Abstract
Objective:
To investigate the cost-effectiveness of a rapid response team (RRT), compared with usual care (UC), for treating suicidal adolescents.
Methods:
Suicidal adolescents (n = 286) presenting at an emergency department were enrolled in a trial to compare UC with enhanced outpatient care provided by an RRT of health professionals. Functioning (Child Global Assessment Scale) and suicidality (Spectrum of Suicidal Behavior Scale) scores were measured at baseline and 6 months later. Resource use and cost data were collected from several sources during the same period.
Results:
As previously reported, there was no statistically or clinically significant difference in either functioning or suicidality between the groups. Costs of the RRT were lower by $1886, thus –$1886 (95% CI –$4238 to $466), from the perspective of the treating hospital, and by $991, thus –$991 (95% CI –$5580 to $3598), from the perspective of society. If decision makers are not willing to pay for any improvement in functioning or suicidality, the RRT has a 95% probability of being cost-effective from the perspective of the treating hospital. From the point of view of society, the probability of the intervention being cost-effective is about 70% for functioning and 63% for suicidality. The difference between the 2 perspectives is mainly attributable to the cost of hospitalizations outside the treating hospital.
Conclusions:
An RRT intervention appears to be cost-effective, compared with UC, from the point of view of the treating hospital, but there is no difference from the point of view of society.
Keywords: suicide, adolescent, costs and cost analysis, cost-effectiveness analysis, rapid reponse teams
Abstract
Objectif :
Étudier la rentabilité d’une équipe d’intervention rapide (EIR), comparativement aux soins usuels (SU), pour traiter des adolescents suicidaires.
Méthodes :
Des adolescents suicidaires (n = 286) qui se sont présentés à un service d’urgence ont été inscrits dans un essai pour comparer les SU avec des soins ambulatoires améliorés fournis par une EIR de professionnels de la santé. Les scores de fonctionnement (échelle d’évaluation globale pour enfants) et de suicidabilité (échelle du spectre du comportement suicidaire) ont été mesurés au départ et au suivi de 6 mois. Les données sur l’utilisation des ressources et les coûts ont été recueillies auprès de plusieurs sources durant la même période.
Résultats :
Comme il a été précédemment constaté, il n’y avait pas de différence statistiquement ou cliniquement significative de fonctionnement ou de suicidabilité entre les groupes. Les coûts de l’EIR étaient inférieurs de 1886 $, donc −1886 $ (IC à 95 % −4238 $ à 466 $), du point de vue de l’hôpital traitant, et de 991 $, donc −991 $ (IC à 95 % −5580 $ à 3598 $), du point de vue de la société. Si les décideurs ne sont pas disposés à payer pour toute amélioration du fonctionnement ou de la suicidabilité, l’EIR a une probabilité de 95 % d’être rentable du point de vue de l’hôpital traitant. Du point de vue de la société, la probabilité que l’intervention soit rentable est d’environ 70 % pour le fonctionnement et de 63 % pour la suicidabilité. La différence entre les 2 points de vue est principalement attribuable au coût des hospitalisations hors de l’hôpital traitant.
Conclusions :
Une intervention d’EIR semble être rentable, comparé aux SU, du point de vue de l’hôpital traitant, mais il n’y a pas de différence du point de vue de la société.
Youth suicide is a public health concern of growing importance.1–3 Worldwide, suicide remains the second leading cause of death among children ages 10 to 19.4,5 In Canada, about 3500 people die by suicide every year, among whom 450 are children and young adults between 10 and 24 years old.3 A much larger number contemplate or attempt suicide.6,7 Following a suicide attempt, many suicidal youth are admitted to the ED for assessment and treatment. Hospitalization may follow in some cases, but recent concerns about the costs and effectiveness of psychiatric hospitalization have led to a greater emphasis on outpatient treatment care.8 Several studies suggest that psychosocial interventions are at least as effective as inpatient care for treatment of young suicide attempters.9–16 In our own trial (see Greenfield et al13), we assigned 286 suicidal adolescents admitted to the ED either to an RRT outpatient follow-up or to UC. Both groups achieved similar improvements in function and suicidality levels, but those assigned to the RRT appeared to have a significantly lower 6-month hospitalization rate. Several reviews agree that more evidence to support one type of intervention over another for youth suicide is needed.17–22
The interest in outpatient treatment alternatives lies not only in improving patient outcome but also in the potential for cost savings. Health care costs associated with inpatient care of youth suicidal behaviour can be substantial.23 Among 4 studies that examined the costs of treatment alternatives to hospitalization for youth in psychiatric crisis,12,23–25 only 2 investigated the cost-effectiveness of community treatment for suicidal youth, but 1 focused exclusively on children who intentionally poisoned themselves,24 and the other focused on self-harm with and without suicidal intent.25
Using data collected alongside a clinical trial,13 the objective of our study was to report on the cost-effectiveness of an RRT, compared with UC, for treating adolescents presenting for suicide attempt at an ED. Analyses were conducted from the points of view of the treating hospital and of society. The hospital perspective includes only the use and cost of resources that are covered by the treating hospital, while the broader societal perspective further includes the use and cost of resources outside the treating hospital, such as visits to other hospitals, as well resources not paid by the health care system, such as out-of-pocket health care expenditures.
Methods
Trial Design
Our trial was conducted in an ED of a large pediatric hospital that serves the youth population in the greater Montreal area, in Quebec. Details of the trial have been described elsewhere.13 Briefly, the study enrolled 286 suicidal adolescents, aged 12 to 17 years, presenting at the ED between 1996 and 1998, and consenting to participate in the study. Patients were assigned to an intervention arm, depending on the group assignment of the psychiatrist who treated them at the ED. Immediately after the psychiatric assessment in the ED, a research assistant administered a battery of semi-structured interviews with the adolescent alone and then separately with one parent. The psychiatrist then either admitted or discharged the patient, with subsequent referral to the experimental condition or control condition. All patients were contacted for a follow-up interview 2 and 6 months after the ED assessment. Approval for the study was obtained from the institutional review board of the Montreal Children’s Hospital.
Interventions
Experimental Group
The RRT included one psychiatrist, one psychiatric nurse, and other health professionals (for example, a social worker, an educational specialist, or an art therapist), the number and nature of which varied over time. The psychiatrist or nurse contacted the patient within 24 hours of the ED visit, and a meeting was scheduled for within 72 hours of the ED visit. Patient and family members were assessed and appropriate treatment was initiated (pharmacological, behavioural, cognitive, and [or] psychodynamic). Patients were also referred to outpatient care and community resources (for example, a family doctor or a school psychologist).
Clinical Implications
An RRT intervention for suicidal adolescents is more cost-effective than UC from the perspective of the treating hospital.
From the point of view of society, owing to some parents seeking hospitalization for their child at other hospitals, the costs using the RRT were equivalent to those with UC.
Limitations
Our study follow-up was limited to 6 months.
Some patients chose to seek additional care outside the treating hospital, which could have biased estimation of effectiveness.
Control Group
Psychiatrists delivering UC could hospitalize the patient, follow the patient as an outpatient, or refer the patient to a hospital-based outpatient psychiatric clinic, a nonhospital-based community health program, a private mental health worker, or other UC health services.
Regardless of group assignment, patients could be hospitalized at any time subsequent to the initial ED visit. However, the intent was that rapid access to outpatient care would significantly reduce the need for hospitalization.
Health Outcomes
Outcome measures were the difference in functionality and suicidality scores between baseline and 6-month follow-up. The CGAS26 measures the patient’s level of functioning. A higher score (maximum 100) indicates better functioning. The SSBS27 measures the severity of suicidal behaviour on a 5-point ordinal scale, from no suicidal behaviour to serious suicide attempts. Additional sociodemographic information was obtained from interviews.
Resource Use
The economic evaluation was carried out from the perspectives of the treating hospital and of society. We relied on several data sources: charts from the treating hospital (including records from the RRT), which yielded detailed information on all in- and outpatient services used at that hospital; government administrative data, from which we obtained data on all hospitalizations in the province, physician services (which are billed to the provincial government), and, for publicly insured patients, medications; and, patient questionnaires. Patient questionnaires, administered at baseline, and at 2 and 6 months, provided information on use of medications for patients not covered by the public plan, use of specialized education and youth protection services (including stays at residential facilities), psychologist and other mental health and social service professionals outside the hospital, and parent and patient time.
Costs
Costs of services used were obtained by multiplying frequencies that services were used during the 6-month period (for example, the number of days hospitalized) by a cost per day or per visit. As no standardized source for these exists in Quebec (or in the rest of Canada), they had to be calculated individually. Unit costs were collected for the 1998/99 fiscal year, during which the trial was conducted, and subsequently transformed to 2011 dollars using the Canadian Consumer Price Index, for Health and Personal Care commodities and services, for the province of Quebec.28
Relevant costs from the hospital viewpoint included those of the experimental and control interventions, ED visits, inpatient stays at the treating hospital, as well as outpatient visits and drugs supplied by the hospital. Physician fees were not considered under this perspective because physicians are paid by the Quebec provincial government and are not covered under a hospital’s budget. Hospital service costs (ED visits, outpatient visits, inpatient stays, and RRT) were based on financial and activity reports of the hospitals, supplemented by information from hospital financial officers and data supplied by the trial research team, and estimated using standard methods.29 Fees paid to physicians were available for all study patients and obtained from the Quebec Health Insurance Board. Unit costs of drugs were also obtained from the Quebec Health Insurance Board. Costs of private visits with a psychiatrist or other health care professionals were obtained from professional boards.
Statistical Analysis
All analyses used an intention-to-treat approach. Given the short time frame of the study, the costs and outcomes were not discounted. ICERs of the outcomes (that is, CGAS and SSBS) were estimated from each perspective. Confidence intervals were calculated using the bootstrap method with 5000 iterations.29 CEACs were then plotted. A CEAC shows the probability that the RRT intervention is more cost-effective than UC (that the net monetary benefit is positive) for different maximum amounts of WTP per unit of improvement (on the CGAS or SSBS scale). In the context of decision making, a CEAC illustrates the trade-off between uncertainty, as to whether an intervention is cost-effective relative to a comparator, and WTP.30 CEACs can be traced by calculating the proportion of points on the cost-effectiveness plane, which are below and to the right of a line that pivots from being horizontal, or superposed on the x axis, to vertical, or superposed on the y axis. Points below the x axis indicate cost-effectiveness if the decision maker is not willing to pay for any improvement in outcome, while points to the right of the y axis indicate cost-effectiveness if the decision maker is willing to pay any amount for any improvement in outcome.
We then used net benefit regression31 to investigate variation in cost-effectiveness by sex, because sex differences in suicidality are known to exist.6 Net benefit regression provides a simple method for exploring subgroup heterogeneity by allowing the inclusion of interaction terms directly in a regression analysis.32–34 We included the following variables in our model: assigned treatment group, sex, and an interaction term between treatment group and sex.
Finally, because of uncertainty in some unit costs (meetings with resident psychiatrists and participation in the Adolescent Treatment Program), we performed several sensitivity analyses of the ICER, using a 50% variation in costs. In preliminary analyses, we found 2 participants in the control group who were outliers in length of hospitalization (more than 19 standard deviations above the mean). We reran analyses excluding these participants. All analyses were performed in STATA (release 9.0, College Station, TX).
Results
Participants
A total of 158 patients were assigned to the experimental group and 128 to the control group.13 About one-third of participants were males. Other sociodemographic and clinical characteristics of participants have been described elsewhere.13 No significant differences in any of these variables were found between the groups at baseline. Suicidal ideation and type of suicide attempt were also comparable between groups, except use of drug overdose as a method of suicide attempt, which was more prevalent in control subjects (10% in the experimental group and 23% in the control group, P = 0.004)
Outcomes
As previously reported, there were no clinically or statistically significant differences in clinical outcomes between the groups at 6-month follow-up.13
Resource Use
Resource use was similar between the 2 groups (Table 1), with the exception that those from the control group were, on average, hospitalized more often at the treating hospital, spent more time being hospitalized, and had more meetings with outpatient psychotherapists and social workers than those from the experimental group. The overall hospitalization rate at the treating hospital was significantly higher in the control group (43%), compared with the experimental group (18%) (P < 0.001). However, when including hospitalizations in nearby hospitals, the average number of hospitalized days was comparable between groups (5.4 days and 5.5 days in the experimental and control groups, respectively; P = 0.97)
Table 1.
Use of resources during the 6-month follow-up
| Experimental group | Control group | Significant differencea | |
|---|---|---|---|
| Variable | Mean (SD) | Mean (SD) | P |
| Inpatient services, n | |||
| Hospital admissions | 0.22 (0.51) | 0.48 (0.63) | <0.001 |
| All hospitalizations, hours | 33.42 (122.49) | 95.98 (378.58) | <0.05 |
| Sitter during all hospitalizations, hours | 14.81 (48.22) | 20.85 (48.06) | ns |
| Psychologist visits | 0.03 (0.22) | 0.03 (0.27) | ns |
| Meetings with psychiatrists | 0.58 (1.14) | 0.68 (1.17) | ns |
| Drop-in visits by psychiatrists | 0.12 (0.47) | 0.26 (0.65) | ns |
| Outpatient services, n | |||
| Meeting with psychotherapist | 0.06 (0.47) | 0.44 (1.60) | <0.01 |
| Meeting with psychiatrist | 0.69 (2.97) | 0.67 (2.54) | ns |
| Meetings with treating hospital’s social worker | 0.13 (0.60) | 0.57 (1.91) | <0.01 |
| Meetings with clinical nurse specialist | 0.43 (1.05) | 0.63 (1.82) | ns |
| Attendance to day ATP | 0.49 (4.35) | 0 | ns |
| Attendance to evening ATP | 0.07 (0.68) | 0.09 (1.06) | ns |
| Meetings with education coordinator | 0.04 (0.23) | 0.08 (0.50) | ns |
| Meetings with occupational therapist | 0.12 (1.08) | 0.19 (1.49) | ns |
| Other resources, n | |||
| Meetings with others | 0.86 (4.18) | 1.24 (4.22) | ns |
| Meetings with school counsellor | 1.84 (6.79) | 4.05 (12.90) | ns |
| Meetings with other community-based therapists | 0.61 (2.66) | 1.06 (3.69) | ns |
| Meetings with youth protection agency | 2.25 (6.64) | 2.02 (9.36) | ns |
| Using specialized accommodation, days | 9.1 (37.9) | 7.7 (35.0) | ns |
| Time, minutes | |||
| Parental time for therapy and hospital visits | 1786 (5559) | 1823 (6292) | ns |
| Child time to and from therapy | 58 (69) | 50 (74) | ns |
ATP = Adolescent Treatment Program; ns = nonsignificant
From Student t test
Costs
Table 2 describes some of the costs incurred during the 6 months of follow-up. From the treating hospital’s perspective, the average cost per person of the experimental group was $2114 (range: $134 to $46 273), compared with $4000 (range: $150 to $127 998) per person for the control group, a statistically nonsignificant difference of $1886 (P = 0.11). From the societal perspective, the average cost per person of the experimental group was $10 785 (range: $1424 to $107 406) and that of the control group, $11 775 (range: $559 to $164 134), a statistically nonsignificant difference of $991 (P = 0.67).
Table 2.
Selected costs per participant during the 6-month follow-up period (in 2011 Can$)
| Experimental group | Control group | Significant differencea | |
|---|---|---|---|
| Variable | Mean (SD) | Mean (SD) | P |
| Intervention | |||
| RRT intervention (excluding psychiatrist from RRT) | 118 (0.80) | 0 | <0.001 |
| Psychiatrist from RRT | 772 (1.09) | 0 | <0.001 |
| Inpatient services | |||
| Hospitalization at treating hospital | 931 (282.60) | 2496 (942) | ns |
| All hospitalizations | 2562 (761.25) | 3000 (1014) | ns |
| Meetings with psychiatrists (excluding psychiatristfrom RRT) | 68 (10.5) | 78 (12) | ns |
| Outpatient services | |||
| Meeting with psychiatrist | 97 (418) | 95 (357) | ns |
ns = nonsignificant; RRT = rapid recovery team
From Student t test
Cost-Effectiveness Analysis
Incremental Cost-Effectiveness Ratios
Table 3 shows the ICER calculations for each outcome and each perspective. The confidence intervals were wide for all ICERs. The point estimates indicate that the experimental intervention would save the treating hospital about $1208, and society about $636, for every additional point improvement on the functional scale (the CGAS), compared with the control intervention. Conversely, the control intervention would save the hospital about $13 780, and society about $7238, for every additional point improvement on the suicide severity scale (the SSBS), compared with the experimental intervention.
Table 3.
ICER and 95% CIs from the treating hospital’s and society’s perspective
| Variable | Functionality (CGAS) Mean estimate (95% CI)a | Suicidality (SSBS) Mean estimate (95% CI)a |
|---|---|---|
| Treating hospital | ||
| Cost differences, $ | −1886 (–4238 to 466) | −1886 (–4238 to 466) |
| Outcome differences, points | 1.56 (–2.22 to 5.42) | −0.14 (–0.43 to 0.15) |
| ICER, $/point | −1218 (–10 633 to 10 266) | 13 780 (–157 874 to 139 950) |
| Society | ||
| Cost differences | −991 (–5580 to 3598) | −991 (–5580 to 3598) |
| Outcome differences | 1.56 (–2.22 to 5.42) | −0.14 (–0.43 to 0.15) |
| ICERb | −636 (–13 607 to 12 127) | 7238 (–129 686 to 171 298) |
Confidence intervals were estimated using the bootstrap method.
ICERs were calculated by dividing the mean cost differences by the mean outcome differences.
CGAS = Children’s Global Assessment Scale; ICER = incremental cost-effectiveness ratio; SSBS = Spectrum of Suicidal Behavior Scale
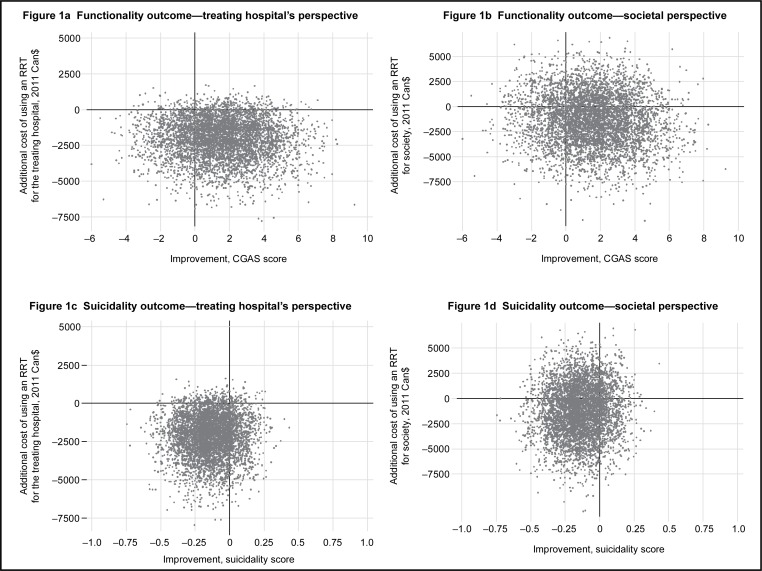
Cost-Effectiveness Planes
Figure 1 illustrates the cost-effectiveness planes using the 5000 bootstrapped replications. From the treating hospital’s perspective, and using the CGAS as the outcome (Figure 1a), most of the points are in the lower-right quadrant, indicating that the experimental treatment is more effective for improving function and less costly than the control intervention; from a societal perspective (Figure 1b), as outcomes are unchanged, the points mostly rise so that the experimental intervention now does not seem either more or less costly than UC. For suicide severity (Figures 1c and 1d), the points are on the left side of the quadrant, reflecting the lower effectiveness of the experimental treatment in improving suicidality than that of the control treatment. From the hospital’s viewpoint, the experimental intervention is also less costly, but from a societal viewpoint, it is about as costly as the control intervention.
Figure 1.
Cost-effectiveness planes of RRT intervention compared to control intervention for functionality and suicidality outcomes from the perspectives of the treating hospital and society (5000 bootstrapped replications)
CGAS = Children’s Global Assessment Scale; RRT = rapid response team
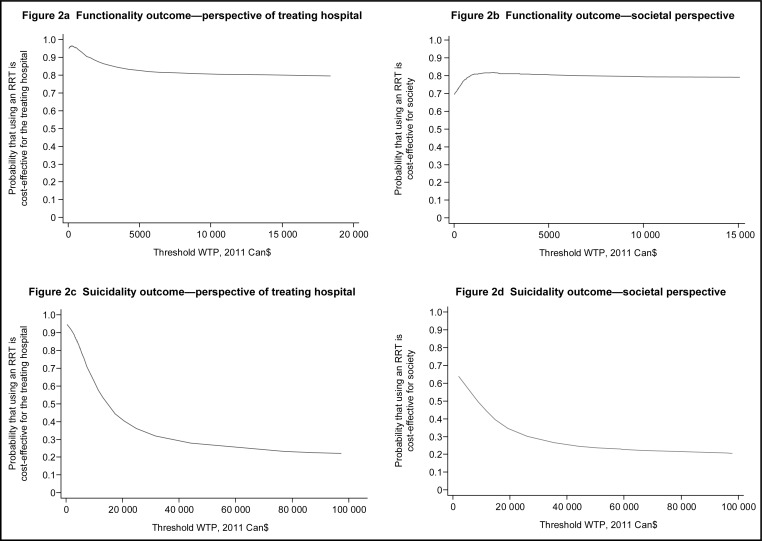
Cost-Effectiveness Acceptability Curves
The CEACs are illustrated in Figure 2 and show the probability that the experimental intervention is more cost-effective than the control intervention, given a WTP of between $0 and $20 000 for a 1-point increase in functionality score (Figures 2a and 2c), and between $0 and $100 000 for a 1-point decrease in suicidality score (Figures 2b and 2d). For functionality scores, the probability that the experimental intervention is more cost-effective is higher at a WTP of less than $5000 for the treating hospital, and at a WTP of more than $1000 for society. For suicidality scores, the probability that the experimental intervention is more cost-effective is highest when the WTP is zero, for both the treating hospital and society.
Figure 2.
Cost-effectiveness acceptability curves for RRT intervention compared to control intervention for functionality and suicidality outcomes from the perspectives of the treating hospital and society
RRT = rapid response team; WTP = willingness to pay
Net Benefit Regression
Results of the net benefit regression models (not shown) indicate that sex did not have a statistically significant impact on any of the cost-effectiveness estimates.
Sensitivity Analysis
Two-way sensitivity analyses of the ICER, varying unit costs for the Adolescent Treatment Program, and meetings with psychiatry residents up or down by 50%, did not significantly alter our results. The exclusion of 2 outliers in hospitalization length from the control group resulted in statistically nonsignificant cost savings of the intervention from the hospital perspective (–$273, P = 0.64) but not from the societal perspective ($951, P = 0.63)
Discussion
The objective of our study was to assess the cost-effectiveness of an RRT intervention, compared with UC, for the treatment of adolescents presenting in an ED for a suicide attempt. We estimated costs from the point of view of the treating hospital and of society. Overall, we found that the RRT was cost-effective from the point of view of the treating hospital, but that there is no difference in costs, or cost-effectiveness, from the point of view of society.
Point estimates indicate that the RRT cost less than UC: $1886 less per patient for the treating hospital, and $991 less for society. This difference between the 2 perspectives was mainly attributable to the costs of hospitalizations outside the treating hospital. Because patients have access to all hospitals under the Canadian health care system, it is possible that these results reflect the decision of parents to seek care outside the treating hospital if their child was randomized to the experimental group and they felt their child needed to be hospitalized.
Analysis of sampling uncertainty suggests that the intervention is cost-effective from the point of view of the treating hospital, but that the intervention and UC are about equally cost-effective from the point of view of society. The near-null difference in suicidality results in an ICER, with a very wide confidence interval, as reflected in the large proportion of points near zero on the x-axis, on the cost-effectiveness planes. It is reasonable for a decision maker to be indifferent to the small, clinically nonsignificant differences in suicidality score that were observed. In this case, the intervention is likely to be cost-effective from the viewpoint of the treating hospital—it is cost-saving, as reflected in most of the points on the cost-effectiveness plane being below the x-axis, and in the high probability of cost-effectiveness at zero on the CEAC. In the case of the CGAS, the intervention appears to have a high probability of being cost-effective, regardless of the perspective and the decision maker’s WTP. However, as it is reasonable for the decision maker to be indifferent to the small, clinically nonsignificant differences in suicidality scores, it is also reasonable to be indifferent to the small, clinically nonsignificant differences in functioning scores. Given the nonsignificant difference in costs from the societal perspective (reflected in the points, which are divided almost equally between the top and bottom halves of the cost-effectiveness planes for the societal perspectives), one can then conclude that the intervention is cost-effective from the point of view of the treating hospital, but that there is no difference in cost-effectiveness from the perspective of society.
Results are not entirely comparable to those of previous economic evaluations of outpatient treatments for suicidal youth,24,25 which focused on the addition of an outpatient service to UC, and targeted specific youth populations different from our own. Green et al25 found that the addition of group psychotherapy to UC was not cost-effective in a sample of adolescents presenting with more than one episode of self-harm. Similar to our study, the authors reported comparable health improvements between treatment groups on suicidality and social functioning, but costs for society were slightly higher for the intervention group, compared with the control group. Byford et al24 observed similar results for a home-based social work intervention, compared with UC alone, in children who intentionally poisoned themselves. The authors found no significant differences in costs or in any of the main health outcomes, including suicidality and mood. Similar to our findings, several studies on psychosocial treatment in suicidal children have reported little to no differences in suicidal behaviours and functional outcomes, compared with UC.9,10,12,16,18,24,25
Our study had some limitations. The study follow-up was limited to 6 months. A longer follow-up time could have yielded larger differences in outcomes, although prior work in this population suggests that such differences are most salient in the short term.13 The study was an open pragmatic randomized trial. We found some patients chose to seek additional care outside the treating hospital, which may have biased estimation of effectiveness. Our analysis, from a societal perspective, did not consider any possible effects of the intervention on parental participation in the labour force, although the parental time involvement is quite similar between the 2 interventions, and clinical effectiveness essentially the same, suggesting that any such effect would be minimal. Finally, the data we used are several years old. However, the question posed in the initial study remains relevant, and there is no reason to believe that the cost offsets revealed in the data would be materially different if the study were conducted today.
This is one of the few studies to assess the cost-effectiveness of outpatient treatments in suicidal youth, and the first to specifically investigate an RRT intervention in a sample of adolescents who attempted suicide. We conducted a detailed assessment of resource use and costs from the perspectives of both the treating hospital and of society, and analyzed the data using state-of-the-art, cost-effectiveness analysis methods.
Conclusions
An RRT intervention appears to be a cost-effective approach for treatment of suicidal youth, compared with UC, from the point of view of the treating hospital. There is essentially no statistical difference in cost-effectiveness between the 2 approaches from the point of view of society. Better addressing the concerns of parents who receive the services of the RRT, so that they are less likely to seek hospitalization for their child elsewhere, may render the intervention cost-effective from a societal perspective.
Acknowledgments
The authors thank Helen Cunningham, MD, for assistance with data collection; and Patti Dray, MA, and Aline Drapeau, PhD, for coordinating the assessments. Funding from the National Health Research Development Program (grant 6605–4656–011) and the Hogg Family Foundation is gratefully acknowledged.
Abbreviations
- CEAC
cost-effectiveness acceptability curve
- CGAS
Children’s Global Assessment Scale
- ED
emergency department
- ICER
incremental cost-effectiveness ratio
- RRT
rapid response team
- SSBS
Spectrum of Suicidal Behavior Scale
- UC
usual care
- WTP
willingness to pay
References
- 1.Bridge JA, Greenhouse JB, Weldon AH, et al. Suicide trends among youths aged 10 to 19 years in the United States, 1996–2005. JAMA. 2008;300(9):1025–1026. doi: 10.1001/jama.300.9.1025. [DOI] [PubMed] [Google Scholar]
- 2.Kidder K, Stein J, Fraser J. The health of Canada’s children: a CICH profile. In: Canadian Institute of Child Health (CICH), editor. The health of Canada’s children: a CICH profile. Ottawa (ON): CICH; 2000. [Google Scholar]
- 3.Statistics Canada . Mortality, summary list of causes. Ottawa (ON): Statistics Canada; 2010. [Google Scholar]
- 4.World Health Organization (WHO) Suicide prevention [Internet] Geneva (CH): WHO; 2006. [cited 2010 Dec 1] Available from: http://www.who.int/mental_health/prevention/suicide/suicideprevent/en. [Google Scholar]
- 5.Statistics Canada . Leading causes of death in Canada: analysis. Ottawa (ON): Statistics Canada; 2009. [Google Scholar]
- 6.Centers for Disease Control and Prevention Youth risk behavior surveillance, United States 2009. MMWR Morb Mortal Wkly Rep. 2009;59(Suppl 5):2–36. [Google Scholar]
- 7.Safer DJ. Self-reported suicide attempts by adolescents. Ann Clin Psychiatry. 1997;9(4):263–269. doi: 10.1023/a:1022364629060. [DOI] [PubMed] [Google Scholar]
- 8.Leslie DL, Rosenheck R. Shifting to outpatient care? Mental health care use and cost under private insurance. Am J Psychiatry. 1999;156(8):1250–1257. doi: 10.1176/ajp.156.8.1250. [DOI] [PubMed] [Google Scholar]
- 9.King CA, Klaus N, Kramer A, et al. The Youth-Nominated Support Team-Version II for suicidal adolescents: a randomized controlled intervention trial. J Consult Clin Psychol. 2009;77(5):880–893. doi: 10.1037/a0016552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Donaldson D, Spirito A, Esposito-Smythers C. Treatment for adolescents following a suicide sttempt: results of a pilot trial. J Am Acad Child Adolesc Psychiatry. 2005;44(2):113–120. doi: 10.1097/00004583-200502000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Huey SJ, Henggeler SW, Rowland MD, et al. Multisystemic therapy effects on attempted suicide by youths presenting psychiatric emergencies. J Am Acad Child Adolesc Psychiatry. 2004;43(2):183–190. doi: 10.1097/00004583-200402000-00014. [DOI] [PubMed] [Google Scholar]
- 12.Blumberg SH. Crisis intervention program: an alternative to inpatient psychiatric treatment for children. Ment Health Serv Res. 2002;4(1):1–6. doi: 10.1023/a:1014071507949. [DOI] [PubMed] [Google Scholar]
- 13.Greenfield B, Larson C, Hechtman L, et al. A rapid-response outpatient model for reducing hospitalization rates among suicidal adolescents. Psychiatr Serv. 2002;53(12):1574–1579. doi: 10.1176/appi.ps.53.12.1574. [DOI] [PubMed] [Google Scholar]
- 14.Wood A, Trainor G, Rothwell J, et al. Randomized trial of group therapy for repeated deliberate self-harm in adolescents. J Am Acad Child Adolesc Psychiatry. 2001;40(11):1246–1253. doi: 10.1097/00004583-200111000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Rotheram-Borus MJ, Piacentini J, Cantwell C, et al. The 18-month impact of an emergency room intervention for adolescent female suicide attempters. J Consult Clin Psychol. 2000;68(6):1081–1093. doi: 10.1037//0022-006x.68.6.1081. [DOI] [PubMed] [Google Scholar]
- 16.Harrington R, Kerfoot M, Dyer E, et al. Randomized trial of a home-based family intervention for children who have deliberately poisoned themselves. J Am Acad Child Adolesc Psychiatry. 1998;37(5):512–518. [PubMed] [Google Scholar]
- 17.Lamb CE. Alternatives to admission for children and adolescents: providing intensive mental healthcare services at home and in communities: what works? Curr Opin Psychiatry. 2009;22(4):345–350. doi: 10.1097/YCO.0b013e32832c9082. [DOI] [PubMed] [Google Scholar]
- 18.Daniel SS, Goldston DB. Interventions for suicidal youth: a review of the literature and developmental considerations. Suicide Life Threat Behav. 2009;39(3):252–268. doi: 10.1521/suli.2009.39.3.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Macgowan MJ. Psychosocial treatment of youth suicide: a systematic review of the research. Res Soc Work Pract. 2004;14(03):147–162. [Google Scholar]
- 20.Steele MM, Doey T. Suicidal behaviour in children and adolescents. Part 2: treatment and prevention. Can J Psychiatry. 2007;52(6 Suppl 1):35S–45S. [PubMed] [Google Scholar]
- 21.Burns J, Dudley M, Hazell P, et al. Clinical management of deliberate self-harm in young people: the need for evidence-based approaches to reduce repetition. Aust N Z J Psychiatry. 2005;39(3):121–128. doi: 10.1080/j.1440-1614.2005.01532.x. [DOI] [PubMed] [Google Scholar]
- 22.Shepperd S, Doll H, Gowers S, et al. Alternatives to inpatient mental health care for children and young people. Cochrane Database Syst Rev. 2009;(2):CD006410. doi: 10.1002/14651858.CD006410.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sheidow AJ, Bradford WD, Henggeler SW, et al. Treatment costs for youths receiving multisystemic therapy or hospitalization after a psychiatric crisis. Psychiatr Serv. 2004;55(5):548–554. doi: 10.1176/appi.ps.55.5.548. [DOI] [PubMed] [Google Scholar]
- 24.Byford S, Harrington R, Torgerson D, et al. Cost-effectiveness analysis of a home-based social work intervention for children and adolescents who have deliberately poisoned themselves. Results of a randomised controlled trial. Br J Psychiatry. 1999;174:56–62. doi: 10.1192/bjp.174.1.56. [DOI] [PubMed] [Google Scholar]
- 25.Green JM, Wood AJ, Kerfoot MJ, et al. Group therapy for adolescents with repeated self harm: randomised controlled trial with economic evaluation. BMJ. 2011;342:d682. doi: 10.1136/bmj.d682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shaffer D, Gould MS, Brasic J, et al. A Children’s Global Assessment Scale (CGAS) Arch Gen Psychiatry. 1983;40(11):1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- 27.Pfeffer CR. The suicidal child. New York (NY): The Guilford Press; 1986. [Google Scholar]
- 28.Statistics Canada . Consumer price index, CANSIM (database) [Internet] Ottawa (ON): Statistics Canada; 2011. [cited 2011 Sep 14 Available from: http://www5.statcan.gc.ca/cansim/a26?lang=eng&retrLang=eng&id=3260021&paSer=&pattern=&stByVal=1&p1=1&p2=-1&tabMode=dataTable&csid= [Google Scholar]
- 29.Drummond MF, Sculpher MJ, Torrance GW, et al. Methods for the economic evaluation of health care programmes. 3rd ed. Oxford (GB): Oxford University Press; 2005. [Google Scholar]
- 30.Fenwick E, O’Brien BJ, Briggs A. Cost-effectiveness acceptability curves—facts, fallacies and frequently asked questions. Health Econ. 2004;13(5):405–415. doi: 10.1002/hec.903. [DOI] [PubMed] [Google Scholar]
- 31.Hoch JS, Briggs AH, Willan AR. Something old, something new, something borrowed, something blue: a framework for the marriage of health econometrics and cost-effectiveness analysis. Health Econ. 2002;11(5):415–430. doi: 10.1002/hec.678. [DOI] [PubMed] [Google Scholar]
- 32.Willan AR, Briggs AH, Hoch JS. Regression methods for covariate adjustment and subgroup analysis for non-censored cost-effectiveness data. Health Econ. 2004;13(5):461–475. doi: 10.1002/hec.843. [DOI] [PubMed] [Google Scholar]
- 33.Wang R, Lagakos SW, Ware JH, et al. Statistics in medicine— reporting of subgroup analyses in clinical trials. N Engl J Med. 2007;357(21):2189–2194. doi: 10.1056/NEJMsr077003. [DOI] [PubMed] [Google Scholar]
- 34.Nixon RM, Thompson SG. Methods for incorporating covariate adjustment, subgroup analysis and between-centre differences into cost-effectiveness evaluations. Health Econ. 2005;14(12):1217–1229. doi: 10.1002/hec.1008. [DOI] [PubMed] [Google Scholar]