Abstract
BACKGROUND AND OBJECTIVE:
Health care provider adherence to asthma guidelines is poor. The objective of this study was to assess the effect of interventions to improve health care providers’ adherence to asthma guidelines on health care process and clinical outcomes.
METHODS:
Data sources included Medline, Embase, Cochrane CENTRAL Register of Controlled Trials, Cumulative Index to Nursing and Allied Health Literature, Educational Resources Information Center, PsycINFO, and Research and Development Resource Base in Continuing Medical Education up to July 2012. Paired investigators independently assessed study eligibility. Investigators abstracted data sequentially and independently graded the evidence.
RESULTS:
Sixty-eight eligible studies were classified by intervention: decision support, organizational change, feedback and audit, clinical pharmacy support, education only, quality improvement/pay-for-performance, multicomponent, and information only. Half were randomized trials (n = 35). There was moderate evidence for increased prescriptions of controller medications for decision support, feedback and audit, and clinical pharmacy support and low-grade evidence for organizational change and multicomponent interventions. Moderate evidence supports the use of decision support and clinical pharmacy interventions to increase provision of patient self-education/asthma action plans. Moderate evidence supports use of decision support tools to reduce emergency department visits, and low-grade evidence suggests there is no benefit for this outcome with organizational change, education only, and quality improvement/pay-for-performance.
CONCLUSIONS:
Decision support tools, feedback and audit, and clinical pharmacy support were most likely to improve provider adherence to asthma guidelines, as measured through health care process outcomes. There is a need to evaluate health care provider-targeted interventions with standardized outcomes.
Keywords: asthma, systematic review, guidelines
In the United States, an estimated 24.6 million people (8.2%) currently have asthma,1 resulting in >14 million missed school days every year, and ∼679 000 childhood emergency department (ED) visits.2 Asthma is the third leading cause of pediatric hospitalizations.2
A number of guidelines have been published (eg, the National Asthma Education and Prevention Program Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma, also known as EPR-33), and following guideline treatment recommendations improves clinical outcomes.4–6 However, health care providers do not routinely follow asthma guideline recommendations,7,8 resulting in substandard care and poor health outcomes.9–14
One of the shortcomings of asthma guidelines is the limited extent to which health care providers are provided with tools to follow the recommended care.15 There have been provider-targeted interventions,16–21 but most interventions have been patient-focused.22–25 There is no consensus on the most effective provider-targeted interventions to improve adherence to guidelines.
The objective of our systematic review was to assess whether interventions targeting health care providers improve adherence to asthma care guidelines and subsequently improve outcomes. We considered health care process outcomes, such as patients receiving appropriate treatment, and clinical outcomes, such as hospitalizations.
Methods
We followed the Agency for Healthcare Research and Quality Methods Guide for Effectiveness and Comparative Effectiveness Reviews (available at www.effectivehealthcare.ahrq.gov/methodsguide.cfm). Our protocol and the full report were subject to review.26,27
Data Sources and Searches
We searched Medline, Embase, the Cochrane Central Register of Controlled Trials, Cumulative Index to Nursing and Allied Health Literature, Educational Resources Information Center, PsycINFO, and Research and Development Resource Base in Continuing Medical Education through July 2012. No limits were imposed based on language or date of publication. We also completed backward citation searching by using Scopus for each eligible article.
Study Selection
Search results were screened independently by 2 trained investigators. Disagreements about eligibility were resolved through discussion. We included randomized and nonrandomized studies. We excluded studies that were conducted in inpatient or ED settings only. Potentially eligible articles not in English were identified but not included in the data abstraction and synthesis. We selected the most common outcomes used in practice, those relied on by clinicians to guide decision-making, and those endorsed by the National Institutes of Health Workshop on Asthma Outcomes.28 These critical outcomes are prescription of asthma controller medicines, provision of asthma action plan/self-management education, ED visits/hospitalizations, and missed days of school or work.29
Data Extraction and Quality Assessment
One reviewer completed data abstraction and a second reviewer confirmed accuracy. Reviewers completed risk of bias assessment independently. We resolved disagreements through discussion and, as needed, through consensus among the investigators.
Risk of Bias Assessment
We used the Cochrane Collaboration’s tool for assessing risk of bias.30 For pre-post studies, we added relevant criteria from the Cochrane Effective Practice and Organization of Care checklist.31 Specifically, the questions ask if the intervention was likely to affect data collection and if the intervention was independent of other changes.
Data Synthesis and Analysis
Heterogeneity in the studies, including the measures of outcomes, population included, and specifics of the interventions, precluded quantitative synthesis. Qualitative synthesis was based on these categories of interventions:
decision support interventions are health information technology– and/or paper-based interventions designed to support/facilitate health care provider decision-making;
organizational change interventions are designed to change the way in which an organization provides care (eg, having an asthma “champion”);
feedback and audit interventions provide performance data to health care providers about their quality of care;
clinical pharmacy support interventions target pharmacists’ delivery of care;
education only interventions are focused on educating health care providers about the content of guidelines;
quality improvement/pay-for-performance interventions are focused on quality improvement initiatives or pay-for-performance;
multicomponent interventions use more than 1 type of intervention, with no intervention clearly the predominant intervention;
information-only interventions provide only information to health care providers about guideline recommendations (eg, provide a pocket guide to guidelines).
For studies that used >1 intervention, we determined the predominant intervention. Studies in which this intervention was unclear were discussed among team members to reach consensus. Some studies used multicomponent interventions with no predominant intervention.
We chose magnitudes of effect felt to be clinically meaningful. Magnitude of effect was considered as small (<10% change or difference), moderate (10%–30% change or difference), and large (>30% change or difference).
We graded the strength of evidence (SOE) for each outcome by using the Methods Guide for Conducting Comparative Effectiveness Reviews.32 We considered 4 domains: risk of bias, directness, consistency, and precision. Our judgments were first based on the ability to make a conclusion (if not able to make a conclusion, then “insufficient” was assigned) and then on the confidence in the conclusion (classified as low, moderate, or high with increasing certainty). Investigators graded the evidence, and this was reviewed by the lead author. Any disagreements were discussed with the full team.
For pediatric health care providers, it is pertinent to know if asthma interventions have included children because these patients often have different natural history, developmental considerations, environmental exposures, advocacy concerns as minors, and phenotypes than adults. In terms of provider behavior, there is no distinction in guidelines regarding asthma diagnosis and management. Thus, for this summary, we considered studies of all providers but have noted those described as being conducted in a pediatric population.
Results
Results of Literature Searches
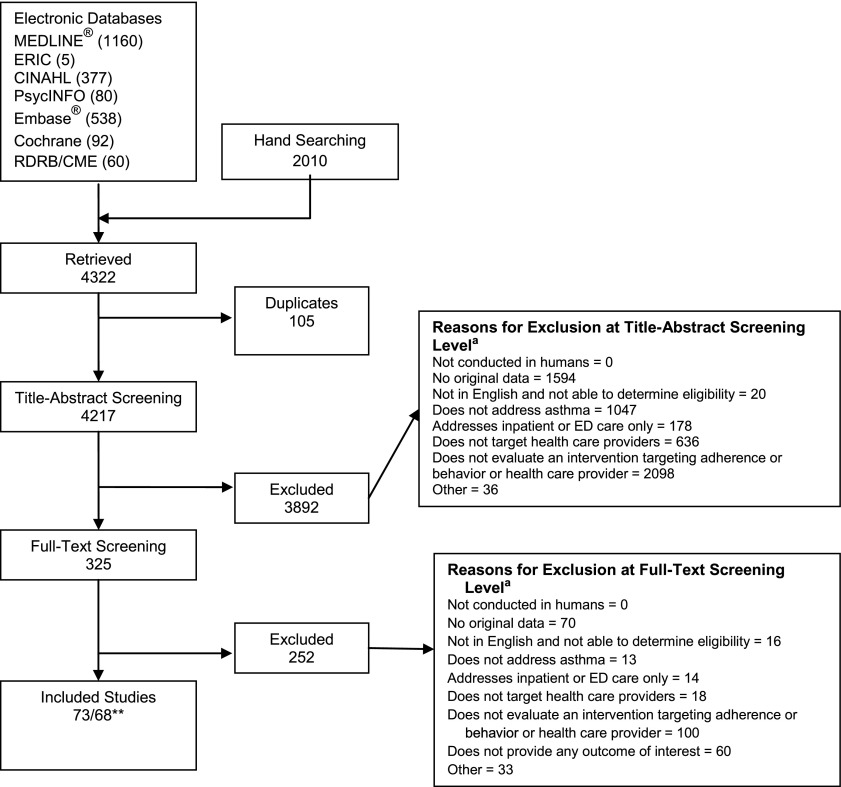
We identified 4217 unique citations of which 68 studies were eligible (Fig 1). We present the evidence addressing health care process outcomes (Table 1) and clinical outcomes (Table 2). Supplemental Tables provide summaries of the evidence by outcome. Twenty-five of the 68 studies were conducted in pediatric-only populations. The tables indicate if the patient population included children only, adults only, a mixture of children and adults, or if the patient population is unknown.
FIGURE 1.
Summary of search (number of articles). ERIC, Educational Resources Information Center; RDRB/CME, Research and Development Resource Base in Continuing Medical Education. * Total exceeds the number in the exclusion box because reviewers did not need to agree on reason for exclusion. ** Three distinct pairs of articles described a single intervention or cohort. For the purposes of this review, each pair was counted as a single study, yielding 68 studies reported in 73 articles.
TABLE 1.
Characteristics of Studies Addressing Health Care Process Outcomes
| Intervention | Author, y | Patient Population | Study Design | Type of Provider | No. of Providers | No. of Patients | Health Care Process Outcomes | |
|---|---|---|---|---|---|---|---|---|
| Prescription for Controller Medicines | Self-management Education/Asthma Action Plan | |||||||
| Clinical pharmacy support | De Vries, 201034 | Pediatrics | Nonrandomized pre-post | Arm A: general practitioner; Arm B: general practitioner, pharmacists; Arm C: general practitioner, pharmacists, pediatrician | 9 | Arm A (control): 3527; Arm B (feedback): 1447 | ↑ | N/A |
| Armour, 200733 | Adults | RCT | Pharmacist | Arm A (control): 25; Arm B (PACP): 32 | Arm A (control): 186; Arm B (PACP): 165 | ↑ | ↑ | |
| Saini, 200435 | Not specified | Pre-post | Arm A: general practitioner, pharmacist; Arm B: pharmacist; Arm C: pharmacist | Arm A (control 1): 13; Arm B (control 2): 12; Arm C (education): NR | Arm A (control 1): 22; Arm B (control 2): 28; Arm C (education): 52 | ↑ | N/A | |
| Decision Support | Bell, 201047 | Pediatrics | RCT | Pediatrician | NR | Arm A (UP control): 5192; Arm B (UP intervention): 5040; Arm C (SP control): 3843; Arm D (UP control): 5375 | ↑ | ∅ |
| Cloutier, 200539 | Pediatrics | Pre-post | Nurse, nurse practitioner, pediatrician, physician assistant, primary health care pediatric residents, medical students | 151 | 3748 | ↑ | N/A | |
| Fairall, 201049 | Pediatrics | RCT | Nurse | 148 | Arm B (intervention): 1000 | ↑ | N/A | |
| Halterman, 200681 | Pediatrics | RCT | Nurse practitioner, pediatrician, physician | NR | Arm A (control): 124; Arm B (intervention): 122 | N/A | ↑ | |
| Lesho, 200538 | Pediatrics | Pre-post | Primary health care | NR | 330 | ∅ | ↑ | |
| Rance, 201141 | Pediatrics | Pre-post | Nurse practitioner, pediatrician | 4 | 41 | ↑ | N/A | |
| Shapiro, 201142 | Pediatrics | Pre-post | Nurse, physician | 25 | Arm B (SBHC): 200; Arm C (NYCHP): 197 | ↑ | N/A | |
| Shiffman, 200046 | Pediatrics | Pre-post | Pediatrician | 11 | Arm A (sole physician arm; patient arm, pre): 91; Arm B (patient arm): 74 | ∅ | N/A | |
| To, 200885 | Mixed (2–55 y) | Pre-post | Primary health care | NR | 1408 | N/A | ↑ | |
| Cho, 201043 | Adults | Pre-post | Allergist, general practitioner, physician | 377 | 2042 | ↑ | N/A | |
| Eccles M, 200245 | Adults | RCT | General practitioner | NR | Arm A (angina): 4851; Arm B (asthma): 4960 | ∅ | ∅ | |
| Cloutier, 200240 | Not specified | Pre-post | Nurse, nurse practitioner, other, pediatrician, physician, physician assistant advanced practice nurses, family practice | 172 | 860 | ↑ | N/A | |
| Davis, 201048 | Not specified | Pre-post | Physician family medicine residents | NR | 180 | ↑ | N/A | |
| Horswell, 200836 | Not specified | Pre-post | Physician | NR | NR | ↑ | ↑ | |
| Kattan, 20065 | Not specified | RCT | Nurse practitioner, physician assistant, primary health care | Arm A (standard practice): NR; Arm B (decision support): 435 | Arm A (standard practice): 466; Arm B (decision support): 471 | ↑ | N/A | |
| Martens, 200744 | Not specified | RCT | General practitioner | Arm A (Control): 54; Arm B (Guidelines and involved in development): 53 | Arm A: 24 160; Arm B: 35 748 | ∅ | N/A | |
| McCowan, 200182 | Not specified | RCT | General practitioner | NR | Arm A (control): 330; Arm B (decision support): 147 | N/A | ∅ | |
| Mitchell, 200537 | Not specified | RCT | General practitioner | 270 | NR | ∅ | N/A | |
| Newton, 201084 | Not specified | Pre-post | Nurse, physician practice managers, other staff | NR | NR | N/A | ↑ | |
| Ruoff, 200219 | Not specified | Pre-post | Family physicians | Arm A: 17; Arm B: 17 | Arm A: 122; Arm B: 122 | N/A | ↑ | |
| Ragazzi, 201083 | Not specified | Pre-post | Nurse, pediatrician | 26–28 | NR | N/A | ↑ | |
| Education only | Davis, 200457 | Pediatrics | Pre-post | Primary health care | 20 | NR | ↑ | N/A |
| Blackstien-Hirsch, 200058 | Pediatrics | Pre-post | Physician | 59 | 195 | ∅ | N/A | |
| Shah, 201150 | Pediatrics | RCT | General practitioner | 150 | Arm A (control):107 Arm B (PACE):110 | ↑ | ↑ | |
| Brown R, 200418 | Pediatrics | RCT | Pediatrician | Arm A (Control): 11; Arm B (Education): 12 | Arm A (control): 122; Arm B (education): 157 | ∅ | ∅ | |
| Clark, 199852 | Pediatrics | RCT | Pediatrician, physician | Arm A (control): 37; Arm B (education):37 | 637 | ↑ | ↑ | |
| Stergachis, 200253 | Pediatrics | RCT | Pharmacist | Arm A (control): NR; Arm B (education): 35 | Arm A (control): 177; Arm B (education): 153 | ∅ | N/A | |
| Sulaiman, 201087 | Pediatrics | RCT | General practitioner | Arm A (control): 18; Arm B (education and guidelines): 18; Arm C (guidelines): 15 | Arm A (control): 121; Arm B (education and guidelines): 156; Arm C (guidelines): 134 | N/A | ∅ | |
| Premaratne, 199954 | Mixed (15–50 y) | RCT | Nurse practice nurses | NR | Arm A (control): 14 410; Arm B (education): 9900 | ∅ | N/A | |
| Holton, 201186 | Adults | RCT | General practitioner | Arm A (control): 45; Arm B (spirometry training): 127 | Arm A (control): 157; Arm B (spirometry training): 240 | N/A | ∅ | |
| Smeele, 199951 | Adults | RCT | General practitioner | Arm A (control): 17; Arm B (education): 17 | Arm A (control): 223; Arm B (education): 210 | ∅ | N/A | |
| Cowie, 200156 | Not specified | Pre-post | NR | NR | Arm A (basic education): NR; Arm B (intermediate education): NR; Arm C (intensive education): NR | ∅ | N/A | |
| Mahi-Taright, 200455 | Not specified | Pre-post | General practitioner | 50 | 49 | ∅ | N/A | |
| Feedback and audit | Schneider A., 200867 | Mixed | RCT | General practitioner | 96 | Arm A (traditional quality circle): NR; Arm B (benchmark quality circle): NR; Arm C (combined arms): 256 | ∅ | ↑ |
| Suh, 200165 | Mixed (4–55 y) | Pre-post | NR | NR | Arm A (intermittent asthma): 566; Arm B (persistent asthma): 1050 | ↑ | N/A | |
| Sondergaard, 200269 | Mixed (6–45 y) | RCT | General practitioner | Arm A (control): 141; Arm B (individual patient count data feedback): 77; Arm C (aggregate data feedback): 74 | 6437 | ∅ | N/A | |
| Veninga, 199959 | Adults | RCT | General practitioner | Arm A (Netherlands): 181; Arm B (Sweden): 204; Arm C (Norway): 199; Arm D (Slovakia): 81 | NR | ↑ | N/A | |
| Feder, 199560 | Adults | RCT | General practitioner | NR | Arm A (diabetes education): NR; Arm B (education, reminders and audit): NR | ↑ | ↑ | |
| Veninga, 200061 | Adults | RCT | General practitioner | Arm A (UTI): 91; Arm B (education and feedback):90 | Arm A (UTI): NR; Arm B (education and feedback): NR | ↑ | N/A | |
| Baker, 200366 | Not specified | RCT | General practitioner | Arm A (guidelines only): 27; Arm B (guidelines with audit criteria): 27; Arm C (guidelines with audit criteria and feedback): 27 | Arm A (guidelines only): 483; Arm B (guidelines with audit criteria): 510; Arm C (guidelines with audit criteria and feedback): 489 | ↑ | ∅ | |
| Coleman, 200363 | Not specified | Pre-post | Pharmacist prescriber | NR | Arm A (patient specific information: prescribers with patients on “high dose”): 510; Arm B (patient-specific information: prescribers with patients on “low dose”): 135 | ∅ | ↑ | |
| Richman, 200064 | Not specified | Pre-post | Pediatrician | 29 | 228 | No statistical testing of results for this outcome | ↑ | |
| Herborg, 200168 | Not specified | Non-RCT | General practitioner, other, pharmacist pharmacy assistant | Arm A (control): 64; Arm B (TOM): 75 | NR | ↑ | N/A | |
| Hoskins, 199762 | Not specified | Pre-post | General practitioner | 91 | Before intervention: 782; Education and feedback intervention: 669 | Unable to discriminate what component of multifaceted intervention was effective | N/A | |
| Information only | Bryce, 199571 | Pediatrics | RCT | General practitioner, nurse | NR | Arm A (control): 1563; Arm B (reminders and tools):1585 | ∅ | N/A |
| Martens, 200670 | Not specified | RCT | General practitioner | Arm A (control): 54; Arm B (guidelines and involved in development): 53; Arm C (guidelines only): 26 | NR | ↓ | N/A | |
| Multi-component | Hagmolen, 200872 | Pediatrics | RCT | General practitioner | Arm A (guidelines only): 34; Arm B (education and guidelines): 34; Arm C (education and guidelines and individualized treatment advice): 38 | Arm A (guidelines only): 98; Arm B (education and guidelines): 133; Arm C (education and guidelines and individualized treatment advice): 131 | ↑ | N/A |
| Frankowski, 200688 | Pediatrics | Pre-post | Nurse, pediatrician, primary health care | NR | Education and feedback: 150 | N/A | ↑ | |
| Lob, 201178 | Pediatrics | Pre-post | Physician, nurse practitioner | NR | Longitudinal evaluation group, patient-level interview: 761 | ↓ | ↓ | |
| Cross-sectional random sample, clinic-level chart review, time 1: 680; Cross-sectional random sample, clinic-level chart review, time 2: 680; Cross-sectional random sample, clinic-level chart review, time 3: 680 | ||||||||
| Cloutier, 201275 | Adults | RCT | Nurse practitioner, pediatrician, physician assistant | Arm A (control): 44; Arm B (physician-directed interventions): 44 | NR | ∅ | ∅ | |
| Daniels, 200573 | Not specified | RCT | General practitioner, internist, nurse practitioner, pediatrician, physician, physician assistant staff | 163 | Arm A (control): 136 079; Arm B (education): 90 555 | ∅ | ∅ | |
| Lundborg, 199974 | Not specified | RCT | General practitioner | Arm A (control): 104; Arm B (education and feedback): 100 | Arm A (control): 1333; Arm B (education and feedback): 1121 | ∅ | N/A | |
| Yawn, 200877 | Not specified | Pre-post | Nurse practitioner, physician, physician assistant | Education and feedback: 211 | Education and feedback: 840 | ↑ | ↑ | |
| Bender, 201176 | Not specified | Pre-post | Nurse, physician, physician assistant medical assistants, practice managers, office staff | 372 | 15 508 | ↑ | ↑ | |
| Organizational change | Finkelstein, 200579 | Pediatrics | RCT | Pediatric medical provider | 228 | Arm A (control): 1531; Arm B (PLE intervention): 2003; Arm C (planned care intervention): 1635 | ∅ | N/A |
| Glasgow, 200389 | Pediatrics | RCT | General practitioner | Arm A (control): 12; Arm B (intervention): 12 | Arm A (control):73; Arm B (intervention):101 | N/A | ↑ | |
| Patel, 200490 | Mixed (4–55 y) | Pre-post | Physicians, nurses | NR | 451 | N/A | ↑ | |
| Thyne, 200780 | Not specified | Pre-post | “Pediatric medical providers,” “urgent care clinicians” | NR | Arm A (time 1, 2002–2003): NR; Arm B (time 2, 2003–2004): NR; Arm C (time 3, 2004–2005): NR | ↑ | N/A | |
| Quality improvement | Fox, 200792 | Pediatrics | Pre-post | Nurse, nurse practitioner, physician caregivers, administrative staff | NR | Chart review sample: 280; Interview sample: 405 | N/A | ↑ |
| Homer, 200591 | Pediatrics | RCT | Nurse, physician front office staff | NR | Arm A (control): 337; Arm B (learning collaborative): 294 | N/A | ∅ | |
| Mangione-Smith, 200593 | Not specified | Pre-post | “Health care providers” | NR | Arm A (control): 126; Arm B (learning collaborative): 385 | N/A | ↑ | |
NR, not reported; NYCHP, New York Children’s Health Project; PACE, Physician Asthma Care Education; PACP, Pharmacy Asthma Care Program; PLE, Peer Leader Education; SBHC, South Bronx Health Center; SP, suburban practice; TOM, therapeutic outcomes monitoring; UP, urban practice; UTI, urinary tract infection. ↑, Statistically significant increase in outcome of interest. ↓, Statistically significant decrease in outcome of interest. ∅, Difference between intervention and control groups or between pre- and postintervention not statistically significant.
TABLE 2.
Characteristics of Studies Addressing Clinical Outcomes
| Intervention | Author, y | Patient Population | Study Design | Type of Provider | No. of Providers | No. of Patients | Clinical Outcomes | |
|---|---|---|---|---|---|---|---|---|
| ED Visits/Hospitalization | Missed Days of School/Work | |||||||
| Clinical pharmacy support | Weinberger, 200294 | Adults | RCT | Pharmacist | NR | Arm A (control): 165; Arm B (peak flow meter monitoring control group): 233 | ∅ | N/A |
| Decision support | Lesho, 200538 | Pediatrics | Pre-post | Primary health care | NR | 330 | ↓ | N/A |
| Shiffman, 200046 | Pediatrics | Pre-post | Pediatrician | 11 | Arm A (sole physician arm; patient arm, pre): 91; Arm B (patient arm): 74 | ↓ | N/A | |
| To, 200885 | Mixed (2–55 y) | Pre-post | Primary health care | NR | 1408 | ↓ | ↓ | |
| Cloutier, 200996 | Not specified | Pre-post | Pediatrician | NR | 3298 | ↓ | N/A | |
| Horswell, 200836 | Not specified | Pre-post | Physician | NR | NR | ↓ | N/A | |
| Kattan, 20065 | Not specified | RCT | Nurse practitioner, physician assistant, primary health care | Arm A (standard practice): NR; Arm B (decision support): 435 | Arm A (standard practice): 466; Arm B (decision support): 471 | ↓ | ∅ | |
| McCowan, 200182 | Not specified | RCT | General practitioner | NR | Arm A (control): 330; Arm B (decision support): 147 | ∅ | N/A | |
| Mitchell, 200537 | Not specified | RCT | General practitioner | 270 | NR | ↓ | N/A | |
| Newton, 201084 | Not specified | Pre-post | Nurse, physician practice managers, other staff | NR | NR | ↓ | N/A | |
| Renzi, 200695 | Not specified | RCT | Primary health care | NR | NR | ↓ | N/A | |
| Education only | Blackstien-Hirsch, 200058 | Pediatrics | Pre-post | Physician | 59 | 195 | ∅ | N/A |
| Brown, 200418 | Pediatrics | RCT | Pediatrician | Arm A (control): 11; Arm B (education): 12 | Arm A (control): 122; Arm B (education): 157 | ↓a | ∅ | |
| Clark, 199852 | Pediatrics | RCT | Pediatrician, physician | Arm A (control): 37; Arm B (education): 37 | 637 | ∅ | N/A | |
| Stergachis, 200253 | Pediatrics | RCT | Pharmacist | Arm A (control): NR; Arm B (education): 35 | Arm A (control): 177; Arm B (education): 153 | ∅ | ∅ | |
| Sulaiman, 201087 | Pediatrics | RCT | General practitioner | Arm A (control): 18; Arm B (education and guidelines): 18; Arm C (guidelines): 15 | Arm A (control): 121; Arm B (education and guidelines): 156; Arm C (guidelines): 134 | ∅ | N/A | |
| Cabana, 200617 | Pediatrics | RCT | Primary health care | Arm A (control): 43; Arm B (PACE): 51 | Arm A (control): 452; Arm B (PACE): 418 | ∅ | N/A | |
| Shah, 201150 | Pediatrics | RCT | General practitioner | 150 | Arm A (control): 107; Arm B (PACE): 110 | N/A | ∅ | |
| Holton, 201186 | Adults | RCT | General practitioner | Arm A (control): 45; Arm B (spirometry training): 127 | Arm A (control): 157; Arm B (spirometry training): 240 | N/A | ∅ | |
| Cowie, 200156 | Not specified | Pre-post | NR | NR | Arm A (basic education): NR; Arm (intermediate education): NR; Arm C (intensive education): NR | ∅ | ∅ | |
| Feedback and audit | Schneider, 200867 | Mixed | RCT | General practitioner | 96 | Arm A (traditional quality circle): NR; Arm B (benchmark quality circle): NR; Arm C (combined arms): 256 | ∅ | N/A |
| Richman, 200064 | Not specified | Pre-post | Pediatrician | 29 | 228 | ∅ | ∅ | |
| Information only | Bryce, 199571 | Pediatrics | RCT | General practitioner, nurse | NR | Arm A (control): 1563; Arm B (reminders and tools): 1585 | ∅ | N/A |
| Multicomponent | Lob, 201178 | Pediatrics | Pre-post | Physician, nurse practitioner | NR | Longitudinal evaluation group, patient-level interview: 761; Cross-sectional random sample, clinic-level chart review, time 1: 680; Cross-sectional random sample, clinic-level chart review, time 2: 680; Cross-sectional random sample, clinic-level chart review, time 3: 680 | ↓ | ↓ |
| Organizational change | Finkelstein, 200579 | Pediatrics | RCT | Pediatric medical provider | 228 | Arm A (control): 1531; Arm B (PLE intervention): 2003; Arm C (planned care intervention): 1635 | ∅ | N/A |
| Glasgow, 200389 | Pediatrics | RCT | General practitioner | Arm A (control): 12; Arm B (intervention): 12 | Arm A (control): 73; Arm B (intervention): 101 | ∅ | ∅ | |
| Patel, 200490 | Mixed (4–55 y) | Pre-post | Physicians, nurses | NR | 451 | ↓ | N/A | |
| Thyne, 200780 | Not specified | Pre-post | “Pediatric medical providers,” “urgent care clinicians” | NR | Arm A (time 1, 2002–2003): NR; Arm B (time 2, 2003–2004): NR; Arm C (time 3, 2004–2005): NR | ↓b | N/A | |
| Quality improvement | Homer, 200591 | Pediatrics | RCT | Nurse, physician front office staff | NR | Arm A (control): 337; Arm B (learning collaborative): 294 | ∅ | N/A |
| Mangione-Smith R., 200593 | Not specified | Pre-post | “Health care providers” | NR | Arm A (control): 126; Arm B (learning collaborative): 385 | ∅ | ∅ | |
NR, not reported; PACE, Physician Asthma Care Education; PLE, Peer Leader Education. ↑, Statistically significant increase in outcome of interest. ↓, Statistically significant decrease in outcome of interest. ∅, Difference between intervention and control groups, or between pre- and post-intervention not statistically significant.
Reduction in ED visit for subgroup of low-income participants only but reduction in annual rate of hospitalization for entire group.
Reduction in ED visit but P value not reported in study.
Outcome: Prescription of Controller Medicines
Clinical Pharmacy Support
We identified 3 studies.33–35 In a randomized controlled trial (RCT), pharmacists trained in risk assessment, medication adherence, and spirometry reported increased dispensation of asthma controller medicines (odds ratio [OR]: 3.80; 95% confidence interval [CI]: 1.40–10.32; P = .01).33 In 2 non-RCTs,34,35 clinical pharmacy support increased controller medication prescribing by 20%35 and 6%34 (P < .05 for both studies). In the controlled pre-post study, the intervention was a specialized asthma service provided by community pharmacies: patient appointments, assessment and intervention of patient medication needs, and goal-setting with the patient.35 In the latter study, pharmacists were encouraged to meet with local practitioners to discuss pediatric asthma care guidelines.34
SOE: moderate.
Decision Support
Fifteen studies were identified that included the provision of asthma guidelines in a more accessible format (eg, “pocket” versions),36–38 use of a specific algorithm, pathway, or flow sheet,37–40 a structured template for taking a history,41,42 a reminder system to raise awareness about the patient’s asthma status,5,43,44 and computer systems.36,43–48 Ten of the studies reported significantly increased prescribing of asthma controller medicines,5,36,39–43,47–49 from 2% to 34%, and 5 reported no statistically significant effect.37,38,44–46
SOE: moderate.
Education Only
The 10 education-only interventions we identified18,50–58 included small-group asthma education programs,51 structured training,58 seminars,52 and grand rounds.58 Certain interventions also emphasized more general skills, such as training in communication.50,52 The studies reported increased prescribing of 3.5% to 50.3%, although statistically significant increases were reported only in 3 of the studies.
SOE: low.
Feedback and Audit
We identified 11 studies; most assessed a multifaceted intervention combined with provider education,59–65 prioritized review criteria for audit,66 benchmarking (comparison with peers or other practices),66,67 or pharmacy monitoring of fill data and feedback.68,69
Increased prescribing of asthma controller medicines was reported for RCTs using (1) targeted key guideline messages (eg, “use inhaled corticosteroids [ICS] promptly”; 5%–12% increase, P = .05),59 (2) prioritized guideline review criteria on a card,66 (3) prompts for annual review of asthma management,60 or (4) individualized feedback on prescribing and decision strategies.61 The 2 RCTs reporting no effect on prescribing of asthma controller medications involved mailed feedback of prescribing data69 and a trial of performance feedback (a “benchmark” group, whose prescribing behavior was compared with a performance benchmark or with other prescribers, versus a traditional or individual feedback group, which did not receive comparison with other prescribers).67 The observed effects between 3 groups (guidelines alone, prioritized guideline review criteria, and review criteria plus feedback on actual prescribing behavior) was a 15.9% increase in controller prescribing in the review criteria plus feedback group, compared with an 11% increase in the review criteria only and no change (0%) in the guideline only group.66 A positive but nonsignificant 2.7% difference (95% CI: –14.4 to 19.7) was noted in the proportion of patients in practices with asthma “prophylaxis” compared with practices provided with diabetes guidelines.60
Three of 5 pre-post studies reported increased prescribing of controller medications (52%–104%): change in prescribing over time (52%), a 104.4% in patients with intermittent asthma but a decrease by 10.8% in patients with persistent asthma.
SOE: moderate.
Information Only
Two RCTs were assessed information only.70,71 One study, which randomized patients to have asthma management information and treatment guidelines inserted into their medical records for provider use, reported no benefit.71 The second study randomly selected providers to participate in developing local asthma guidelines mailed to providers in both intervention and comparison groups.70 Intervention providers wrote 8 fewer prescriptions per 1000 patients (P < .01).
SOE: insufficient.
Multicomponent
We identified 7 studies of multicomponent interventions.72–78 All interventions included information, education, and at least 2 of the following: organizational change, decision support, and feedback and audit. Two of the 3 pre-post studies reported 25% to 49% increases in prescribing rates.76,77 Three of the 4 RCTs reported no statistically significant effects.
SOE: low.
Organizational Change
The 2 studies of organizational change focused on pediatric providers.79,80 An RCT assessed the use of an asthma nurse educator,79 and the pre-post study evaluated use of a community health worker.80 The RCT reported no significant increase in prescriptions for ICS or asthma controller medications (4%–16%).79 In the pre-post study, investigators observed a 12% increase in ICS prescriptions (no P value reported).80
SOE: low.
Quality Improvement and Pay-for-Performance
No studies were identified.
SOE: insufficient.
Outcome: Self-Management Education and Asthma Action Plans
Clinical Pharmacy Support
We identified 1 RCT in which patients of pharmacists in the Pharmacy Asthma Care Program had increased asthma action plan possession (40.4%; 95% CI: 31.9–48.9; P < .001); however, there are no data for the control group.33
SOE: moderate.
Decision Support
We identified 10 studies19,36,38,45,47,81–85 that included computerized support,36,45,47,82,84 a flow sheet/algorithm,19,85 and/or the provision of guidelines.38 Two of the 3 studies focused on pediatricians.81,83 Seven studies reported statistically significant increase in the provision of patient education/asthma action plans of 14% to 84% (all reported as statistically significant).19,36,38,81,83–85 Three of the 4 RCTs reported no significant difference.45,47,82
SOE: moderate.
Education Only
Of the 5 RCTs of education-only interventions,18,50,52,86,87 1 focused on pediatricians and used small-group asthma education programs, structured training, and interactive seminars. Two studies increased use of asthma action plans by 10% (P = .03)52 and 15% (P = .046).50 The other 3 studies reported no increase.18,86,87
SOE: low.
Feedback and Audit
Five studies evaluated feedback and audit.60,63,64,66,67 Significant increases in provision of self-management education/asthma action plans (1%–40%) were reported in 4 studies.60,63,64,67 For peak flow meter use, one study reported a 3.6% decrease, while a second study reported a minimal increase of 0.7% (95% CI: –15.2 to 16.7) after practices received asthma guidelines.60 A moderate increase was noted for inhaler technique, 12.9% (95% CI: 1.9 to 23.9),51 and a small increase in change of asthma action plan use (7.6%) in a benchmarking feedback group.67
SOE: low.
Information Only
No studies were identified.
SOE: insufficient.
Multicomponent
Of the 6 studies we reviewed,73,75–78,88 most included an educational component but also included (1) training in communication techniques with provision of a spirometer and training in use of the spirometer76; (2) laminated posters of guidelines and medications with feedback on asthma action plan use and monthly calls from an intervention team to troubleshoot communication problems88; (3) asthma kits (peak flow meters, spacers, educational materials) and systems-level changes (flow sheets and standing medication orders)73; (4) systematic use of a patient questionnaire and an asthma management algorithm77; (5) an asthma coordinator and feedback on performance as part of continuous quality improvement efforts; or (6) an educational toolbox with seminars, teleconferences, mini fellowships, opinion leader visits, clinician-specific feedback, and pay for performance.75 The pre-post studies reported increases in the provision of action plans (27%–46%).76–78,88 Both RCTs reported nonsignificant increases in patient education/asthma action plans (7% in 1 study; relative risk = 1.82 in the other study).73,75
SOE: low.
Organizational Change
We identified 2 studies.89,90 A pre-post study (instituting a registry to track asthma patients and an asthma case manager) reported a 10% increase in patient education (P < .001) and a 14% increase in asthma action plan dispensations (P < .001).90 In the RCT (a restructured clinical protocol for how asthma patients are cared for during ambulatory care encounters; “3+ visit plan”), there was a 10% increase in the provision of asthma education (P = .01).89
SOE: low.
Quality Improvement and Pay-for-Performance
Three studies, each including pediatric health care providers, were identified.91–93 Two studies assessed participation in a Breakthrough Series Collaborative,91,93 and 1 study assessed a combination of continuous quality improvement and the addition of a community health worker.92 One of these studies showed a difference of 33% in the intervention arm.93 Two of the 3 studies showed a 28% to 32% increase in the proportion of patients who had received an asthma action plan.92,93 These 2 studies enrolled practices that had already joined a quality improvement initiative93 or were part of a demonstration project.92
The RCT showed no significant effect, with a 3% lower rate for the intervention versus control group.91 However, there were decreases in participation and in outcome reporting over time. In the controlled pre-post study, documented self-management education increased by 21%.93
SOE: low.
Outcome: ED Visits/Hospitalizations
Clinical Pharmacy Support
In an RCT, pharmacists were provided with patient specific clinical data, training about asthma management, patient educational materials, resource guides, and pragmatic strategies.94 Patients of intervention pharmacists were more likely to have a reduction in ED visits/hospitalizations compared with patients seen by pharmacists who received peak flowmeter instruction only (OR: 2.16; 95% CI: 1.76–2.63) but not compared with patients of the usual care control group (OR 1.08; 95% CI: 0.93–1.25).94
SOE: insufficient.
Decision Support
For the 10 studies addressing this outcome,5,36–38,46,82,84,85,95,96 decision support interventions included computer systems,36,46,82,84 checklists,95 supplemental feedback protocols,5 and structured pathways/algorithms.37,96 Several studies included children.5,37,46,85,96
Nine studies reported a reduction in ED visits or hospitalizations5,36–38,46,84,85,95,96 (5%–60%) among pre-post studies (all statistically significant) and 1% to 7% among the RCTs.5,37,95
SOE: moderate.
Education Only
We identified 7 studies17,18,52,53,56,58,87 involving interactive seminars, structured training, and medical grand rounds. One study reported statistically significant reduction in ED visits (only in a subgroup of low-income participants; –1.23 visits per year, P = .001) and in the overall annual hospitalization rate.18
SOE: low.
Feedback and Audit
We identified 2 studies: (1) an RCT of a traditional quality circle intervention of provider feedback on individual performance and the aggregate performance of the provider group was compared with a benchmark quality circle intervention (feedback on providers’ individual performance was explicitly compared with a performance benchmark)67; and (2) a pre-post study comparing individual providers’ practice patterns with their peers plus providing asthma education to office staff.64 Patients in the benchmark quality circle had a 6.7-point decrease in ED visits, although patients in the traditional quality circle intervention had a 12.2-point decrease (P = .064).67
No significant change in ED visits (1% decrease) or hospitalizations (2% decrease) was reported in the pre-post study.64
SOE: insufficient.
Information Only
The 1 study identified randomized patients to have information about asthma guidelines inserted in their medical records for provider use; each provider thus managed patients in both intervention and control arms simultaneously.71 No differences in rates of ED visits or hospitalizations were observed between intervention and control arms of the study.
SOE: insufficient.
Multicomponent
One study included quality improvement, decision support, organizational change, and feedback-and-audit.78 This study reported a 69% reduction in ED visits and hospitalizations. However, 44% of the patient sample was lost to follow-up, and significant heterogeneity in results was seen across participating sites.
SOE: insufficient.
Organizational Change
We identified 4 studies,79,80,89,90 which included restructured asthma care visits,89 supplemental trained personnel, and provider education.79,80,90 Three studies focused on pediatric providers.79,80,89
Only 1 of 4 studies, a pre-post study, reported a significant reduction in ED visits: a 41% reduction in ED visits and 54% reduction in hospitalizations (P < .001 for both).90 The other pre-post study reported a 4% reduction in hospitalizations (no P value reported).80 The 2 RCTs reported 1% (P > .05)79 and 7% (P = .06)89 reductions.
SOE: low.
Quality Improvement and Pay-for-Performance
One RCT91 and 1 controlled pre-post study93 evaluated a Breakthrough Series Collaborative quality improvement strategy among pediatric providers in community health centers. Neither study showed a significant reduction in either outcome. However, in the RCT, when analyses were limited to the 9 practices that attended all 3 learning sessions, significant reductions in ED visits were reported.91
SOE: low.
Outcome: Missed Days of Work/School
Clinical Pharmacy Support
No studies identified.
SOE: insufficient.
Decision Support
An RCT reported no reduction in missed school (0.05 days; P = .4) after mailing patient-specific asthma morbidity information to their health care provider.5 A pre-post study reported a 49% reduction (P < .001) in school absenteeism and a 51% reduction in the odds of missed work (OR: 0.49; 95% CI: 0.34–0.71) after using an asthma care map, a treatment flowchart, program standards, management flowchart, and action plan.85 Both studies were conducted in a pediatric population.
SOE: insufficient.
Education Only
Five studies evaluated the effect of provider education on missed school or missed work.18,50,53,56,86 Three RCTs used structured training, seminars, and workshops for health care providers to examine the effects on missed school. They reported small but statistically nonsignificant reductions in missed school (0.6–4 days). To evaluate the impact on missed work, 2 RCTs50,86 and 1 pre-post study56 provided workshops and training in how to perform spirometry, and 1 study compared asthma program development with a nurse educator program to continuing education. All studies reported small, statistically nonsignificant reductions in missed school or work.
SOE: insufficient.
Feedback and Audit
We identified 1 pre-post study that provided asthma education to office staff and observed an 11% reduction in school days missed and a 0% reduction in parent workdays missed.64
SOE: insufficient.
Information Only
No studies were reviewed.
SOE: insufficient.
Multicomponent
One study implemented decision support, organizational change, and feedback and audit. This study found significant reductions in missed days of school (53%) and work (72%). However, 44% of the patient sample was lost to follow-up, and significant heterogeneity in results was reported.78
SOE: insufficient.
Organizational Change
One RCT of organizational change based on restructuring the clinical protocol for patient care during ambulatory care encounters (“3+ visit plan”)89 did not reduce missed school days (OR: 0.8; 95% CI: 0.5–1.2; P = .3).
SOE: low.
Quality Improvement and Pay-for-Performance
One controlled pre-post study reported that patients of providers participating in the Breakthrough Series Collaborative quality improvement strategy showed no significant reduction in the mean number of school days or parental workdays missed.93
SOE: insufficient.
Discussion
Of the 68 studies we identified, a minority of studies focused on pediatric health care providers or involved children (14 studies assessing clinical outcomes; 24 studies assessing health care process outcomes). We acknowledge that there are a number of ways in which providing care for children is different from providing care for adults: (1) physiology; (2) disease presentation, natural history, and morbidity; (3) the need to consider congenital, genetic, and developmental issues; and (4) support structure, including that children are minors so parents are a necessary element to any medical decision-making process. However, there are a few reasons that findings of provider-targeted asthma interventions should be applicable across the health care provider spectrum: (1) asthma guideline recommendations generally do not distinguish different types of providers; (2) a number of provider behaviors in asthma care are universal (eg, assessing asthma control/severity; prescribing controller medications for persistent asthma; providing self-management education); (3) the goals for patient outcomes are the same (eg, reducing acute care visits for exacerbations; limiting missed school/work); and (4) the mainstay treatment options are the same (eg, inhaled steroids and short-acting bronchodilators). Therefore, for pediatricians, as with other providers, it is reasonable that the decision to choose and implement a given intervention to improve their adherence to asthma guidelines be based on (1) the data on the effectiveness of the intervention, (2) the feasibility of implementing the intervention within their own practice setting, and (3) the sustainability of the intervention. There is always a need for pediatric-focused studies, but we believe that the findings of our review may provide lessons for all providers.
Decision support, feedback/audit, and education only were the most common interventions and were tested for each of the outcomes we evaluated. Conversely, organizational change, clinical pharmacy support, quality improvement/pay-for-performance, information only, and multicomponent strategies were less consistently tested (see Table 3). Evidence suggests that some of the interventions are not effective in achieving specific outcomes: education to increase prescribing of asthma controller medications or to reduce ED visits/hospitalizations; organizational change to reduce ED visits/hospitalizations or to reduce missed days of school/work; and quality improvement to reduce ED visits/hospitalizations. Notably, these findings were limited by having only a few studies, typically nonrandomized, on which to draw conclusions. Most of the studies used a pre-post design, which more often reported a beneficial effect than the RCTs.
TABLE 3.
Summary of SOE for Interventions Designed to Modify Clinician Adherence to Asthma Guidelines
| Intervention | Outcome: Prescription of Controller Medications | Outcome: Self-management Education/Asthma Action Plans | Outcome: ED Visits/Hospitalizations | Outcome: Missed Days of Work/School |
|---|---|---|---|---|
| Clinical pharmacy support | Benefit within 3 studies with moderate magnitude of effect; SOE moderate | Benefit in 1 study with moderate magnitude of effect; SOE moderate | Unable to make a conclusion based on 1 study with imprecise results; SOE insufficient | No studies; SOE insufficient |
| Decision support | Benefit with large magnitude of effect; SOE moderate | Studies consistently favor intervention with large magnitude of effect; SOE moderate | Benefit with moderate magnitude of effect (larger in pre-post studies); SOE moderate | Unable to conclude due to inconsistent results; SOE insufficient |
| Education only | No benefit; SOE low | Small to moderate increases in a minority of studies; SOE low | No benefit; inconsistent results (reductions and increases); low SOE | No conclusion due to inconsistent and imprecise estimates of effect in 5 studies; SOE insufficient |
| Feedback and audit | Benefit with moderate magnitude of effect; SOE moderate | Benefit with low magnitude of effect; SOE low | No conclusion could be made due to conflicting results in few studies; SOE insufficient | No conclusion due to inconsistent results in 1 included study; SOE insufficient |
| Information only | Unable to make conclusion; SOE insufficient | No studies; SOE insufficient | Unable to make conclusion; no difference seen, but study quality was low; SOE insufficient | No studies; SOE insufficient |
| Multicomponent interventions | Benefit with moderate magnitude of effect; SOE low | Benefit, with moderate magnitude of effect (larger in observational studies); SOE low | Unable to make conclusion; although the 1 study reported a large reduction, the study quality was low; insufficient SOE | No conclusion; 1 study reported a large reduction, but study quality was low; SOE insufficient |
| Organizational change | Benefit with small magnitude of effect; SOE low | Two studies show benefit with moderate magnitude of effect; SOE low | No benefit with range of magnitudes of effect; SOE low | No benefit (for missed school days); SOE low |
| Quality improvement and pay-for-performance | No studies; SOE insufficient | Observational studies showed benefit, but the RCT did not; benefit with moderate magnitude of effect; SOE low | No benefit; SOE low | Unable to draw conclusions; 1 study (with high risk of bias) reported a nonsignificant reduction in schooldays missed; SOE insufficient |
There was much more evaluation of the health care process than the clinical outcomes; most common was the prescribing of asthma controller medications, and least common was missed days of work/school. Three interventions were not assessed in terms of missed days of work/school. There was insufficient evidence to comment on the effectiveness of many of the interventions, particularly for missed school or workdays.
Heterogeneity, such as variation in personnel delivering and length of intervention, made it challenging to draw conclusions. Future studies should thus include standardization of outcome measures, more information about the dose and frequency of the intervention, improved description of the study populations, and more use of RCTs to isolate the effectiveness of each intervention. The interventions may also need to more comprehensively meet the needs of health care providers to deliver asthma care (ie, help providers complete multiple elements of providing asthma care, eg, prescribe controller medications and provide asthma action plans).
Conclusions
We found more information about the effect of interventions on health care process outcomes than for clinical outcomes. There is low to moderate evidence to support the use of decision support, feedback and audit, and clinical pharmacy support to improve the adherence of health care providers to asthma guidelines and to improve clinical outcomes. There is a need to further evaluate health care provider–targeted interventions with a focus on standardized measures of outcomes and more rigorous study designs.
Supplementary Material
Acknowledgments
We acknowledge the continuing support of our Agency for Healthcare Research and Quality Task Order Officer, Christine Chang, MD, MPH. We extend our appreciation to our Key Informants and members of our Technical Expert Panel, all of whom provided thoughtful advice and input during our research process. The Evidence-based Practice Center thanks Oluwatosin Ikotun, Nelson Biodun Olagbuji, and Oluwaseun Omole for their assistance with screening articles and data abstraction.
Glossary
- CI
confidence interval
- ED
emergency department
- ICS
inhaled corticosteroids
- OR
odds ratio
- RCT
randomized controlled trial
- SOE
strength of evidence
Footnotes
Dr Okelo developed the protocol, completed data collection and data synthesis, drafted the manuscript, and critically reviewed the manuscript; Dr Butz, Ms Sharma, Drs Diette, Pitts, and King, Ms Linn, Ms Reuben, and Dr Chelladurai developed the protocol, completed data collection and data synthesis, and critically reviewed the manuscript; Dr Robinson developed the protocol, completed data collection and data synthesis, drafted the manuscript, and critically reviewed the manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Agency for Healthcare Research and Quality contract number: HHSA 290 2007 10061 I. The authors of this article are responsible for its contents, including any clinical or treatment recommendations. No statement in this article should be construed as an official position of Agency for Healthcare Research and Quality or of the US Department of Health and Human Services.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Centers for Disease Control and Prevention . Vital signs: asthma prevalence, disease characteristics, and self-management education: United States, 2001—2009. MMWR Morb Mortal Wkly Rep. 2011;60(17):547–552 [PubMed] [Google Scholar]
- 2.Akinbami L, Centers for Disease Control and Prevention National Center for Health Statistics . The state of childhood asthma, United States, 1980–2005. Adv Data. 2006;(381):1–24 [PubMed] [Google Scholar]
- 3.National Asthma Education and Prevention Program . Expert Panel Report 3 (EPR-3): Guidelines for the diagnosis and management of asthma—summary report 2007. J Allergy Clin Immunol. 2007;120(suppl 5):S94–S138 [DOI] [PubMed] [Google Scholar]
- 4.Evans R, III, Gergen PJ, Mitchell H, et al. A randomized clinical trial to reduce asthma morbidity among inner-city children: results of the National Cooperative Inner-City Asthma Study. J Pediatr. 1999;135(3):332–338 [DOI] [PubMed] [Google Scholar]
- 5.Kattan M, Crain EF, Steinbach S, et al. A randomized clinical trial of clinician feedback to improve quality of care for inner-city children with asthma. Pediatrics. 2006;117(6). Available at: www.pediatrics.org/cgi/content/full/117/6/e1095 [DOI] [PubMed] [Google Scholar]
- 6.Szefler SJ, Mitchell H, Sorkness CA, et al. Management of asthma based on exhaled nitric oxide in addition to guideline-based treatment for inner-city adolescents and young adults: a randomised controlled trial. Lancet. 2008;372(9643):1065–1072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wisnivesky JP, Lorenzo J, Lyn-Cook R, et al. Barriers to adherence to asthma management guidelines among inner-city primary care providers. Ann Allergy Asthma Immunol. 2008;101(3):264–270 [DOI] [PubMed] [Google Scholar]
- 8.Halterman JS, Aligne CA, Auinger P, McBride JT, Szilagyi PG. Inadequate therapy for asthma among children in the United States. Pediatrics. 2000;105(1 pt 3):272–276 [PubMed] [Google Scholar]
- 9.Halterman JS, Yoos HL, Kaczorowski JM, et al. Providers underestimate symptom severity among urban children with asthma. Arch Pediatr Adolesc Med. 2002;156(2):141–146 [DOI] [PubMed] [Google Scholar]
- 10.Cabana MD, Slish KK, Nan B, Lin X, Clark NM. Asking the correct questions to assess asthma symptoms. Clin Pediatr (Phila). 2005;44(4):319–325 [DOI] [PubMed] [Google Scholar]
- 11.Cabana MD, Bruckman D, Meister K, Bradley JF, Clark N. Documentation of asthma severity in pediatric outpatient clinics. Clin Pediatr (Phila). 2003;42(2):121–125 [DOI] [PubMed] [Google Scholar]
- 12.Ortega AN, Gergen PJ, Paltiel AD, Bauchner H, Belanger KD, Leaderer BP. Impact of site of care, race, and Hispanic ethnicity on medication use for childhood asthma. Pediatrics. 2002;109(1). Available at: www.pediatrics.org/cgi/content/full/109/1/e1 [DOI] [PubMed] [Google Scholar]
- 13.Akinbami LJ, Moorman JE, Garbe PL, Sondik EJ. Status of childhood asthma in the United States, 1980–2007. Pediatrics. 2009;123(suppl 3):S131–S145 [DOI] [PubMed] [Google Scholar]
- 14.Flores G, Snowden-Bridon C, Torres S, et al. Urban minority children with asthma: substantial morbidity, compromised quality and access to specialists, and the importance of poverty and specialty care. J Asthma. 2009;46(4):392–398 [DOI] [PubMed] [Google Scholar]
- 15.Bracha Y, Brottman G, Carlson A. Physicians, guidelines, and cognitive tasks. Eval Health Prof. 2011;34(3):309–335 [DOI] [PubMed] [Google Scholar]
- 16.Bratton SL, Cabana MD, Brown RW, et al. Asthma educational seminar targeting Medicaid providers. Respir Care. 2006;51(1):49–55 [PubMed] [Google Scholar]
- 17.Cabana MD, Slish KK, Evans D, et al. Impact of physician asthma care education on patient outcomes. Pediatrics. 2006;117(6):2149–2157 [DOI] [PubMed] [Google Scholar]
- 18.Brown R, Bratton SL, Cabana MD, Kaciroti N, Clark NM. Physician asthma education program improves outcomes for children of low-income families. Chest. 2004;126(2):369–374 [DOI] [PubMed] [Google Scholar]
- 19.Ruoff G. Effects of flow sheet implementation on physician performance in the management of asthmatic patients. Fam Med. 2002;34(7):514–517 [PubMed] [Google Scholar]
- 20.Lozano P, Finkelstein JA, Carey VJ, et al. A multisite randomized trial of the effects of physician education and organizational change in chronic-asthma care: health outcomes of the Pediatric Asthma Care Patient Outcomes Research Team II Study. Arch Pediatr Adolesc Med. 2004;158(9):875–883 [DOI] [PubMed] [Google Scholar]
- 21.Halterman JS, McConnochie KM, Conn KM, et al. A randomized trial of primary care provider prompting to enhance preventive asthma therapy. Arch Pediatr Adolesc Med. 2005;159(5):422–427 [DOI] [PubMed] [Google Scholar]
- 22.Butz AM, Eggleston P, Huss K, Kolodner K, Vargas P, Rand C. Children with asthma and nebulizer use: parental asthma self-care practices and beliefs. J Asthma. 2001;38(7):565–573 [DOI] [PubMed] [Google Scholar]
- 23.Coffman JM, Cabana MD, Yelin EH. Do school-based asthma education programs improve self-management and health outcomes? Pediatrics. 2009;124(2):729–742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Teach SJ, Crain EF, Quint DM, Hylan ML, Joseph JG. Improved asthma outcomes in a high-morbidity pediatric population: results of an emergency department-based randomized clinical trial. Arch Pediatr Adolesc Med. 2006;160(5):535–541 [DOI] [PubMed] [Google Scholar]
- 25.Wise RA, Bartlett SJ, Brown ED, et al. Randomized trial of the effect of drug presentation on asthma outcomes: the American Lung Association Asthma Clinical Research Centers. J Allergy Clin Immunol. 2009;124(3):436–444, 444e1–8 [DOI] [PMC free article] [PubMed]
- 26.Interventions to Modify Healthcare Provider Adherence to Asthma Guidelines. Research protocol. Available at: http://effectivehealthcare.ahrq.gov/ehc/products/372/993/AsthmaAdherenceGuidelines_20120302.pdf. Accessed July 16, 2013 [PubMed]
- 27.Okelo SO, Butz AM, Sharma R, et al. Interventions to Modify Adherence to Asthma Guidelines. Evidence Report (prepared by the Johns Hopkins University Evidence-based Practice Center, under Contract No. HHSA 290 2007 10061 I). Comparative Effectiveness Reviews No. 95. Rockville, MD: Agency for Healthcare Research and Quality; 2013
- 28.Akinbami LJ, Sullivan SD, Campbell JD, et al. Asthma outcomes: healthcare utilization and costs. J Allergy Clin Immunol. 2012;129(suppl 3):S49–S64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Guyatt G, Oxman AD, Sultan S, et al. GRADE guidelines 11—making an overall rating of confidence in effect estimates for a single outcome and for all outcomes. J Clin Epidemiol. 2012;66(2):15–17 [DOI] [PubMed] [Google Scholar]
- 30.Higgins JPT, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration; 2009. Available at: http://www.cochrane-handbook.org. Accessed July 16, 2013
- 31.Cochrane Effective Practice and Organization of Care Group. Data collection checklist. 2002. Available at: http://epoc.cochrane.org/sites/epoc.cochrane.org/files/uploads/datacollectionchecklist.pdf. Accessed July 16, 2013
- 32.Owens DK, Lohr KN, Atkins D, et al. AHRQ series paper 5: grading the strength of a body of evidence when comparing medical interventions—agency for healthcare research and quality and the effective health-care program. J Clin Epidemiol. 2010;63(5):513–523 [DOI] [PubMed] [Google Scholar]
- 33.Armour C, Bosnic-Anticevich S, Brillant M, et al. Pharmacy Asthma Care Program (PACP) improves outcomes for patients in the community. Thorax. 2007;62(6):496–502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.de Vries TW, van den Berg PB, Duiverman EJ, de Jong-van den Berg LT. Effect of a minimal pharmacy intervention on improvement of adherence to asthma guidelines. Arch Dis Child. 2010;95(4):302–304 [DOI] [PubMed] [Google Scholar]
- 35.Saini B, Krass I, Armour C. Development, implementation, and evaluation of a community pharmacy-based asthma care model. Ann Pharmacother. 2004;38(11):1954–1960 [DOI] [PubMed] [Google Scholar]
- 36.Horswell R, Butler MK, Kaiser M, et al. Disease management programs for the underserved. Dis Manag. 2008;11(3):145–152 [DOI] [PubMed] [Google Scholar]
- 37.Mitchell EA, Didsbury PB, Kruithof N, et al. A randomized controlled trial of an asthma clinical pathway for children in general practice. Acta Paediatr. 2005;94(2):226–233 [DOI] [PubMed] [Google Scholar]
- 38.Lesho EP, Myers CP, Ott M, Winslow C, Brown JE. Do clinical practice guidelines improve processes or outcomes in primary care? Mil Med. 2005;170(3):243–246 [DOI] [PubMed] [Google Scholar]
- 39.Cloutier MM, Hall CB, Wakefield DB, Bailit H. Use of asthma guidelines by primary care providers to reduce hospitalizations and emergency department visits in poor, minority, urban children. J Pediatr. 2005;146(5):591–597 [DOI] [PubMed] [Google Scholar]
- 40.Cloutier MM, Wakefield DB, Carlisle PS, Bailit HL, Hall CB. The effect of Easy Breathing on asthma management and knowledge. Arch Pediatr Adolesc Med. 2002;156(10):1045–1051 [DOI] [PubMed] [Google Scholar]
- 41.Rance K, O’Laughlen M, Ting S. Improving asthma care for African American children by increasing national asthma guideline adherence. J Pediatr Health Care. 2011;25(4):235–249 [DOI] [PubMed] [Google Scholar]
- 42.Shapiro A, Gracy D, Quinones W, Applebaum J, Sarmiento A. Putting guidelines into practice: improving documentation of pediatric asthma management using a decision-making tool. Arch Pediatr Adolesc Med. 2011;165(5):412–418 [DOI] [PubMed] [Google Scholar]
- 43.Cho SH, Jeong JW, Park HW, et al. Effectiveness of a computer-assisted asthma management program on physician adherence to guidelines. J Asthma. 2010;47(6):680–686 [DOI] [PubMed] [Google Scholar]
- 44.Martens JD, van der Weijden T, Severens JL, et al. The effect of computer reminders on GPs’ prescribing behaviour: a cluster-randomised trial. Int J Med Inform. 2007;76(suppl 3):S403–S416 [DOI] [PubMed] [Google Scholar]
- 45.Eccles M, McColl E, Steen N, et al. Effect of computerised evidence based guidelines on management of asthma and angina in adults in primary care: cluster randomised controlled trial. BMJ. 2002;325(7370):941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shiffman RN, Freudigman M, Brandt CA, Liaw Y, Navedo DD. A guideline implementation system using handheld computers for office management of asthma: effects on adherence and patient outcomes. Pediatrics. 2000;105(4 pt 1):767–773 [DOI] [PubMed] [Google Scholar]
- 47.Bell LM, Grundmeier R, Localio R, et al. Electronic health record-based decision support to improve asthma care: a cluster-randomized trial. Pediatrics. 2010;125(4). Available at: www.pediatrics.org/cgi/content/full/125/4/e770 [DOI] [PubMed] [Google Scholar]
- 48.Davis AM, Cannon M, Ables AZ, Bendyk H. Using the electronic medical record to improve asthma severity documentation and treatment among family medicine residents. Fam Med. 2010;42(5):334–337 [PubMed] [Google Scholar]
- 49.Fairall L, Bachmann MO, Zwarenstein M, et al. Cost-effectiveness of educational outreach to primary care nurses to increase tuberculosis case detection and improve respiratory care: economic evaluation alongside a randomised trial. Trop Med Int Health. 2010;15(3):277–286 [DOI] [PubMed] [Google Scholar]
- 50.Shah S, Sawyer SM, Toelle BG, et al. Improving paediatric asthma outcomes in primary health care: a randomised controlled trial. Med J Aust. 2011;195(7):405–409 [DOI] [PubMed] [Google Scholar]
- 51.Smeele IJ, Grol RP, van Schayck CP, van den Bosch WJ, van den Hoogen HJ, Muris JW. Can small group education and peer review improve care for patients with asthma/chronic obstructive pulmonary disease? Qual Health Care. 1999;8(2):92–98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Clark NM, Gong M, Schork MA, et al. Impact of education for physicians on patient outcomes. Pediatrics. 1998;101(5):831–836 [DOI] [PubMed] [Google Scholar]
- 53.Stergachis A, Gardner JS, Anderson MT, Sullivan SD. Improving pediatric asthma outcomes in the community setting: does pharmaceutical care make a difference? J Am Pharm Assoc (Wash). 2002;42(5):743–752 [DOI] [PubMed] [Google Scholar]
- 54.Premaratne UN, Sterne JA, Marks GB, Webb JR, Azima H, Burney PG. Clustered randomised trial of an intervention to improve the management of asthma: Greenwich asthma study. BMJ. 1999;318(7193):1251–1255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mahi-Taright S, Belhocine M, Aït-Khaled N. Can we improve the management of chronic obstructive respiratory disease? The example of asthma in adults. Int J Tuberc Lung Dis. 2004;8(7):873–881 [PubMed] [Google Scholar]
- 56.Cowie RL, Underwood MF, Mack S. The impact of asthma management guideline dissemination on the control of asthma in the community. Can Respir J. 2001;8(suppl A):41A–45A [DOI] [PubMed]
- 57.Davis RS, Bukstein DA, Luskin AT, Kailin JA, Goodenow G. Changing physician prescribing patterns through problem-based learning: an interactive, teleconference case-based education program and review of problem-based learning. Ann Allergy Asthma Immunol. 2004;93(3):237–242 [DOI] [PubMed] [Google Scholar]
- 58.Blackstien-Hirsch P, Anderson G, Cicutto L, McIvor A, Norton P. Implementing continuing education strategies for family physicians to enhance asthma patients’ quality of life. J Asthma. 2000;37(3):247–257 [DOI] [PubMed] [Google Scholar]
- 59.Veninga CCM, Lagerløv P, Wahlström R, et al. Drug Education Project Group . Evaluating an educational intervention to improve the treatment of asthma in four European countries. Am J Respir Crit Care Med. 1999;160(4):1254–1262 [DOI] [PubMed] [Google Scholar]
- 60.Feder G, Griffiths C, Highton C, Eldridge S, Spence M, Southgate L. Do clinical guidelines introduced with practice based education improve care of asthmatic and diabetic patients? A randomised controlled trial in general practices in east London. BMJ. 1995;311(7018):1473–1478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Veninga CCM, Denig P, Zwaagstra R, Haaijer-Ruskamp FM. Improving drug treatment in general practice. J Clin Epidemiol. 2000;53(7):762–772 [DOI] [PubMed] [Google Scholar]
- 62.Hoskins G, Neville RG, Smith B, Clark RA. Does participation in distance learning and audit improve the care of patients with acute asthma attacks? The General Practitioners in Asthma Group. Health Bull (Edinb). 1997;55(3):150–155 [PubMed] [Google Scholar]
- 63.Coleman CI, Reddy P, Laster-Bradley NM, Dorval S, Munagala B, White CM. Effect of practitioner education on adherence to asthma treatment guidelines. Ann Pharmacother. 2003;37(7-8):956–961 [DOI] [PubMed] [Google Scholar]
- 64.Richman MJ, Poltawsky JS. Partnership for excellence in asthma care: evidence-based disease management. Stud Health Technol Inform. 2000;76:107–121 [PubMed] [Google Scholar]
- 65.Suh DC, Shin SK, Okpara I, Voytovich RM, Zimmerman A. Impact of a targeted asthma intervention program on treatment costs in patients with asthma. Am J Manag Care. 2001;7(9):897–906 [PubMed] [Google Scholar]
- 66.Baker R, Fraser RC, Stone M, Lambert P, Stevenson K, Shiels C. Randomised controlled trial of the impact of guidelines, prioritized review criteria and feedback on implementation of recommendations for angina and asthma. Br J Gen Pract. 2003;53(489):284–291 [PMC free article] [PubMed] [Google Scholar]
- 67.Schneider A, Wensing M, Biessecker K, Quinzler R, Kaufmann-Kolle P, Szecsenyi J. Impact of quality circles for improvement of asthma care: results of a randomized controlled trial. J Eval Clin Pract. 2008;14(2):185–190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Herborg H, Soendergaard B, Jorgensen T, et al. Improving drug therapy for patients with asthma—part 2: use of antiasthma medications. J Am Pharm Assoc (Wash). 2001;41(4):551–559 [DOI] [PubMed] [Google Scholar]
- 69.Søndergaard J, Andersen M, Vach K, Kragstrup J, Maclure M, Gram LF. Detailed postal feedback about prescribing to asthma patients combined with a guideline statement showed no impact: a randomised controlled trial. Eur J Clin Pharmacol. 2002;58(2):127–132 [DOI] [PubMed] [Google Scholar]
- 70.Martens JD, Winkens RA, van der Weijden T, de Bruyn D, Severens JL. Does a joint development and dissemination of multidisciplinary guidelines improve prescribing behaviour: a pre/post study with concurrent control group and a randomised trial. BMC Health Serv Res. 2006;6:145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Bryce FP, Neville RG, Crombie IK, Clark RA, McKenzie P. Controlled trial of an audit facilitator in diagnosis and treatment of childhood asthma in general practice. BMJ. 1995;310(6983):838–842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hagmolen of ten Have W, van den Berg NJ, van der Palen J, van Aalderen WM, Bindels PJ. Implementation of an asthma guideline for the management of childhood asthma in general practice: a randomised controlled trial. Prim Care Respir J. 2008;17(2):90–96 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Daniels EC, Bacon J, Denisio S, et al. Translation squared: improving asthma care for high-disparity populations through a safety net practice-based research network. J Asthma. 2005;42(6):499–505 [DOI] [PubMed] [Google Scholar]
- 74.Lundborg CS, Wahlström R, Oke T, Tomson G, Diwan VK. Influencing prescribing for urinary tract infection and asthma in primary care in Sweden: a randomized controlled trial of an interactive educational intervention. J Clin Epidemiol. 1999;52(8):801–812 [DOI] [PubMed] [Google Scholar]
- 75.Cloutier MM, Tennen H, Wakefield DB, Brazil K, Hall CB. Improving clinician self-efficacy does not increase asthma guideline use by primary care clinicians. Acad Pediatr. 2012;12(4):312–318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bender BG, Dickinson P, Rankin A, Wamboldt FS, Zittleman L, Westfall JM. The Colorado Asthma Toolkit Program: a practice coaching intervention from the High Plains Research Network. J Am Board Fam Med. 2011;24(3):240–248 [DOI] [PubMed] [Google Scholar]
- 77.Yawn BP, Bertram S, Wollan P. Introduction of asthma APGAR tools improve asthma management in primary care practices J Asthma Allergy. 2008;(August 31):1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lob SH, Boer JH, Porter PG, Núñez D, Fox P. Promoting best-care practices in childhood asthma: quality improvement in community health centers. Pediatrics. 2011;128(1):20–28 [DOI] [PubMed] [Google Scholar]
- 79.Finkelstein JA, Lozano P, Fuhlbrigge AL, et al. Pediatric Asthma Care Patient Outcomes Research Team . Practice-level effects of interventions to improve asthma care in primary care settings: the Pediatric Asthma Care Patient Outcomes Research Team. Health Serv Res. 2005;40(6 pt 1):1737–1757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Thyne SM, Marmor AK, Madden N, Herrick G. Comprehensive asthma management for underserved children. Paediatr Perinat Epidemiol. 2007;21(suppl 3):29–34 [DOI] [PubMed] [Google Scholar]
- 81.Halterman JS, Fisher S, Conn KM, et al. Improved preventive care for asthma: a randomized trial of clinician prompting in pediatric offices. Arch Pediatr Adolesc Med. 2006;160(10):1018–1025 [DOI] [PubMed] [Google Scholar]
- 82.McCowan C, Neville RG, Ricketts IW, Warner FC, Hoskins G, Thomas GE. Lessons from a randomized controlled trial designed to evaluate computer decision support software to improve the management of asthma. Med Inform Internet Med. 2001;26(3):191–201 [DOI] [PubMed] [Google Scholar]
- 83.Ragazzi H, Keller A, Ehrensberger R, Irani AM. Evaluation of a practice-based intervention to improve the management of pediatric asthma. J Urban Health. 2011;88(suppl 1):38–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Newton WP, Lefebvre A, Donahue KE, Bacon T, Dobson A. Infrastructure for large-scale quality-improvement projects: early lessons from North Carolina Improving Performance in Practice. J Contin Educ Health Prof. 2010;30(2):106–113 [DOI] [PubMed] [Google Scholar]
- 85.To T, Cicutto L, Degani N, McLimont S, Beyene J. Can a community evidence-based asthma care program improve clinical outcomes?: a longitudinal study. Med Care. 2008;46(12):1257–1266 [DOI] [PubMed] [Google Scholar]
- 86.Holton C, Crockett A, Nelson M, et al. Does spirometry training in general practice improve quality and outcomes of asthma care? Int J Qual Health Care. 2011;23(5):545–553 [DOI] [PubMed] [Google Scholar]
- 87.Sulaiman ND, Barton CA, Liaw ST, et al. Do small group workshops and locally adapted guidelines improve asthma patients’ health outcomes? A cluster randomized controlled trial. Fam Pract. 2010;27(3):246–254 [DOI] [PubMed] [Google Scholar]
- 88.Frankowski BL, Keating K, Rexroad A, et al. Community collaboration . Community collaboration: concurrent physician and school nurse education and cooperation increases the use of asthma action plans. J Sch Health. 2006;76(6):303–306 [DOI] [PubMed] [Google Scholar]
- 89.Glasgow NJ, Ponsonby AL, Yates R, Beilby J, Dugdale P. Proactive asthma care in childhood: general practice based randomised controlled trial. BMJ. 2003;327(7416):659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Patel PH, Welsh C, Foggs MB. Improved asthma outcomes using a coordinated care approach in a large medical group. Dis Manag. 2004;7(2):102–111 [DOI] [PubMed] [Google Scholar]
- 91.Homer CJ, Forbes P, Horvitz L, Peterson LE, Wypij D, Heinrich P. Impact of a quality improvement program on care and outcomes for children with asthma. Arch Pediatr Adolesc Med. 2005;159(5):464–469 [DOI] [PubMed] [Google Scholar]
- 92.Fox P, Porter PG, Lob SH, Boer JH, Rocha DA, Adelson JW. Improving asthma-related health outcomes among low-income, multiethnic, school-aged children: results of a demonstration project that combined continuous quality improvement and community health worker strategies. Pediatrics. 2007;120(4). Available at: www.pediatrics.org/cgi/content/full/120/4/e902 [DOI] [PubMed] [Google Scholar]
- 93.Mangione-Smith R, Schonlau M, Chan KS, et al. Measuring the effectiveness of a collaborative for quality improvement in pediatric asthma care: does implementing the chronic care model improve processes and outcomes of care? Ambul Pediatr. 2005;5(2):75–82 [DOI] [PubMed] [Google Scholar]
- 94.Weinberger M, Murray MD, Marrero DG, et al. Effectiveness of pharmacist care for patients with reactive airways disease: a randomized controlled trial. JAMA. 2002;288(13):1594–1602 [DOI] [PubMed] [Google Scholar]
- 95.Renzi PM, Ghezzo H, Goulet S, Dorval E, Thivierge RL. Paper stamp checklist tool enhances asthma guidelines knowledge and implementation by primary care physicians. Can Respir J. 2006;13(4):193–197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Cloutier MM, Grosse SD, Wakefield DB, Nurmagambetov TA, Brown CM. The economic impact of an urban asthma management program. Am J Manag Care. 2009;15(6):345–351 [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.