's exact test. Means were compared using Student's t test for independent samples. Medians were compared using the Mann-Whitney test. The SAS 9.3 program (Statistical Analysis System, Cary, NC) was used for the statistical analysis of data. P values are two-tailed and p < 0.05 were considered statistically significant.
This registry is proprietary of SBC, using its own financial resources dedicated to this purpose. The Instituto de Ensino e Pesquisa do Hospital do Coração de São Paulo (IEP/Hcor) was hired to operationalize the performance of this registry, under coordination of SBC.
Results
We analyzed 2608 patients enrolled until December 2011, corresponding to phase I of the project; their dedicated electronic file was fully filled up (at admission, 30 and 180 days), and 640 had undergone primary PCI. A total of 8.1% of patients (52 cases) were lost to follow-up at six months, thus the final analysis was restricted to 588 patients, 410 of whom were allocated to the femoral group and 178 to the radial group. Their baseline clinical characteristics and demographics are shown inTable 1.
Table 1.
Baseline clinical characteristics and demographics
| Variables | Overall (n=588) | Femoral (n=410) | Radial (n=178) | p |
|---|---|---|---|---|
| Age, mean ± standard deviation | 61.8 ± 12.3 | 63.1 ± 12.3 | 58.9 ± 11.7 | < 0.001 |
| Male gender, n (%) | 442 (75.2) | 300 (73.2) | 142 (79.8) | 0.097 |
| Female gender, n (%) | 146 (24.8) | 110 (26.8) | 36 (20.2) | 0.097 |
| Systemic hypertension, n (%) | 395 (67.2) | 279 (68.0) | 116 (65.2) | 0.505 |
| Diabetes mellitus, n (%) | 142 (24.1) | 97 (23.7) | 45 (25.3) | 0.676 |
| Dyslipidemia, n (%) | 278 (47.3) | 203 (49.5) | 75 (42.1) | 0.106 |
| Obesity, n (%) | 187 (31.8) | 132 (32.2) | 55 (30.9) | 0.773 |
| Smoking habit, n (%) | 185 (31.5) | 115 (28.0) | 70 (39.3) | 0.009 |
| Previous acute myocardial infarction (%) | 121 (20.6) | 91 (22.2) | 30 (16.9) | 0.150 |
| Previous stroke, n (%) | 47 (7.9) | 27 (6.6) | 20 (11.2) | 0.068 |
| Chronic kidney failure, n (%) | 17 (2.9) | 15 (3.7) | 2 (1.1) | 0.111 |
The mean age was 61.8 years, 75% were males, 24% had diabetes mellitus, and 20% had history of previous AMI. There was a predominance of patients with one-vessel coronary atherosclerotic disease, and the angiographic success rate of primary PCI was achieved in 96.6% of cases by means of broad utilization of coronary endoprostheses, most of which were non-drug eluting stents (Table 2). Double antiplatelet therapy with acetylsalicylic acid and clopidogrel, and anticoagulation therapy with enoxaparin were the most frequently used antithrombotic . Glycoprotein IIb-IIIa inhibitors were prescribed for approximately 20% of procedures, predominantly in the group in which the radial access was used.
Table 2.
Characteristics of the procedures and in-hospital antithrombotic therapy
| Variables | Overall (n = 588) | Femoral (n = 410) | Radial (n = 178) | p |
|---|---|---|---|---|
| Procedural success rate, n (%) | 568 (96.6) | 397 (96.8) | 171 (96.1) | 0.627 |
| Stent implantation, n (%) | 562 (98.9) | 395 (99.5) | 167 (97.7) | 0.192 |
| Drug-eluting stent, n (%) | 126 (21.4) | 116 (28.3) | 10 (5.6) | < 0.001 |
| Non-drug-eluting stent, n (%) | 436 (74.1) | 279 (68.0) | 157 (88.2) | < 0.001 |
| One-vessel, n (%) | 275 (48.5) | 197 (49.1) | 78 (47.0) | 0.369 |
| Two-vessel, n (%) | 172 (30.3) | 131 (32.7) | 41 (24.7) | 0.030 |
| Multivessel, n (%) | 111 (19.6) | 69 (17.2) | 42 (25.3) | 0.066 |
| Acetylsalicylic acid, n (%) | 578 (98.3) | 405 (98.8) | 173 (97.2) | 0.179 |
| Clopidogrel, n (%) | 561 (95.4) | 395 (96.3) | 166 (93.3) | 0.131 |
| Prasugrel, n (%) | 4 (0.7) | 4 (100.0) | 0 (0.0) | 0.320 |
| Ticagrelor, n (%) | 7 (1.2) | 1 (0.2) | 6 (3.4) | 0.004 |
| Glycoprotein IIb-IIIa inhibitors, n (%) | 105 (17.9) | 61 (14.9) | 44 (24.7) | 0.005 |
| Unfractioned heparin, n (%) | 101 (17.2) | 83 (20.2) | 18 (10.1) | 0.003 |
| Enoxaparin, n (%) | 377 (64.1) | 261 (63.7) | 116 (65.2) | 0.779 |
| Fondaparinux, n (%) | 31 (5.3) | 6 (1.5) | 25 (14.0) | < 0.001 |
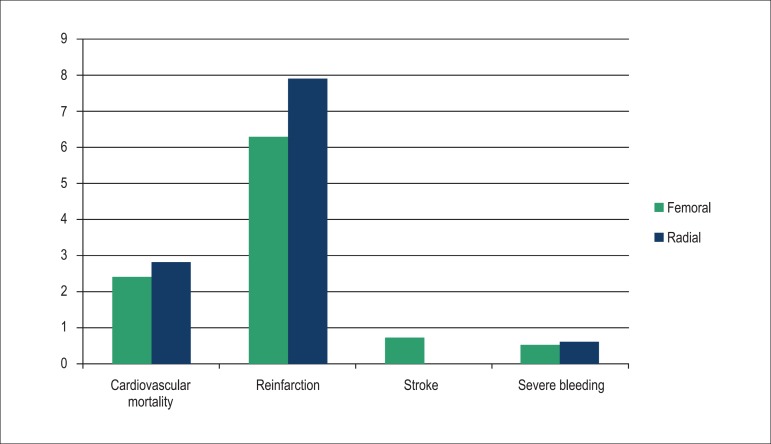
The rate of adverse cardiac ischemic events at six months of follow-up was low, and the occurrence of a new AMI was the most frequent complication (Graph 1). Severe bleeding was reported in 1.1% of the sample analyzed, with no statistical difference regarding the access route used.
Graph 1.
Clinical endpoints (%) at six months of follow-up.
Discussion
In 2009, a meta-analysis of 23 randomized studies showed that the radial access provides a higher than 70% reduction in the prevalence of severe bleeding when compared to the femoral access, especially among patients undergoing primary or rescue PCI, with a potential impact on the reduction of ischemic events11. Two years later, a similar investigation hypothesis was formulated by the Radial versus Femoral Access for Coronary Intervention (RIVAL) study, which compared 7021 patients diagnosed with ACS, of whom 1958 had ST-segment elevation, and found a reduction by 61% in mortality with the use of the radial technique (1.3% versus 3.2%, p = 0.006) in this subgroup of patients12.
With methodology and statistical power to compare the access routes in the setting of ST-segment elevation ACS, the multicenter study Radial Versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome (RIFLE-STEACS) analyzed 1001 patients, and showed a significant clinical benefit with the use of the radial access translated into lower rates of cardiovascular mortality, stroke, AMI, target-vessel revascularization, and severe bleeding (13.6% versus 21.0%, p = 0.003)13. The individual analysis of the components of the primary endpoint showed a significant reduction in cardiovascular mortality and severe bleeding among patients randomized for the radial access, with a considerable reduction of vascular complications in the puncture site as regards the severe bleeding event. A recent meta-analysis involving 12 studies on primary PCI, including the results of the previously mentioned RIVAL and RIFLE-STEACS, and counting with 5055 patients, showed a reduction by 45% in the death risk and by 49% in the risk of severe bleeding with the use of the radial in relation to the femoral technique7.
The role of the learning curve in the proficiency and acquisition of better results with the radial access is recognized14. In the RIVAL study, centers characterized by having a high volume of procedures using the radial access (> 146 transradial PCI/operator/year) benefited from the cross-rate between the techniques, severe vascular complications, and the primary endpoint comprising death, AMI or stroke12. Thus, an important limitation of these publications lies on the concentration of centers having operators experienced in the use of the radial technique, a situation that is evidenced by the low cross-rate between the access routes and the procedure duration in the case series. On the other hand, the improvement of the femoral technique, by means of the reduction of endovascular device diameter, early removal of the arterial introducer, preference for the femoral puncture technique, sometimes guided by fluoroscopy or ultrasound, and the option for antithrombotic agents with a better safety profile, also translates into a lower incidence of complications. In fact, a Brazilian case series of 205 consecutive patients with AMI undergoing the invasive drug strategy with tenecteplase showed an incidence of only 1.5% of severe vascular hemorrhagic complications after femoral puncture15.
In the ACCEPT registry, the rate of ischemic and hemorrhagic events was low using both access routes, but in agreement with that of other studies published with a similar population12. We can assume that, once national reference centers with a broad experience in the use of interventional techniques are included, the differences in the success and complication rates will be attenuated in the final assessment. However, the registry has limitations. The voluntary inclusion of patients by center, in a non-consecutive fashion, and the non-systematic adjudication of events are restrictions to the unequivocal acceptance of its results.
Conclusions
The femoral and radial access routes are equally safe and effective for the performance of primary percutaneous coronary interventions. The low rate of cardiovascular events and of hemorrhagic complications reflects the quality of the centers participating in the ACCEPT registry and the operators expertise with the use of both techniques.
Footnotes
Author contributions
Conception and design of the research and Analysis and interpretation of the data and Critical revision of the manuscript for intellectual content: Andrade PB, Berwanger O, Piva e Mattos LA; Acquisition of data: Andrade PB, Andrade MVA, Barbosa RA, Labrunie A, Hernandes ME, Marino RL, Precoma DB, Sá FCF, Berwanger O, Piva e Mattos LA; Statistical analysis and Obtaining financing: Berwanger O; Writing of the manuscript: Andrade PB.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Sources of Funding
There were no external funding sources for this study.
Study Association
This study is not associated with any thesis or dissertation work.
References
- 1.Pocock SJ, Mehran R, Clayton TC, Nikolsky E, Parise H, Fahy M, et al. Prognostic modeling of individual patient risk and mortality impact of ischemic and hemorrhagic complications: assessment from the Acute Catheterization and Urgent Intervention Triage Strategy trial. Circulation. 2010;121(1):43–51. doi: 10.1161/CIRCULATIONAHA.109.878017. [DOI] [PubMed] [Google Scholar]
- 2.Doyle BJ, Rihal CS, Gastineau DA, Holmes, Jr DR. Bleeding, blood transfusion, and increased mortality after percutaneous coronary intervention: implications for contemporary practice. J Am Coll Cardiol Interv. 2009;22(22):2019–2027. doi: 10.1016/j.jacc.2008.12.073. [DOI] [PubMed] [Google Scholar]
- 3.de Andrade PB, Tebet MA, Maia da Silva FS, Athanazio de Andrade MV, Labrunie A, Piva e Mattos LA. Major bleeding in acute coronary syndromes. J Invasive Cardiol. 2011;23(11):485–490. [PubMed] [Google Scholar]
- 4.Ndrepepa G, Neumann FJ, Richardt G, Schulz S, Tölg R, Stoyanov KM, et al. Prognostic value of access and non-access sites bleeding after percutaneous coronary intervention. Circ Cardiovasc Interv. 2013;6(4):354–361. doi: 10.1161/CIRCINTERVENTIONS.113.000433. [DOI] [PubMed] [Google Scholar]
- 5.Steg PG, James SK, Atar D, Badano LP, Blomstrom-Lundqvist C, Borger MA, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. The Task Force on the management of St-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC) Eur Heart J. 2012;33(20):2569–2619. doi: 10.1093/eurheartj/ehs215. [DOI] [PubMed] [Google Scholar]
- 6.Levine GN, Bates ER, Blankenship JC, Bailey SR, Bittl JA, Cercek B, et al. 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. J Am Coll Cardiol. 2011;58(24):e44–122. doi: 10.1016/j.jacc.2011.08.007. Erratum in: Circulation. 2012;125(8):e412. [DOI] [PubMed] [Google Scholar]
- 7.Karrowni W, Vyas A, Giacomino B, Schweizer M, Blevins A, Girotra S, et al. Radial versus femoral access for primary percutaneous interventions in ST-segment elevation myocardial infarction patients. JACC Cardiovasc Interv. 2013;6(8):814–823. doi: 10.1016/j.jcin.2013.04.010. [DOI] [PubMed] [Google Scholar]
- 8.Mattos LA. Registro Brasileiro da Prática Clínica nas Síndromes Coronarianas Agudas da Sociedade Brasileira de Cardiologia. Arq Bras Cardiol. 2011;97(2):94–99. doi: 10.1590/s0066-782x2011005000064. [DOI] [PubMed] [Google Scholar]
- 9.Piva e Mattos LA, Berwanger O, Santos ES, Reis HJL, Romano ER, Petriz JLF, et al. Desfechos clínicos aos 30 dias do Registro Brasileiro das Síndromes Coronárias Agudas (ACCEPT) Arq Bras Cardiol. 2013;100(1):6–13. [Google Scholar]
- 10.Mehran R, Rao SV, Bhatt DL, Gibson CM, Caixeta A, Eikelboom J, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011;123(23):2736–2747. doi: 10.1161/CIRCULATIONAHA.110.009449. [DOI] [PubMed] [Google Scholar]
- 11.Jolly SS, Amlani S, Hamon M, Yusuf S, Mehta SR. Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am Heart J. 2009;157(1):132–140. doi: 10.1016/j.ahj.2008.08.023. [DOI] [PubMed] [Google Scholar]
- 12.Jolly SS, Yusuf S, Cairns J, Niemelä K, Xavier D, Widimsky P, et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): a randomised, parallel group, multicentre trial. Lancet. 2011;377(9775):1409–1420. doi: 10.1016/S0140-6736(11)60404-2. [DOI] [PubMed] [Google Scholar]
- 13.Romagnoli E, Biondi-Zoccai G, Sciahbasi A, Politi L, Rigattieri S, Pendenza G, et al. Radial versus femoral randomized investigation in ST-elevation acute coronary syndrome: the RIFLE-STEACS (Radial Versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome) study. J Am Coll Cardiol. 2012;60(24):2481–2489. doi: 10.1016/j.jacc.2012.06.017. [DOI] [PubMed] [Google Scholar]
- 14.Rao SV, Tremmel JA, Gilchrist IC, Shah PB, Gulati R, Shroff AR, et al. Best practices for transradial angiography and intervention: a consensus statement from the society for cardiovascular angiography and intervention's transradial working group. Catheter Cardiovasc Interv. 2013;83(2):228–236. doi: 10.1002/ccd.25209. [DOI] [PubMed] [Google Scholar]
- 15.Caluza AC, Barbosa AH, Gonçalves I, Oliveira CA, Matos LN, Zeefried C, et al. Rede de infarto com supradesnivelamento de ST: sistematização em 205 casos diminui eventos clínicos na rede pública. Arq Bras Cardiol. 2012;99(5):1040–1048. doi: 10.1590/s0066-782x2012005000100. [DOI] [PubMed] [Google Scholar]