Abstract
Background
Systemic hypertension is highly prevalent and an important risk factor for cardiovascular events. Blood pressure control in hypertensive patients enrolled in the Hiperdia Program, a program of the Single Health System for the follow-up and monitoring of hypertensive patients, is still far below the desired level.
Objective
To describe the epidemiological profile and to assess blood pressure control of patients enrolled in Hiperdia, in the city of Novo Hamburgo (State of Rio Grande do Sul, Brazil).
Methods
Cross-sectional study with a stratified cluster random sample, including 383 adults enrolled in the Hiperdia Program of the 15 Basic Health Units of the city of Porto Alegre, conducted between 2010 and 2011. Controlled blood pressure was defined as ≤140 mmHg × 90 mmHg. The hypertensive patients were interviewed and their blood pressure was measured using a calibrated aneroid device. Prevalence ratios (PR) with 95% confidence interval, Wald's χ2 test, and simple and multiple Poisson regression were used in the statistical analysis.
Results
The mean age was 63 ± 10 years, and most of the patients were females belonging to social class C, with a low level of education, a sedentary lifestyle, and family history positive for systemic hypertension. Diabetes mellitus (DM) was observed in 31%; adherence to the antihypertensive treatment in 54.3%; and 33.7% had their blood pressure controlled. DM was strongly associated with inadequate BP control, with only 15.7% of the diabetics showing BP considered as controlled.
Conclusion
Even for hypertensive patients enrolled in the Hiperdia Program, BP control is not satisfactorily reached or sustained. Diabetic hypertensive patients show the most inappropriate BP control.
Keywords: Hypertension / complications, Risk factors, Hypertension / epidemiology, Government Programs, Epidemiological Monitoring, Medication Adherence
Introduction
Chronic non-communicable diseases (CNCDs) represent one of the major health challenges for the global development in the coming decades1. Among them, systemic hypertension is an important risk factor for cardiovascular diseases and is present in 69% of patients with a first myocardial infarction, in 77% of patients with a first stroke, in 74% of patients with chronic heart failure, and in 60% of patients with peripheral artery disease2.
Blood pressure control in hypertensive patients is closely related to adherence to the treatment prescribed. Medication non-adherence is a major concern for health care professionals and stakeholders, so that studies are required to improve adherence to antihypertensive treatments, especially in hypertensive patients at a high cardiovascular risk. In these patients, control of complications may significantly reduce mortality for these diseases, as well as the costs of treating these complications3. Additionally, an inadequate blood pressure control may increase the risk of hypertensive crises with the need for hospitalization4. Several factors may be related to adherence, including the patients' characteristics, quality of the doctor-patient relationship, severity of disease, access to health care, and specific factors related to the drug prescription5.
Thus, the objective of this study is to describe the epidemiological profile of and to evaluate blood pressure control in patients enrolled in the Hiperdia Program, analyzing their association with socioeconomic aspects; cigarette smoking and alcohol intake; family history for SH; treatment adherence; awareness of adequate practices to health; and participation in health education groups - involving patients with hypertension and diabetes mellitus, and performance of physical activities in a mid-sized city in Southern Brazil.
Methods
This is a cross-sectional study with a territory-based random sample stratified by Basic Health Unit (Unidade Básica de Saúde - UBS), comprising the Basic Health Care Network of Novo Hamburgo (State of Rio Grande do Sul, Brazil). All 15 UBS of the city were included, as shown in Table 1. A proportional raffle was carried out according to the number of patients enrolled in Hiperdia6 in each UBS, ordered in numbered tables for each unit. The Hiperdia Program was developed by the Ministry of Health for the enrollment, follow-up and assessment of hypertensive patients, generating quantitative reports according to the patients' age range, gender, medications used, and follow-up of blood pressure. Data inclusion is in charge of the city health departments.
Table 1.
Patients registered In the Hiperdia Program of Novo Hamburgo (RS) — 2011
| UBS | Hypertension | Hypertension + DM | Total | Stratified sample | Unanswered questionnaires | Answered questionnaires |
|---|---|---|---|---|---|---|
| TOTAL | 3.722 | 865 | 4.587 | 383 | 30 | 353 |
| Santo Afonso | 828 | 155 | 983 | 82 | 7 | 75 |
| Hamburgo Velho | 296 | 69 | 365 | 30 | 2 | 28 |
| Hamburgo Velho | 225 | 64 | 289 | 24 | 2 | 22 |
| Guarani | 178 | 31 | 209 | 17 | 1 | 16 |
| Canudos | 554 | 135 | 689 | 58 | 5 | 53 |
| Iguaçu | 67 | 11 | 78 | 7 | 0 | 7 |
| Lomba Grande | 250 | 68 | 318 | 26 | 2 | 24 |
| Rondônia | 87 | 14 | 101 | 9 | 1 | 8 |
| Kephas | 219 | 64 | 283 | 24 | 2 | 22 |
| Roselândia | 128 | 28 | 156 | 13 | 1 | 12 |
| Rincão | 320 | 41 | 361 | 30 | 2 | 28 |
| Kraemer | 78 | 45 | 123 | 10 | 1 | 9 |
| Redentora | 80 | 15 | 95 | 8 | 1 | 7 |
| Boa Saúde | 211 | 85 | 296 | 25 | 2 | 23 |
| Liberdade | 201 | 40 | 241 | 20 | 1 | 19 |
The following parameters were used for the calculation of the sample size: prevalence of systemic hypertension of 28%, 95% CI, and acceptable error of 5%, thus giving a total of 383 patients. Initially, a screening was made in the Hiperdia data base, to remove double-entered patient data due to errors in their name and family name spelling, patients enrolled in more than one UBS, and those diagnosed exclusively with diabetes mellitus. The subjects included were patients 20 years old or older, of both genders, enrolled in the Hiperdia Program, and diagnosed with hypertension (≥140 mmHg × 90 mmHg) or hypertension plus diabetes mellitus (≥130 mmHg × 80 mmHg). Patients institutionalized in hospitals or nursing homes, those imprisoned, or who had moved to other UBS zone or other city when the research questionnaire was administered, were excluded from the study.
The instruments used for data collection comprised a structured questionnaire including questions regarding the socioeconomic identification of the subject enrolled as hypertensive in Hiperdia, according to the Brazil Economic Classification Criterion (BECC)7; awareness about health care measures; risk factors such as cigarette smoking and sedentary lifestyle; family history; presence of DM; perception of the disease; and treatment adherence as assessed by the Morisky test8. The instrument was administered by trained interviewers, nurses or nursing technicians.
Blood pressure (BP) was measured using a Solidor aneroid device, batch BE15B, certified by Inmettro, according to the technique proposed by the VI Brazilian Guidelines of Systemic Hypertension9. Individual appointments for each study subject were scheduled in their respective UBS with the support of the City Health Department or by means of a domiciliary visit. Two BP measurements were taken; the first one after half the questionnaire had been administered, and the second one, after the questionnaire had been terminated, in the UBS itself or in the patients' home, when they could not attend the visit in the UBS. Data were collected between June 2010 and April 2011. For the quality control of data collection, the questionnaire was re-administered in 4% of the total sample, also selected in a random fashion according to the proportion of patients in each UBS, thus ensuring that every unit was evaluated. BP was also measured up to five days after the first data collection.
The interviewers participated in preparatory meetings for discussion and training so that the questionnaire would be correctly filled up, by administering it in a pilot study. Sphygmomanometer handling and Korotkoff sound auscultation were trained in practical workshops guided by an instructions manual.
Data were doubled entered in the Epidata program and analyzed using the Statistical Package for the Social Sciences (SPSS), version 19.0. The analysis included the calculation of measures of frequency; percentage for categorical variables and standard deviation for continuous variables contained in the questionnaire; and BP measurement. The measure of effect used was the prevalence ratio (PR), with 95% confidence interval, and Wald's χ2 test with simple and multiple Poisson regression.
Multivariate analysis was carried out using Poisson regression, considering p < 0.20 for the control of confounding factors, whose variables analyzed were: gender; age; level of education; socioeconomic classification; physical activity; cigarette smoking; time of awareness of hypertension; awareness of healthy habits regarding the use of salt; regular visits to the doctor; alcohol use; and presence of DM.
The research project was approved by the Research Ethics Committee under protocol no. UP 4344/09. All interviewees gave written informed consent.
Results
The data from 353 patients diagnosed with SH or SH plus DM were studied, because 30 individuals of the sample either refused to participate in the research, or had moved, or were institutionalized. Table 2 shows the sociodemographic characteristics of the study sample. Most of the sample was comprised of women (69.4%) and patients older than 60 years (62.1%); 64.7% of the interviewees belonged to social classes C1 and C2; 31% were diagnosed with DM. Blood pressure was not controlled in 63.3% of the hypertensive patients.
Table 2.
Characteristics of the sample of hypertensive patients enrolled in the Hiperdia Program of Novo Hamburgo (2011)
| Variables | Frequency (%) |
|---|---|
| Female gender | 245 (69.4) |
| Age, mean ± standard-deviation | 63 ± 10 |
| Skin color | |
| White | 316 (89.5) |
| Mixed | 16 (4.5) |
| Black | 21 (6.0) |
| Social class* | |
| B1 + B2 | 23 (6.5) |
| C1 | 86 (24.4) |
| C2 | 142 (40.3) |
| D + E | 101 (28.8) |
| Level of education | |
| Illiterate/Elementary school (1st to 4th) | 196 (57.8) |
| Elementary school (5th to 8th) | 125 (36.9) |
| High school/College | 18 (5.3) |
| Married/living with partner | 226 (65.9) |
Social class: Brazil Economic Classification Criterion, 2011.
In relation to the history of hospitalization in the past two years, 27.1% reported to have been hospitalized for SH or for a related condition. Of these, 4.1% had been hospitalized twice and 1.9%, more than three times.
Of the total of respondents, only 51 reported to participate in groups of hypertensive patients, which represent 47.1% of patients with controlled BP.
Table 3 shows the distribution of variables in relation to BP control as well as crude and adjusted prevalence ratios. In the crude analysis, BP control was significantly associated with the female gender, performance of physical activities, absence of DM, and awareness of the diagnosis of hypertension for less than 10 years.
Table 3.
Variables distribution of patients registered in the Hiperdia Program in relation to controlled BP
| N | Controlled BP | p* value | PR (95%CI) | Adjusted PR (95%CI) | p** value | |||
|---|---|---|---|---|---|---|---|---|
| Gender | ||||||||
| Male | 108 | 25% | - | 1.00 | 1.00 | - | ||
| Female | 245 | 37.60% | 0.016 | 1.50 (1.04 a 2.16) | 1.50 (0.81 a 2.79) | 0.197 | ||
| Age | ||||||||
| < 60 years | 133 | 38.30% | - | 1.00 | 1.00 | - | ||
| ≥ 60 years | 220 | 30.90% | 0.148 | 0.81 (0.60 a 1.08) | 0.87 (0.57 a 1.33) | 0.533 | ||
| Level of education | ||||||||
| Up to 4th grade | 196 | 29.60% | - | 1.00 | 1.00 | - | ||
| High school | 125 | 38.40% | 0.099 | 1.30 (0.95 a 1.77) | 0.91 (0.59 a 1.40) | 0.657 | ||
| or above | 18 | 33.30% | 0.735 | 1.13 (0.57 a 2.24) | 0.69 (0.26 a 1.82) | 0.449 | ||
| Marital status | ||||||||
| Married | 226 | 32.70% | - | 1.00 | - | - | ||
| Other | 117 | 34.20% | 0.787 | 1.04 (0.76 a 1.43) | - | - | ||
| ABEP Class | ||||||||
| B1 + B2 | 23 | 34.80% | 0.212 | 1.53 (0.79 a 2.97) | 1.95 (0.47 a 8.15) | 0.361 | ||
| C1 | 86 | 41.90% | 0.006 | 1.84 (1.19 a 2.84) | 2.70 (1.32 a 5.52) | 0.006 | ||
| C2 | 142 | 36.60% | 0.026 | 1.61 (1.06 a 2.45) | 2.26 (1.22 a 4.54) | 0.022 | ||
| D + E | 101 | 22.80% | - | 1.00 | 1.00 | - | ||
| Physical activity | ||||||||
| Do not perform physical activity | 64 | 15.60% | - | 1.00 | 1.00 | - | ||
| Perform physical activity | 164 | 36.00% | 0.007 | 2.30 (1.26 a 4.21) | 1.82 (0.95 a 3.45) | 0.071 | ||
| Cigarette smoking | ||||||||
| Do not smoke | 266 | 36.10% | - | 1.00 | 1.00 | - | ||
| Smoker | 27 | 25.90% | 0.324 | 0.72 (0.37 a 1.37) | 0.92 (0.31 a 2.77) | 0.885 | ||
| Former smoker | 60 | 26.70% | 0.187 | 0.74 (0.47 a 1.16) | 0.93 (0.46 a 1.89) | 0.839 | ||
| Alcohol intake | ||||||||
| No | 332 | 34.90% | - | 1.00 | 1.00 | - | ||
| Yes | 21 | 14.30% | 0.098 | 0.41 (0.14 a 1.18) | 0.62 (0.15 a 2.56) | 0.512 | ||
| Perceived health status | ||||||||
| Very good/good/regular | 311 | 34.10% | 0.926 | 1.02 (0.64 a 1.64) | - | - | ||
| Poor/very poor | 39 | 33.30% | - | 1.00 | - | - | ||
| Diabetes | ||||||||
| No DM | 245 | 41.60% | < 0.001 | 2.65 (1.67 a 4.19) | 2.39 (1.22 a 4.68) | 0.011 | ||
| With DM | 108 | 15.70% | - | 1.00 | 1.00 | - | ||
| Family history of SH | ||||||||
| Negative | 145 | 35.20% | - | 1.00 | - | - | ||
| Positive | 197 | 34.00% | 0.823 | 0.97 (0.72 a 1.30) | - | - | ||
| Adherence | ||||||||
| Adherent | 189 | 36.00% | - | 1.00 | - | - | ||
| Non-adherent | 159 | 30.20% | 0.257 | 0.84 (0.62 a 1.14) | - | - | ||
| Time of awareness of SH | ||||||||
| > 10 years | 164 | 25.60% | - | 1.00 | 1.00 | - | ||
| < 10 years | 171 | 39.20% | 0.009 | 1.53(1.11 a 2.11) | 1.13 (0.71 a 1.78) | 0.610 | ||
| Participation in groups | ||||||||
| Do not participate | 299 | 33.40% | - | 1.00 | - | - | ||
| Participate | 51 | 35.30% | 0.794 | 1.05 (0.70 a 1.58) | - | - | ||
| Lifestyle change | ||||||||
| Healthy diet | ||||||||
| Did not mention | 46 | 30.40% | - | 1.00 | - | - | ||
| Mentioned | 307 | 34.20% | 0.622 | 1.12 (0.71 s 1.79) | - | - | ||
| Salt intake control | ||||||||
| Did not mention | 103 | 27.20% | - | 1.00 | - | - | ||
| Mentioned | 250 | 36.40% | 0.108 | 1.34 (0.94 a 1.91) | 1.20 (0.78 a 1.84) | 0.418 | ||
| See doctor | ||||||||
| Did not mention | 143 | 28.70% | - | 1.00 | - | - | ||
| Mentioned | 210 | 37.10% | 0.105 | 1.29 (0.95 a 1.77) | 1.03 (0.69 a 1.54) | 0.892 | ||
Wald's χ2 test obtained in the Poisson's simple regression analysis.
Wald's χ2 test obtained in the Poisson's multiple regression analysis.
DM: diabetes mellitus; SH: systemic hypertension; CI: confidence interval; BP: blood pressure; PR: prevalence ratio.
In the adjusted analysis, only the presence of DM remained as a factor associated with BP control, and only 15.7% of hypertensive patients with diabetes showed controlled BP in comparison to 41% of controlled BP among non-diabetic hypertensive patients (p = 0.011).
Of the hypertensive patients assessed, 96.9% were aware of the diagnosis of SH for 14 ± 9 years and 54.3% reported treatment adherence. There was no statistically significant difference between non-adherent and adherent patients in relation to BP control (p = 0.257).
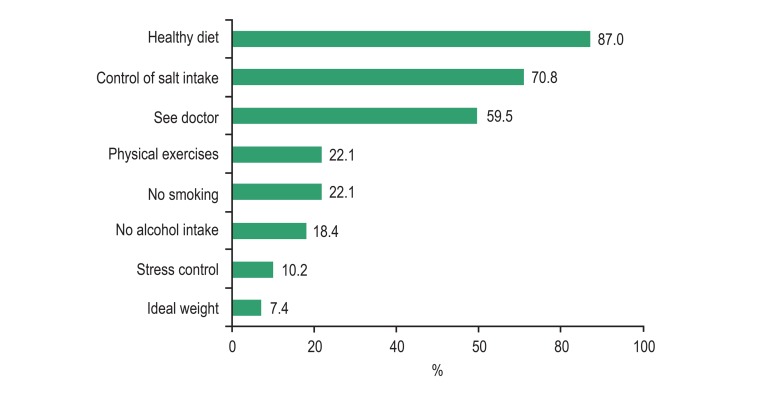
As regards awareness of important measures to maintain good health, 87% reported to be aware of the importance of a healthy diet, 70.8% reported to be aware that they should control salt intake, and 59.5% said they were aware they should see the doctor regularly (Figure 1).
Figure 1.
Awareness of relevant measures to keep good health.
Discussion
In this cross-sectional study, we observed that, albeit receiving antihypertensive treatment, the hypertensive patients assessed showed unsatisfactory blood pressure levels, with low BP control and insufficient treatment adherence. However, they were aware of the importance of adopting good lifestyle practices.
The proportion of patients with controlled BP was similar to that of other studies10,11 corrected for normal BP parameters for hypertensive and diabetic hypertensive patients, and was much lower than that found in individuals seen in community-based services in the United States12, where 71.4% of hypertensive patients were controlled. However, results more similar to ours were found in a study conducted in 26 countries13, with 23.7% of patients with controlled BP. The changes recommended by national8 and international14 guidelines are necessary to improve BP control.
In a study with non-adherent patients3, adherence reached 72.3% after mail interventions. Another study, with Finnish public workers5, found 79.6% of treatment adherence in a cohort that analyzed recordings of pharmacy sales; and yet another, using telephone survey15, reported adherence of 61% of hypertensive patients. Rates of treatment adherence range from 50% to 90% among hypertensives16. In order to improve these rates, it is necessary to implement measures of primary health care17.
A significant association was observed between time of awareness of the diagnosis of systemic hypertension and BP control in the bivariate analysis, but not in the multivariate analysis. In another study, opposite results were found, with time of awareness of the diagnosis being associated with a poorer blood pressure control18.
Women comprised the major part of our study sample, like in other studies19-22, and they sustained better BP control in comparison to men (25% and 37.6%, respectively). Fucks's population-based study23 found a greater number of hypertensive women, but a slightly smaller number of individuals above 60 years of age.
The proportion of women and elderly individuals enrolled in Hiperdia is greater than that of population-based studies, precisely because these populations tend to seek health services more frequently. This is important to help guide planning measures in the care of hypertensive patients, with possible active search of less represented populations, such as those of men and patients younger than 60 years of age.
In another study conducted in a group of UBS in São Paulo18, the percentage of BP control among men was 30.9%, and 52.6% among women. These findings were better than ours, but worse than those of patients followed up in an outpatient service in Rio de Janeiro, where only 27% had controlled BP24.
The frequency of diabetes mellitus among the hypertensive patients analyzed was 31%, identical to that of another study13 on the control of hypertension and cardiometabolic risk. Hypertension control, as assessed in a specialized service25, was found in only 13.4% of diabetic hypertensive patients. The presence of diabetes mellitus in hypertensive patients characterizes a scenario in which it is more difficult to control BP according to the parameters elected as ideal by the VI Brazilian Guidelines of Hypertension9. In our study, DM as a comorbidity was associated with worse BP control in hypertensive patients. In view of these findings, we conclude that diabetic hypertensive patients require closer follow-up and support from the health care team and their family in order to adhere to treatment and improve their lifestyle as a condition to achieve better results in their BP control.
The percentage of patients who had attended school up to the 4th grade was 57.8%, and 64.7% among individuals from economic classes C1 and C2. Fuchs et al23, Gus et al26 and Piccini and Victora27 found association between low level of education and hypertension, and stated that poor life conditions predispose to the development of diseases. For Piccini et al28, the level of education was associated with blood pressure control, with worse control among those had attended school for fewer years. This factor, associated with hypertension, may be classified as a modifiable risk factor.
The frequency of cigarette smoking and alcohol intake reported by the hypertensive patients was lower than that usually found in the literature10,18; still, alcohol intake was associated with poorer BP control.
In our study, more than half of the interviewees reported not to perform physical activities. This corroborates the findings of other studies10,18,29. Nonetheless, albeit reaching borderline significance in the adjusted analysis, physical activity contributed to BP control.
In our study, it was not possible to compare patients participating in groups of hypertensive individuals with those not participating, due to the low attendance rate and small number of groups formed in the UBS, where only 14.4% of the respondents reported to participate in group activities in the past year. This intervention has been proved useful in the control of these chronic diseases18,29,30.
We found evidences that most of the hypertensive patients remain with inadequate BP control, especially those also diagnosed with DM. The latter have an almost three-time higher possibility of not having controlled BP in comparison to those diagnosed with SH alone, like observed in the ACCORD study31, therefore deserving careful attention on the part of health care teams. Diabetic hypertensive patients have a two- to six-time higher risk of cardiovascular death than hypertensive patients without diabetes32.
An effective patient follow-up is one of the most difficult goals to achieve in Hiperdia, whether due to the physical distance between patients and the health care services, or to difficulties reported by professionals to reach these patients in their homes, or also due to the lack of patient awareness regarding SH and DM. Also, these patients are strongly linked to factors of social vulnerability such as low level of education and lack of contact with the health care team; thus, the change in this panorama falls on the primary health care teams, with promotion and prevention actions, especially among diabetic hypertensive patients33.
It is important to consider possible study limitations characterized by measurement bias; current cigarette smoking and alcohol intake, whose percentages were much lower than those found in the literature; a possible influence of the observer, of the data collection environment, of the device used, and, finally, of the white coat effect. As regards the performance of physical activities, reverse causality bias may have occurred. Selection bias may also have occurred because the Hiperedia recordings of the 15 UBS do not include all hypertensive patients living in Novo Hamburgo. With the use of the Morisky test, recall bias may have occurred regarding the accuracy of the responses to the test. However, the findings showed low adherence, which seems to reflect real life.
Further research on Hiperdia and BP control is still necessary in the Brazilian Southern region. Our findings will help plan actions to improve the access of Hiperdia users to primary health care measures, such as: monitoring of diabetic hypertensive patients through monthly visits of community health care agents; quantitative and qualitative assessment of Hiperdia recordings, aiming to improve patient enrollment; implementation of the recommendations of the VI Guidelines of SH9, especially for diabetic hypertensive patients; automation of UBSs for full operation of the enrollment system; enrollment in the Health Clubs Project of the Ministry of Health; training of multidisciplinary teams (NASF); and enrollment in the Care of people with Chronic Diseases Network of the Ministry of Health34.
Based on our findings, we can conclude that blood pressure control in the patients studied is unsatisfactory and that this control is even harder in diabetic patients. Thus, a policy of emphasis on this group of patients should be developed.
Footnotes
Author contributions
Conception and design of the research, Analysis and interpretation of the data, Statistical analysis, Writing of the manuscript and Critical revision of the manuscript for intellectual content: Souza CS, Stein AT, Bastos GAN, Pellanda LC; Acquisition of data: Souza CS, Bastos GAN; Obtaining financing: Pellanda LC.
Potential Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Sources of Funding
This study was funded by Fundo de apoio à pesquisa do ICFUC (FAPICC).
Study Association
This article is part of a thesis submitted by Clarita Silva de Souza to obtain her masters' degree from Instituto de Cardiologia/Fundação Universitária de Cardiologia do Rio Grande do Sul.
References
- 1.Casado L, Viana LM, Thuler LC. Fatores de risco para doenças crônicas não transmissíveis no Brasil: uma revisão sistemática. Rev Bras Cancerol. 2009;55(4):379–388. [Google Scholar]
- 2.Aronow WS. Treatment of systemic hypertension. Am J Cardiovasc Dis. 2012;2(3):160–170. [PMC free article] [PubMed] [Google Scholar]
- 3.Jing S, Naliboff A, Kaufman MB, Choy M. Descriptive analysis of mail interventions with physicians and patients to improve adherence with antihypertensive and antidiabetic medications in a mixed-model managed care organization of commercial and Medicare members. J Manag Care Pharm. 2011;17(5):355–366. doi: 10.18553/jmcp.2011.17.5.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cordero A, Bertomeu-González V, Moreno-Arribas J, Agudo P, López-Palop R, Masiá MD, et al. Burden of systemic hypertension in patients admitted to cardiology hospitalization units. Am J Cardiol. 2011;108(11):1570–1575. doi: 10.1016/j.amjcard.2011.07.016. [DOI] [PubMed] [Google Scholar]
- 5.Oksanen T, Kawachi I, Kouvonen A, Suzuki E, Takao S, Sjösten N, et al. Workplace social capital and adherence to antihypertensive medication: a cohort study. PloS One. 2011;6(9): doi: 10.1371/journal.pone.0024732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brasil. Ministério da Saúde. Departamento de Informação e Informática do Sistema Único de Saúde [Acesso em 2011 out. 20];Sistema de Informação Hiperdia [on-line] Disponível em: http:/hiperdia.datasus.gov.br.
- 7.Associação Brasileira de Empresas de Pesquisa Critério de Classificação Econômica Brasil [on-line] 2011. [Acesso em 2011 set.12]. Disponível em: www.abep.org/novo/Content.aspx?ContentID=302.
- 8.Ben AJ, Neumann CR, Mengue SS. Teste de Morisky-Green e Brief Medication Questionare para avaliar adesão a medicamentos. Rev Saúde Pública. 2012;46(2):279–289. doi: 10.1590/s0034-89102012005000013. [DOI] [PubMed] [Google Scholar]
- 9.Sociedade Brasileira de Cardiologia. Sociedade Brasileira de Hipertensão. Sociedade Brasileira de Nefrologia VI Diretrizes brasileiras de hipertensão. Arq Bras Cardiol. 2010;95(1) supl.1:1–51. [PubMed] [Google Scholar]
- 10.Lima LM, Schwartz E, Muniz RM, Zilmer JG, Ludtke I. Perfil dos usuários do Hiperdia de três unidades básicas de saúde do sul do Brasil. Rev gaúch enferm. 2011;32(2):323–329. doi: 10.1590/s1983-14472011000200016. [DOI] [PubMed] [Google Scholar]
- 11.Santa Helena ET, Nemes MI, Eluf J., Neto Avaliação da assistência a pessoas com hipertensão arterial em Unidades de Estratégia Saúde da Família. Saude Soc São Paulo. 2010;19(3):614–626. [Google Scholar]
- 12.Romanelli RJ, Schiro TA, Jukes T, Wong KS, Ishisaka DY. Disparities in blood pressure control within a community-based provider network: an exploratory analysis. Ann Pharmacotter. 2011;45(12):1473–1482. doi: 10.1345/aph.1Q523. [DOI] [PubMed] [Google Scholar]
- 13.Thoenes M, Bramlage P, Zhong S, Shang S, Volpe M, Spirk D. Hypertension control and cardiometabolic risk: a regional perspective. Cardiol Res Pract. 2012;2012:925046. doi: 10.1155/2012/925046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Institute for Health and Clinical Excellence - NICE [acesso em 2011 out.20];Prevetion of cardiovascular disease at population level [on-line] 2010 Disponível em: http://www.nice.org.uk/guidance/PH25.
- 15.Nair KV, Belletti DA, Doyle JJ, Allen RR, McQueen RB, Saseen JJ, et al. Understanding barriers to medication adherence in the hypertensive population by evaluating responses to a telephone survey. Patient Prefer Adherence. 2011;5:195–206. doi: 10.2147/PPA.S18481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bugalho A, Carneiro AV. Intervenções para aumentar a adesão terapêutica em patologias crônicas. Lisboa: Centro de Estudos de Medicina Baseada em Evidência; 2004. pp. 9–16. [Google Scholar]
- 17.Souza LG, Menandro MC. Atenção primária à saúde: diretrizes, desafios e recomendações. Revisão de bibliografia internacional. Physis. 2011;21(2):517–539. [Google Scholar]
- 18.Pierin AM, Marroni SN, Taveira LA, Benseñor IJ. [Hypertension control and related factors at primary care located in the west side of the city of São Paulo, Brazil]. Cien Saúde Colet. 2011;16(Suppl 1):1389–1400. doi: 10.1590/s1413-81232011000700074. [DOI] [PubMed] [Google Scholar]
- 19.Rosário TM, Scala LC, França GV, Pereira MR, Jardim PC. Prevalência, controle e tratamento da hipertensão arterial sistêmica em Nobres - MT. Arq Bras Cardiol. 2009;93(6):672–678. doi: 10.1590/s0066-782x2009001200018. [DOI] [PubMed] [Google Scholar]
- 20.Duarte MT, Cyrino AP, Cerqueira AT, Nemes MI, Iyda M. Motivos do abandono do seguimento médico no cuidado a portadores de hipertensão arterial: a perspectiva do sujeito. Ciênc Saúde Coletiva. 2010;15(5):2603–2610. doi: 10.1590/s1413-81232010000500034. [DOI] [PubMed] [Google Scholar]
- 21.Cesarino CB, Cipullo JP, Martin JF, Ciorlia LA, Godoy MR, Cordeiro JA, et al. Prevalência e fatores sociodemográficos em hipertensos de São José do Rio Preto - SP. Arq Bras Cardiol. 2008;91(1):29–35. doi: 10.1590/s0066-782x2008001300005. [DOI] [PubMed] [Google Scholar]
- 22.Rosini N, Machado MJ, Xavier HT. Estudo da prevalência e multiplicidade de fatores de risco cardiovascular em indivíduos hipertensos da cidade de Brusque, SC, Brasil. Arq Bras Cardiol. 2006;86(3):219–222. doi: 10.1590/s0066-782x2006000300010. [DOI] [PubMed] [Google Scholar]
- 23.Fuchs FD, Moreira LB, Moraes RS, Bredemeier M, Cardozo SC. Prevalência de hipertensão arterial sistêmica e fatores associados na região urbana de Porto Alegre. Estudo de base populacional. Arq Bras Cardiol. 1994;63(6):473–479. [PubMed] [Google Scholar]
- 24.Muxfeldt ES, Nogueira Ada R, Salles GF, Bloch KV. Características clínicas e demográficas dos pacientes hipertensos acompanhados no ambulatório de clínica médica de um hospital universitário na cidade do Rio de Janeiro. São Paulo Med J. 2004;122(3):87–93. doi: 10.1590/S1516-31802004000300003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Freitas JB, Tavares A, Kohlmann O, Jr, Zanella MT, Ribeiro AB. Estudo transversal sobre o controle da pressão arterial no serviço de nefrologia da Escola Paulista de Medicina - Unifesp. Arq Bras Cardiol. 2002;79(2):123–128. doi: 10.1590/s0066-782x2002001100003. [DOI] [PubMed] [Google Scholar]
- 26.Gus I, Harzhein E, Zaslavsky C, Medina C, Gus M. Prevalência da hipertensão arterial sistêmica no Rio Grande do Sul e fatores de risco associados. Arq Bras Cardiol. 2004;83(5):424–428. doi: 10.1590/s0066-782x2004001700009. [DOI] [PubMed] [Google Scholar]
- 27.Piccini RX, Victora CG. Hipertensão arterial sistêmica em área urbana no sul do Brasil: prevalência e fatores de risco. Rev Saúde Pública. 1994;28(4):261–267. doi: 10.1590/s0034-89101994000400004. [DOI] [PubMed] [Google Scholar]
- 28.Piccini RX, Facchini LA, Tomasi E, Siqueira FV, Silveira DS, Thumé E, et al. Promoção, prevenção e cuidado da hipertensão arterial no Brasil. Rev Saúde Pública. 2012;46(3):543–550. doi: 10.1590/s0034-89102012005000027. [DOI] [PubMed] [Google Scholar]
- 29.Teixeira ER, Silva JC, Lamas AR, Matos RM. O estilo de vida do cliente com hipertensão arterial e o cuidado com a saúde. Esc Anna Nery Rev Enferm. 2006;10(3):378–384. [Google Scholar]
- 30.Silva TR, Feldmam C, Lima MH, Nobre MC, Domingues RZ. Controle de diabetes mellitus e hipertensão arterial com grupos de intervenção educacional e terapêutica em seguimento ambulatorial de uma Unidade Básica de Saúde. Saúde e Sociedade. 2006;15(3):180–189. [Google Scholar]
- 31.Cushman WC, Evans GW, Byington RP, Goff DC, Jr, Grimm RH, Jr, Cutler JA, et al. ACCORD Study Group Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1575–1585. doi: 10.1056/NEJMoa1001286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gaede P, Vedel P, Larsen N, Jensen GV, Parving HH, Petersen O. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348(5):383–393. doi: 10.1056/NEJMoa021778. [DOI] [PubMed] [Google Scholar]
- 33.Carvalho FS, Filho, Nogueira LT, Viana LM, Costa AC, Silva AC. [Acesso em 2012 set.14];Programa Hiperdia: uma análise de aspectos de vulnerabilidade de usuários da atenção primária à saúde [on-line] 2012 Disponível em: http://189.75.118.68/cbcenf/sistemainscricoes/arquivosTrabalhos/I38083.E10.T7279.D6AP.pdf.
- 34.Brasil. Ministério da Saúde. Secretaria de Atenção à Saúde (SAS) [Acesso em 2012 nov.10];Consulta pública n.º 13 e 16, de 24 de setembro de 2012 [on-line] Disponível em: http://portalsaude.saude.gov.br/portalsaude/arquivos/pdf/2012/Set/25/cp16.pdf.