Abstract
Objective:
About one-half to two-thirds of all suicides are by people who suffer from mood disorders; preventing suicides among those who suffer from them is thus central for suicide prevention. Understanding factors underlying suicide risk is necessary for rational preventive decisions.
Method:
The literature on risk factors for completed and attempted suicide among subjects with depressive and bipolar disorders (BDs) was reviewed.
Results:
Lifetime risk of completed suicide among psychiatric patients with mood disorders is likely between 5% and 6%, with BDs, and possibly somewhat higher risk than patients with major depressive disorder. Longitudinal and psychological autopsy studies indicate suicidal acts usually take place during major depressive episodes (MDEs) or mixed illness episodes. Incidence of suicide attempts is about 20- to 40-fold, compared with euthymia, during these episodes, and duration of these high-risk states is therefore an important determinant of overall risk. Substance use and cluster B personality disorders also markedly increase risk of suicidal acts during mood episodes. Other major risk factors include hopelessness and presence of impulsive–aggressive traits. Both childhood adversity and recent adverse life events are likely to increase risk of suicide attempts, and suicidal acts are predicted by poor perceived social support. Understanding suicidal thinking and decision making is necessary for advancing treatment and prevention.
Conclusion:
Among subjects with mood disorders, suicidal acts usually occur during MDEs or mixed episodes concurrent with comorbid disorders. Nevertheless, illness factors can only in part explain suicidal behaviour. Illness factors, difficulty controlling impulsive and aggressive responses, plus predisposing early exposures and life situations result in a process of suicidal thinking, planning, and acts.
Keywords: major depressive disorder, bipolar disorder, suicide, attempted suicide
Abstract
Objectif :
Entre la moitié et les deux tiers de tous les suicides sont le fait de personnes qui souffrent de troubles de l’humeur; la prévention du suicide chez ceux qui en souffrent est donc primordiale à cette prévention. Il est nécessaire de comprendre les facteurs sousjacents du risque de suicide pour prendre des décisions rationnelles de prévention.
Méthode :
La littérature sur les facteurs de risque de suicide et de tentatives de suicide chez les sujets souffrant de troubles dépressifs et bipolaires (TB). a été revue
Résultats :
Le risque à vie de suicide chez les patients psychiatriques souffrant de troubles de l’humeur se situe probablement entre 5 % et 6 %, pour le TB, et le risque est possiblement plus élevé que chez les patients souffrant de trouble dépressif majeur. Les études longitudinales d’autopsie psychologique indiquent que les gestes suicidaires ont habituellement lieu durant les épisodes dépressifs majeurs (EDM) ou les épisodes de maladies mixtes. L’incidence des tentatives de suicide est environ de 20 à 40 fois plus que celle de l’euthymie durant ces épisodes, et la durée de ces états à risque élevé est donc un déterminant important du risque global. L’utilisation de substance et les troubles de la personnalité du groupe B accroissent aussi assurément le risque de gestes suicidaires durant les épisodes affectifs. D’autres importants facteurs de risque inlcuent notamment le désespoir et la présence de traits impulsifs-agressifs. Tant l’adversité vécue durant l’enfance que les événements de vie indésirables récents sont susceptibles d’accroître le risque de tentatives de suicide, et les gestes suicidaires sont prédits par un mauvais soutien social perçu. Comprendre la pensée et la prise de décision suicidaires est nécessaire pour que progressent le traitement et la prévention.
Conclusion :
Chez les sujets souffrant de troubles de l’humeur, les gestes suicidaires surviennent habituellement durant les EDM ou les épisodes mixtes de troubles comorbides. Néanmoins, les facteurs de la maladie n’expliquent que partiellement le comportement suicidaire. Les facteurs de la maladie, la difficulté de contrôler des réactions impulsives et agressives, en plus des expositions précoces et des situations de vie qui y prédisposent forment un processus de pensée, de planification, et de gestes suicidaires.
Completed suicide is a major cause of death. According to the World Health Organization, annually, worldwide, about 1 million people take their own lives. Suicide is a complex phenomenon, with multiple domains of risk factors, and valid perspectives for both scientific explanation and prevention. For psychiatry, however, a central fact is that, according to numerous psychological autopsy studies,1,2 almost all subjects (about 90%) have suffered from some— usually multiple—mental disorders at time of death. Among all completed suicides, one-half to two-thirds are by people who have suffered from mood disorders.1,2 This means that prevention of suicides by people suffering from mood disorders is central for suicide prevention in general.
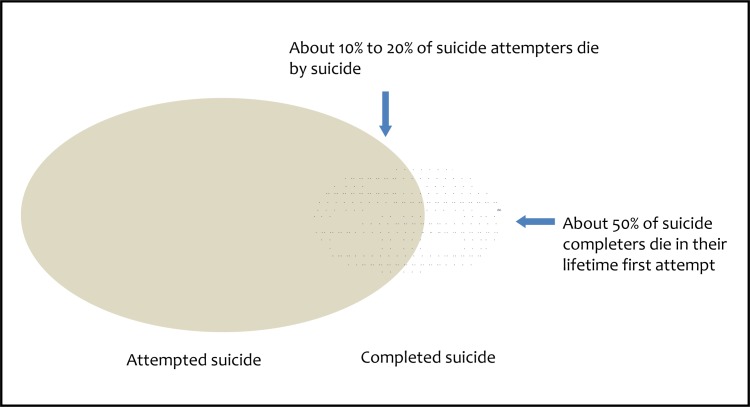
Suffering from a mood disorder thus means a risk of death by suicide. While knowing risk factors for suicide in mood disorders is of utmost importance for prevention, there are many limitations in the available literature. Of necessity, much of the literature focuses on suicide attempts as proxy for completed suicide. Studies on suicide attempts provide important information on suicidal acts, but it is important to remember differences in characteristics between populations of completed and attempted suicide. In general, completers are much more often males, have used more lethal methods than overdoses, are somewhat older, have, in about 50%, died in their lifetime first attempt,3 and suffered from more severe psychopathology than the attempters.4,5 Up to 20% of suicide attempters will eventually die by suicide6 (Figure 1).
Figure 1.
The relation between completed and attempted suicide
Lifetime Risk of Suicide in Mood Disorders
Early estimates of lifetime risk of patients with mood disorders suggested 15% to 19% of patients die by suicide.7–9 However, there were significant limitations, in both the available data as well as the methodology that later authors have noted, showing, for example, incompatibility of the high estimates with high prevalence estimates of depression in the general population.10–12 Bostwick and Pankratz13 documented a gradient of lifetime suicide risk (case fatality prevalence) from general population to suicidal inpatients with mood disorders ranging from 0.5% to 8.6%. The most accurate current estimates of lifetime suicide risk are from a national study of suicide risk14 following all subjects born between 1955 and 1991 who had been treated in a psychiatric hospital in Denmark up to the year 2006, or as outpatients (after 1995). The study found absolute lifetime risk for men with BD to be 7.77% (95% CI 6.01% to 10.05%), and for those with unipolar affective disorder, 6.67% (95% CI 5.72% to 7.78%); for females with BD, 4.78% (95% CI 3.48% to 6.56%) and unipolar (MDD) affective disorder, 3.77% (95% CI 3.05% to 4.66%). While these figures are still high, they are more compatible with the epidemiology of mood disorders. They do not generalize to primary care patients, or general population subjects not having treatment contacts for their disorder. Conversely, with a median follow-up of 18 years, they likely underestimate true lifetime risk. In the longest follow-up study reported, Angst et al15 found 11.1% of the 406 patients who died by suicide ranged between 40 and 44 years. It is unavoidable that all these case fatality estimates reflect treatments as provided during the past decades, not outcomes of patients in current treatment settings.
Clinical Implications
Suicidal acts by patients with mood disorders are temporally strongly associated with course of illness, particularly MDEs and mixed mood disorder episodes. Rapidly alleviating symptoms and preventing recurrences, thus reducing the time patients spend in these high-risk states, are credible measures in reducing overall risk of suicidal acts.
Risk of suicidal acts during MDEs or mixed episodes is strongly related to concurrent cluster B personality and substance use disorders and impulsive–aggressive traits, particularly among young adults below age 40.
Understanding suicidal thinking and decision making is necessary for advancing treatment and prevention.
Limitations
This is a narrative, selective review with no quantitative meta-analysis.
The focus is on clinical and epidemiologic research.
Risk factors and risk evaluation, not of treatment or intervention studies, are reviewed.
Prevalence and Incidence of Suicide Attempts Among Patients With MDD and BD
Suicidal behaviour is common among people with mood disorders. However, the exact prevalence and incidence of suicidal ideation or attempts depends on the setting and characteristics of the patients treated. In most psychiatric settings, most patients with mood disorders who are treated either have attempted suicide or have significant suicidal ideation.16,17 In cross-sectional studies, the prevalence of attempters is higher among patients with type BD I or II than those with MDD.16,17 Reported prevalence of positive lifetime history of suicide attempts among psychiatric patients with mood disorders varies widely between studies and settings, but has been found in regionally representative samples with both out- and inpatients to be 30% to 40% in MDD and about 50% among patients with BD.16–18 In prospective studies, incidence either appears higher among patients with BD19 than MDD,20,21 or grossly similar.22,23 Prevalence of suicide attempts is similar in BD I and II disorders.24
Risk Factors for Completed Suicide Among Subjects With Mood Disorders
Information on risk factors for completed suicide in mood disorders is relatively limited. The register-based Danish national study14 found male sex, history of a suicide attempt, and comorbid SUD all associated with higher risk of completed suicide, both in depressive and bipolar mood disorders. Prospective clinical cohort studies of patients with mood disorders25–27 have found risk factors for completed suicide to include male sex, family history of suicide, previous suicide attempts, hopelessness, suicidal ideation, psychotic symptoms, comorbid personality disorders, alcohol dependence or misuse, and anxiety disorders. In a recent systematic review by Hawton et al,28 the role of these risk factors was confirmed, with the exceptions of psychotic symptoms and suicidal ideation not reaching statistical significance. A 2005 meta-analysis by Hawton et al29 of risk factors for completed suicide among subjects with BD found male sex, previous suicide attempts, and hopelessness to be the most robust risk factors. A recent, large, register-based cohort study found male sex and concurrent diagnosis of anxiety disorder risk factors for suicide in patients with BD.30
Some psychological autopsy studies have specifically focused or reported on people with mood disorders who died by suicide, and their findings are largely concordant with the above studies. Almost all people with MDD or BD who die by suicide have significant psychiatric or somatopsychiatric comorbidity, with some gender-specific patterns.31,32 The higher number of diagnosed mental disorders among depressive people who die by suicide than among community or depressive control subjects highlights the increased risk related to comorbidity.33,34 Among specific comorbid disorders, SUDs (alcoholism, drug abuse, or polysubstance abuse) and cluster B or borderline personality disorders are particularly strongly associated with suicides among subjects with depression.33–36 Aggressive and extremes of impulsive traits may either predispose people to these mental disorders,35 or directly predispose them to suicide.36 However, the role of these disorders and traits is much more important among younger (less than 40 years) than older people who die by suicide,35,36 and among males than females. In contrast, among older adults with depression, the role of concurrent physical illness may be more important.31 Adverse life events, particularly losses, are the typical psychosocial context of suicide.33,37 Multiple stressors, some perhaps precipitating mood episodes, others more likely triggering the act, appear common among suicides by subjects with both unipolar (MDD) or bipolar mood disorders.38
The psychological autopsy literature focusing on BDs is very limited but documents the roles of depressive and mixed episodes as likely risk states, and the role of SUDs among males with BD who die by suicide.38 There is some controversy concerning the role of BD II in psychological autopsies, as an early Hungarian study39 found one-half of all people with depression who died by suicide, and one-quarter of all, to have suffered from BD II. This is in contrast with other psychological studies1,2 that rarely find the proportion of all BDs to exceed 10%; whether this is a true finding and specific to Hungary, or owing to differences in diagnostic procedures, remains open. Most psychological autopsy studies have likely underestimated prevalence of BD, particularly of BD II.
Risk Factors for Suicide Attempts Among Psychiatric Patients With MDD
In clinical studies conducted in psychiatric settings, numerous risk factors for suicide attempts, from multiple domains, have been investigated. These have included sociodemographic and social factors, such as younger age16,22 and poor social support16,18,20,40,41; illness-related factors, such as severe or recurrent depression, or failure to achieve remission,20,42 early age at onset,19 psychotic symptoms,43,44 melancholia,43 and presence of MDE21,22; and psychiatric comorbidity, including personality disorders (especially borderline),45 alcohol dependence or misuse,18,22,45–47 or chronic physical illness.46 More specifically related to suicidal behaviour are history of a preceding suicide attempt by the patient,18,20,21,22,46,47 or suicidal behaviour in the family,18 hopelessness,22,45 suicidal ideation,22,45 or aggressive or impulsive traits.18,22,45,48 In addition, causal or not, cigarette smoking22,45 is associated with suicide attempts.
In the published prospective studies, risk factors for suicide attempt42,46,49,50 or completed suicide25,27,51 have included a history of suicide attempts by the patient or suicide in the family,25,49–51 high severity of depression,27,42 comorbid personality disorder,27,49 comorbid alcohol dependence or abuse,2,46,50 comorbid chronic physical illness,46 younger age,49 hopelessness,25 and suicidal ideation.25 However, most of these prospective studies have been either conducted within exclusively inpatient settings, have had relatively small sample sizes, or investigated diagnostically mixed populations. This may limit generalizability of their findings to other settings, or power to detect risk factors. A review of the prospective studies found history of past suicidal behaviour, recurrent or refractory depression, and comorbid alcoholism the most robust predictors.43
Suicide Attempts Among Depressive Patients in Primary Care
The role of improved detection and management of depression in primary health care is one of the central tenets of suicide prevention strategies.52 Despite this central role, suicidal behaviour among primary care patients with depression has been little investigated, particularly concerning young and middle-aged patients. Poor recognition, especially of mild depressions, is a common problem in primary care (see, for example, Thompson et al53), but it is unclear whether this is also true concerning depressions that eventually lead to attempted or completed suicide, as they may be clinically more severe or complicated. Whether the risk for suicidal acts depends on severity, chronicity, or comorbidity, that is, whether a meaningful risk is present in all depressions, however mild, or clustered into a more ill subgroup, is decisive for creating optimal preventive strategies. Overall, suicide mortality among depressed patients is lower in primary care than in psychiatric settings.15,54 A psychological autopsy study focusing on depression in primary care55 found that most suicides are by males with psychiatric comorbidity and untreated depression, and with their intent rarely communicated, particularly during the last appointment preceding suicide.55,56 Similarly, studies on suicide attempters in primary care report rare communication of suicidal ideation, even if they have been receiving treatment for depression.57,58 A cohort study representing depressive primary care patients in a Finnish city59 found one-sixth (17%) of them having ever attempted suicide. The attempters were patients with moderate to severe MDD, psychiatric comorbidity with personality disorders, and a history of psychiatric care. Most were already receiving treatment for depression, but their suicidal ideation had usually remained unrecognized. A 5-year follow-up of the cohort found suicide attempts to occur almost exclusively during MDEs, often with concurrent substance abuse, but hardly ever known by the attending primary care physician.60 Thus the available studies accord that suicidal acts tend to cluster in MDEs of complicated high-risk patients, but their suicidal intention or acts commonly remain unrecognized.
Overall, improving quality of care of primary care depressions is, in itself, important, but whether education and training are the optimal strategy also for preventing suicide remains open, and may depend on time and setting. The temporary success of the early Gotland study (see Rutz et al61) has turned out difficult to replicate,62 and effectiveness of educational interventions in changing doctors’ behaviour is known to be limited.63 However, a multimodal, population-level German intervention study64 also involved primary care doctors, and was successful in reducing at least nonfatal suicidal acts in the city of Nuremberg. Another major intervention study focusing on education and training of primary care doctors in Hungary was, to some extent, successful in reducing suicide rate in the county of intervention.65
Risk Factors for Suicide Attempts Among Patients With BD
Risk of suicidal behaviour among patients with BD is unlikely to be exceeded by any other Axis I disorder.66 Estimates for the lifetime prevalence of a nonfatal suicide attempt among patients with BD vary widely. Most studies report prevalences of 30% to 40%,24 but estimates can exceed 50%,17,19 particularly including attempts not leading to a health care contact. A systematic review29 of the risk factors for suicide attempts among patients with BD found them to include family history of suicide, early onset, extent of depressive symptoms, high severity, presence of mixed affective states, rapid cycling, comorbid Axis I disorders, and abuse of alcohol or drugs. However, the review had to rely almost exclusively on retrospective and cross-sectional studies, with few of the prospective studies available at the time.29
In prospective studies, risk factors predicting suicide attempts have included a history of past suicide attempts,19,22,67,68 suicidal ideation,69 family history of suicidal behaviour,70,71 subjective rating of depression severity, depressive index phase, or percentage of depressive days during the preceding year,19,22,67 comorbid alcohol dependence or abuse,70 anxiety disorder,30 cigarette smoking,22 hopelessness,19,22 hostility,70 aggression and (or) impulsivity,22 and young age.19,70
In cross-sectional and retrospective studies,72–77 mixed states have been found strongly related to suicidal behaviour. There are also cross-sectional and retrospective studies suggesting affective temperaments,78 particularly cyclothymic, but also depressive, anxious, and irritable temperaments, to associate with suicidal acts.79,80 It would be important for prospective studies to clarify whether this is due to these temperaments per se, for example, rapid mood switches,81 or them (that is, affective temperaments) predicting future depressive or mixed episodes.
The predominant polarity of illness episodes has recently been shown to be associated with occurrence of suicide attempts.82 As expected, patients with predominantly depressive course of illness have a 2-fold risk of suicide attempts, compared with predominantly manic patients; including patients with mixed states into depressive polarity strengthens the association to 4.5-fold.82 Considered together with studies showing more prior hospitalizations for depression,69 current depressive type of index episode,19 or proportion of time spent depressed preceding the time of evaluation67 to predict suicide attempt, there is good evidence that patients with predominantly depressive and mixed course of illness are at higher risk for future suicidal acts than those with predominantly manic course.
Retrospective studies have indicated that besides illness course, early adversity is likely to have strong influence on risk of suicidal behaviour. History of childhood sexual or physical abuse has been found strongly associated with suicide attempts among patients with BD,69,83 with the most severe exposures likely predicting the highest risk for suicide attempts.69
Presence and intensity of suicidal ideation is a clinical indicator of risk for a suicidal act. Valtonen et al19 investigated, in a receiver operating characteristic (commonly referred to as an ROC curve) analysis, the degree to which the SSI predicts risk for suicide attempts in the next 6 months. A score of 8 was found to have relatively good sensitivity (0.82), moderate specificity (0.69), and PPV of 31% for a suicide attempt. Given that PPV strongly depends on base rate of suicide attempts, the SSI may be most useful among patients with BD in settings with particularly high risk of suicidal behaviour.
Overall, risk of suicide attempts is strongly associated with course of bipolar illness and predicted by history of past suicidal behaviour, but also significantly influenced by risk factors from other domains. Whether risk factors may differ between different types of illness phases remains unclear. Valtonen et al77 found suicide attempts to cluster exclusively among people with depressive, depressive mixed, or mixed episodes, with hopelessness most strongly predicting suicide attempts during depressive phases, and subjective severity of depressive symptoms during mixed phases. Age and sex are other likely modifiers of risk, with studies generally finding higher risk of attempts among the young19,70; besides the higher risk of completed suicide among males, some evidence also exists for possible differences in risk factors between males and females.68
The Influence of Mood Episodes and Their Temporal Course on Risk of Suicidal Acts
A clinician treating patients with suicidal ideation and mood disorder usually finds it self-evident that the patients’ symptomatic state must be promptly alleviated to prevent suicidal acts, and it is common clinical experience to see suicidal ideation abate upon alleviation of symptoms.83–86 Therefore, it is astonishing how clinical suicide research has thus far largely failed to provide a sound database to evaluate the role of symptom improvement or treatment in prevention of suicidal behaviour among patients with mood disorders. This is largely due to the scarcity of intensive longitudinal observational studies of suicidal patients able to inform about longitudinal covariation of symptoms and timing of suicidal acts, and to the few clinical trials including suicidal patients.
The paradigmatic stress–diathesis model by Mann and colleagues45,87 conceptualizes suicidal acts as the outcome of the balance between trait- and state-related predisposing and protective factors. The stress–diathesis model is a widely accepted and valid conceptual framework. However, the role of not only presence and severity of symptoms as time-varying risk factors but also time spent at risk in the high-risk states should be explicitly accounted for in this context. Suicide risk is known to vary remarkably, even during short periods of time. For example, in the Danish national register-based study of suicides after psychiatric hospitalization,88 the incidence of suicide among patients with affective disorder during the first postdischarge week was found to be extremely high (ARR 219 for males and 1977 for females), but then to steeply decline within the first months to reach a much lower, albeit still elevated level (ARR < 15) after 1 year. A national Swedish study89 had similar results. The effect sizes of these temporal variations far exceed those of known high-risk traits, and indicate obvious targets for prevention.
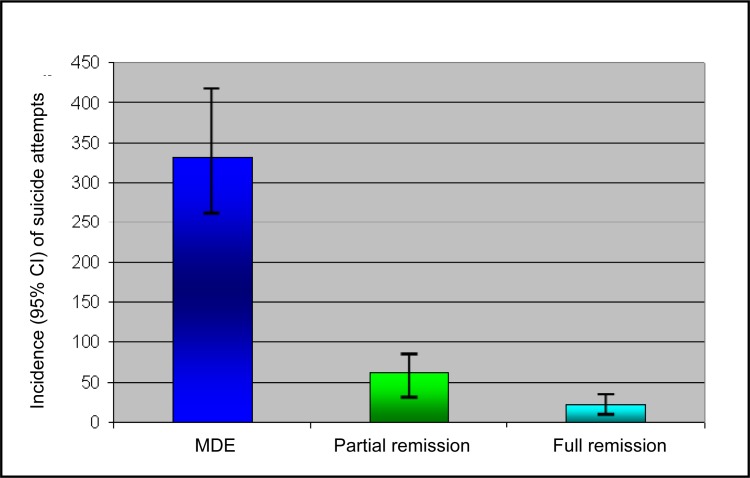
The time a person spends in high-risk states can be expected to exert a major influence in the overall risk of a suicidal act over time. Temporal variations in risk states, such as depression, and time spent in them, are likely to be important determinants of cumulative overall risk for suicidal acts. However, very few long-term studies on mood disorder have linked information on suicide attempts to patients’ concurrent clinical state and cumulative exposure to risk states. Longitudinal studies combining life-chart methodology with precise timing of attempts are scarce. Thus the relative importance (effect size) of state and trait factors has remained elusive. Within the context of longitudinal, life-chart–based studies of depression (the Vantaa Depression Study; see Sokero et al20 and Holma et al21) and BD I and II (the Jorvi Bipolar Study, see Valtonen et al90), we investigated the incidence of suicide attempts over time across variable mood states. We found that during a 5-year follow-up of psychiatric patients with MDD, three-fourths of suicide attempts took place during MDEs. The incidence of attempts was 21-fold during the time depressed and 4-fold during partial remission, compared with time in full remission21 (Figure 2). In long-term follow-up of psychiatric MDD patients, their proportion of time spent in MDEs is much higher in the early than the later years of follow-up, thus suicidal acts also cluster in the early years. Among patients with BD, the incidence of suicide attempts also varied remarkably, depending on the type of illness phase, with the highest (38-fold) risk involving mixed and depressive mixed phases, and high (18-fold) risk also occurring during MDEs.90 The population attributable fraction of time spent in MDEs for suicide attempts was 78% among patients with MDD,21 and 86% for patients with BD (including total time in MDEs, and depressive mixed and mixed states).90 These findings are consistent with the findings of Oquendo et al,42 who reported similar markedly elevated hazard during MDEs in a postdischarge patient cohort, and our own findings (see Riihimäki et al60) from a primary care depression cohort. Thus time spent in high-risk illness phases is likely the major determinant of overall risk for suicide attempts among patients with mood disorders. Note that life charts only very crudely catch the true clinical variation in mood states; thus all the above risk estimates, even if high, are likely to be gross underestimates of true risk variation. The obvious but poorly documented clinical implication is that effective management of these states may be crucial for prevention.
Figure 2.
Incidence of suicide attempts during MDEs and partial or full remission among psychiatric patients with MDD during 5 years of follow-up
Data indicate the incidence rate per 1000 patient-years based on Poisson distribution.
Reprinted with permission from the American Journal of Psychiatry (Copyright 2010).21 American Psychiatric Association.
Accounting for differences in incidence across mood states and durations of high-risk periods may also shed light on the long controversy of existence and reasons for differences in suicide risk between MDD and BD I and II.24 It appears that risk of both completed suicide14 and attempted suicide20,21,90 may be slightly higher in BD. However, incidence of suicide attempts during MDEs is unlikely to be markedly different between the types of mood disorders.20,21,23,90 Differences in overall risk could be largely due to differences in the distribution of time spent at risk, and thus vary depending on the longitudinal course of illness rather than on the type of disorder, per se. Spending more time in depressed or in the mixed illness phases may well explain why BD II is often associated with more frequent suicidal behaviour than BD I. The same factor would apply to MDD.
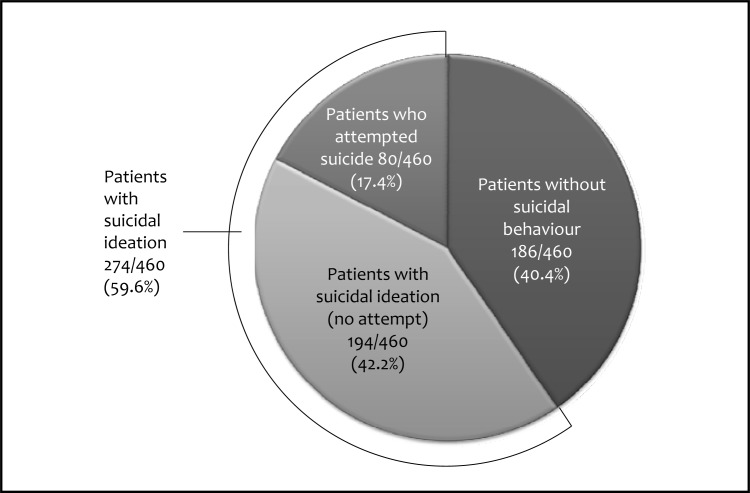
Why Are Not All Patients With Mood Disorders Suicidal?
Not all people who suffer from major mood disorders plan or attempt suicide, despite often intensive suffering. In epidemiologically representative cohorts of patients in community psychiatric care services in neighbouring Finnish cities, we found that about 40% of patients report no significant suicidal ideation, while about 50% did, and about 17% had attempted suicide during the index episode16,17 (Figure 3). Thus a significant minority, in general patients with currently milder symptoms and less comorbid disorders, had no suicidal ideation or attempts during the index episode. However, as one-third of patients with depression16 and about one-half of patients with BD I or II17 reported having ever attempted suicide, many of the currently nonsuicidal patients had previously been so. Among patients with BD, suicidal ideation and attempts were strongly related to type of index episode, as ideation and attempts were common during an MDE, or in mixed or depressive mixed illness phases, but absent during the manic or hypomanic periods.90 The observed differences between patients with BD or MDD persisted over time, both for proportion of attempters and for cumulative incidences of attempt.20,21,90 Nevertheless, although findings may vary from one setting to another, it is obvious that even a severe mood disorder alone is not a sufficient explanation for suicidal behaviour. While presence of comorbidity significantly, in part, explains the individual differences in propensity toward suicidal behaviour, other factors must also have a role.
Figure 3.
Suicidal behaviour during the index episode among psychiatric patients with mood disorder in the Vantaa Depression Study16 and Jorvi Bipolar Study17 (Ntotal = 460)
Impulsive and aggressive traits are important for suicidal behaviour overall, and for suicidal behaviour in depression specifically.91,92 Even if suicidal acts among patients with mood disorders almost always take place in the presence of a major mood episode and are preceded by suicidal ideation,16,17,30,31,93 these traits are likely to play a major role in determining who will act on the urge. The role of these traits as risk factors is less clear among patients with BD, as impulsive and aggressive behaviour is commonplace during manic, hypomanic, or mixed illness phases. However, when assessed with laboratory performance measures (immediate and delayed memory tasks), severe suicidal behaviour was found to be associated with impulsivity in BD.94 Information on these traits adds to that of preceding suicidal acts as an indicator of high risk, and may be especially valuable in the young age groups,36 remembering that one-half of all people who die by suicide do so in their first attempt.3
Psychological vulnerability to suicidal behaviour can be conceptualized in multiple ways. In an influential cognitive model of suicidal acts,95 activation of a suicide schema leads to (state) hopelessness, selective attention toward suicide-relevant cues, and inability to disengage from them, all of which predispose to suicidal ideation. The frequency, duration, and severity of suicide-relevant cognitions will determine the probability that a person will engage in a suicidal act. Further, suicide schemas are postulated to strengthen with each suicidal act, thus previous suicide attempts can be thought of as true (causal) risk factors for future suicidal acts, not merely as indicators of underlying vulnerability. Cognitive therapy has been shown to reduce repetitions of suicide attempts in a randomized clinical trial96 among recent suicide attempters, the vast majority with MDD, and is undoubtedly one of the most promising interventions available.
Who, When and Why—Implications for Prevention and Research
As most psychiatric patients suffering from a major depressive or a mixed mood episode actually consider, plan, or attempt suicide,16,17 mere suffering from a major mood disorder itself explains much of the associated suicidal behaviour. The temporal and dose-exposure association with severity of illness, duration of illness risk states, and suicidal acts strengthens the argument, and is essential for prevention. As suicidal acts by patients with mood disorders are rare in the absence of a major depressive or a mixed mood episode, reducing time spent in these high-risk states by means of treatment is a highly credible preventive measure. Nevertheless, it is obvious that a mood disorder itself still only partly explains suicidal behaviour. Presence of other mental disorders—SUDs, anxiety disorders, borderline personality disorder—usually significantly contributes to the risk. High impulsive and aggressive traits are likely to strongly influence who will act on suicidal ideas when depressed; meaningful and important relationships are powerful and proven protective factors. Personal history of childhood neglect or abuse may lead to developmental and neuroendocrinological scars through, for example, epigenetic mechanisms,97 which render a person vulnerable in adulthood crises. However, attempted and completed suicides are ultimately to be understood as acts to which illnesses and traits only predispose a person. Advances in understanding suicidal thinking, strongly intertwined with mood states, as well as psychological and neurocognitive factors influencing a person’s decision making,95,98–102 are needed to advance the clinical care of suicidal patients and prevention of suicidal behaviour. It is an area where psychotherapy and neuroscience must meet.
Table 1.
Central risk factors for suicidal behaviour in mood disorders
| Type of suicidal behaviour | Risk factor domain | Risk factor |
|---|---|---|
| Completed suicide | Sex | • Male |
| Suicidal behaviour | • Previous suicide attempts • Suicidal ideation and planning |
|
| Illness-related | • High severity of depressive syndrome • Postdischarge period |
|
| Comorbidity | • SUDs • Anxiety disorders • Cluster B personality disorders |
|
| Cognitions | • Hopelessness | |
| Life events | • Adverse events (losses and conflicts) | |
| Traits | • Impulsive–aggressive traits (particularly, <40 years) | |
| Specific to BD | • Mixed states | |
| Suicide methods | • Availability and acceptability of a lethal method | |
| Attempted suicide | Sex | • Female |
| Suicidal behaviour | • Previous suicide attempts • Suicidal ideation and planning |
|
| Illness-related | • High severity of depressive syndrome (subjective more than objective) • Accumulating total duration of MDEs |
|
| Age | • Young age • Young age at onset |
|
| Comorbidity | • SUDs • Anxiety disorders • Cluster B personality disorders |
|
| Cognitions | • Hopelessness or pessimism | |
| Traits | • Impulsive–aggressive traits, hostility • Hostility |
|
| Specific to BD | • Mixed states (also MDEs with hypomanic symptoms) • Cyclothymic affective temperament |
Acknowledgments
During the last 3 years, the author has thrice received honoraria for lecturing, and once also chairing and participating in planning of educational meetings sponsored by a pharmaceutical company (Servier). He has also twice received support for participating in a scientific meeting abroad from a pharmaceutical company (H Lundbeck).
Abbreviations
- ARR
adjusted risk ratio
- BD
bipolar disorder
- MDD
major depressive disorder
- MDE
major depressive episode
- PPV
positive predictive value
- SSI
Scale for Suicidal Ideation
- SUD
substance use disorder
References
- 1.Cavanagh JT, Carson AJ, Sharpe M, et al. Psychological autopsy studies of suicide: a systematic review. Psychol Med. 2003;33(3):395–405. doi: 10.1017/s0033291702006943. [DOI] [PubMed] [Google Scholar]
- 2.Arsenault-Lapierre G, Kim C, Turecki G. Psychiatric diagnoses in 3275 suicides: a meta-analysis. BMC Psychiatry. 2004;4:37. doi: 10.1186/1471-244X-4-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Isometsä ET, Lönnqvist JK. Suicide attempts preceding completed suicide. Br J Psychiatry. 1998;173:531–536. doi: 10.1192/bjp.173.6.531. [DOI] [PubMed] [Google Scholar]
- 4.Beautrais AL. Suicides and serious suicide attempts: two populations or one? Psychol Med. 2001;31:837–845. doi: 10.1017/s0033291701003889. [DOI] [PubMed] [Google Scholar]
- 5.Beautrais AL. Suicide and serious suicide attempts in youth: a multiple-group comparison study. Am J Psychiatry. 2003;160:1093–1099. doi: 10.1176/appi.ajp.160.6.1093. [DOI] [PubMed] [Google Scholar]
- 6.Suominen K, Isometsä E, Suokas J, et al. Completed suicide after a suicide attempt: a 37-year follow-up study. Am J Psychiatry. 2004;161:562–563. doi: 10.1176/appi.ajp.161.3.562. [DOI] [PubMed] [Google Scholar]
- 7.Guze SB, Robins E. Suicide and primary affective disorders. Br J Psychiatry. 1970;117:437–438. doi: 10.1192/bjp.117.539.437. [DOI] [PubMed] [Google Scholar]
- 8.Miles CP. Conditions predisposing to suicide: a review. J Nerv Ment Dis. 1977;164:231–246. doi: 10.1097/00005053-197704000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Goodwin FK, Jamison KR. Manic-depressive illness. New York (NY): Oxford University Press; 1990. [Google Scholar]
- 10.Blair-West GW, Mellsop GW, Eyeson-Annan ML. Down-rating lifetime suicide risk in major depression. Acta Psychiatr Scand. 1997;95:259–263. doi: 10.1111/j.1600-0447.1997.tb09629.x. [DOI] [PubMed] [Google Scholar]
- 11.Blair-West GW, Cantor CH, Mellsop GW, et al. Lifetime suicide risk in major depression: sex and age determinants. J Affect Disord. 1999;55:171–178. doi: 10.1016/s0165-0327(99)00004-x. [DOI] [PubMed] [Google Scholar]
- 12.Inskip HM, Harris EC, Barraclough B. Lifetime risk of suicide for affective disorder, alcoholism and schizophrenia. Br J Psychiatry. 1998;172:35–37. doi: 10.1192/bjp.172.1.35. [DOI] [PubMed] [Google Scholar]
- 13.Bostwick JM, Pankratz VS. Affective disorders and suicide risk: a reexamination. Am J Psychiatry. 2000;157:1925–1932. doi: 10.1176/appi.ajp.157.12.1925. [DOI] [PubMed] [Google Scholar]
- 14.Nordentoft M, Mortensen PB, Pedersen CB. Absolute risk of suicide after first hospital contact in mental disorder. Arch Gen Psychiatry. 2011;68:1058–1064. doi: 10.1001/archgenpsychiatry.2011.113. [DOI] [PubMed] [Google Scholar]
- 15.Angst J, Angst F, Gerber-Werder R, et al. Suicide in 406 mood-disorder patients with and without long-term medication: a 40 to 44 years’ follow-up. Arch Suicide Res. 2005;9:279–300. doi: 10.1080/13811110590929488. [DOI] [PubMed] [Google Scholar]
- 16.Sokero TP, Melartin TK, Rytsala HJ, et al. Suicidal ideation and attempts among psychiatric patients with major depressive disorder. J Clin Psychiatry. 2003;64:1094–1100. doi: 10.4088/jcp.v64n0916. [DOI] [PubMed] [Google Scholar]
- 17.Valtonen H, Suominen K, Mantere O, et al. Suicidal ideation and attempts in bipolar I and II disorders. J Clin Psychiatry. 2005;66:1456–1462. doi: 10.4088/jcp.v66n1116. [DOI] [PubMed] [Google Scholar]
- 18.Malone KM, Haas GL, Sweeney JA, et al. Major depression and the risk of attempted suicide. J Affect Disord. 1995;34:173–185. doi: 10.1016/0165-0327(95)00015-f. [DOI] [PubMed] [Google Scholar]
- 19.Valtonen HM, Suominen K, Mantere O, et al. Prospective study of risk factors for attempted suicide among patients with bipolar disorder. Bipolar Disord. 2006;8:576–585. doi: 10.1111/j.1399-5618.2006.00341.x. [DOI] [PubMed] [Google Scholar]
- 20.Sokero TP, Melartin TK, Rytsala HJ, et al. Prospective study of risk factors for attempted suicide among patients with DSM-IV major depressive disorder. Br J Psychiatry. 2005;186:314–318. doi: 10.1192/bjp.186.4.314. [DOI] [PubMed] [Google Scholar]
- 21.Holma KM, Melartin TK, Haukka J, et al. Incidence and predictors of suicide attempts in DSM-IV major depressive disorder: a five-year prospective study. Am J Psychiatry. 2010;167:801–808. doi: 10.1176/appi.ajp.2010.09050627. [DOI] [PubMed] [Google Scholar]
- 22.Oquendo MA, Galfalvy H, Russo S, et al. Prospective study of clinical predictors of suicidal acts after a major depressive episode in patients with major depressive disorder or bipolar disorder. Am J Psychiatry. 2004;161:1433–1441. doi: 10.1176/appi.ajp.161.8.1433. [DOI] [PubMed] [Google Scholar]
- 23.Fiedorowicz JG, Leon AC, Keller MB, et al. Do risk factors for suicidal behavior differ by affective disorder polarity? Psychol Med. 2009;39:763–771. doi: 10.1017/S0033291708004078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Novick DM, Swartz HA, Frank E. Suicide attempts in bipolar I and bipolar II disorder: a review and meta-analysis of the evidence. Bipolar Disord. 2010;12:1–9. doi: 10.1111/j.1399-5618.2009.00786.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fawcett J, Scheftner WA, Fogg L, et al. Time-related predictors of suicide in major affective disorder. Am J Psychiatry. 1990;147:1189–1194. doi: 10.1176/ajp.147.9.1189. [DOI] [PubMed] [Google Scholar]
- 26.Angst F, Stassen HH, Clayton PJ, et al. Mortality of patients with mood disorders: follow-up over 34–38 years. J Affect Disord. 2002;68(2–3):167–181. doi: 10.1016/s0165-0327(01)00377-9. [DOI] [PubMed] [Google Scholar]
- 27.Hansen PE, Wang AG, Stage KB, et al. Danish University Antidepressant Group Comorbid personality disorder predicts suicide after major depression: a 10-year follow-up. Acta Psychiatr Scand. 2003;107:436–440. [PubMed] [Google Scholar]
- 28.Hawton K, Casañas I, Comabella C, et al. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord. 2013;147:17–28. doi: 10.1016/j.jad.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 29.Hawton K, Sutton L, Haw C, et al. Suicide and attempted suicide in bipolar disorder: a systematic review of risk factors. J Clin Psychiatry. 2005;66:693–704. doi: 10.4088/jcp.v66n0604. [DOI] [PubMed] [Google Scholar]
- 30.Simon GE, Hunkeler E, Fireman B, et al. Risk of suicide attempt and suicide death in patients treated for bipolar disorder. Bipolar Disord. 2007;9:526–530. doi: 10.1111/j.1399-5618.2007.00408.x. [DOI] [PubMed] [Google Scholar]
- 31.Isometsä ET, Henriksson MM, Aro HM, et al. Suicide in major depression. Am J Psychiatry. 1994;151:530–536. doi: 10.1176/ajp.151.4.530. [DOI] [PubMed] [Google Scholar]
- 32.Isometsä ET, Henriksson MM, Aro HM, et al. Suicide in bipolar disorder in Finland. Am J Psychiatry. 1994;151:1020–1024. doi: 10.1176/ajp.151.7.1020. [DOI] [PubMed] [Google Scholar]
- 33.Foster T, Gillespie K, McClelland R, et al. Risk factors for suicide independent of DSM-III-R Axis I disorder. Case–control psychological autopsy study in Northern Ireland. Br J Psychiatry. 1999;175:175–179. doi: 10.1192/bjp.175.2.175. [DOI] [PubMed] [Google Scholar]
- 34.Cheng AT, Mann AH, Chan KA. Personality disorder and suicide. A case-control study. Br J Psychiatry. 1997;170:441–446. doi: 10.1192/bjp.170.5.441. [DOI] [PubMed] [Google Scholar]
- 35.Dumais A, Lesage AD, Alda M, et al. Risk factors for suicide completion in major depression: a case–control study of impulsive and aggressive behaviors in men. Am J Psychiatry. 2005;162:2116–2124. doi: 10.1176/appi.ajp.162.11.2116. [DOI] [PubMed] [Google Scholar]
- 36.McGirr A, Renaud J, Bureau A, et al. Impulsive–aggressive behaviours and completed suicide across the life cycle: a predisposition for younger age of suicide. Psychol Med. 2008;38:407–417. doi: 10.1017/S0033291707001419. [DOI] [PubMed] [Google Scholar]
- 37.Cheng AT, Chen TH, Chen CC, et al. Psychosocial and psychiatric risk factors for suicide. Case–control psychological autopsy study. Br J Psychiatry. 2000;177:360–365. doi: 10.1192/bjp.177.4.360. [DOI] [PubMed] [Google Scholar]
- 38.Isometsä E, Heikkinen M, Henriksson M, et al. Recent life events and completed suicide in bipolar affective disorder. A comparison with major depressive suicides. J Affect Disord. 1995;33:99–106. doi: 10.1016/0165-0327(94)00079-o. [DOI] [PubMed] [Google Scholar]
- 39.Rihmer Z, Barsi J, Arató M, et al. Suicide in subtypes of primary major depression. J Affect Disord. 1990;18:221–225. doi: 10.1016/0165-0327(90)90039-b. [DOI] [PubMed] [Google Scholar]
- 40.Mann JJ, Waternaux C, Haas GL, et al. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156:181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- 41.Malone KM, Oquendo KM, Haas GL, et al. Protective factors against suicidal acts in major depression: reasons for living. Am J Psychiatry. 2000;157:1084–1088. doi: 10.1176/appi.ajp.157.7.1084. [DOI] [PubMed] [Google Scholar]
- 42.Oquendo MA, Kamali M, Ellis SP, et al. Adequacy of antidepressant treatment after discharge and the occurrence of suicidal acts in major depression. Am J Psychiatry. 2002;159:1746–1751. doi: 10.1176/appi.ajp.159.10.1746. [DOI] [PubMed] [Google Scholar]
- 43.Oquendo MA, Currier D, Mann JJ. Prospective studies of suicidal behavior in major depressive and bipolar disorders: what is the evidence for predictive risk factors? Acta Psychiatr Scand. 2006;114(3):151–158. doi: 10.1111/j.1600-0447.2006.00829.x. [DOI] [PubMed] [Google Scholar]
- 44.Warman DM, Forman EM, Henriques GR, et al. Suicidality and psychosis: beyond depression and hopelessness. Suicide Life Threat Behav. 2004;34(1):77–86. doi: 10.1521/suli.34.1.77.27775. [DOI] [PubMed] [Google Scholar]
- 45.Mann JJ, Waternaux C, Haas GL, et al. Toward a clinical model of suicidal behavior in psychiatric patients. Am J Psychiatry. 1999;156:181–189. doi: 10.1176/ajp.156.2.181. [DOI] [PubMed] [Google Scholar]
- 46.Duggan CF, Sham P, Lee AL, et al. Can future suicidal behaviour in depressed patients be predicted? J Affect Disord. 1991;21:111–118. doi: 10.1016/0165-0327(91)90044-s. [DOI] [PubMed] [Google Scholar]
- 47.Maser JD, Akiskal HS, Schettler P, et al. Can temperament identify affectively ill patients who engage in lethal or near-lethal suicidal behavior? A 14-year prospective study. Suicide Life Threat Behav. 2002;32:10–32. doi: 10.1521/suli.32.1.10.22183. [DOI] [PubMed] [Google Scholar]
- 48.Mann JJ, Ellis SP, Waternaux CM, et al. Classification trees distinguish suicide attempters in major psychiatric disorders: a model of clinical decision making. J Clin Psychiatry. 2008;69:23–31. doi: 10.4088/jcp.v69n0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Paykel ES, Dienelt MN. Suicide attempts following acute depression. J Nerv Ment Dis. 1971;153(4):234–243. doi: 10.1097/00005053-197110000-00002. [DOI] [PubMed] [Google Scholar]
- 50.Bronisch T, Hecht H. Comparison of depressed patients with and without suicide attempts in their past history. Acta Psychiatr Scand. 1987;76:438–449. doi: 10.1111/j.1600-0447.1987.tb05629.x. [DOI] [PubMed] [Google Scholar]
- 51.Nordström P, Asberg M, Aberg-Wistedt A, et al. Attempted suicide predicts suicide risk in mood disorders. Acta Psychiatr Scand. 1995;92:345–350. doi: 10.1111/j.1600-0447.1995.tb09595.x. [DOI] [PubMed] [Google Scholar]
- 52.Mann JJ, Apter A, Bertolote J, et al. Suicide prevention strategies: a systematic review. JAMA. 2005;294:2064–2074. doi: 10.1001/jama.294.16.2064. [DOI] [PubMed] [Google Scholar]
- 53.Thompson C, Ostler K, Peveler RC, et al. Dimensional perspective on the recognition of depressive symptoms in primary care: The Hampshire Depression Project 3. Br J Psychiatry. 2001;179:317–323. doi: 10.1192/bjp.179.4.317. [DOI] [PubMed] [Google Scholar]
- 54.Simon GE, von Korff M. Suicide mortality among patients treated for depression in an insured population. Am J Epidemiol. 1998;147:155–160. doi: 10.1093/oxfordjournals.aje.a009428. [DOI] [PubMed] [Google Scholar]
- 55.Isometsä ET, Aro HM, Henriksson MM, et al. Suicide in major depression in different treatment settings. J Clin Psychiatry. 1994;55:523–527. [PubMed] [Google Scholar]
- 56.Isometsä ET, Heikkinen ME, Marttunen MJ, et al. The last appointment before suicide: is suicide intent communicated? Am J Psychiatry. 1995;152:919–922. doi: 10.1176/ajp.152.6.919. [DOI] [PubMed] [Google Scholar]
- 57.Haw C, Houston K, Townsend E, et al. Deliberate self-harm patients with depressive disorders: treatment and outcome. Affect Disord. 2002;70:57–65. doi: 10.1016/s0165-0327(01)00317-2. [DOI] [PubMed] [Google Scholar]
- 58.Houston K, Haw C, Townsend E, et al. General practitioner contacts with patients before and after deliberate self-harm. Br J Gen Pract. 2003;53:365–370. [PMC free article] [PubMed] [Google Scholar]
- 59.Vuorilehto M, Melartin T, Isometsa E. Suicidal behaviour among primary care patients with depressive disorders. Psychol Med. 2006;36:203–210. doi: 10.1017/S0033291705006550. [DOI] [PubMed] [Google Scholar]
- 60.Riihimäki K, Vuorilehto M, Melartin T, et al. Incidence and predictors of suicidal attempts among primary-care patients with depressive disorders: a 5-year prospective study. Psychol Med. 2013:1–12. doi: 10.1017/S0033291713000706. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 61.Rutz W, von Knorring L, Wålinder J. Long-term effects of an educational program for general practitioners given by the Swedish Committee for the Prevention and Treatment of Depression. Acta Psychiatr Scand. 1992;85:83–88. doi: 10.1111/j.1600-0447.1992.tb01448.x. [DOI] [PubMed] [Google Scholar]
- 62.Thompson C, Kinmonth AL, Stevens L, et al. Effects of a clinical-practice guideline and practice-based education on detection and outcome of depression in primary care: Hampshire Depression Project randomised controlled trial. Lancet. 2000;355:185–191. doi: 10.1016/s0140-6736(99)03171-2. [DOI] [PubMed] [Google Scholar]
- 63.Gilbody S, Whitty P, Grimshaw J, et al. Educational and organizational interventions to improve the management of depression in primary care: a systematic review. JAMA. 2003;289:3145–3151. doi: 10.1001/jama.289.23.3145. [DOI] [PubMed] [Google Scholar]
- 64.Hegerl U, Althaus D, Schmidtke A, et al. The alliance against depression: 2-year evaluation of a community-based intervention to reduce suicidality. Psychol Med. 2006;36:1225–1233. doi: 10.1017/S003329170600780X. [DOI] [PubMed] [Google Scholar]
- 65.Szanto K, Kalmar S, Hendin H, et al. A suicide prevention program in a region with a very high suicide rate. Arch Gen Psychiatry. 2007;64:914–920. doi: 10.1001/archpsyc.64.8.914. [DOI] [PubMed] [Google Scholar]
- 66.Goodwin FK, Jamison KR. Manic-depressive illness Bipolar disorders and recurrent depression. 2nd ed. New York (NY): Oxford University Press; 2007. [Google Scholar]
- 67.Marangell LB, Bauer MS, Dennehy EB, et al. Prospective predictors of suicide and suicide attempts in 1,556 patients with bipolar disorders followed for up to 2 years. Bipolar Disord. 2006;8:566–575. doi: 10.1111/j.1399-5618.2006.00369.x. [DOI] [PubMed] [Google Scholar]
- 68.Oquendo MA, Bongiovi-Garcia ME, Galfalvy H, et al. Sex differences in clinical predictors of suicidal acts after major depression: a prospective study. Am J Psychiatry. 2007;164:134–141. doi: 10.1176/appi.ajp.164.1.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Leverich GS, Altshuler LL, Frye MA, et al. Factors associated with suicide attempts in 648 patients with bipolar disorder in the Stanley Foundation Bipolar Network. J Clin Psychiatry. 2003;64:506–515. doi: 10.4088/jcp.v64n0503. [DOI] [PubMed] [Google Scholar]
- 70.Galfalvy H, Oquendo MA, Carballo JJ, et al. Clinical predictors of suicidal acts after major depression in bipolar disorder: a prospective study. Bipolar Disord. 2006;8:586–595. doi: 10.1111/j.1399-5618.2006.00340.x. [DOI] [PubMed] [Google Scholar]
- 71.Romero S, Colom F, Iosif AM, et al. Relevance of family history of suicide in the long-term outcome of bipolar disorders. J Clin Psychiatry. 2007;68:1517–1521. doi: 10.4088/jcp.v68n1007. [DOI] [PubMed] [Google Scholar]
- 72.Dilsaver SC, Chen YW, Swann AC, et al. Suicidality in patients with pure and depressive mania. Am J Psychiatry. 1994;151:1312–1315. doi: 10.1176/ajp.151.9.1312. [DOI] [PubMed] [Google Scholar]
- 73.Goldberg JF, Garno JL, Portera L, et al. Correlates of suicidal ideation in dysphoric mania. J Affect Disord. 1999;56:75–81. doi: 10.1016/s0165-0327(99)00025-7. [DOI] [PubMed] [Google Scholar]
- 74.Balázs J, Benazzi F, Rihmer Z, et al. The close link between suicide attempts and mixed (bipolar) depression: implications for suicide prevention. J Affect Disord. 2006;91:133–138. doi: 10.1016/j.jad.2005.12.049. [DOI] [PubMed] [Google Scholar]
- 75.Akiskal HS, Benazzi F. Delineating depressive mixed states: their therapeutic significance. Clin Approaches Bipolar Disord. 2003;2:41–47. [Google Scholar]
- 76.Akiskal HS, Benazzi F. Psychopathologic correlates of suicidal ideation in major depressive outpatients: is it all due to unrecognized (bipolar) depressive mixed states? Psychopathology. 2005;38:273–280. doi: 10.1159/000088445. [DOI] [PubMed] [Google Scholar]
- 77.Valtonen HM, Suominen K, Mantere O, et al. Suicidal behaviour during different phases of bipolar disorder. J Affect Disord. 2007;97:101–107. doi: 10.1016/j.jad.2006.05.033. [DOI] [PubMed] [Google Scholar]
- 78.Rihmer Z, Akiskal KK, Rihmer A, et al. Current research on affective temperaments. Curr Opin Psychiatry. 2010;23:12–18. doi: 10.1097/YCO.0b013e32833299d4. [DOI] [PubMed] [Google Scholar]
- 79.Azorin JM, Kaladjian A, Besnier N, et al. Suicidal behaviour in a French cohort of major depressive patients: characteristics of attempters and nonattempters. J Affect Disord. 2010;123:87–94. doi: 10.1016/j.jad.2009.09.004. [DOI] [PubMed] [Google Scholar]
- 80.MacKinnon DF, Potash JB, McMahon FJ, et al. National Institutes of Mental Health Bipolar Disorder Genetics Initiative Rapid mood switching and suicidality in familial bipolar disorder. Bipolar Disord. 2005;7:441–448. doi: 10.1111/j.1399-5618.2005.00236.x. [DOI] [PubMed] [Google Scholar]
- 81.Baldessarini RJ, Undurraga J, Vázquez GH, et al. Predominant recurrence polarity among 928 adult international bipolar I disorder patients. Acta Psychiatr Scand. 2012;125:293–302. doi: 10.1111/j.1600-0447.2011.01818.x. [DOI] [PubMed] [Google Scholar]
- 82.Carballo JJ, Harkavy-Friedman J, Burke AK, et al. Family history of suicidal behavior and early traumatic experiences: additive effect on suicidality and course of bipolar illness? J Affect Disord. 2008;109:57–63. doi: 10.1016/j.jad.2007.12.225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sokero P, Eerola M, Rytsälä H, et al. Decline in suicidal ideation among patients with MDD is preceded by decline in depression and hopelessness. J Affect Disord. 2006;95:95–102. doi: 10.1016/j.jad.2006.04.028. [DOI] [PubMed] [Google Scholar]
- 84.Bruce ML, Ten Have TR, Reynolds CF, 3rd, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: a randomized controlled trial. JAMA. 2004;291:1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 85.Zisook S, Lesser IM, Lebowitz B, et al. Effect of antidepressant medication treatment on suicidal ideation and behavior in a randomized trial: an exploratory report from the Combining Medications to Enhance Depression Outcomes Study. J Clin Psychiatry. 2011;72(10):1322–1332. doi: 10.4088/JCP.10m06724. [DOI] [PubMed] [Google Scholar]
- 86.Gibbons RD, Brown CH, Hur K, et al. Suicidal thoughts and behaviour with antidepressant treatment. Reanalysis of randomized placebo-controlled studies of fluoxetine and venlafaxine. Arch Gen Psychiatry. 2012;69(6):580–587. doi: 10.1001/archgenpsychiatry.2011.2048. Epub 2012 Feb 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Mann JJ, Ellis SP, Waternaux CM, et al. Classification trees distinguish suicide attempters in major psychiatric disorders: a model of clinical decision making. J Clin Psychiatry. 2008;69:23–31. doi: 10.4088/jcp.v69n0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Qin P, Nordentoft M. Suicide risk in relation to psychiatric hospitalization: evidence based on longitudinal registers. Arch Gen Psychiatry. 2005;62:427–432. doi: 10.1001/archpsyc.62.4.427. [DOI] [PubMed] [Google Scholar]
- 89.Ösby U, Brandt L, Correia N, et al. Excess mortality in bipolar and unipolar disorder in Sweden. Arch Gen Psychiatry. 2001;58:844–850. doi: 10.1001/archpsyc.58.9.844. [DOI] [PubMed] [Google Scholar]
- 90.Valtonen HM, Suominen K, Haukka J, et al. Differences in incidence of suicide attempts during phases of bipolar I and II disorders. Bipolar Disord. 2008;10:588–596. doi: 10.1111/j.1399-5618.2007.00553.x. [DOI] [PubMed] [Google Scholar]
- 91.Mann JJ. Neurobiology of suicidal behaviour. Nat Rev Neurosci. 2003;4:819–828. doi: 10.1038/nrn1220. [DOI] [PubMed] [Google Scholar]
- 92.Mann JJ, Arango VA, Avenevoli S, et al. Candidate endophenotypes for genetic studies of suicidal behavior. Biol Psychiatry. 2009;65:556–563. doi: 10.1016/j.biopsych.2008.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Nock MK, Hwang I, Sampson N, et al. Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS Med. 2009;6(8):e1000123. doi: 10.1371/journal.pmed.1000123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Swann AC, Dougherty DM, Pazzaglia PJ, et al. Increased impulsivity associated with severity of suicide attempt history in patients with bipolar disorder. Am J Psychiatry. 2005;162:1680–1687. doi: 10.1176/appi.ajp.162.9.1680. [DOI] [PubMed] [Google Scholar]
- 95.Wenzel A, Brown GK, Beck AT. Cognitive therapy for suicidal patients Scientific and clinical applications. Washington (DC): American Psychological Association; 2009. [Google Scholar]
- 96.Brown GK, Ten Have T, Henriques GR, et al. Cognitive therapy for the prevention of suicide attempts: a randomized controlled trial. JAMA. 2005;294:563–570. doi: 10.1001/jama.294.5.563. [DOI] [PubMed] [Google Scholar]
- 97.Turecki G, Ernst C, Jollant F, et al. The neurodevelopmental origins of suicidal behavior. Trends Neurosci. 2012;35:14–23. doi: 10.1016/j.tins.2011.11.008. [DOI] [PubMed] [Google Scholar]
- 98.Jollant F, Bellivier F, Leboyer M, et al. Impaired decision making in suicide attempters. Am J Psychiatry. 2005;162:304–310. doi: 10.1176/appi.ajp.162.2.304. [DOI] [PubMed] [Google Scholar]
- 99.Dombrovski AY, Clark L, Siegle GJ, et al. Reward/punishment reversal learning in older suicide attempters. Am J Psychiatry. 2010;167:699–707. doi: 10.1176/appi.ajp.2009.09030407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Jollant F, Lawrence NL, Olié E, et al. The suicidal mind and brain: a review of neuropsychological and neuroimaging studies. World J Biol Psychiatry. 2011;12:319–339. doi: 10.3109/15622975.2011.556200. [DOI] [PubMed] [Google Scholar]
- 101.Nock MK, Park JM, Finn CT, et al. Measuring the suicidal mind: implicit cognition predicts suicidal behavior. Psychol Sci. 2010;21:511–517. doi: 10.1177/0956797610364762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Disner SG, Beevers CG, Haigh EA, et al. Neural mechanisms of the cognitive model of depression. Nat Rev Neurosci. 2011;12:467–477. doi: 10.1038/nrn3027. [DOI] [PubMed] [Google Scholar]