In recent years, there is an impression that there has been increasing use of tidal prescriptions in automated peritoneal dialysis (APD). This is occurring despite the evidence that tidal peritoneal dialysis (TPD) does not enhance peritoneal clearances (1,2). The trend to use more TPD is likely being driven by high rates of what is known as “drain pain” (3). This, in turn, is thought to be related to hydraulic suction which has replaced gravity as the means of fluid drainage in modern cyclers and which may, depending on catheter placement, lead to painful suction on visceral organs or on parietal peritoneum. Tidal peritoneal dialysis is also being used in situations where peritoneal catheter drainage is sub-optimal in order to minimize total drain time (4). There has been great variation in the way TPD is prescribed, with different centers using contrasting approaches although there is little published information on this (5,6,7).
To investigate these impressions, we carried out a cross-sectional survey at six large PD units in the province of Ontario, Canada, in the summer of 2010. All centers used the Baxter Home Choice 10.2 cycler (Baxter, Deerfield, IL, USA). At the time of the survey, this was the only Baxter cycler used in Canada. The lead author (PGB) is anecdotally aware that Baxter had in excess of 90% of peritoneal dialysis (PD) business in Ontario at the time concerned. Therefore, this was by far the most common cycler in clinical practice and the study is likely quite representative.
The survey was provided to the PD nurses at each of the six sites. They were asked the size of their PD program, the number of patients on cycler and the percentage of those patients who were on TPD. They were also asked for the indication for which TPD was being used and the details of the TPD prescription.
Results
All six centers responded. They varied in size from 24 to 106 patients. In total, they were treating 375 prevalent PD patients. Of these, 293 (78%) were on APD and 82 (22%) were on continuous ambulatory peritoneal dialysis. Of the 293 APD patients, 84 (28%) were on TPD.
Percentage use of TPD among APD patients at the individual centers ranged from 4 to 37%. Among these 84 patients, the indication for TPD was drain pain in 72 (86%) cases. The second most common indication was ‘low transport status’ in 8 patients - all at one center. The remaining 4 patients were on TPD because of frequent low-drain-volume alarms disrupting sleep.
The degree of TPD varied between 70 and 95%. The single most common percentage tidal settings were 75% and 80%, which, between them, accounted for almost half of all the patients (Table 1, Figure 1).
TABLE 1.
Variation in Percentage of TPD Used in 78 Patients
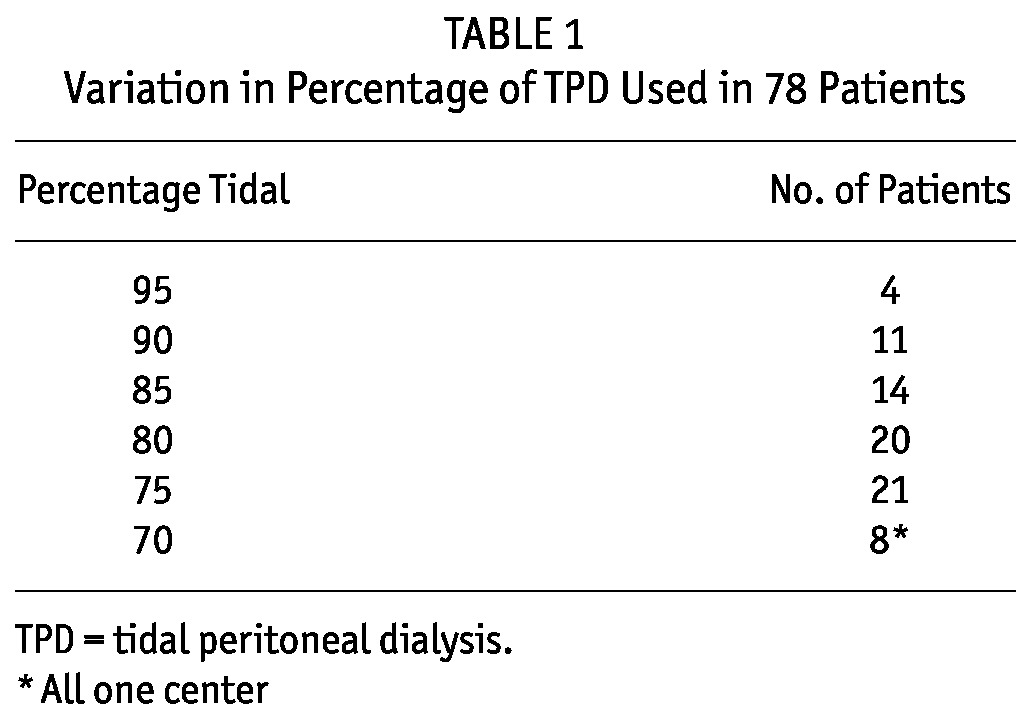
Figure 1 —

Variation in % TPD used in 78 patients. TPD = tidal peritoneal dialysis.
Two distinct settings can be programmed when TPD is being done on the Home Choice 10.2 cycler. Setting the “Tidal Full Drain” option allows a complete drainage of the peritoneal cavity at drain cycle intervals as defined by the clinician. This is prescribed to avoid a situation where ultrafiltration (UF) leads to a progressive rise in residual volume, resulting in increased intraperitoneal volume and raised intraperitoneal pressure. This setting was prescribed at only one of the six centers. At this center, 22 (63%) of the 35 tidal patients had full drains programmed into their cycler, all at a frequency of every third drain cycle. The second programmable TPD setting is “Tidal Total Ultrafiltration.” This requires that the clinician input into the cycler program the volume of total UF expected during the time that the patient is on the cycler. A percentage of this UF volume will be drained along with the tidal volume in each cycle, depending on the number of cycles programmed. This setting was used in 64 of the 84 patients (76%). This comprised all the TPD patients at two centers and 3 out of 9 at a third center. At two of the centers it was not used at all. Only in one center were both options used in the majority of TPD patients.
Discussion
This survey shows that there is widespread use of TPD in patients treated with APD in Ontario, Canada. The commonest indication for TPD was drain pain. This is quite a frequent problem in many centers, likely related to the widespread utilization of cyclers which use hydraulic suction, rather than gravity, to drain the PD solution (4). TPD is also being used in situations where catheter function is poor and where full drainage takes too much time, detracting from the efficiency of dialysis. However, this was a much less frequent indication in the centers we surveyed (5). Both issues may sometimes be related to PD catheter placement and location in the peritoneal cavity. As such, problems with drain pain and slow drainage may coexist.
What is notable is that there is substantial variation in how TPD is prescribed. The majority of TPD patients are receiving 75 - 80% tidal, while others are receiving 70% or levels greater than 85%. Some of the variation may result from a process of trial and error, carried out in order to find the amount of tidal required to minimize drain pain. Overall, the impression is that the choice of the tidal volume percent is arbitrary from center to center and is not based on any specific evidence.
Similarly, the practice of fully draining a TPD patient every third or fourth cycle is used in the majority of patients in one center, but not at all in the other five, suggesting a similar degree of arbitrariness. The same applies to setting the “Tidal Total Ultrafiltration” volume greater than the default value of zero. This was used universally in two centers and not at all in three others. In only one center were both selections used in the majority of TPD patients. These cycler settings were both designed to prevent a progressive rise in residual volume, as ultrafiltrate accumulates during TPD, potentially resulting in increased intraperitoneal volume and consequent raised intraperitoneal pressure. The potential adverse consequences of this have been highlighted in a recent study looking at the problem of “overfill” in PD patients (8). Adverse events including a number of deaths were associated with overfill. In theory, TPD may increase the risk of overfill (8). The default for both these TPD prescription settings was “off” in the Home Choice 10.2 cycler. Conversely, both of these settings are now programmed “on” by default in the new Home Choice 10.4 software, with full drains every third cycle and minimum “Total UF” of 1,000 mL. The change was implemented specifically to reduce the possibility of overfill. Prescribers now need to actively turn off or alter these settings if they are unwanted or if they desire a different frequency of Tidal Full Drain, or a greater or lesser Tidal Total UF. This change reflects recent concerns about overfill (8).
There is clearly a need for greater understanding of how TPD is best used and studies on this issue would be helpful. There is a need to understand better how effective TPD is for drain pain or a poorly draining PD catheter, how real the risks of overfill are, and how much TPD might contribute to them. At present, there is insufficient information in the literature to provide evidence-based guidelines on how to deliver TPD. However, use of the prescription settings to prevent overfill may be particularly important in patients who have substantial ultrafiltration on TPD.
Disclosures
Peter G. Blake and Arsh K. Jain have received research funds fom Baxter. James A. Sloand, Susan McMurray and Sandee Matthews are employees of Baxter.
References
- 1. Perez RA, Blake PG, McMurray S, Mupas L, Oreopoulos DG. What is the optimal frequency of cycling in automated peritoneal dialysis? Perit Dial Int 2000; 20:548–56 [PubMed] [Google Scholar]
- 2. Juergensen PH, Murphy AL, Pherson KA, Kliger AS, Finkelstein FO. Tidal peritoneal dialysis: comparison of different tidal regimens and automated peritoneal dialysis. Kidney Int 2000; 57:2603–7 [DOI] [PubMed] [Google Scholar]
- 3. Juergensen PH, Murphy AL, Pherson KA, Chorney WS, Kliger AS, Finkelstein FO. Tidal peritoneal dialysis to achieve comfort in chronic peritoneal dialysis patients. Adv Perit Dial 1999; 15:125–6 [PubMed] [Google Scholar]
- 4. Neri L, Viglino G, Cappelletti A, Gandolfo C. Evaluation of drainage times and alarms with various automated peritoneal dialysis modalities. Adv Perit Dial 2001; 17:72–4 [PubMed] [Google Scholar]
- 5. Mujais S, Childers RW. Profiles of automated peritoneal dialysis prescriptions in the US 1997-2003. Kidney Int Suppl 2006; (103):S84–90 [DOI] [PubMed] [Google Scholar]
- 6. Davis DI, Cizman B, Mundt K, Wu L, Childers R, Mell R, et al. Relationship between drain volume/fill volume ratio and clinical outcomes associated with overfill complaints in peritoneal dialysis patients. Perit Dial Int 2011; 31:148–53 [DOI] [PubMed] [Google Scholar]
- 7. Mujais S, Childers RW. Profiles of automated peritoneal dialysis prescriptions in the US 1997-2003. Kidney Int Suppl 2006; 103:S84–90 [DOI] [PubMed] [Google Scholar]
- 8. Fernando SK, Finkelstein FO. Tidal PD: Its role in the current practice of peritoneal dialysis. Kidney Int Suppl 2006; (103):S91–5 [DOI] [PubMed] [Google Scholar]


