Abstract
Objective:
The concept of food addiction has recently been proposed by applying the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision, criteria for substance dependence to eating behaviour. Food addiction has received increased attention given that it may play a role in binge eating, eating disorders, and the recent increase in obesity prevalence. Currently, there is no psychometrically sound tool for assessing food addiction in French. Our study aimed to test the psychometric properties of a French version of the Yale Food Addiction Scale (YFAS) by establishing its factor structure and construct validity in a nonclinical population.
Method:
A total of 553 participants were assessed for food addiction (French version of the YFAS) and binge eating behaviour (Bulimic Investigatory Test Edinburgh and Binge Eating Scale). We tested the scale’s factor structure (factor analysis for dichotomous data based on tetrachoric correlation coefficients), internal consistency, and construct validity with measures of binge eating.
Results:
Our results supported a 1-factor structure, which accounted for 54.1% of the variance. This tool had adequate reliability and high construct validity with measures of binge eating in this population, both in its diagnosis and symptom count version. A 2-factor structure explained an additional 9.1% of the variance, and could differentiate between patients with high, compared with low, levels of insight regarding addiction symptoms.
Conclusions:
In our study, we validated a psychometrically sound French version of the YFAS, both in its symptom count and diagnostic version. Future studies should validate this tool in clinical samples.
Keywords: food addiction, addiction, addictive behaviour, Yale Food Addiction Scale, French, psychometrics, factor analysis, binge eating disorder, Bulimic Investigatory Test Edinburgh, Binge Eating Scale
Abstract
Objectif :
La dépendance alimentaire est un concept qui a été récemment proposé en appliquant au comportement alimentaire les critères de dépendance à une substance du Manuel diagnostique et statistique des troubles mentaux, 4e édition, révisé. La dépendance alimentaire a suscité une attention accrue car elle pourrait jouer un rôle dans la boulimie, les troubles alimentaires, et la récente augmentation de la prévalence de l’obésité. À l’heure actuelle, il n’y a pas d’instrument fiable sur le plan psychométrique pour évaluer la dépendance alimentaire en français. Notre étude visait à vérifier les propriétés psychométriques d’une version française de l’échelle de dépendance alimentaire de Yale (YFAS) en en établissant la structure factorielle, la cohésion interne, et la validité du construct dans une population non clinique.
Méthode :
Un total de 553 participants ont été évalués pour la dépendance alimentaire (version française de l’YFAS) et le comportement boulimique (questionnaire de dépistage de la boulimie d’Édinbourg et échelle de boulimie). Nous avons vérifié la structure factorielle de l’échelle (analyse factorielle pour les données dichotomiques d’après les coefficients de corrélation tétrachorique), la cohésion interne, et la validité du construct avec des mesures de la boulimie.
Résultats :
Nos résultats soutenaient une structure à 1 facteur, qui représentait 54,1 % de la variance. Nous avons démontré que cet instrument avait une fiabilité adéquate et une validité de construct élevée à l’aide de mesures de la boulimie dans cette population, tant dans sa version diagnostique que dans celle du compte de symptômes. Une structure à 2 facteurs expliquait un autre 9,1 % de la variance, et pouvait contribuer à différencier entre les patients ayant des niveaux élevés et ceux ayant des niveaux faibles de conscience à l’égard des symptômes de dépendance.
Conclusions :
Dans notre étude, nous avons validé une version française fiable sur le plan psychométrique de l’YFAS, tant dans sa version diagnostique que dans celle du compte de symptômes. Les futures études devraient valider cet instrument dans des échantillons cliniques.
Drug addictions are chronic relapsing disorders characterized by compulsion to seek and take the drug, a loss of control over drug-seeking and drug-taking behaviours, and the addictions typically involve maintaining drug use despite adverse consequences.1 In recent years, interesting clinical and scientific shifts in perspective have occurred, with many believing that addiction should include a person’s compulsive engagement in activities, such as gaming, Internet use, and shopping, in addition to pharmacologic rewards.2 Current debates have even extended the definition of addiction to, so-called, behavioural addictions (also called nonchemical addictions or nondrug addictions), which include the use of natural rewards, such as behaviours that are intrinsically necessary for our survival and in which we freely engage with pleasure and without social sanction, including sex, gambling, and eating.3,4 A growing body of evidence suggests that behavioural addictions resemble substance addictions across numerous domains, including natural history, phenomenology, tolerance, comorbidity, overlapping genetic contributions, neurobiological mechanisms, and responses to treatment.2 As a part of this growing body of research, the concept of food addiction has recently been proposed by applying the DSM-IV-TR criteria for substance dependence to eating behaviours. Patients who exhibit eating patterns that are similar to behaviours classically seen in patients with drug addiction are described as having a food addiction.5 This concept has received increasing attention given the role it may play in binge eating, eating disorders, and the recent increase in obesity prevalence.6 Although the evidence for and against the food addiction or compulsive eating model is debatable,6–8 and it is unclear whether this model explains the increased prevalence in obesity,9,10 the possibility that addiction to food represents a reliable phenotypical description of numerous patients is increasingly supported by research with humans and animals.5,11,12 Current literature5,12 suggests that a wide range of patients exhibit significant distress in their relations to food, lose control over their food consumption, suffer from repeated failed attempts to reduce their intake, and are unable to abstain from specific types of foods or reduce their consumption despite negative consequences.
Clinical Implications
Food addiction is a prevalent disorder that can be reliably assessed in French using the YFAS.
The French version of the YFAS has a 1-factor structure and a high construct validity with measures of binge eating.
A 2-factor structure explained an additional 9.1% variance, and may distinguish between patients with and without insight regarding addiction symptoms.
Limitations
We did not assess the YFAS factor structure, internal consistency, and validity in clinical samples.
The cross-sectional study design did not permit test–retest validity to be established.
Specifically, a growing body of research10,13 supports the hypothesis that specific types of food (for example, refined foods that are high in fat and sugar) may have addictive properties similar to those of classic substances, such as alcohol, tobacco, or cocaine. Refined food addiction has been proposed as a classic substance use disorder.10 Thus researchers have been motivated to apply the DSM-IVTR substance dependence criteria to the field of eating behaviours. Food addiction is diagnosed when at least 3 symptoms (1 of 7) are present during the past 12 months and a clinically significant impairment or level of distress is endorsed.
Therefore, a psychometrically sound tool for assessing food addiction that applies the DSM-IV-TR substance dependence criteria to the field of eating behaviours is needed. Gearhardt et al14 developed the YFAS to identify people who are exhibiting signs of addiction regarding specific types of food (for example, high fat and sugar) by extrapolating the 7 DSM-IV-TR criteria for substance dependence to the field of eating behaviours. This self-administered scale has demonstrated adequate reliability and validity in clinical and nonclinical samples, and is considered the gold standard for assessing food addiction. Studies using this scale have shown that food addiction is highly prevalent in a subpopulation of obese patients and in patients with binge eating disorders.15,16 In an examination of obese patients with binge eating disorders, the criteria for food addiction was met by 57% of the sample, and food addiction scores were significant predictors of binge eating frequencies, even when controlling for other factors, such as eating disorder psychopathology and negative affect.17 Moreover, scores on the YFAS correlated with neural activation patterns in a manner consistent with findings regarding substance dependence (for example, elevated activation in reward circuitry in response to food cues and reduced activation in inhibitory regions).18 These findings support the appropriateness of this scale for assessing food addiction.
To our knowledge, there is not currently a French version of the YFAS, and only a limited number of studies have assessed food addiction in non-United States and non-European locations. To date, no studies have been conducted in French-speaking countries, and Meule19 highlighted the need for studies that assess the prevalence of food addiction and the factors associated with food addiction.
Our study aimed to measure the psychometric properties of a French version of the YFAS with a nonclinical sample by establishing its factor structure, internal consistency, and construct validity with measures of binge eating behaviours.
Methods
Participants and Procedures
A total of 553 participants participated in our study. Participants completed a web-based questionnaire, which was created using Sphinx software (Sphinx Plus 2 version 5.1.0.4).20 The questionnaire included items regarding sociodemographic characteristics (for example, age, sex, and current BMI) and the following 3 self-administered scales: the YFAS, the BITE, and the BES.
We obtained permission from Ashley Gearhardt for the translation and validation of a French version of the YFAS. The YFAS translation procedure used in our study was consistent with existing guidelines for scale validation.21 First, the YFAS was translated from English to French by 3 translators who were qualified specialists in addiction, psychology, and psychiatry, and who were native French speakers. This step ensured the production of a translation that achieved consensus from all of the translators. Second, a translator whose native language was English performed a blind-backward translation of the initially translated version of the YFAS. Finally, a committee of 3 expert psychiatrists from the fields of addictive behaviours and eating disorders compared the back-translated scale with the initially translated version of the YFAS to produce a final French version of the YFAS. The committee’s aims were to verify the cross-cultural equivalence of the source and final versions, ensure that the translation was fully comprehensible, and modify the items, instructions, or format if necessary. Finally, a pilot version of the scale was tested with a small sample of French participants to evaluate the scale’s instructions, response format, and items for clarity. The online eAppendix presents the final French version of the YFAS.
Measures
The Yale Food Addiction Scale
The YFAS is a 25-item, self-report scale designed by Gearhardt et al14 to measure the symptoms of food addiction that have occurred over the past 12 months. The authors developed this scale to identify people exhibiting signs of addiction regarding specific types of foods (for example, high fat and sugar) by extrapolating the DSM-IV-TR criteria for substance dependence to the field of eating behaviours.5 This scale includes mixed response categories (that is, items that are presented in either a dichotomous or Likert-type format). In accordance with the diagnostic criteria for substance dependence, as stated by the DSM-IV-TR,1 this scale assesses the following 7 food addiction criteria14:
tolerance (items 20 and 21);
withdrawal (items 12, 13, and 14);
the substance is often taken in larger amounts or over a longer period than was intended (items 1, 2, and 3);
a persistent desire or unsuccessful effort to cut down or control substance use (items 4, 22, 24, and 25);
spending a great deal of time in activities necessary to obtain the substance, use the substance, or recover from its effects (items 5, 6, and 7);
giving up social, occupational, or recreational activities because of substance use (items 8, 9, 10, and 11); and
continuing substance use with the knowledge that it is causing or exacerbating a persistent or recurrent physical or psychological problem (item 19).
The YFAS has 2 additional items that assess people’s clinically significant impairment or distress caused by eating (items 15 and 16). Items 17, 18, and 23 are primers for other questions and are not scored.
Gearhardt et al14 defined specific cut-offs such that each of the 7 diagnostic criteria was satisfied when 1 or more item representing that criterion was endorsed. The YFAS provides 2 scoring options, which are a symptom count version and a diagnostic version. The symptom count version reflects the number of dependence symptoms experienced in the past 12 months (that is, YFAS symptom count scores range from 0 to 7). In the diagnostic version, food addiction is diagnosed when 3 or more symptoms were present during the past 12 months and clinically significant impairment or distress was endorsed.
This scale has been validated in English, has exhibited adequate internal consistency (Cronbach α = 0.86), and has shown good construct validity with measures of similar constructs and with measures of related but dissimilar constructs.14 Additionally, this scale has been validated in German, with clinical22 and nonclinical samples,23 with similar psychometric properties.
The Binge Eating Scale
The BES is a 16-item scale designed to assess people’s severity of binge eating using behavioural, affective, and cognitive symptoms.24 The BES is a widely used scale to assess binge eating disorder25 and provides an overall score by summing each of the items (each ranging from 0 to 3), with a higher score reflecting more severe binge eating problems. Internal consistency in our sample for this measure was excellent (Cronbach α = 0.92).
The Bulimic Investigatory Test, Edinburgh
The BITE is a 33-item, self-report measure developed by Henderson and Freeman to assess the severity and frequency of binge eating symptoms.26 The severity of people’s binge eating behaviour is assessed according to the symptom score from this scale, which ranges from 0 to 30. According to Henderson and Freeman,26 this scale has satisfactory reliability and validity when used with binge eating patients. Internal consistency in our sample for this measure was excellent (KR-20 internal reliability coefficient was 0.96).
Statistical Analyses and Ethical Considerations
Analyses were conducted using the R statistical package version 2.15.27 with the Psych package.28 Statistical analyses included descriptive statistics and tests examining the psychometric properties of the scale, including its factor structure, the item statistics, internal consistency, and construct validity.
To test the scale’s factor structure, we used the procedure used in Gearhardt’s original publication.14 Therefore, we conducted a factor analysis for dichotomous data based on polychoric correlation coefficients29 to explore the number of underlying factors. The initial factor analysis for the original 22 dichotomous items revealed that 1 item (item 24) did not strongly correlate with the remaining items of the scale, as it had a low factor loading of −0.03. In accordance with Gearhardt and colleagues’ previous research, we excluded this item from the analysis and performed new statistical analyses. We determined the number of factors to extract by examining the scree plot (eigenvalues and by examining Cattell’s scree test30,31), and by conducting Horn’s parallel analysis test.32 Final factor analysis was thus based on the original 21 items that were included in the YFAS (excluding the significance questions), and was conducted using a varimax rotation. We also tested the factor structure of the YFAS in its diagnostic version, by conducting a factor analysis using a varimax rotation for the 8 dichotomous diagnostic criteria (7 diagnostic DSM criteria in addition to significance questions).
We tested the internal consistency of the scale, as in the extent to which the items in a dimension were correlated with each other, using the KR-20 coefficient, given that the items were all dichotomous.33 Construct validity was assessed by examining the associations between the YFAS scores and the measures of binge eating behaviours. First, we described the construct validity of the YFAS symptom count, and then we described that of the diagnostic version. We examined the associations between the YFAS symptom count score and both the BES total score and the BITE symptom score (Spearman rho correlation coefficients). We used nonparametric tests for these analyses, given that we rejected the normality hypothesis for the YFAS symptom scores (a Shapiro–Wilk test was significant). Next, we tested construct validity for the diagnosis version. We used Mann-Whitney U tests to assess the associations between the diagnosis of food addiction and binge eating, as assessed by the BES and the BITE. All analyses were 2-tailed, with P values of less than 0.05 considered statistically significant. There were no missing data, as all of the questions required responses to proceed to the next page of the survey. Our study did not require institutional review board approval because it was not considered biomedical research under French law; however, it followed the tenets of the Declaration of Helsinki.
Results
Sample Characteristics
Participants had a mean age of 28.9 years (SD 12.0 years; 95% CI 27.9 to 29.9 years), a mean current BMI of 22.5 kg/m2 (SD 4.5 kg/m2; 95% CI 22.2 to 22.9 kg/m2). Food addiction was diagnosed in 8.7% of our sample. The median YFAS symptom count (the number of criteria satisfied for food dependence) was 1, and the mean YFAS symptom count score was 1.9 (SD 1.4; 95% CI 1.8 to 2.0). The mean BES total score was 8.2 (SD 8.9; 95% CI 7.4 to 8.9), and the mean BITE symptom score was 7.7 (SD 6.4; 95% CI 7.1 to 8.2).
Item Statistics, Factor Structure, and Reliability
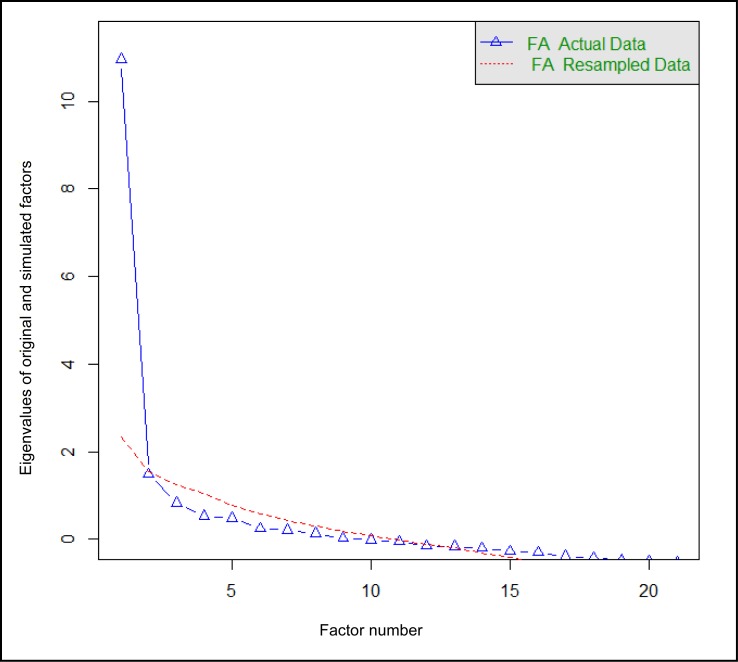
Table 1 summarizes the item statistics, including the mean, standard deviation, and item total correlation for each item. By examining the scree plot in Figure 1, the factor analysis based on the original 21 items identified 2 factors based on their eigenvalues (factor 1: 10.96 and factor 2: 1.48), suggesting a 1- or 2-factor structure. An examination of Cattell’s scree test and a parallel analysis suggested the extraction of 1 factor. Following Cattell’s advice,34 we extracted an extra factor and studied the 1- and 2-factor solutions.
Table 1.
Item statistics for the YFAS
| Criteria and items of the YFAS | Mean (SD) | Item total correlation |
|---|---|---|
| Criterion A: Tolerance | ||
| Item 20 | 0.09 (0.28) | 0.42 |
| Item 21 | 0.19 (0.39) | 0.40 |
| Criterion B: Withdrawal | ||
| Item 12 | 0.02 (0.13) | 0.53 |
| Item 13 | 0.07 (0.25) | 0.52 |
| Item 14 | 0.08 (0.27) | 0.57 |
| Criterion C: Substance often taken in larger amounts or over a longer period than was intended | ||
| Item 1 | 0.09 (0.28) | 0.58 |
| Item 2 | 0.12 (0.32) | 0.51 |
| Item 3 | 0.04 (0.20) | 0.62 |
| Criterion D: Persistent desire or unsuccessful effort to cut down or control substance use | ||
| Item 4 | 0.12 (0.32) | 0.51 |
| Item 22 | 0.59 (0.49) | 0.34 |
| Item 24 | 0.57 (0.50) | −0.02 |
| Item 25 | 0.25 (0.44) | 0.50 |
| Criterion E: Spending a great deal of time in activities necessary to obtain the substances, use the substance, or recover from its effects | ||
| Item 5 | 0.13 (0.33) | 0.48 |
| Item 6 | 0.06 (0.23) | 0.29 |
| Item 7 | 0.05 (0.22) | 0.48 |
| Criterion F: Giving up social, occupational, or recreational activities because of substance use | ||
| Item 8 | 0.05 (0.22) | 0.66 |
| Item 9 | 0.04 (0.19) | 0.72 |
| Item 10 | 0.04 (0.20) | 0.55 |
| Item 11 | 0.04 (0.20) | 0.47 |
| Criterion G: Continuing substance use despite physical or psychological problem | ||
| Item 19 | 0.20 (0.40) | 0.49 |
| Significant distress | ||
| Item 15 | 0.10 (0.30) | 0.68 |
| Item 16 | 0.03 (0.17) | 0.66 |
Figure1.
Scree plot and eigenvalues of the French version of the YFAS
Eigenvalues of tetrachoric and polychoric matrix
FA = factor analysis
A 1-factor structure explained 54.1% of the variance. For this 1-factor structure, all of the factor loadings were greater than 0.57 except for item 6, which had a factor loading of 0.46, and the KR-20 internal reliability coefficient was good (KR-20 = 0.84) for these items (Table 2). An alternative 2-factor structure explained an additional 9.5% of the variance (factor 1 explained 34.3% of variance and factor 2 explained 29.4% of variance). For the 2-factor structure, all of the factor loadings were greater than 0.43 (Table 2), and the KR-20 internal reliability coefficient was good for the first factor (KR-20 = 0.81) and adequate for the second factor (KR-20 = 0.67). In this 2-factor solution, the first factor consisted of items belonging primarily to DSM criteria A, B, C, E, F, and G (Table 2). The second factor consisted of items belonging primarily to DSM criteria D and F, and significant distress (giving up social, occupational, or recreational activities because of substance use), and significant distress (Table 2). Thus our results mainly support a 1-factor structure, which explained 54.1% of the variance.
Table 2.
Factor loadings for the 1- and 2-factor structures of the YFAS factor analysis
| Criteria and items of the YFAS | 1-factor structure
|
2-factor structure
|
|
|---|---|---|---|
| Factor 1 loading | Factor 1 loading | Factor 2 loading | |
| Criterion A: Tolerance | |||
| Item 20 | 0.61 | 0.49a | 0.36 |
| Item 21 | 0.57 | 0.43a | 0.36 |
| Criterion B: Withdrawal | |||
| Item 12 | 0.82 | 0.66a | 0.49 |
| Item 13 | 0.74 | 0.70a | 0.33 |
| Item 14 | 0.78 | 0.72a | 0.36 |
| Criterion C: Substance often taken in larger amounts or over a longer period than was intended | |||
| Item 1 | 0.78 | 0.80a | 0.27 |
| Item 2 | 0.69 | 0.77a | 0.17 |
| Item 3 | 0.85 | 0.77a | 0.41 |
| Criterion D: Persistent desire or unsuccessful effort to cut down or control substance use | |||
| Item 4 | 0.70 | 0.53a | 0.46 |
| Item 22 | 0.58 | 0.18 | 0.66b |
| Item 24c | — | — | — |
| Item 25 | 0.71 | 0.31 | 0.71b |
| Criterion E: Spending a great deal of time in activities necessary to obtain the substances, use the substance, or recover from its effects | |||
| Item 5 | 0.67 | 0.54a | 0.40 |
| Item 6 | 0.46 | 0.76a | −0.16 |
| Item 7 | 0.70 | 0.73a | 0.23 |
| Criterion F: Giving up social, occupational, or recreational activities because of substance use | |||
| Item 8 | 0.87 | 0.65a | 0.57 |
| Item 9 | 0.93 | 0.69a | 0.62 |
| Item 10 | 0.76 | 0.21 | 0.90b |
| Item 11 | 0.64 | — | 0.92b |
| Criterion G: Continuing substance use despite physical or psychological problem | |||
| Item 19 | 0.67 | 0.54a | 0.41 |
| Significant distress | |||
| Item 15 | 0.86 | 0.49 | 0.74b |
| Item 16 | 0.90 | 0.47 | 0.82b |
Items associated with the first factor of the 2-factor structure
Items associated with the second factor of the 2-factor structure
Item 24 was not included in the analysis because of its low factor loading
As for the factor structure of the YFAS in its diagnostic version, a parallel factor analysis, based on the 8 dichotomous diagnostic criteria (7 diagnostic DSM criteria in addition to significance questions), identified a single-factor structure. In this single-factor structure, all of the criteria had factor loadings for the single factor of 0.61 or greater. The KR-20 internal reliability coefficient was 0.76 when considering all of the diagnostic criteria.
Construct Validation
First, we assessed construct validity by examining the correlations between the YFAS symptom count scores and the measures of binge eating behaviours (that is, the BES total and the BITE symptom scores). The YFAS symptom score was significantly correlated with the BITE symptom score (Spearman ρ = 0.59; P < 0.001) and the BES total score (Spearman ρ = 0.58; P < 0.001).
Second, we evaluated the associations between the diagnosis of a food addiction and binge eating scores. The diagnosis of a food addiction was associated with higher binge eating scores, as assessed by the BITE symptom score (20.5 [SD 5.1], compared with 6.5 [SD 5.0]; P < 0.001) and the BES total score (26.0 [SD 10.2], compared with 6.5 [SD 6.6]; P < 0.001).
Discussion
Our study aimed to measure the psychometric properties of a French version of the YFAS and to establish its reliability and construct validity in a nonclinical sample. We demonstrated that this scale had a 1-factorial structure, good internal consistency, and high construct validity with 1 measure of binge eating, both in its diagnostic and symptom count versions.
We found that the previously proposed 1-factor structure for this scale was the best factorial structure and explained a high proportion of the variance for the French version of this scale, which is consistent with Gearhardt et al’s original results.14 This 1-factor structure was obtained after excluding item 24, which assessed the existence of failed attempts to limit the consumption of foods that are high in fat and sugar. This item is categorized within the fourth DSM-IV-TR addiction criterion, known as persistent desire or unsuccessful effort to cut down or control substance use (items 4, 22, 24, and 25). The low factor loadings and high standard deviations for items 22 and 24 have been discussed by Meule et al,22 suggesting that these items do not sufficiently differentiate between people with and without food addictions. These 2 items (22 and 24) refer to the persistent desire to control food that may be experienced by patients with obesity, who binge eat, who are food-addicted, or who are suffering from bulimia nervosa or anorexia nervosa. Therefore, item 24 could be eliminated from the scale or rephrased, given its low psychometric qualities, and replaced by a more specific item for food addiction. Additional items assessing persistent desire or unsuccessful effort to cut down or control food would be necessary to better differentiate between control, owing to food addiction, and control, owing to fear of weight gain, as this latter dimension is frequently evident in patients with anorexia nervosa and a subtype of bulimia nervosa.
We confirmed the adequate reliability of this scale, both in its diagnostic and symptom count versions. The high factor loadings evident in the factor analysis for the dichotomous criteria support the use of the 7 DSM-IV-TR criteria for substance dependence in the fields of eating behaviours and food addiction. Our results support the adequate reliability of the food addiction concept, as assessed by the DSM-IVTR addiction criteria. In our study, we found a prevalence rate for food addiction (8.7%) that was comparable with the rates reported for the United States (11.4%) and Germany (8.8%).14,19 Additionally, the median number of food addiction criteria found in this sample was one, which was comparable with the United States and German versions. These results suggest that the French version of the YFAS has similar psychometric properties to the previously validated American and German versions in nonclinical samples. These results support the use of the YFAS as an interesting tool for assessing food addiction in the overall population.
We demonstrated that the French version of the YFAS has high construct validity with measures of binge eating. This result is consistent with previous research showing a strong association between food addiction and binge eating.35
In addition, our results suggest that a 2-factor structure of the scale slightly improved the explained variance. Interestingly, this 2-factor solution may help differentiate between the following 2 subtypes of patients with food addiction: patients with either high or low insight regarding addiction symptoms. Factor 1 includes the DSM criteria that assess addiction symptoms independent of the patients’ level of insight regarding their addiction (criteria A, B, C, F, and G), whereas factor 2 includes the DSM criteria that assess this level of insight (criteria D and F, and significant distress). The dimension of high or low insight may be important for both clinical practice and research because it implies different therapeutic strategies. Approaches that develop adequate management strategies for patients depending on their level of insight into their addiction may be optimal. Future research should better assess this dimension of insight among patients with food addiction.
Among the potential limitations of our study, we studied the YFAS only in a nonclinical population. Future studies should assess reliability and construct validity of the YFAS in clinical samples, including patients with binge eating disorder, bulimia nervosa, and anorexia nervosa, as well as the test–retest reliability of this scale. Future studies should also assess food addiction using both semistructured interviews and self-administered scales to establish the sensitivity and specificity of the YFAS. To be consistent with recent DSM-5 criteria for food addiction, the YFAS could be updated in the future by adding items that could assess the 4 additional DSM-5 criteria.
Conclusions
In conclusion, we demonstrated that this French version of the YFAS is a psychometrically sound tool that can be used in future food addiction studies to assess patients who experience addiction-related symptoms in their eating behaviours. One future aim is to use this scale with a clinical sample to better understand the psychopathologic and psychiatric factors associated with food addiction. Another interesting future aim is to study people’s insights into their addictions in these populations. A deeper understanding of these issues will provide a crucial preliminary step that will aid in the development of effective psychotherapeutic and psychopharmacological strategies for patients with food addiction.
Acknowledgments
We thank Yacine Raouf Dendane for assistance with data collection. We thank Ashley Gearhardt for the kind permission to translate and use the YFAS and for providing us references that helped us in the validation of this French version. We thank William Revelle for helping us in using the psych statistical package. We thank AJE for editing our manuscript.
The authors declare that they have no potential or perceived conflicts of interest. The authors received no funding for this study.
Abbreviations
- BES
Binge Eating Scale
- BITE
Bulimic Investigatory Test, Edinburgh
- BMI
body mass index
- DSM
Diagnostic and Statistical Manual of Mental Disorders
- KR-20
Kuder–Richardson’s Formula 20
- YFAS
Yale Food Addiction Scale
References
- 1.American Psychiatric Association (APA) Text revision. 4th ed. Washington (DC): APA; 2000. Diagnostic and statistical manual of mental disorders. [Google Scholar]
- 2.Grant JE, Potenza MN, Weinstein A, et al. Introduction to behavioral addictions. Am J Drug Alcohol Abuse. 2010;36(5):233–241. doi: 10.3109/00952990.2010.491884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davis C, Claridge G. The eating disorders as addiction: a psychobiological perspective. Addict Behav. 1998;23(4):463–475. doi: 10.1016/s0306-4603(98)00009-4. [DOI] [PubMed] [Google Scholar]
- 4.Nestler EJ. Is there a common molecular pathway for addiction? Nat Neurosci. 2005;8(11):1445–1449. doi: 10.1038/nn1578. [DOI] [PubMed] [Google Scholar]
- 5.Gearhardt AN, Corbin WR, Brownell KD. Food addiction: an examination of the diagnostic criteria for dependence. J Addict Med. 2009;3(1):1–7. doi: 10.1097/ADM.0b013e318193c993. [DOI] [PubMed] [Google Scholar]
- 6.Corsica JA, Pelchat ML. Food addiction: true or false? Curr Opin Gastroenterol. 2010;26(2):165–169. doi: 10.1097/MOG.0b013e328336528d. [DOI] [PubMed] [Google Scholar]
- 7.Corwin RL, Grigson PS. Symposium overview—food addiction: fact or fiction? J Nutr. 2009;139(3):617–619. doi: 10.3945/jn.108.097691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davis C, Carter JC. Compulsive overeating as an addiction disorder. A review of theory and evidence. Appetite. 2009;53(1):1–8. doi: 10.1016/j.appet.2009.05.018. [DOI] [PubMed] [Google Scholar]
- 9.Gold MS, Graham NA, Cocores JA, et al. Food addiction? J Addict Med. 2009;3(1):42–45. doi: 10.1097/ADM.0b013e318199cd20. [DOI] [PubMed] [Google Scholar]
- 10.Ifland JR, Preuss HG, Marcus MT, et al. Refined food addiction: a classic substance use disorder. Med Hypotheses. 2009;72(5):518–526. doi: 10.1016/j.mehy.2008.11.035. [DOI] [PubMed] [Google Scholar]
- 11.Avena NM, Gold MS. Food and addiction—sugars, fats and hedonic overeating. Addiction. 2011;106(7):1214–1215. doi: 10.1111/j.1360-0443.2011.03373.x. [DOI] [PubMed] [Google Scholar]
- 12.Blumenthal DM, Gold MS. Neurobiology of food addiction. Curr Opin Clin Nutr Metab Care. 2010;13(4):359–365. doi: 10.1097/MCO.0b013e32833ad4d4. [DOI] [PubMed] [Google Scholar]
- 13.Avena NM, Rada P, Hoebel BG. Evidence for sugar addiction: behavioral and neurochemical effects of intermittent, excessive sugar intake. Neurosci Biobehav Rev. 2008;32(1):20–39. doi: 10.1016/j.neubiorev.2007.04.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gearhardt AN, Corbin WR, Brownell KD. Preliminary validation of the Yale Food Addiction Scale. Appetite. 2009;52(2):430–436. doi: 10.1016/j.appet.2008.12.003. [DOI] [PubMed] [Google Scholar]
- 15.Davis C, Curtis C, Levitan RD, et al. Evidence that ‘food addiction’ is a valid phenotype of obesity. Appetite. 2011;57(3):711–717. doi: 10.1016/j.appet.2011.08.017. [DOI] [PubMed] [Google Scholar]
- 16.Gearhardt AN, White MA, Masheb RM, et al. An examination of food addiction in a racially diverse sample of obese patients with binge eating disorder in primary care settings. Compr Psychiatry. 2013;54(5):500–505. doi: 10.1016/j.comppsych.2012.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gearhardt AN, White MA, Masheb RM, et al. An examination of the food addiction construct in obese patients with binge eating disorder. Int J Eat Disord. 2012;45(5):657–663. doi: 10.1002/eat.20957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gearhardt AN, Yokum S, Orr PT, et al. Neural correlates of food addiction. Arch Gen Psychiatry. 2011;68(8):808–816. doi: 10.1001/archgenpsychiatry.2011.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meule A. How prevalent is food addiction? Front Psychiatry. 2011;2(61):1–4. doi: 10.3389/fpsyt.2011.00061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Le Sphinx Mise en place d’une enquête avec Sphinx, support d’utilisation, service formations [Internet] Annecy (FR): Le Sphinx Développement; 2010 [cited 2013 Aug 30]. Available from: http://www.lesphinx.eu.
- 21.Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol. 1993;46(12):1417–1432. doi: 10.1016/0895-4356(93)90142-n. [DOI] [PubMed] [Google Scholar]
- 22.Meule A, Heckel D, Kübler A. Factor structure and item analysis of the Yale Food Addiction Scale in obese candidates for bariatric surgery. Eur Eat Disord Rev. 2012;20(5):419–422. doi: 10.1002/erv.2189. [DOI] [PubMed] [Google Scholar]
- 23.Meule A, Vögele C, Kübler A. German translation and validation of the Yale Food Addiction Scale. Diagnostica. 2012;58(3):115–126. [Google Scholar]
- 24.Gormally J, Black S, Daston S, et al. The assessment of binge eating severity among obese persons. Addict Behav. 1982;7(1):47–55. doi: 10.1016/0306-4603(82)90024-7. [DOI] [PubMed] [Google Scholar]
- 25.Wilfley DE, Wilson GT, Agras WS. The clinical significance of binge eating disorder. Int J Eat Disord. 2003;34(S1):S96–S106. doi: 10.1002/eat.10209. [DOI] [PubMed] [Google Scholar]
- 26.Henderson M, Freeman CP. A self-rating scale for bulimia. The ‘BITE.’. Br J Psychiatry. 1987;150(1):18–24. doi: 10.1192/bjp.150.1.18. [DOI] [PubMed] [Google Scholar]
- 27.R Development Core Team R: a language and environment for statistical computing [Internet] Vienna (AU): R Foundation for Statistical Computing 2013 [cited 2013 Aug 30]. Available from: http://www.R-project.org.
- 28.Revelle W. Psych: procedures for personality and psychological research Version 1310 [Internet] Evanston (IL): Northwestern University; 2013. [cited 2013 Aug 30]. Available from: http://CRAN.R-project.org/package=psych. [Google Scholar]
- 29.Kubinger KD. On artificial results due to using factor analysis for dichotomous variables. Psychol Sci. 2003;45(1):106–110. [Google Scholar]
- 30.Cattell RB. The scree test for the number of factors. Multivariate Behav Res. 1966;1(2):245–276. doi: 10.1207/s15327906mbr0102_10. [DOI] [PubMed] [Google Scholar]
- 31.Jolliffe IT. Principal component analysis. New York (NY): Springer; 2005. [Google Scholar]
- 32.Horn JL. A rationale and test for the number of factors in factor analysis. Psychometrika. 1965;30(2):179–185. doi: 10.1007/BF02289447. [DOI] [PubMed] [Google Scholar]
- 33.Kuder GF, Richardson MW. The theory of the estimation of test reliability. Psychometrika. 1937;2(3):151–160. [Google Scholar]
- 34.Gorsuch RL. Factor analysis. 2nd ed. London (GB): Psychology Press; 2008. [Google Scholar]
- 35.Gearhardt AN, White MA, Potenza MN. Binge eating disorder and food addiction. Curr Drug Abuse Rev. 2011;4(3):201–207. doi: 10.2174/1874473711104030201. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.