Abstract
Objective:
To determine whether people who have died from suicide in a large epidemiologic sample form clusters based on demographic, clinical, and psychosocial factors.
Method:
We conducted a coroner’s chart review for 2886 people who died in Toronto, Ontario, from 1998 to 2010, and whose death was ruled as suicide by the Office of the Chief Coroner of Ontario. A cluster analysis using known suicide risk factors was performed to determine whether suicide deaths separate into distinct groups. Clusters were compared according to person- and suicide-specific factors.
Results:
Five clusters emerged. Cluster 1 had the highest proportion of females and nonviolent methods, and all had depression and a past suicide attempt. Cluster 2 had the highest proportion of people with a recent stressor and violent suicide methods, and all were married. Cluster 3 had mostly males between the ages of 20 and 64, and all had either experienced recent stressors, suffered from mental illness, or had a history of substance abuse. Cluster 4 had the youngest people and the highest proportion of deaths by jumping from height, few were married, and nearly one-half had bipolar disorder or schizophrenia. Cluster 5 had all unmarried people with no prior suicide attempts, and were the least likely to have an identified mental illness and most likely to leave a suicide note.
Conclusions:
People who die from suicide assort into different patterns of demographic, clinical, and death-specific characteristics. Identifying and studying subgroups of suicides may advance our understanding of the heterogeneous nature of suicide and help to inform development of more targeted suicide prevention strategies.
Keywords: suicide, Toronto, coroner records, cluster analysis
Abstract
Objectif :
Déterminer si les personnes qui sont mortes par suicide dans un vaste échantillon épidémiologique forment des groupes selon des facteurs démographiques, cliniques et psychosociaux.
Méthode :
Nous avons mené une revue des dossiers du coroner des 2886 personnes qui sont décédées à Toronto, Ontario, de 1998 à 2010, et dont le décès a été classé comme un suicide par le Bureau du coroner en chef de l’Ontario. Une analyse en grappe a été menée à l’aide des facteurs connus du risque de suicide, afin de déterminer si les décès par suicide se divisaient en groupes distincts. Les grappes ont été comparées en vertu des facteurs propres à la personne et au suicide.
Résultats :
Cinq groupes se sont dégagés. Le groupe 1 avait la proportion la plus élevée de femmes et de méthodes non violentes, et tous avaient des antécédents de dépression et de tentative de suicide. Le groupe 2 avait la proportion la plus élevée de personnes ayant eu un stresseur récent et des méthodes de suicide violentes, et toutes étaient mariées. Le groupe 3 se composait surtout d’hommes de 20 à 64 ans, et tous avaient soit subi des stresseurs récents, soit souffert de maladie mentale, soit eu des antécédents d’abus de substances. Le groupe 4 contenait les personnes les plus jeunes et la proportion la plus élevée de décès attribuables à une chute d’une hauteur, peu étaient mariés, et près de la moitié souffrait d’un trouble bipolaire ou de schizophrénie. Le groupe 5 ne contenait que des personnes célibataires sans antécédents de tentative de suicide, et elles étaient les moins susceptibles d’avoir une maladie mentale identifiée et les plus enclines à laisser une note de suicide.
Conclusions :
Les personnes qui meurent par suicide se répartissent en différents modèles de caractéristiques démographiques, cliniques et de mort particulières. L’identification et l’étude des sous-groupes de suicides peuvent nous faire mieux comprendre la nature hétérogène du suicide, et contribuer à éclairer l’élaboration de stratégies de prévention du suicide mieux ciblées.
It has been estimated that 1 million people, worldwide, die from suicide each year, and many countries have adopted national suicide prevention strategies to try to address this important public health issue.1 Suicide is a complex behavioural outcome, often resulting from the confluence of demographic and psychiatric risk factors along with stressful life events.2,3 Therefore, it has been argued that suicide prevention efforts are more likely to succeed if they simultaneously target multiple risk factors.4 However, many historical efforts at preventing suicide at a population level have focused on restricting access to the means of suicide5,6 despite evidence that such strategies in isolation may not alter suicide rates.7–14 In contrast, there have been several recent attempts to identify different paths to suicide by examining patterns of risk factors common to groups of people who die by suicide. O’Conner et al15 examined coroner records for 142 suicides in Belfast and found 3 clusters that differed according to contact with health care, depression, other mental illness, substance abuse, past attempts, and living circumstances. A similar study16 analyzed 148 suicide deaths in Hong Kong and found 2 groups: one associated with psychotic disorders, psychiatric treatment, and acute stress, and one associated with financial problems, chronic stress, and no psychiatric illness. Most recently, Logan et al17 examined US National Violent Death Reporting System data on 28 703 suicide deaths and identified 9 different suicide clusters that differed based on rates of mental illness, substance abuse, past suicide attempts, stressors, and acute alcohol intoxication. While this is the largest and most comprehensive study examining suicide clusters to date, it is unclear to what extent the results can be generalizable outside the United States, most strikingly because 50% of them occurred by firearms. This is in sharp contrast to countries, such as England or Scotland, where the most common methods of suicide are hanging, jumping from height and (or) being struck by a train, and self-poisoning, while firearms are used in fewer than 10% of deaths.18 This large difference in suicide methods may mean that a larger proportion of impulsive attempts in the United States result in actual death,19 which, in turn, limits generalizability.
Reviews of coroner records in Canada have typically used small samples on the order of 100 suicide deaths20–22 or have involved linkages with administrative databases with limited person- or suicide-specific details.23,24 Our study is the largest of its kind in Canada, examining a sample about 20 times larger than those in Belfast and Hong Kong described above. It aims to identify distinct clusters of suicides in Toronto. Toronto is arguably the most multicultural city in the world, with 50% of its population having been born outside of Canada.25 Therefore, it provides a unique venue for researching whether suicide deaths assort into clusters based on common risk factors in a culturally heterogeneous setting. Our study is the first to be published as part of the Toronto Analysis of Suicide for Knowledge and Prevention, which involves ongoing collection and analysis of data on all suicides in Toronto to better characterize and understand suicide in an effort to inform future suicide prevention initiatives.
Method
Study Design
The Office of the Chief Coroner (OCC) of Ontario granted us access to its records for the purposes of this research. Data were collected from OCC’s charts for all deaths occurring in the city of Toronto from 1998–2010, inclusive, that were ruled as suicides. Deaths were ruled as suicides according to a standard of a high degree of probability. Data beyond 2010 were not available at the time of data analysis because it takes about 2 years before all OCC investigations are complete. The goal of the study was to characterize suicide in Toronto residents. Therefore, people who travelled into Toronto from outside the city to die from suicide were excluded, as were people who had made a suicide attempt in other parts of Ontario and had been transported to hospitals in Toronto for more subspecialized care where they later died.
Clinical Implications
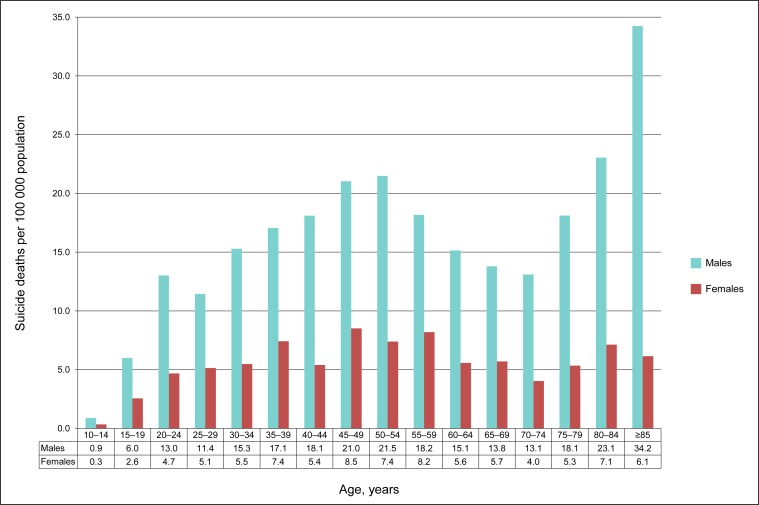
Suicide occurs in all age groups, but per-capita rates peak in middle age for both sexes and in elderly males.
Suicide deaths are heterogeneous and assort into different patterns of demographic, clinical, and death-related factors.
Future prevention efforts need to account for these differences.
Limitations
This study compares groups of people who died from suicide with no living control group.
Although clusters emerged, there was some overlap between them.
Suicide deaths by nonviolent means may be underestimated.
Data were abstracted by the primary investigator and 2 research assistants. Initially, 10 charts were coded independently to ensure good interrater reliability. Throughout the period of data abstraction, the investigators and research assistants were in continuous contact to resolve questions about how to code each chart while maintaining consistency. Each chart contained a coroner’s investigation report, which included a determination of death, a pathology report, and commonly other sources of information, such as police reports, letters from family members, and copies of suicide notes. The coroner’s investigation also frequently included information from direct interviews with family members, acquaintances, and, in some cases, the deceased’s physician(s). The presence and type of mental illness, stressors, as well as recent physician or hospital contact were sometimes available via copies of medical records but often came from interviews with family and friends. Data were collected through reviews of any and all information present in charts for each death as detailed above. Data for each variable of interest were available in most but not all charts. Data collected included
demographics: age, sex, and marital status;
mental illness;
contact with a hospital and (or) emergency department or psychiatrist within 7 days prior to suicide;
recent stressors (noted to have occurred or caused distress within the last year), including bereavement, unemployment, financial problems, immigration stressors, relationship breakup, interpersonal conflict, recent medical stressors (including being upset about a diagnosis, diminishing health, or loss of independence due to a medical condition), and criminal justice involvement;
method of suicide; and
other details of the suicide, including location of death and the presence of a suicide note.
Suicide deaths by self-poisoning and nonhanging asphyxia were considered nonviolent, while all other methods were considered violent. Other variables of potential interest, such as sexual orientation and race, were not typically available.
Census data were also collected from the Statistics Canada website for population by age group in Toronto according to the 1996,26 2006,27 and 201128 censuses to determine suicide rates by population.
Statistical Analysis
Suicide rates by population were calculated by dividing the number of suicides in males and females in a given year by the Toronto population by sex for that year and then taking the average of all years in the study. Population during noncensus years was interpolated assuming linear growth. All statistics were performed using IBM SPSS Statistics 20.0 (IBM SPSS Inc, Armonk, NY). The primary analysis used a 2-step method of cluster analysis to identify different clusters in the data. Cluster distance was determined using the log-likelihood measure and the optimal number of clusters was determined automatically by the statistical software based on Schwartz’s Bayesian information criterion. The silhouette measure of cohesion and separation provided a measure of the degree to which clusters were distinct. Age was the only continuous variable included in the analysis. Dichotomous variables included sex, marital status (married or unmarried), presence of any stressor, depression, other mental illness, substance abuse (drug and [or] alcohol), and a history of suicide attempts. Details of the suicide, such as specific methods used, location of death, and presence of a note, were analyzed subsequently but not included in determining the clusters, given the goal of finding clusters that could be targeted prior to the act of suicide. One-way ANOVA tests with the Tukey honestly significant difference post hoc tests and chi-square tests were conducted to determine which continuous and categorical variables, respectively, were significantly different between the clusters, at a threshold for significance of 0.05.
Our study was approved by the Research Ethics Board at Sunnybrook Health Sciences Centre in Toronto.
Results
There were 2886 suicide deaths in Toronto from 1998 to 2010 (mean 222 deaths/year). Suicide rates by age and sex are shown in Figure 1. A peak was observed for both sexes for ages from 45 to 54, and in males older than 80. Analysis of these deaths yielded 5 clusters, with an average silhouette width of 0.3, which indicates that these clusters are distinct but overlap to some degree. Such overlap was seen regardless of which variables were included in the analysis. Demographic, clinical, and stressor data for each cluster are shown in Table 1. Suicide-specific data for each cluster are shown in Table 2.
Figure 1.
Death rates according to age and sex for people dying from suicide in Toronto from 1998 to 2010
Table 1.
Cluster analysis results showing demographic and clinical variables for people dying from suicide in Toronto from 1998 to 2010
| Variable | Cluster 1 n = 304 | Cluster 2 n = 488 | Cluster 3 n = 561 | Cluster 4 n = 584 | Cluster 5 n = 949 | F | df | P |
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Mean age, years | 48.1 | 55.6 | 43.3 | 42.9 | 46.5 | 45.96 | 4/2881 | <0.001 |
|
| ||||||||
| % | % | % | % | % | χ2 | df | P | |
| Age, years | 264.5 | 16 | <0.001 | |||||
| ≤19 | 1.6 | 0.2 | 1.8 | 3.1 | 5.9 | |||
| 20–34 | 19.7 | 11.5 | 23.2 | 30.8 | 26.0 | |||
| 35–49 | 36.2 | 28.1 | 43.9 | 35.8 | 28.1 | |||
| 50–64 | 26.0 | 28.7 | 25.5 | 20.7 | 20.2 | |||
| ≥65 | 16.4 | 31.6 | 5.7 | 9.6 | 19.7 | |||
| Sex, male | 57.6 | 73.9 | 80.0 | 61.6 | 73.7 | 81.4 | 8 | <0.001 |
| Marital status | 1991 | 12 | <0.001 | |||||
| Single | 46.1 | 0 | 54.9 | 77.1 | 73.2 | |||
| Married | 32.2 | 100 | 21.0 | 4.3 | 0 | |||
| Divorced or separated | 18.1 | 0 | 22.1 | 16.1 | 17.7a | |||
| Widowed | 3.6 | 0 | 2.0 | 2.6 | 9.2a | |||
| Any stressor in past year | 47.4 | 61.9 | 60.1 | 32.4 | 51.7 | 124.5 | 4 | <0.001 |
| Specific stressor in past year | ||||||||
| Interpersonal conflict | 16.8 | 18.6 | 17.5 | 10.1 | 11.9 | 26.5 | 4 | <0.001 |
| Employment and (or) financial | 16.1 | 20.5 | 24.4 | 9.4 | 18.5 | 47.9 | 4 | <0.001 |
| Intimate partner breakup | 9.5 | 1.0 | 14.1 | 5.1 | 10.0 | 70.9 | 4 | <0.001 |
| Criminal and (or) legal | 3.9 | 4.3 | 12.8 | 5.1 | 4.4 | 54.9 | 4 | <0.001 |
| Bereavement | 6.2 | 3.7 | 7.3 | 4.3 | 6.0 | 9.00 | 4 | 0.06 |
| Medical health | 10.5 | 25.0 | 6.8 | 5.3 | 13.1 | 118.8 | 4 | <0.001 |
| Immigration | 0.7 | 3.5 | 0.7 | 0.7 | 1.8 | 19.6 | 4 | 0.001 |
| Past suicide attempts | 100 | 4.5 | 33.9 | 45.2 | 0 | 1409 | 4 | <0.001 |
| Mental illness | ||||||||
| Depression | 100 | 58.4 | 63.5 | 26.7 | 49.7 | 465.5 | 4 | <0.001 |
| Bipolar disorder | 0 | 2.9 | 6.1 | 20.9 | 0 | 323.5 | 4 | <0.001 |
| Schizophrenia | 0 | 2.3 | 6.4 | 26.9 | 0 | 462.0 | 4 | <0.001 |
| Other mental illness | 0 | 14.1 | 12.8 | 45.4 | 0 | 679.3 | 4 | <0.001 |
| Substance abuse | 0 | 0 | 100 | 3.8 | 0 | 2754.7 | 4 | <0.001 |
There was one case in which a person was known to be both divorced and widowed. This case has been included numerically in both categories but was excluded from the statistical analysis for marital status only.
Table 2.
Cluster analysis results showing details of suicide death and the events immediately preceding it for people dying from suicide in Toronto from 1998 to 2010
| Variable | Cluster 1 n = 304 % | Cluster 2 n = 488 % | Cluster 3 n = 561 % | Cluster 4 n = 584 % | Cluster 5 n = 949 % | χ2 | df | P |
|---|---|---|---|---|---|---|---|---|
| Suicide occurred at home | 82.2 | 71.5 | 74.9 | 67.3 | 68.4 | 1991 | 12 | <0.001 |
| Violent cause of deatha | 56.9 | 81.6 | 70.2 | 71.7 | 73.0 | 65.2 | 4 | <0.001 |
| Specific cause of death | 219.9 | 36 | <0.001 | |||||
| Hanging | 32.6 | 36.1 | 33.7 | 19.0 | 27.7 | |||
| Jumping from height | 13.8 | 24.6 | 19.8 | 32.2 | 25.4 | |||
| Self-poisoning | 30.9 | 11.7 | 26.2 | 22.8 | 14.3 | |||
| Subway or train collision | 3.0 | 7.0 | 5.7 | 10.3 | 9.6 | |||
| Nonhanging asphyxia | 12.2 | 6.8 | 3.6 | 5.5 | 9.6 | |||
| Firearm | 1.6 | 7.0 | 4.5 | 2.2 | 6.6 | |||
| Cutting and (or) stabbing | 2.0 | 3.5 | 3.0 | 3.8 | 3.5 | |||
| Drowning and (or) hypothermia | 3.3 | 2.0 | 2.5 | 2.9 | 2.0 | |||
| Fire, burns, and (or) electrocution | 0.7 | 1.4 | 0.9 | 1.4 | 1.3 | |||
| Suicide note left | 34.5 | 29.1 | 25.1 | 27.4 | 35.0 | 22.1 | 4 | <0.001 |
| Contact with psychiatry and (or) emergency department services in past week | 11.5 | 4.5 | 11.8 | 14.2 | 2.7 | 89.9 | 4 | <0.001 |
All suicide deaths not occurring by self-poisoning or nonhanging asphyxia are considered violent.
Cluster 1 is the smallest cluster (n = 304). It is characterized by the highest proportion of females of any cluster (42.4%), a 100% rate of past attempts as well as depression, and the highest proportions of deaths at home (82.2%) and by nonviolent means (43.1%), including self-poisoning (30.9%) and nonhanging asphyxia (12.2%).
Cluster 2 (n = 488) is characterized by being the oldest (mean age 55.6 years; 31.6% aged 65 years and older), all married (100%), with the largest proportion of people having experienced any stressor (61.9%), particularly interpersonal conflict (18.6%), employment and (or) financial (20.5%), medical (25.0%), and immigration (4.5%) stressors. Few had past attempts (4.5%), and this cluster involved the highest proportion of violent suicide methods (81.6%), including the most hanging (36.1%) and firearm deaths (7.0%) and the least from self-poisoning (11.7%).
Cluster 3 (n = 561) is characterized by a 100% rate of substance abuse, which was often comorbid with depression (63.5%). It is the cluster with the highest proportion of males (80.0%) and includes the smallest proportion of adolescents or the elderly (92.5% between the ages of 20 and 64). It has the largest proportion of divorced or separated people (22.1%), people with employment and (or) financial (24.4%) and criminal legal stressors (12.8%), as well as bereavement (7.3%) and intimate partner breakup (14.1%).
Cluster 4 (n = 584) is the youngest cluster (mean age 42.9 years; 69.7% less than 50 years). People in this cluster were nearly all unmarried (95.7%), with the fewest experiencing a stressor in the past year (32.4%), the second highest proportion of past attempts (45.2%), and the highest proportion suffering from bipolar disorder (BD) (20.9%), schizophrenia (26.9%), and any mental illness apart from depression (66.4%). This group had the largest amount of recent contact with a hospital or psychiatry (14.1%), and had the highest proportion of deaths outside the home (32.7%), by jumping from height (32.2%), and by subway or train collision (10.3%).
Cluster 5 is the largest cluster (n = 949). No one in this cluster was married, and 9.2% were widowed. They had no past attempts, the lowest rates of any mental illness, the least recent contact with a hospital or psychiatry (2.7%), and were the most likely to leave a suicide note (35.0%).
Discussion
Suicide in the Total Sample
With about 1 death per 1000 population each decade, suicide is an important cause of death in Toronto, as in most other cities around the world. Overall, our study confirmed several previous findings, including that the 10-year age group from age 45 to 54 account numerically for the most suicides. This further supports the notion that middle adulthood has become a high-risk period for suicide, especially given evidence from both the United Kingdom and the United States showing suicide rates to be highest in this group.18,29,30 That suicide rates peak in elderly men also confirms what is known in the literature.31
Suicide Clusters
Suicide is a complex phenomenon that is unlikely to adhere to rigid archetypes. The identification of subgroups of people who die by suicide is an important step toward a more advanced approach to understanding the causes and pathways to suicide, and ultimately to develop more targeted and effective suicide prevention measures.
Our study reports on the largest detailed review of coroner data on suicide deaths ever conducted in Canada. We found that suicide deaths predominantly occurred among males, age 18 to 65, who suffered from depression or another major mental illness. These demographic patterns are in keeping with the literature on suicide,17,29,32 and their strong effect helps to explain why the identified clusters all overlap to some degree. Nevertheless, our study did identify 5 clinically meaningful patterns of demographic, psychiatric, and stress-related factors associated with suicides in Toronto.
Cluster 1 had the highest proportion of females and involves suicidal acts that may have been less well planned and more impulsive. All members of cluster 1 were depressed and had a history of suicide attempts, and it had the highest proportion of deaths at home and by nonviolent means. A growing literature shows that outreach to people who have attempted suicide, through efforts such as phone calls and postcards, may decrease suicide attempts in similar populations.33–36 Such programs could be implemented in Toronto at relatively little cost.
Cluster 2 is notable because everyone was married and very few had prior suicide attempts despite both of these factors being considered protective against suicide.37,38 This finding would support the need for ongoing and universal surveillance of suicidal ideation, even in people who may appear at low risk. For example, one might advocate for increased physician awareness that it is important to screen for suicidal ideation and plans in those who are elderly and (or) dealing with a significant stressors, both common features of this cluster.
Everyone in cluster 3 had problems with substance abuse and most suffered from mental illness. This was the cluster that was mostly composed of middle-aged males with high rates of stressors. While it has been shown that alcohol is associated with suicide independent of psychiatric illness,39 this cluster underscores the complex interplay between substance use, underlying mental illness, and stress. It may be that various health care providers and organizations that commonly see people with this confluence of risk factors should be more aware of the risks of suicide. For example, 12.8% of people in this cluster had criminal–legal stressors. It has previously been argued that the court system could be an important ally in suicide prevention strategies.17 Perhaps such efforts would be best focused on middle-aged men with substance histories.
Cluster 4 is the youngest cluster, with the fewest stressors and the most nondepression, major mental illness, including nearly one-half with schizophrenia or BD. This cluster was most likely to have had contact with mental health services in the past week. However, we should note that more than 85% of people in this cluster still had no known contact in the past week. The cluster analysis in Hong Kong by Chen et al16 demonstrated 2 clusters, with 1 having higher rates of psychotic illness, death by jumping from height, and lower rates of chronic stressors. This pattern is in keeping with the findings for cluster 4. If stressful life events are less of a factor in this group, it may be that a combination of poorly controlled mental illness and poor coping skills were the driving factors in these deaths. Efforts to prevent suicides in people like those in this cluster may involve more vigorous surveillance and treatment of symptoms in those with identified major mental illness. They may also involve greater access to urgent mental health care, both in hospital settings and via specialized resources in the community, such as mobile crisis teams.
Cluster 5 is the largest, accounting for about one-third of all of the suicide deaths, and perhaps the most enigmatic. All were unmarried, and roughly one-half had recent stressors, but they had the lowest rates of identified mental illness and contact with psychiatric care in the past week. This cluster appears to be the most socially isolated. An analysis of the content of suicide notes may be an important next step in understanding the motivation for suicide in this group, and, indeed, in each of the other groups, although some evidence suggests that studies of those who leave notes may not be generalizable to everyone who dies from suicide.40
Directly comparing these clusters to the 9 clusters identified in the United States by Logan et al17 is challenging, given that their study separated known mental health diagnoses from depressed mood at the time of death without a prior diagnosis and separated a history of substance abuse from the presence of alcohol at the time of death. The nature of the data in our study meant that we were unable to make these distinctions. Nevertheless, there are some important similarities and points of difference between the cluster analyses. Both studies found a relatively high degree of overlap between age and gender among clusters. Cluster 2 in our study includes elements of class 2 (mental health conditions with recent crises), class 4 (current depressed mood with financial problems), and class 6 (medical health problems with depressed mood) from the US study.17 Cluster 3 in our study includes elements of class 1 (mental health conditions with alcohol problems), class 5 (alcohol problems with other stressful life events, and class 7 (recent stressors with criminal legal problems) from the US study. The US study also distinguished clusters with known histories of mental illness (classes 1–3) from those without known mental illness that had combinations of stressors and substance abuse with or without depressed mood (classes 4–9). Note a similar pattern here between clusters 1–4 and cluster 5. A crucial distinction between the 2 studies involves firearm use as a method of suicide death. While both of the oldest clusters in each study had the highest rates of death by firearms, these corresponded to 7% in cluster 2 here and 74% in class 5 of the US study. This large discrepancy is likely due, at least in part, to availability of firearms.
Strengths and Limitations
The key strengths of our study are that it involves one of the largest coroner chart reviews ever conducted and that it examines suicide deaths in Toronto, which, given its diverse populace, makes it an important setting for examining suicides that may be more generalizable to suicide deaths in cities around the world. This is reflected by the demographics of the sample and the distribution of suicide methods, which are consistent with what has been reported outside the United States.18,41
Our study also has 3 broad limitations. These relate to the study’s reliance on coroner records, its lack of a control group, and how the clusters were determined. While OCC reports in Toronto are extremely thorough, any such system of population-based data collection is necessarily imperfect. It has been argued that, in some cases, suicides, particularly by self-poisoning or drowning, may sometimes be misclassified as accidental or natural deaths.42 Given the large number of deaths, it was not practically possible to review those ruled to have causes other than suicide. Therefore, we should assume that the suicide deaths described here, particularly by those methods, may be an underestimate. This may be especially important in elderly women. Given that women as a group are more likely to use nonviolent means, such as self-poisoning, it may be that suicide rates per-capita in women, like men, peak in older age, but that this was obscured because these deaths were not identified as suicides. Further, while some elements of the data collected, such as age, sex, method of death, and presence of a suicide note, are likely highly accurate, other data, such as psychiatric diagnoses and stressors, were often derived from interviews with next of kin and may be less valid43 and not available for all cases. It may be that certain stressors were underreported or that certain diagnoses, such as borderline personality disorder or BD, were mistakenly described as depression. Nevertheless, it is likely that most suicide deaths in Toronto are captured in this dataset and that the data overall are generally reliable. Not having a population-based control group also limits our ability to fully interpret our study. It may be that certain variables cluster together anyway in the population. For example, we would anticipate, given that males are more likely to abuse substances, that the most male cluster would have the highest rate of substance abuse, which was the case in cluster 3. However, we would also expect, for example, that the oldest cluster would be the most widowed, though this was not the case. The oldest cluster was the only cluster with no widows (cluster 2), which is the opposite of what we would logically expect in the general population. Thus, while these clusters likely do differ to some degree from their age- and sex-matched population equivalents, our study was not designed to determine those differences. Finally, the modest silhouette width between clusters underscores that suicide deaths do not fit neatly into perfect categories and that the results presented here may be instructive but should not be overstated. This result is also in keeping with previous cluster analyses, such as the one conducted in Belfast, which also showed significant cluster overlap in terms of demographics, stressors, and methods of suicide.15
Conclusions
Suicide is an important public health issue, and our study was the first step in an effort to characterize who dies from suicide in Toronto. Five clusters of suicide deaths emerged according to demographic, clinical, and death-related factors. More work needs to be done to further understand the motivations of people in these different groups. Future avenues would include detailed comparisons of suicide notes, toxicology, and psychiatric records between people in different clusters.
Acknowledgments
We thank Dr James Edwards, June Lindsell, Andrew Stephen, and the staff at the OCC of Ontario for their support in making this research possible. We also thank the Physicians’ Services Incorporated (PSI) Foundation for their generous grant support for this project. We further thank Catherine Reis, Michelle Messner, and Dr Andrew Howlett for their efforts to make this work possible.
Our research received funding from the PSI Foundation. The funding source had no role in the design and conduct of the study; in the collection, analysis, and interpretation of the data; or in the preparation, review, or approval of the manuscript.
Dr Sinyor and Dr Streiner report no competing interests. Dr Schaffer has acted as a consultant for Lundbeck, Sunovion, Bristol-Myers Squibb, and the Canadian Network for Mood and Anxiety Treatments. Dr Schaffer has also received grant funding from AstraZeneca Canada and Pfizer, and payment for lectures, presentations, and (or) speakers bureau honoraria from Eli Lilly, Bristol-Myers Squibb, and AstraZeneca Canada.
References
- 1.Hawton K, van Heeringen K. Suicide. Lancet. 2009;373:1372–1381. doi: 10.1016/S0140-6736(09)60372-X. [DOI] [PubMed] [Google Scholar]
- 2.Overholser JC, Braden A, Dieter L. Understanding suicide risk: identification of high-risk groups during high-risk times. J Clin Psychol. 2012;68(3):349–61. doi: 10.1002/jclp.20859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mościcki EK. Identification of suicide risk factors using epidemiologic studies. Psychiatr Clin North Am. 1997;20(3):499–517. doi: 10.1016/s0193-953x(05)70327-0. [DOI] [PubMed] [Google Scholar]
- 4.Mościcki EK. Epidemiology of suicide. Int Psychogeriatr. 1995;7(2):137–148. [PubMed] [Google Scholar]
- 5.Gunnell D, Middleton N, Frankel S. Method availability and the prevention of suicide: a re-analysis of secular trends in England and Wales 1950–1975. Soc Psychiatry Psychiatr Epidemiol. 2000;35:437–443. doi: 10.1007/s001270050261. [DOI] [PubMed] [Google Scholar]
- 6.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: a systematic review. JAMA. 2005;294(16):2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 7.Bateman DN. Limiting paracetamol pack size: has it worked in the UK? Clin Toxicol. 2009;47:536–541. doi: 10.1080/15563650903093192. [DOI] [PubMed] [Google Scholar]
- 8.Lester D. The effects of detoxification of domestic gas on suicide in the United States. Am J Public Health. 1990;80:80–81. doi: 10.2105/ajph.80.1.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lester D. Effects of detoxification of domestic gas on suicide in the Netherlands. Psychol Rep. 1991;68:202. doi: 10.2466/pr0.1991.68.1.202. [DOI] [PubMed] [Google Scholar]
- 10.Ohberg A, Lonnqvist J, Sarna S, et al. Trends and availability of suicide methods in Finland. Proposals for restrictive measures. Br J Psychiatry. 1995;166(1):35–43. doi: 10.1192/bjp.166.1.35. [DOI] [PubMed] [Google Scholar]
- 11.Rich CL, Young JG, Fowler RC, et al. Guns and suicide: possible effects of some specific legislation. Am J Psychiatry. 1990;147:342–346. doi: 10.1176/ajp.147.3.342. [DOI] [PubMed] [Google Scholar]
- 12.Sinyor M, Levitt AJ. Effect of a barrier at Bloor Street Viaduct on suicide rates in Toronto: natural experiment. BMJ. 2010;341:c2884. doi: 10.1136/bmj.c2884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sloan JH, Rivara FP, Reay DT, et al. Firearm regulations and rates of suicide. A comparison of two metropolitan areas. N Engl J Med. 1990;322:369–373. doi: 10.1056/NEJM199002083220605. [DOI] [PubMed] [Google Scholar]
- 14.Wiedenmann A, Weyerer S. The impact of availability, attraction and lethality of suicide methods on suicide rates in Germany. Acta Psychiatr Scand. 1993;88:364–368. doi: 10.1111/j.1600-0447.1993.tb03474.x. [DOI] [PubMed] [Google Scholar]
- 15.O’Conner RC, Sheehy NP, O’Connor DB. The classification of completed suicide into subtypes. J Ment Health. 1999;8(6):629–637. [Google Scholar]
- 16.Chen EY, Chan WS, Chan SS, et al. A cluster analysis of the circumstances of death in suicides in Hong Kong. Suicide Life Threat Behav. 2007;37(5):576–584. doi: 10.1521/suli.2007.37.5.576. [DOI] [PubMed] [Google Scholar]
- 17.Logan J, Hall J, Karch D. Suicide categories by patterns of known risk factors: a latent class analysis. Arch Gen Psychiatry. 2011;68(9):935–941. doi: 10.1001/archgenpsychiatry.2011.85. [DOI] [PubMed] [Google Scholar]
- 18.The University of Manchester Centre for Mental Health and Risk . Annual report: England, Wales, Scotland, and Northern Ireland [Internet] Manchester (GB): The University of Manchester; 2012. National confidential inquiry into suicide and homicide by people with mental illness. [cited 2013 Feb 3]. Available from: http://www.bbmh.manchester.ac.uk/cmhr/research/centreforsuicideprevention/nci/reports/annual_report_2012.pdf. [Google Scholar]
- 19.Lewiecki EM, Miller SA. Suicide, guns, and public policy. Am J Public Health. 2013;103(1):27–31. doi: 10.2105/AJPH.2012.300964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lesage A, Séguin M, Guy A, et al. Systematic services audit of consecutive suicides in New Brunswick: the case for coordinating specialist mental health and addiction services. Can J Psychiatry. 2008;53(10):671–678. doi: 10.1177/070674370805301006. [DOI] [PubMed] [Google Scholar]
- 21.Séguin M, Lesage A, Chawky N, et al. Suicide cases in New Brunswick from April 2002 to May 2003: the importance of better recognizing substance and mood disorder comorbidity. Can J Psychiatry. 2006;51(9):581–586. doi: 10.1177/070674370605100906. [DOI] [PubMed] [Google Scholar]
- 22.Kisely S, Campbell LA, Cartwright J, et al. Factors associated with not seeking professional help or disclosing intent prior to suicide: a study of medical examiners’ records in Nova Scotia. Can J Psychiatry. 2011;56(7):436–440. doi: 10.1177/070674371105600707. [DOI] [PubMed] [Google Scholar]
- 23.Morrison KB, Laing L. Adults’ use of health services in the year before death by suicide in Alberta. Health Rep. 2011;22(3):15–22. [PubMed] [Google Scholar]
- 24.Edwards N, Alaghehbandan R, MacDonald D, et al. Suicide in Newfoundland and Labrador: a linkage study using medical examiner and vital statistics data. Can J Psychiatry. 2008;53(4):252–259. doi: 10.1177/070674370805300406. [DOI] [PubMed] [Google Scholar]
- 25.Statistics Canada . Population by immigrant status and period of immigration, 2006 counts, for Canada and census divisions—20% sample data. Ottawa (ON): Statistics Canada; 2006. [Google Scholar]
- 26.Statistics Canada . Census of population. Statistics Canada catalogue no 95F0181XDB96001 (Toronto Metropolitan Municipality, code 3520) [Internet] Ottawa (ON): Statistics Canada; 1996. 2006. [cited 2013 Jan 18]. Available from: http://www12.statcan.gc.ca/english/census96/data/profiles/Rp-eng.cfm?TABID=1&LANG=E&APATH=3&DETAIL=0&DIM=0&FL=A&FREE=0&GC=0&GID=202018&GK=0&GRP=1&PID=35782&PRID=0&PTYPE=3&S=0&SHOWALL=0&SUB=0&Temporal=1996&THEME=34&VID=0&VNAMEE=&VNAMEF=&D1=0&D2=0&D3=0&D4=0&D5=0&D6=0. [Google Scholar]
- 27.Statistics Canada . Statistics Canada catalogue no 92-591-XWE [Internet] Ottawa (ON): Statistics Canada; 2007. Mar 13, Toronto, Ontario (code 3520005) (table). 2006 community profiles. 2006 Census. [cited 2013 Jan 18]. Available from: http://www12.statcan.ca/census-recensement/2006/dp-pd/prof/92-591/details/|page.cfm?Lang=E&Geo1=CD&Code1=3520&Geo2=PR&Code2=35&Data=Count&SearchText=toronto&SearchType=Begins&SearchPR=01&B1=All&Custom=. [Google Scholar]
- 28.Statistics Canada . Statistics Canada catalogue no 98–316-XWE [Internet] Ottawa (ON): Statistics Canada; 2012. Oct 24, Toronto, Ontario (code 3520005) and Toronto, Ontario (code 3520) (table). Census profile. 2011 Census. [cited 2013 Jan 18]. Available from: http://www12.statcan.gc.ca/census-recensement/2011/dp-pd/prof/index.cfm?Lang=E. [Google Scholar]
- 29.Centres for Disease Control and Prevention (CDC), Morbidity and Mortality Weekly Report . QuickStats: suicide and homicide rates,* by age group—United States, 2009 [figure] [Internet] Atlanta (GA): CDC; 2012. [cited 2013 Feb 2]. Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6128a8.htm. [Google Scholar]
- 30.Langlois S, Morrison P. Suicide deaths and suicide attempts. Health Rep. 2002;13(2):9–22. [PubMed] [Google Scholar]
- 31.Conwell Y, Van Orden K, Caine ED. Suicide in older adults. Psychiatr Clin North Am. 2011;34(2):451–468. ix. doi: 10.1016/j.psc.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Harris EC, Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry. 1997;170:205–228. doi: 10.1192/bjp.170.3.205. [DOI] [PubMed] [Google Scholar]
- 33.Carter GL, Clover K, Whyte IM, et al. Postcards from the EDge project: randomised controlled trial of an intervention using postcards to reduce repetition of hospital treated deliberate self poisoning. BMJ. 2005;331(7520):805. doi: 10.1136/bmj.38579.455266.E0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Motto JA, Bostrom AG. A randomized controlled trial of postcrisis suicide prevention. Psychiatr Serv. 2001;52(6):828–833. doi: 10.1176/appi.ps.52.6.828. [DOI] [PubMed] [Google Scholar]
- 35.Vaiva G, Vaiva G, Ducrocq F, et al. Effect of telephone contact on further suicide attempts in patients discharged from an emergency department: randomised controlled study. BMJ. 2006;332(7552):1241–1245. doi: 10.1136/bmj.332.7552.1241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fleischmann A, Bertolote JM, Wasserman D, et al. Effectiveness of brief intervention and contact for suicide attempters: a randomized controlled trial in five countries. Bull World Health Organ. 2008;86:703–709. doi: 10.2471/BLT.07.046995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Griffiths C, Ladva G, Brock A, et al. Trends in suicide by marital status in England and Wales, 1982–2005. Health Stat Q. 2008;(37):8–14. [PubMed] [Google Scholar]
- 38.McLean J, Maxwell M, Platt S, et al. Risk and protective factors for suicide and suicidal behaviour: a literature review Scottish Government Social Research [Internet] Edinburgh (GB): The Scottish Government; 2008. [cited 2013 Feb 2]. Available from: http://www.scotland.gov.uk/Publications/2008/11/28141444/0. [Google Scholar]
- 39.Flensborg-Madsen T, Knop J, Mortensen EL, et al. Alcohol use disorders increase the risk of completed suicide—irrespective of other psychiatric disorders: a longitudinal cohort study. Psychiatry Res. 2009;167(1–2):123–130. doi: 10.1016/j.psychres.2008.01.008. [DOI] [PubMed] [Google Scholar]
- 40.Haines J, Williams CL, Lester D. The characteristics of those who do and do not leave suicide notes: is the method of residuals valid? Omega (Westport) 2011;63(1):79–94. doi: 10.2190/OM.63.1.d. [DOI] [PubMed] [Google Scholar]
- 41.Nordentoft M. Prevention of suicide and attempted suicide in Denmark. Epidemiological studies of suicide and intervention studies in selected risk groups. Dan Med Bull. 2007;54(4):306–369. [PubMed] [Google Scholar]
- 42.Speechley M, Stavraky KM. The adequacy of suicide statistics for use in epidemiology and public health. Can J Public Health. 1991;82(1):38–42. [PubMed] [Google Scholar]
- 43.Campbell LA, Jackson L, Bassett R, et al. Can we use medical examiners’ records for suicide surveillance and prevention research in Nova Scotia? Chronic Dis Inj Can. 2011;31(4):165–171. [PubMed] [Google Scholar]