Abstract
Objective:
Prevention of self-injurious behaviour is an important priority in correctional settings given higher rates among inmates. Our study estimated the reported incidence of self-injury during the first 180 days in prison and tested potential risk and protective factors using official prison records.
Methods:
We conducted a retrospective cohort study using secondary data for 5154 admissions to the Correctional Service of Canada during 2011. Relative risks were estimated with Poisson regression. Recursive partitioning was used to create a parsimonious model of characteristics of offenders who engage in self-injury.
Results:
Thirty-six of 5154 (0.7%) offenders engaged in 1 or more incidents of self-injury during their first 180 days of incarceration. Educational and occupational achievement, family history, demographic factors, mental health service use, and results of mental health screening at intake were predictive of self-injury. Recursive partitioning models identified about 23% of inmates who presented with multiple risk factors, and had increased incidence of self-injury. A comparison of a model using information at intake to a model also incorporating events in prison suggested that events in prison added little to the detection of self-injury.
Conclusions:
Given high rates of most risk factors, screening for self-injury during early incarceration will be overinclusive. However, it may identify a group of inmates with complex needs for whom interdisciplinary responses are needed to address wide-ranging social, family, behavioural, and mental health deficits.
Keywords: deliberate self-harm, prisons, mass screening, social adjustment, cohort study, risk factors
Abstract
Objectif :
La prévention du comportement d’automutilation est une priorité importante des milieux correctionnels, étant donné leurs taux élevés chez les détenus. Notre étude a estimé l’incidence signalée d’automutilation durant les 180 premiers jours en prison, et vérifié le risque potentiel et les facteurs de protection à l’aide des dossiers carcéraux officiels.
Méthodes :
Nous avons mené une étude de cohorte rétrospective à l’aide des données secondaires de 5154 incarcérations à Service correctionnel Canada en 2011. Les risques relatifs ont été estimés avec la régression de Poisson. Le partitionnement récursif a servi à créer un modèle parcimonieux de caractéristiques des délinquants qui s’adonnent à l’automutilation.
Résultats :
Trente-six des 5154 (0,7 %) des délinquants ont eu 1 incident ou plus d’automutilation durant leurs 180 premiers jours d’incarcération. Le rendement scolaire et professionnel, les antécédents familiaux, les facteurs démographiques, l’utilisation des services de santé mentale, et les résultats du dépistage de la santé mentale à l’admission étaient prédicteurs d’automutilation. Les modèles de partitionnement récursif ont identifié environ 23 % des détenus qui présentaient de multiples facteurs de risque, et qui avaient une incidence accrue d’automutilation. Une comparaison d’un modèle utilisant l’information à l’admission avec un modèle incorporant aussi les événements en prison suggérait que les événements en prison ajoutaient peu à la détection de l’automutilation.
Conclusions :
Étant donné les taux élevés de la plupart des facteurs de risque, le dépistage de l’automutilation au début de l’incarcération sera modéré. Cependant, il peut identifier un groupe de détenus ayant des besoins complexes pour qui des réponses interdisciplinaires sont nécessaires pour traiter un large éventail de déficiences sociales, familiales, comportementales, et de santé mentale.
Preventing self-injury is an ongoing issue of concern in correctional environments because of the risk of death, other costs and consequences of self-injury to inmates and staff, and owing to legal obligations.1,2 According to a recent review,3 7% to 48% of offenders reported a history of self-injury, compared with 4% of adults in the community. However, few studies have made the distinction between self-injury that occurred in prison and that in the community; most studies have reported lifetime rates. Seventeen per cent of male prisoners in the United Kingdom self-reported a history of self-injury, although only 5% reported an incident while incarcerated.4 A retrospective cohort study5 using administrative data reported that 0.1% of offenders had at least 1 incident of self-injury during a 30-month period. Neither study controlled for unequal time at risk among inmates in their samples or the time that the inmate had been incarcerated prior to the incident. As noted by Lohner and Konrad,6 distress, and consequently the risk of self-injury, are considerably higher at intake to prison and following transfers between institutions.
There have been discrepant findings regarding self-injury predictors, which may in part be because of methodological differences between studies (for example, choice of comparison group and the definition of self-injury).3,6 Given that self-injury is relatively rare, predictors of self-injury often lack predictive power. Many demographic (for example, younger), social (for example, lower education, and adverse life events, such as histories of abuse), and clinical (for example, mental disorder) characteristics associated with self-injury are common in a prison population.6 Interactions may change the predictive power of specific factors, but this has rarely been considered in research. Dear7 argues that distress is a necessary ingredient for self-injury in prison. However, he proposes a model where the capacity for distress to lead to self-injury is also dependent on individual vulnerability, the prison environment, and the management of distress by the prison system. Incorporating interactions in risk assessment could offer an opportunity for a more dynamic assessment. In a clinical setting it could be the basis of a system that allows a person’s risk of self-injury to be updated regularly based on new information. It may be possible to improve the sensitivity or specificity of intake screening by incorporating information about the inmate’s behaviour in prison and the services that have been provided.
Clinical Implications
Inmates engaging in self-injury in prison have complex histories, with multiple related deficits that may impact treatment planning.
Interactions among risk factors should be considered to achieve a more manageable referral rate that prioritizes the highest needs cases.
Collaboration between mental health and security staff is needed to monitor for signs of increasing risk of self-injury.
Limitations
Underreporting of incidents may have affected our estimates of the risk associated with various factors in an unknown direction.
Our findings may not generalize to pre-trial or short-term detention jails and forensic hospitals, as inmates face different circumstances in these settings.
Longer-term follow-up studies are needed to identify whether risk factors for self-injury differ at various points of incarceration.
Our study aims were 4-fold:
to estimate the reported incidence of self-injury during the first 180 days in prison;
to test various demographic, clinical, and situational predictors of self-injury during the first 180 days of incarceration;
to create a parsimonious model to predict incidents of self-injury; and
to test the incremental predictive validity of incorporating information on events during early imprisonment relative to screening based solely on information available at intake to prison.
Methods
Context and Sample
In Canada, people convicted of a criminal offence and sentenced to 2 years or longer are incarcerated in a CSC prison. We sampled a retrospective cohort of all 5154 prisoners who were admitted to a CSC prison in 2011. An additional 26 prisoners who were incarcerated for less than 180 days in prison were excluded, as they were often released within less than 1 month and were missing data on most of the predictors. None had an incident of self-injury.
Data Collection
Data were retrieved from prison data sources: the CoMHISS, OMS, and the MHTS. CoMHISS is typically offered to inmates within 14 days of admission. At the time of the study, 2 self-report measures of psychological distress were administered: the DHS8 and the BSI.9 Cut-off scores that balance the sensitivity and specificity of the tests in a prison population—developed in our previous work and recently adopted by CSC—are used in our study.10
The BSI is a 53-item, self-report inventory that captures psychological distress over the past 7 days on a 0 (never) to 4 (always) scale. The GSI is calculated by taking the average of all items. Nine subscale scores (somatization, obsessive–compulsive, interpersonal-sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism) are also calculated as the average of items on each respective scale.
The DHS consists of 39 true–false items to measure signs of depression, hopelessness, and risk for suicide. Seventeen items are used to calculate a depression score, and 10 measure hopelessness. The remaining 12 items were defined by the authors as critical items for suicide risk. The authors describe 5 items, as measuring historical suicide (that is, history of suicide attempts or ideation), 3 as current suicide ideation items, and 2 cognitive suicide items (that is, whether the person considers suicide to be an option). The last 2 critical items are a past diagnosis of depression and a friend or family member who completed suicide. In a validation study of the DHS, we found that a subset of 5 critical items related to previous self-injury, current thoughts of self-injury, multiple suicide attempts, or a suicide attempt in the last 2 years was optimal to balance statistical accuracy and policy considerations. We present results for the subscales presented by Mills and Kroner in the DHS user guide8 and this optimal set of 5 critical items.
The OMS is the electronic case management file used by prison staff. Staff use forced choice fields to record the type of incident and the inmate’s role (instigator, associate, or victim) and involvement (for example, commit, attempt to commit, or threaten to commit) in the incident. Our outcome variable was any self-inflicted incident, which captures intentional, direct injuring of body tissue without suicidal intent.11 We only included actions by the inmate (for example, commit or attempt to commit), and excluded threats. As part of the clinical assessment and service provision following an incident, the mental health professional (typically a psychologist) determines intent to the extent possible, and revises the coding of the incident as necessary. Historical underreporting of incidents of self-injury12 led to recent changes in reporting practices in CSC, such as allowing staff to enter multiple incident categories for the same incident. The first author reviewed 200 randomly selected files to validate file information. Two (1%) files had at least 1 incident of self-injury. There was 100% agreement between information coded based on file review and the extracted data. This does not address undetected incidents, and is based on a very small number of incidents, but tentatively suggests an improvement in the recording of self-injury.
We also collected data regarding sex, race, segregation admissions, treatment centre admissions, and responses to the OIA.13 This assessment includes 100 questions administered by a parole officer. We extracted responses to questions regarding employment, experience of abuse, family relations, leisure activities, community attachment, criminal history, and current offence. Finally, we extracted substance abuse ratings, based on a computerized assessment14 that includes the Michigan Alcoholism Screening Test, the Drug Abuse Screening Test, the Alcohol Dependence Scale, and the Severity of Dependence Scale. Ratings are on a 4-point scale, which we dichotomized into none and low, compared with moderate to severe, consistent with uses of the tool by CSC.15
The MHTS tracks primary mental health services provided to inmates (that is, excluding services in treatment centres). We created 2 binary variables. The first captured receipt of any primary mental health services. The second indicated any missed or refused contacts for primary mental health services.
Data Analysis
Analyses were conducted using PASW Statistics version 18 (IBM SPSS Inc, Armonk, NY). Poisson models with robust covariance estimators were fit using the GENLIN function to estimate RRs for each variable.16 We also considered combinations of individual variables in 4 areas that had multiple indicators or subscales: social history, family history, BSI results, and DHS results. We compared 2 approaches to combining individual indicators:
use of simple referral criteria, where any factor associated with increased risk would lead to referral; and
selecting the optimal number of risk factors to achieve a sensitivity of at least 80%.17
To address our secondary question, we created classification trees.18 The variable with the largest chi-square value was used to partition the sample until none of the chi-square values were significant at the P < 0.05 level or the subgroup had fewer than 5 offenders with an incident of self-injury. A minimum group size of 50 (about 1% of the sample) was selected to minimize overfitting the model.
Missing Data
Missing data owing to inmate refusals, resource issues, or other reasons are inevitable in research and in practice. Among our sample, 18.6% (n = 958) of inmates did not complete the CoMHISS, and 12.6% (n = 647) of inmates did not complete the OIA. Among those who completed the OIA, 509 (11.3%) did not answer at least 1 social history question, and 246 (5.5%) did not answer at least 1 family history question. Finally, 1.2% (n = 63) of inmates did not have a rating of their substance abuse level of need. In our validation of the DHS, we compared the characteristics of those who did and did not complete the CoMHISS. While their demographic characteristics, childhood experiences, and substance abuse needs were similar, those who did not complete the CoMHISS had worse outcomes in prison and higher rates of social risk factors. Among those who did not complete the OIA, there were no incidents of self-injury. They were also less likely to have institutional incidents or segregation admissions. Five hundred (77.3%) of the inmates who did not complete the OIA did complete the CoMHISS. They reported less psychological distress and histories or thoughts of self-injury.1 Inmates are excluded from bivariate analyses for variables on which they were missing data. All inmates are included in our classification trees, through the inclusion of missing data as a category. This reflects the potential use of a model in practice.
Ethics Review Board
Ethics approval was obtained from the Centre for Addiction and Mental Health Ethics Review Board. CSC’s Research Committee also reviewed and approved the research. Inmate consent was not obtained, as the analyses used secondary data.
Results
The sample was primarily male (n = 4840; 93%), with a mean age of 34.9 (SD 11.8). Based on self-report data from prison files, 57.5% of participants (n = 2964) are of white race, 20.9% (n = 1077) are Aboriginal (First Nations, Métis, or Inuit), and 9.2% (n = 472) are black (race codes are reported as per the standardized race categories used by all Canadian federal government departments19). Race was missing for 206 (4.0%) participants.
There were 36 (0.7%) inmates who had at least 1 incident of self-injury during the first 180 days of incarceration. Table 1 shows the cumulative incidence of self-injury stratified by each risk factor. Most variables were associated with increased incidence of self-injury among those for whom the factor was present. However, completion of the suicide awareness workshop and a current conviction for a drug crime were associated with a significantly lower incidence of self-injury. Receipt of primary mental health services, having a violent incident, being a prior victim of spousal assault, and a current homicide conviction also had rate ratios of less than one, although they were not statistically significant. Similarly, a small number of variables were associated with modest (but not statistically significant) increases in the incidence of self-injury, including Aboriginal race, and previous offences, either as a youth or an adult.
Table 1.
RR of self-injury by risk factor
| Risk factor | Factor present
|
Factor not present
|
RR (95%CI) | ||
|---|---|---|---|---|---|
| n (%) | Inc, % | n (%) | Inc, % | ||
| Female | 339 (7) | 1.77 | 4815 (93) | 0.62 | 2.84 (1.19–6.78) |
| Aboriginal | 1077 (22) | 1.02 | 3871 (78) | 0.62 | 1.65 (0.81–3.35) |
| Age, years | |||||
| 26–49, compared with ≤25 | 3213 (62) | 0.96 | 1307 (25) | 0.38 | 2.52 (0.98–6.47) |
| ≥50, compared with ≤25 | 634 (12) | 0.0 | 1308 (25) | 0.38 | n/a |
| Social history | |||||
| <Grade 10 | 2428 (55) | 1.07 | 1975 (45) | 0.41 | 2.64 (1.20–5.83) |
| Unemployed at time of arrest | 2853 (65) | 1.05 | 1557 (35) | 0.32 | 3.28 (1.27–8.42) |
| Unstable accommodation | 1596 (36) | 1.57 | 2852 (64) | 0.39 | 4.06 (2.00–8.23) |
| Financial instability | 2872 (65) | 1.01 | 1580 (35) | 0.38 | 2.66 (1.11–6.39) |
| Has used social assistance | 2582 (60) | 1.08 | 1719 (40) | 0.29 | 3.73 (1.44–9.64) |
| Limited community attachment | 2092 (47) | 1.24 | 2333 (53) | 0.39 | 3.22 (1.51–6.86) |
| Leisure activities are limited | 2448 (56) | 1.23 | 1904 (44) | 0.21 | 5.83 (2.06–16.53) |
| Any social history factor | 4201 (94) | 0.86 | 265 (6) | 0.0 | n/a |
| At least 4 social history factors | 2520 (58) | 1.19 | 1837 (42) | 0.22 | 5.47 (1.93–15.49) |
| Victim of spousal abuse | 677 (15) | 0.74 | 3734 (85) | 0.80 | 0.92 (0.36–2.36) |
| Childhood family history | |||||
| Limited attachment to family | 1358 (30) | 1.55 | 3112 (70) | 0.45 | 3.44 (1.75–6.74) |
| Negative relations with parent | 2015 (45) | 1.29 | 2423 (55) | 0.33 | 3.91 (1.77–8.61) |
| Witnessed family violence | 1517 (35) | 1.12 | 2812 (65) | 0.53 | 2.10 (1.05–4.19) |
| Victim of abuse | 1615 (37) | 1.11 | 2751 (63) | 0.51 | 2.19 (1.09–4.39) |
| Any childhood family factors | 2602 (59) | 1.11 | 1815 (41) | 0.28 | 4.05 (1.57–10.43) |
| Criminal history | |||||
| Prior youth offences | 2081 (46) | 1.01 | 2451 (54) | 0.61 | 1.65 (0.85–3.19) |
| Previous adult offences | 3653 (80) | 0.90 | 912 (20) | 0.33 | 2.75 (0.84–8.93) |
| Current drug offence | 894 (20) | 0.11 | 3679 (80) | 0.95 | 0.12 (0.02–0.86) |
| Current violent offence | 1950 (43) | 1.23 | 2623 (57) | 0.46 | 2.69 (1.35–5.37) |
| Current sex offence | 680 (15) | 0.88 | 3890 (85) | 0.77 | 1.14 (0.48–2.74) |
| Current homicide offence | 356 (8) | 0.56 | 4217 (92) | 0.81 | 0.70 (0.17–2.89) |
| Substance abuse | 3020 (59) | 0.96 | 2071 (41) | 0.34 | 2.84 (1.25–6.47) |
| Events during incarceration | |||||
| Suicide awareness workshop | 1526 (30) | 0.13 | 3628 (70) | 0.94 | 0.14 (0.03–0.58) |
| Did not complete CoMHISS | 958 (19) | 1.98 | 4196 (81) | 0.41 | 4.89 (2.55–9.38) |
| Treatment centre admission | 171 (3) | 6.43 | 4983 (97) | 0.50 | 12.82 (6.42–25.63) |
| Received primary MH services | 3502 (68) | 0.63 | 1652 (32) | 0.85 | 0.74 (0.38–1.45) |
| Missed contact with MH staff | 308 (6) | 2.92 | 4846 (94) | 0.56 | 5.25 (2.49–11.05) |
| Segregation admission | 876 (17) | 1.71 | 4278 (83) | 0.49 | 3.49 (1.81–6.74) |
| Victim of incident | 132 (3) | 0.00 | 5022 (97) | 0.72 | n/a |
| Committed violent incident | 281 (5) | 0.36 | 4873 (95) | 0.72 | 0.50 (0.07–3.60) |
| Committed disciplinary incident | 487 (9) | 1.44 | 4667 (91) | 0.62 | 2.31 (1.02–5.25) |
CoMHISS = Computerized Mental Health Intake Screening System; Inc = cumulative incidence (that is, percentage with at least one incident of self-injury); MH = mental health; n/a = not defined due to incidence of 0 in 1 of the 2 groups
As seen in Table 1, 94% of inmates had at least 1 social history risk factor, thus limiting its predictive ability. Four or more social risk factors was the optimal cut-off to achieve a sensitivity of at least 80%. The 58% of inmates with 4 or more social risk factors were 5.47 times more likely to have an incident of self-injury. Fifty-nine per cent of inmates reported at least 1 childhood family history risk factor, and were 4.05 times more likely to have an incident of self-injury. One childhood family risk factor was the optimal cut-off to achieve 80% sensitivity.
As seen in Table 2, RRs were above 1 for all CoMHISS scales, indicating higher incidence of self-injury among those reporting distress. However, the lower limits of the RRs for the phobic anxiety and somatization subscales on the BSI were slightly below one, indicating marginal statistical significance. The RR for inmates who have a friend or family member who completed suicide was the lowest of all CoMHISS results, and the confidence interval ranged from 0.73 to 5.03, suggesting that it was a relatively weak predictor.
Table 2.
RR of self-injury based on mental health screening results (n = 4196)
| Screening result | Factor present
|
Factor not present
|
RR (95%CI) | ||
|---|---|---|---|---|---|
| n (%) | Inc, % | n (%) | Inc, % | ||
| Depression Hopelessness Suicide Screening Form | |||||
| Suicide ideation ≥ 1 | 215 (5) | 1.86 | 3981 (95) | 0.33 | 5.70 (1.87–17.33) |
| Cognitive suicide ≥ 1 | 353 (8) | 1.13 | 3843 (92) | 0.34 | 3.35 (1.10–10.22) |
| Historical suicide ≥ 1 | 993 (24) | 1.51 | 3203 (76) | 0.06 | 24.19 (5.54–105.61) |
| Friend or family completed suicide | 1121 (27) | 0.62 | 3075 (73) | 0.33 | 1.92 (0.73–5.03) |
| Past diagnosis of depression | 1089 (26) | 1.10 | 3107 (74) | 0.16 | 6.85 (2.42–19.39) |
| Depression ≥ 5 | 1893 (45) | 0.69 | 2303 (55) | 0.17 | 3.95 (1.29–12.11) |
| Hopelessness ≥ 1 | 2172 (52) | 0.60 | 2024 (48) | 0.20 | 3.03 (0.99–9.27) |
| Any of the above | 3040 (72) | 0.56 | 1156 (28) | 0.0 | n/a |
| ≥3 of the above | 1448 (35) | 1.04 | 2748 (65) | 0.07 | 14.23 (3.26–62.16) |
| ≥1 of the 5 critical items | 742 (18) | 2.02 | 3454 (82) | 0.06 | 34.91 (8.00–152.34) |
| Brief Symptom Inventory | |||||
| Somatization ≥ 0.41 | 1737 (41) | 0.63 | 2459 (59) | 0.24 | 2.60 (0.96–7.00) |
| Obsessive–compulsive ≥ 1.08 | 1332 (32) | 0.75 | 2864 (68) | 0.24 | 3.07 (1.17–8.05) |
| Interpersonal-sensitivity ≥ 0.915 | 1184 (28) | 0.84 | 3012 (72) | 0.23 | 3.63 (1.39–9.52) |
| Depression ≥ 0.815 | 1648 (39) | 0.85 | 2548 (61) | 0.12 | 7.22 (2.08–25.07) |
| Anxiety ≥ 0.615 | 1806 (43) | 0.78 | 2390 (57) | 0.13 | 6.18 (1.78–21.46) |
| Hostility ≥ 0.55 | 1292 (31) | 0.85 | 2904 (69) | 0.21 | 4.12 (1.53–11.12) |
| Phobic anxiety ≥ 0.005 | 2029 (48) | 0.59 | 2167 (52) | 0.23 | 2.56 (0.91–7.26) |
| Paranoid ideation ≥ 0.9 | 1718 (41) | 0.81 | 2478 (59) | 0.12 | 6.73 (1.94–23.39) |
| Psychoticism ≥ 0.5 | 2298 (55) | 0.61 | 1898 (45) | 0.16 | 3.85 (1.11–13.39) |
| Global Severity Index ≥ 0.765 | 1449 (35) | 0.90 | 2747 (65) | 0.15 | 6.16 (2.01–18.86) |
| Any of the above | 3149 (75) | 0.51 | 1047 (25) | 0.10 | 5.32 (0.71–40.07) |
| ≥5 of the above | 1623 (39) | 0.86 | 2573 (61) | 0.12 | 7.40 (2.13–25.70) |
Inc = cumulative incidence (that is, percentage with at least one incident of self-injury); n/a = not defined due to incidence of 0 in 1 of the 2 groups
Referring all inmates exceeding at least 1 cut-off on the DHS would result in a referral rate of 72%, and would detect all incidents of self-injury. Three or more cut-offs was the optimal cut-off to achieve a sensitivity of at least 80%. The 35% of inmates who exceeded at least 3 cut-offs were 14.23 times more likely to have an incident of self-injury. Seventy-five per cent of inmates exceeded at least 1 cut-off on the BSI, and were 5.32 times more likely to have an incident of self-injury. The optimal cut-off to achieve a sensitivity of 80% was 5 or more cut-offs. The 39% of inmates exceeding at least 5 cut-offs were 7.40 times more likely to have an incident of self-injury.
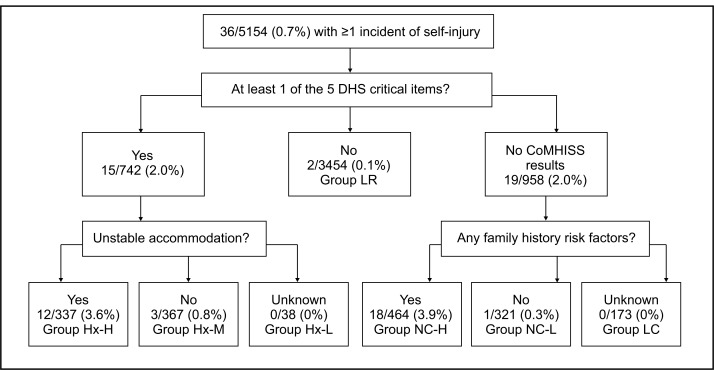
To address our third objective, we created 2 prediction trees. The first tree incorporated only the information collected at intake to prison. The intake tree (Figure 1), included only 3 variables—endorsement of 1 of the 5 DHS critical items, unstable accommodation at the time of arrest, and the presence of 1 or more family history variables. Seven groups are identified by the model. Two groups had an incidence of self-injury approaching 4%, which is roughly 5.5 times the population incidence. The groups included inmates endorsing 1 of the 5 DHS critical items and unstable accommodation at the time of arrest (labelled as group Hx-H in Figure 1) and CoMHISS noncompleters with at least 1 family risk factor (group NC-H). The group of inmates endorsing 1 of the 5 DHS critical items, who did not report unstable accommodation, had an incidence of 0.8%, similar to the total population. The remaining 4 groups had an incidence ranging from 0% to 0.3%.
Figure 1.
Intake tree predicting incidents of self-injury
- Group
- Characteristics of inmates in group
- Hx-H
- Reported at least 1 of the 5 Depression Hopelessness Suicide Screening Form (DHS) critical items and reported unstable accommodation at the time of arrest
- Hx-L
- Reported at least 1 of the 5 DHS critical items and with missing data regarding accommodation at the time of arrest
- Hx-M
- Reported at least 1 of the 5 DHS critical items and did not report unstable accommodation at the time of arrest
- LC
- Did not complete Computerized Mental Health Intake Screening System (CoMHISS) or the Offender Intake Assessment questions regarding family history
- LR
- Did not report any of the 5 DHS critical items
- NC-H
- Did not complete CoMHISS and reported at least one family history risk factor
- NC-L
- Did not complete CoMHISS and reported no family history risk factors
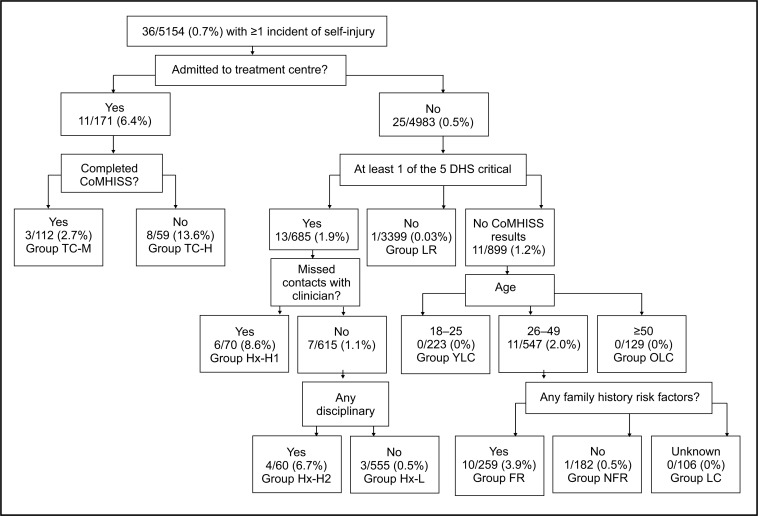
The second tree included events in prison to determine if this additional information could improve the prediction of self-injury. The events tree (Figure 2) was a more complex model. There were 11 groups of inmates, with incidence rates of self-injury ranging from 0% to 13.6%. The highest risk group in this model consisted of inmates admitted to a treatment centre without having completed the CoMHISS (group TC-H; incidence = 13.6%). Higher incidence of self-injury was also seen among those who were not admitted to a treatment centre but endorsed at least 1 of the 5 DHS critical items and either missed a primary mental health service (group Hx-H1; incidence = 8.6%) or who had a disciplinary incident (group Hx-H2; incidence = 6.7%). Finally, inmates from 26 to 49 years of age who did not have treatment centre admissions or complete the CoMHISS, but who reported at least 1 family risk factor, had an increased incidence of self-injury (group FR; incidence = 3.9%).
Figure 2.
Events tree predicting incidents of self-injury
- Group
- Characteristics of inmates in group
- FR
- No treatment centre admissions, did not complete Computerized Mental Health Intake Screening System (CoMHISS), age 26–49, and reported at least 1 family history risk factor
- Hx-H1
- No treatment centre admissions, reported at least 1 of the 5 Depression Hopelessness Suicide Screening Form (DHS) critical items and missed at least one contact with a clinician
- Hx-H2
- No treatment centre admissions, reported at least 1 of the 5 DHS critical items, no missed contacts with a clinician, and at least one disciplinary incident
- Hx-L
- No treatment centre admissions, reported at least 1 of the 5 DHS critical items, no missed contacts with a clinician, and no disciplinary incidents
- LC
- No treatment centre admissions, did not complete CoMHISS, age 26–49, and missing data regarding family history risk factors
- LR
- No treatment centre admissions and did not report any of the 5 DHS critical items
- NFR
- No treatment centre admissions, did not complete CoMHISS, age 26–49, and reported no family history risk factors
- OLC
- No treatment centre admissions, did not complete CoMHISS, and ≥50 years
- TC-H
- At least one admission to a Treatment Centre and did not complete CoMHISS
- TC-M
- At least one admission to a Treatment Centre and did complete CoMHISS
- YLC
- No treatment centre admissions, did not complete CoMHISS, and aged 18–25
Discussion
Our study is one of few population-based cohort studies on self-injury in prison. The findings highlight the challenges inherent in the prediction of rare events, such as self-injury. While many risk factors were highly common, only 0.7% of inmates had at least 1 documented incident of self-injury during their first 180 days in prison. Given that we relied on official prison records, this incidence is likely an underestimate of self-injury that reflects the most severe or challenging cases. Our findings are consistent with previous findings that while many factors are associated with increased risk of self-injury, most inmates with each risk factor did not have incidents. Conversely, less common risk factors (for example, suicide ideation) had high RRs, but most inmates who self-injured did not present with the risk factor. Our recursive partitioning models highlight the co-occurrence and complex relations among predictors of self-injury. They may offer a way to integrate numerous risk factors without overwhelming resources by referring most offenders.
Studying risk for self-injury through randomized controlled trials or without any intervention is almost always unethical.20 Therefore, it is difficult to accurately estimate the incidence of self-injury, as there are selection biases and confounding by indication regarding who receives interventions. Monitoring may have also differed based on perceived risk, which could impact detection of self-injury. Post hoc analyses (online eTables 3 and 4), show that many low-risk groups in our models had limited contact with prison staff. Undetected incidents may be more likely among these groups, although this is unlikely to fully explain the difference in incidence. Other groups with a low incidence of self-injury would be considered high risk based on their history of self-injury (for example, the Hx-M group in the intake tree and the Hx-L group in the event tree). As these groups had high rates of service use, it is unknown whether these groups are truly lower risk, or if incidents were prevented in these groups. If the latter explanation is true, this would suggest characteristics that buffer against high risk or that are related to responsiveness to interventions.
Subjectivity would be required if our models were used to develop screening protocols. Based on the consistent findings that a history of self-injury is the best predictor of future self-injury,3 all inmates with a history of self-injury in the intake tree (that is, all groups beginning with Hx) might be referred, as well as those who did not complete the CoMHISS, but reported at least 1 family history risk factor (group NC-H). This would result in a 23.4% referral rate, including 33 (91.7%) of 36 inmates who had an incident of self-injury. Similarly, the events tree could lead to a referral for inmates with treatment centre admissions (groups beginning with TC), any of the 5 DHS critical items (groups beginning with Hx) or for the group FR (inmates aged 26 to 49 years who did not complete the CoMHISS, with at least 1 family risk factor). This would lead to a slightly lower referral rate of 21.6%, including 34 (94.4%) of 36 of inmates with an incident of self-injury. Both models clearly lead to over-referral relative to the actual incidence of self-injury (for example, the positive predictive value of the intake tree would be 2.7%). However, those inmates who would be classified as false positives likely require further follow-up (and potentially treatment) in light of high rates of history of self-injury, distress, and adverse childhood and social histories, and increased likelihood of institutional infractions and incidents among the referral groups.
A comparison of the intake and events models reveals that events in prison did little to improve the prediction of self-injury during early imprisonment. While events during incarceration are strong predictors at a bivariate level, they may be common outcomes of an accumulation of family and social risk factors and psychological distress, rather than causes of self-injury. Misattribution of events in prison, such as rule violations and missed mental health contacts, as risk factors for self-injury—as opposed to risk markers21 or proxies for the true risk factor22—may lead to incorrect assumptions about the motivations of inmates who self-injure. Coid et al23 noted that it would be concerning if prisoners with severe mental illness were punished for illness-related behaviours rather than offered treatment. The events model may be of limited clinical use as it would suggest a passive approach of monitoring for additional warning signs rather than a proactive prevention approach. In other instances, the groups are those that are identified by already having a referral (for example, the treatment centre admission groups).
Replication of these findings is needed given the low incidence of self-injury and potential for underreporting of incidents. Similarly, longer follow-up is required to explore any potential differences in predictors of self-injury among inmates who have their first incident later during their incarceration. However, the intake tree suggests screening for risk of self-injury during early imprisonment may be possible with 10 questions. The questions could potentially be asked by a nonclinical staff member or through the use of computers.10 While the model inevitably results in overreferral relative to the incidence of self-injury, the rate of overreferral is significantly less than what would result from considering risk factors independently. Further, the characteristics of people who would be referred highlight significant challenges for prisons and ultimately communities. Over 20% of inmates were classified in moderate- to high-risk groups for self-injury, which had high rates of adverse social, family, and criminal histories and poor adjustment to prison. Addressing these deficits is likely to require multidisciplinary interventions during imprisonment and on release to the community. From a prevention perspective, the characteristics of these inmates also highlight the need for early interventions to reduce the impacts of early childhood events, poor social functioning, and symptoms of distress to prevent numerous long-term consequences, including self-injury.
Acknowledgments
Mr Martin is supported by a Vanier Canada Graduate Scholarship, and was previously supported by a Canadian Institutes of Health Research Training Fellowship through the Social Aetiology of Mental Illness Training Program. Dr Colman is supported by the Canada Research Chairs program. Mr Martin is currently on unpaid education leave from employment with CSC. Ms Dorken has also been previously employed by CSC. This research was supported by CSC, who provided access to data. However, CSC had no role in the conduct of the study. The views expressed are those of the authors, and do not necessarily reflect the views of CSC.
Abbreviations
- BSI
Brief Symptom Inventory
- CoMHISS
Computerized Mental Health Intake Screening System
- CSC
Correctional Service of Canada
- DHS
Depression Hopelessness Suicide Screening Form
- GSI
Global Severity Index
- MHTS
Mental Health Tracking System
- OIA
Offender Intake Assessment
- OMS
Offender Management System
- RR
relative risk
References
- 1.Lohner J, Konrad N. Deliberate self-harm and suicide attempt in custody: distinguishing features in male inmates’ self-injurious behavior. Int J Law Psychiatry. 2006;29(5):370–385. doi: 10.1016/j.ijlp.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 2.DeHart DD, Smith HP, Kaminski RJ. Institutional responses to self-injurious behavior among inmates. J Correct Health Care. 2009;15(2):129–141. doi: 10.1177/1078345809331444. [DOI] [PubMed] [Google Scholar]
- 3.Dixon-Gordon K, Harrison N, Roesch R. Non-suicidal self-injury within offender populations: a systematic review. Int J Forensic Ment Health. 2012;11(1):33–50. [Google Scholar]
- 4.Maden A, Chamberlain S, Gunn J. Deliberate self-harm in sentenced male prisoners in England and Wales: some ethnic factors. Crim Behav Ment Health. 2000;10(3):199–204. [Google Scholar]
- 5.Smith HP, Kaminski RJ. Inmate self-injurious behaviors: distinguishing characteristics within a retrospective study. Crim Justice Behav. 2009;37(1):81–96. [Google Scholar]
- 6.Lohner J, Konrad N. Risk factors for self-injurious behaviour in custody: problems of definition and prediction. Int J Prison Health. 2007;3(2):135–161. [Google Scholar]
- 7.Dear GE. Ten years of research into self-harm in the Western Australian prison system: where to next? Psychiatr Psychol Law. 2008;15(3):469–481. [Google Scholar]
- 8.Mills JF, Kroner DG. A new instrument to screen for depression, hopelessness, and suicide in incarcerated offenders. Psychol Serv. 2004;1(1):83–91. [Google Scholar]
- 9.Derogatis L. Brief Symptom Inventory: administration, scoring, and procedures manual. 4th ed. Minneapolis (MN): National Computer Systems; 1993. [Google Scholar]
- 10.Martin MS, Wamboldt AD, O’Connor SL, et al. A comparison of scoring models for computerised mental health screening for federal prison inmates. Crim Behav Ment Health. 2013;23(1):6–17. doi: 10.1002/cbm.1853. [DOI] [PubMed] [Google Scholar]
- 11.Usher A, Power J, Wilton G. Assessment, intervention, and prevention of self-injurious behaviour in correctional environments. Ottawa (ON): Correctional Service of Canada; 2010. [Google Scholar]
- 12.Gordon A. Self-injury incidents in CSC institutions over a thirty-month period. Ottawa (ON): Correctional Service of Canada; 2010. [Google Scholar]
- 13.Brown SL, Motiuk LL. The Dynamic Factors Identification and Analysis [DFIA] component of the Offender Intake Assessment [OIA] process: a meta-analytic, psychometric and consultative review. Ottawa (ON): Correctional Service of Canada; 2005. [Google Scholar]
- 14.Kunic D, Grant BA. The Computerized Assessment of Substance Abuse (CASA): results from the demonstration project. Ottawa (ON): Correctional Service of Canada; 2006. [Google Scholar]
- 15.Matheson FI, Doherty S, Grant BA. Women offender substance abuse programming and community reintegration. Ottawa (ON): Correctional Service of Canada; 2009. [Google Scholar]
- 16.Vittinghoff E, Glidden D, Shiboski S, et al. Regression methods in biostatistics. 2nd ed. New York (NY): Springer; 2012. [Google Scholar]
- 17.Zhou X-H, Obuchowski NA, McClish DK. Statistical methods in diagnostic medicine. 2nd ed. Hoboken (NJ): John Wiley & Sons, Inc; 2011. [Google Scholar]
- 18.Zhang H, Singer BH. Recursive partitioning and application. 2nd ed. New York (NY): Springer; 2010. [Google Scholar]
- 19.Statistics Canada. Population group of person [Internet] Ottawa (ON): Statistics Canada; 2012. [cited 2012 Sep 2]. Available from: http://www.statcan.gc.ca/concepts/defintions/ethnicity-ethnicite-eng.htm. [Google Scholar]
- 20.Mishara BL, Weisstub DN. Ethical and legal issues in suicide research. Int J Law Psychiatry. 2005;28(1):23–41. doi: 10.1016/j.ijlp.2004.12.006. [DOI] [PubMed] [Google Scholar]
- 21.Kraemer H, Kazdin A, Offord DR, et al. Coming to terms with the terms of risk. Arch Gen Psychiatry. 1997;54:337–343. doi: 10.1001/archpsyc.1997.01830160065009. [DOI] [PubMed] [Google Scholar]
- 22.Kraemer HC, Stice E, Kazdin A, et al. How do risk factors work together? Mediators, moderators and independent, overlapping, and proxy risk factors. Am J Psychiatry. 2001;158(6):848–856. doi: 10.1176/appi.ajp.158.6.848. [DOI] [PubMed] [Google Scholar]
- 23.Coid J, Petruckevitch A, Bebbington P, et al. Psychiatric morbidity in prisoners and solitary cellular confinement. I: disciplinary segregation. J Forens Psychiatry Psychol. 2003;14(2):298–319. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.