Abstract
Background
Tetracaine and proparacaine are two of the most commonly used medications for providing topical anesthesia in laser in situ keratomileusis (LASIK) and photorefractive keratectomy (PRK). These agents have not been previously compared in a prospective manner to determine their efficacy in these settings.
Methods
This prospective, single-masked, randomized study comprised 256 eyes from 128 consecutive patients being treated with LASIK or PRK who were randomized to receive tetracaine in one eye and proparacaine in the other. The patients were blinded as to which anesthetic agent was used in each eye. Pain levels were graded on a 0–10 scale, and were assessed upon instillation, during surgery, immediately postoperatively, 30 minutes postoperatively, overnight, and on postoperative day 1. Patients were asked 30 minutes after surgery which anesthetic agent they would choose.
Results
Both anesthetic agents resulted in diminished amounts of subjective pain in patients undergoing LASIK and PRK. Tetracaine caused significantly more pain upon instillation than proparacaine for both LASIK and PRK patients. LASIK patients noted significantly less pain 30 minutes after surgery when treated with tetracaine. Significantly more LASIK patients preferred the eye treated with tetracaine. These differences were not present in the PRK group.
Conclusion
Both tetracaine and proparacaine are effective methods of topical anesthesia in LASIK and PRK. Tetracaine caused significantly more pain upon instillation in all patients, but resulted in greater analgesia 30 minutes after surgery in the LASIK group. Patients in the LASIK group expressed a preference for tetracaine over proparacaine. There was no significant drop preference among PRK patients.
Keywords: tetracaine, pain control, laser in situ keratomileusis, photorefractive keratectomy
Introduction
Laser in situ keratomileusis (LASIK) and photorefractive keratectomy (PRK) are widely used and highly efficacious surgical procedures for treating refractive error. Achieving effective pain control, both intraoperatively and postoperatively, is of paramount importance to patients who choose to undergo these elective procedures.
Proparacaine hydrochloride (Bausch and Lomb, Inc, Tampa, FL, USA) and tetracaine hydrochloride (preservative-free, Alcon, Inc., Fort Worth, TX, USA) are two of the most commonly used topical anesthetics in LASIK and PRK. These agents have been widely used in ophthalmic surgery for years, but their efficacy has only been studied and compared in emergency room settings1 and in the setting of intravitreal injection.2 Studies comparing the efficacy of these anesthetic agents in LASIK and PRK are lacking. We conducted a prospective, randomized, contralateral eye study to evaluate the efficacy of proparacaine and tetracaine for pain control in patients undergoing LASIK and PRK.
Patients and methods
Two hundred and fifty-six eyes from 128 consecutive patients undergoing LASIK or PRK at the John A Moran Eye Center, Department of Ophthalmology, University of Utah, between November 2011 and September 2012 were studied. LASIK and PRK were performed using both the VISX Custom-Vue™ STAR S4 IR™ (Abbott Medical Optics, Santa Ana, CA, USA) and Wavelight® Allegretto 400 Hz Wave® Eye-Q (Alcon, Inc. Erlangen, Germany) excimer lasers, chosen for each patient at the surgeon’s discretion.
The University of Utah Hospital institutional review board approved the research protocol in accordance with the tenets of the Declaration of Helsinki (approval numbers 51250 and 51251). All patients provided their informed consent after they received an explanation of the procedure, including all risks and benefits. Patients were appraised of the anesthetic variance inherent within the design of the study. Each patient had a preoperative discussion of relevant medical history, including history of herpetic eye disease and family history of keratoconus. All participants in this study were over the age of 21 years.
Patients were excluded if they: had a history of clinically significant lens opacity, previous corneal or intraocular surgery, thin corneas, keratoconus, unstable refraction, amblyopia, autoimmune disease; were pregnant or lactating; or were on immunosuppressive therapy.
Eligible patients were scheduled for bilateral LASIK or PRK with distance correction planned in each eye. Patients desiring monovision or treating only one eye were excluded. Patients were randomly assigned to have proparacaine or tetracaine applied to either the right or left eye. Each patient was masked with respect to which anesthetic agent they were receiving in each eye. The right eye was operated on first in all patients.
All LASIK flaps were created with the iFS™ Advanced Femtosecond Laser (Abbott Medical Optics) at 150 kHz in a raster pattern with a bed energy of 1.15 μJ, and pocket enabled. Flaps were created with an intended thickness of 110 μm, a diameter of 8.4–9.0 mm, a superior hinge arc of 55°, and a side cut angle of 70°. The ablation diameter range was typically 6.5 mm to a blended transition zone of 8 mm. If the 8.0 mm maximum intended ablation diameter exceeded the flap diameter, the hinge and flap were shielded during ablation. Cases in which the ablation diameter exceeded 8.0 mm were encountered when the Wavelight Allegretto 400 Hz Wave Eye-Q platform was used, due to variation in software parameters.
Prior to ablation, the epithelial layer was removed with a spatula after application of 20% alcohol solution for a period of 30 seconds. Pain was the primary outcome variable, measured upon instillation of proparacaine or tetracaine intraoperatively, immediately postoperatively, 30 minutes postoperatively, overnight, and on postoperative day 1. Patients were asked to grade the degree of pain in each eye on a numeric pain rating scale according to severity (0= no pain, 5= moderate pain, 10= severe pain) in accordance with the frequently used metric devised by McCaffery and Pasero.3 Intraoperative assessment of pain was performed either immediately after epithelial scraping or after lifting the flap in PRK and LASIK, respectively. Thirty minutes after the procedure, patients were asked which anesthetic agent they would choose.
Anesthetic agents used in the study included 0.5% tetracaine hydrochloride (preservative-free, Alcon, Inc.) and 0.5% proparacaine hydrochloride (Bausch and Lomb, Inc). The proparacaine drops used contain 0.01% benzalkonium chloride. If patients reported pain during the procedure or asked for more anesthetic medicine, additional drops of each respective agent were given. Requests for additional anesthetic drops were documented.
Postoperatively, each eye received one drop of gatifloxacin 0.3% (Allergan Inc, Irvine, CA, USA) and prednisolone acetate 1% (Allergan Inc). No preoperative anxiolytic medications were administered. Postoperatively, LASIK and PRK patients were treated with prednisolone acetate hourly on postoperative day 0, and then four times daily starting on day 1. Gatifloxacin administration was continued postoperatively, four times daily for one week. PRK patients were also treated with Acuvail® (ketorolac tromethamine 0.45%, Allergan Inc) twice daily for 3 days beginning on the day of surgery. All PRK patients had a bandage contact lens (Acuvue® Oasys®, Johnson & Johnson Vision Care Inc, Jacksonville, FL, USA) placed at the completion of surgery.
Statistical analysis
The study outcomes were modeled using multivariable mixed effects regression models, which permitted a paired comparison between eyes in the same patient, while controlling for covariates. Mixed effects linear regression was used for continuous outcomes, and mixed effects logistic regression was used for binary or dichotomous outcomes.
Pain was measured using a visual analog scale and treated as a continuous variable in the analysis. Pain at each time point was compared between the anesthetic agents using a multivariable mixed effects linear regression, controlling for the pain rating at the previous time point. This was to adjust for a potential carry-over effect of “pain anticipation” recalled from the previous pain measurement made by the patient. For example, for the comparison of pain between anesthetic agents upon drop instillation, the patient’s baseline pain rating was controlled.
For comparison of patient preference between the two topical anesthetics, a multivariable mixed effects logistic regression model was used. In this model, anesthetic (proparacaine versus tetracaine) was the primary predictor. The order in which the specific anesthetic eye drops were instilled (first eye or second eye) was included as a covariate. The patient choice of “no preference” was dropped from the analysis, resulting in two possible responses remaining for the model. This is consistent with the McNemar test, which is a paired sample cross-tabulation analysis. The McNemar test drops all subjects who do not change from pre to post, or from right to left eye, as these subjects provide no information for detecting a change. The mixed effects logistic regression model is simply an extension of the McNemar test to allow for covariates in the analysis. A separate model of preference was fitted for LASIK and PRK surgeries, as effect measure modification (statistical interaction) was observed. A similar approach was used to investigate the preference of the surgery between the two eyes, based on which eye was first operated on, controlling for the anesthetic eye drop instilled. Statistical analysis of the data was performed using Stata 12 software (StataCorp, College Station, TX, USA). All reported P-values are for a two-sided comparison.
Results
The study sample consisted of 256 eyes from 128 patients. The mean patient age was 33 (range 21–55) years, with 55% of the patients being female (Table 1). Sixty-seven patients received bilateral LASIK and 61 received bilateral PRK during the study. Seventy-seven patients were treated with the Allegretto laser and 51 with the VISX platform. Mean preoperative spherical equivalent was −3.80 for the LASIK group and −3.81 for the PRK group.
Table 1.
Patient demographics and treatment data
| LASIK (n=67 patients; n=134 eyes) | PRK (n=61 patients; n=122 eyes) | Combined sample (n=128 patients; n=256 eyes) | |
|---|---|---|---|
| Patient age, years | |||
| Mean ± SD (range) | 33.5±7.1 (21–52) | 32.1±6.9 (21–55) | 32.8±7.0 (21–55) |
| Sex, n (%) | |||
| Male | 28 (42) | 29 (48) | 57 (45) |
| Female | 39 (58) | 32 (52) | 71 (55) |
| Preoperative spherical equivalent | |||
| Mean ± SD | −3.80±1.93 | −3.81±1.69 | −3.81±1.81 |
| Laser used, n (%) | |||
| Allegretto | 48 (72) | 29 (48) | 77 (60) |
| Visx | 19 (28) | 32 (52) | 51 (40) |
| Order of operation, n (%) | |||
| Proparacaine eye first | 35 (52) | 36 (59) | 71 (55) |
| Tetracaine eye first | 32 (48) | 25 (41) | 57 (45) |
Abbreviations: LASIK, laser in situ keratomileusis; PRK, photorefractive keratectomy; SD, standard deviation.
Although randomized, a block randomization scheme was not used, resulting in a slight imbalance as to which topical anesthetic was used in the first and second eye operated on. Proparacaine was instilled in the first eye operated on 55% of the time, and tetracaine was instilled in the first eye 45% of the time (Table 1). The imbalance was less pronounced in the LASIK surgeries (52% and 48%) and more pronounced in the PRK surgeries (59% and 41%).
The average pain scores experienced at the various time points in the study are shown in Table 2. Upon drop instillation, patients perceived 2.1 points more pain in eyes treated with tetracaine than in eyes treated with proparacaine (95% confidence interval [CI] 1.8–2.5, P<0.001), after controlling for baseline pain. Intraoperatively, patients perceived a marginally significant 0.4 points more pain in the eye treated with tetracaine than in the eye treated with proparacaine (95% CI 0.0–0.8, P=0.067), after controlling for pain experienced during drop instillation.
Table 2.
Pain outcomes: proparacaine versus tetracaine, graded 0 to 10
| Time point | Proparacaine pain adjusted mean ± SE | Tetracaine pain adjusted mean ± SE | Adjusted mean difference (P-T)* (95% CI) | P-value |
|---|---|---|---|---|
| Total sample (n=128 patients) | ||||
| Instillation | 1.1±0.2 | 3.2±0.2 | −2.1 (−2.5, −1.8) | <0.001 |
| During surgery | 1.2±0.2 | 1.6±0.2 | −0.4 (−0.8, 0.0) | 0.067 |
| Immediately postoperatively | 0.9±0.1 | 0.9±0.1 | 0.1 (−0.2, 0.3) | 0.60 |
| 30 minutes postoperatively | 2.2±0.1 | 1.3±0.1 | 0.8 (0.5, 1.2) | <0.001 |
| Overnight | 1.3±0.2 | 1.6±0.2 | −0.3 (−0.6, 0.2) | 0.23 |
| Postoperative day 1 | 1.0±0.2 | 1.0±0.2 | 0.0 (−0.2, 0.3) | 0.89 |
| LASIK (n=67 patients) | ||||
| Instillation | 1.0±0.2 | 3.1±0.2 | −2.1 (−2.5, −1.6) | <0.001 |
| During surgery | 1.2±0.2 | 1.6±0.2 | −0.4 (−1.1, 0.2) | 0.22 |
| Immediately postoperatively | 1.1±0.1 | 1.0±0.1 | 0.1 (−0.2, 0.5) | 0.48 |
| 30 minutes postoperatively | 2.9±0.2 | 1.4±0.2 | 1.5 (1.0, 2.0) | <0.001 |
| Overnight | 0.9±0.3 | 1.3±0.2 | −0.4 (−1.1, 0.2) | 0.15 |
| Postoperative day 1 | 0.4±0.1 | 0.3±0.1 | 0.1 (−0.2, 0.3) | 0.53 |
| PRK (n=61 patients) | ||||
| Instillation | 1.2±0.2 | 3.3±0.2 | −2.2 (−2.7, −1.6) | <0.001 |
| During surgery | 1.2±0.2 | 1.6±0.2 | −0.4 (−1.1, 0.2) | 0.12 |
| Immediately postoperatively | 0.7±0.1 | 0.8±0.1 | 0.0 (−0.3, 0.2) | 0.92 |
| 30 minutes postoperatively | 1.4±0.2 | 1.3±0.2 | 0.1 (−0.2, 0.5) | 0.53 |
| Overnight | 1.7±0.3 | 1.9±0.3 | −0.2 (−0.7, 0.4) | 0.52 |
| Postoperative day 1 | 1.7±0.3 | 1.8±0.3 | 0.0 (−0.5, 0.5) | 0.90 |
Notes:
Adjusted for pain at previous measurement time using a multivariable mixed effects linear regression model; after instillation, also adjusted for surgical procedure (LASIK or PRK).
Abbreviations: LASIK, laser in situ keratomileusis; PRK, photorefractive keratectomy; P, proparacaine; T, tetracaine; SE, standard error of the mean; CI, confidence interval.
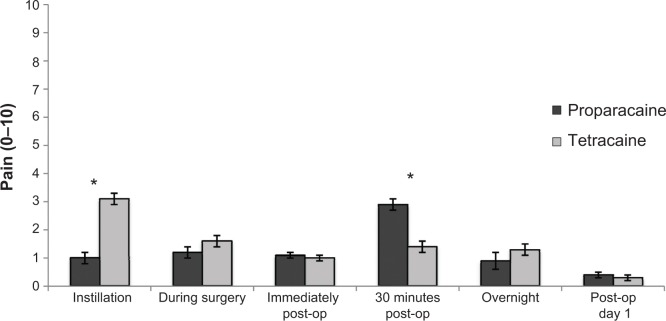
Immediately following surgery, patients discerned a nonsignificant (0.1 point) increase in pain perception in the eye treated with proparacaine relative to the eye treated with tetracaine (95% CI −0.2, 0.3, P=0.58), after controlling for pain experienced during surgery. At 30 minutes postoperatively, there was a distinction between patients who underwent LASIK surgery rather than PRK surgery. The PRK patients did not perceive a difference in pain control between proparacaine and tetracaine (0.1 points difference, 95% CI −0.2, 0.5, P=0.53) after controlling for pain experienced immediately following surgery (Figure 1). The LASIK patients, however, perceived 1.5 points greater pain in the eye treated with proparacaine as opposed to the eye treated with tetracaine (95% CI 1.0–2.0, P<0.001) after controlling for pain experienced immediately following surgery (Figure 2). No differences in pain were seen overnight or one day after the procedure.
Figure 1.
Pain outcomes for photorefractive keratectomy: proparacaine versus tetracaine.
Note: *Statistically significant (P<0.05).
Abbreviation: op, operative.
Figure 2.
Pain outcomes for laser in situ keratomileusis: proparacaine versus tetracaine.
Note: *Statistically significant (P<0.05).
Abbreviation: op, operative.
At 30 minutes postoperatively, patients were asked which eye they preferred. Forty-four percent of patients preferred the first eye operated on (the right eye), while 37% preferred the second (left) eye. Nineteen percent expressed no preference. After controlling for the anesthetic eye drop used in each specific eye, this first-eye preference did not achieve statistical significance (P=0.13, Table 3).
Table 3.
Order effect (preference by order in which eyes operated on)
| Preferred eye | LASIK (n=67) | PRK (n=61) | Combined sample (n=128) |
|---|---|---|---|
| Right (first) eye | 29 (43) | 28 (46) | 57 (45) |
| Left (second) eye | 27 (40) | 20 (33) | 27 (37) |
| No preference | 11 (16) | 13 (21) | 24 (19) |
| Adjusted OR* (95% CI), odds of preferring first eye to second eye | OR 1.80 | OR 1.38 | OR 1.53 |
| 95% CI 0.78–4.11 | 95% CI 0.63–3.01 | 95% CI 0.88–2.67 | |
| P-value | 0.16 | 0.42 | 0.13 |
Note:
After dropping the “no preference” patients, and then controlling for topical anesthetic in a mixed effects logistic regression model.
Abbreviations: CI, confidence interval; OR, odds ratio; LASIK, laser in situ keratomileusis; PRK, photorefractive keratectomy.
Thirty-nine percent of all patients preferred the eye treated with proparacaine while 42% preferred the eye treated with tetracaine, and 19% had no preference. The preferred anesthetic agent varied by type of procedure. After controlling for a potential order effect (which eye was operated on first), patients who underwent LASIK surgery in both eyes had a significant preference for tetracaine (51% versus 33%, P=0.019, Table 4). Patients who underwent PRK surgery in both eyes had a nonsignificant preference for proparacaine (46% versus 33%, P=0.16).
Table 4.
Drug preferred
| LASIK (n=67) | PRK (n=61) | Combined sample (n=128) | |
|---|---|---|---|
| Proparacaine, n (%) | 22 (33) | 28 (46) | 50 (39) |
| Tetracaine, n (%) | 34 (51) | 20 (33) | 54 (42) |
| No preference, n (%) | 11 (16) | 13 (21) | 24 (19) |
| Adjusted OR* (95% CI), odds of preferring proparacaine to tetracaine | OR 0.39 | OR 1.80 | NA** |
| 95% CI 0.18–0.86 | 95% CI 0.79–4.11 | ||
| P-value | 0.019 | 0.16 | |
Notes:
After dropping the “no preference” patients, and then controlling for order of instillation in a mixed effects logistic regression model. **not applicable since effect measure modification occurred, where the effect is in the opposite direction depending on type of surgery.
Abbreviations: CI, confidence interval; OR, odds ratio; LASIK, laser in situ keratomileusis; PRK, photorefractive keratectomy; NA, not applicable.
Discussion
Presently, utilization of ablative techniques such as LASIK and PRK for correction of refractive error remains highly prevalent due to the favorable efficacy and safety profiles associated with each respective procedure. Obvious discernment of variation with regard to intraoperative pain between each respective procedure is not typically possible. Nevertheless, on account of distinct differences in technique and anatomical location associated with each procedural approach, a comparative analysis regarding anesthetic preference for each procedure was performed for definitive evaluation. Proparacaine and tetracaine are two of the most commonly used topical anesthetics for controlling pain associated with each of the aforementioned procedures. Proparacaine and tetracaine are both ester-type anesthetics that exert their analgesic effects by blocking axonal sodium channels.4 While the abundance of corneal nerves makes it difficult to achieve complete anesthesia, both agents are generally effective for reduction of pain in patients undergoing LASIK and PRK.5 To date, there have not been any reported studies that have evaluated these medications for determination of superiority regarding efficacy as it relates to pain control during LASIK and PRK.
The results of our study show that patients experience significantly less pain upon instillation of proparacaine drops when compared with tetracaine drops. Intraoperatively, patients described slightly more pain with tetracaine than proparacaine, but this difference was not significant. There was no significant difference in pain reported immediately following the surgery. Thirty minutes postoperatively, patients reported significantly more pain in eyes treated with proparacaine. This finding remained significant in the LASIK subgroup, but disappeared in the PRK subgroup. In addition, there was no significant comparative difference reported overnight or on the first postoperative day.
Patients were asked which eye they preferred 30 minutes after their procedure. Because eyes in the study were randomized to receive one anesthetic drop or another, eye preference served as an analogue for anesthetic agent preference. All patients were unaware of which drop they received in each eye. Significantly more LASIK patients stated a preference for tetracaine. This may relate to the finding that LASIK patients who received proparacaine experienced more pain at this particular time point. This observation also suggests that tetracaine likely had a slightly longer clinical duration of action in these patients. There was no difference in drop preference among PRK patients. This is plausibly attributable to the use of bandage contact lenses in this group. It does not seem tenable that observed postoperative dissimilarities in discomfort and drop preference between the two procedures were associated with the surgical technique itself. A more pronounced degree of postoperative discomfort, and therefore more prominent discriminative anesthetic preference, would typically be expected to occur within the PRK group; however, this was not observed in our study.
Prior studies have examined the duration of anesthesia in patients receiving these eye drops. Bartfield et al conducted a contralateral eye study comparing proparacaine and tetracaine, and found similar durations of action in both drops, with tetracaine lasting 9.4 minutes and proparacaine lasting 10.7 minutes on average.1 Nomura et al measured the duration of action of 0.5% tetracaine by esthesiometry and found a duration of 10 minutes before eyes returned to baseline sensitivity.6 Weiss and Goren evaluated the duration of action of 0.5% proparacaine by esthesiometry and found this to be 34 minutes in normal subjects.7 Rifkin et al reported significantly less pain 15 minutes after intravitreal injection in patients who received tetracaine than in those who received proparacaine.2
Studies examining the effects of these medications in LASIK or PRK have been few. Shah et al reported a prospective study comparing tetracaine drops and lidocaine gel in patients undergoing femtosecond-laser assisted LASIK.8 Similar pain levels were described in both groups. The study was halted after eleven patients due to thinner, irregular flaps occurring in the lidocaine gel group.
In all contralateral-eye studies such as this one, the order effect becomes an important variable to consider. Several studies have suggested differences in patient perception between first-eye and second-eye surgeries. El Rami et al compared first-eye and second-eye LASIK surgeries and showed that patients experienced more pain during second-eye LASIK.9 Cheng et al also reported more pain in second-eye LASIK surgeries, especially during the microkeratome pass and placement of the lid speculum.10
While more patients in our study did prefer the first eye, the difference did not achieve statistical significance. This finding is in line with studies by Sharma et al11 and Nijkamp et al12 who found no significant differences in pain during second-eye cataract surgeries compared with first-eye surgeries.
The tetracaine drops used in our study were preservative-free, while proparacaine drops contained 0.01% benzalkonium chloride. It has been suggested that benzalkonium chloride and other preservatives can improve corneal penetration by loosening tight junctions.13 This would be expected to increase the efficacy of the proparacaine drops used in our study. However, more patients in our LASIK sample preferred the preservative-free tetracaine drops to proparacaine.
Corneal epithelial toxicity resulting from prolonged use of topical anesthetics has been well documented, potentially resulting in suppression of epithelial regeneration, in addition to several other unfavorable side effects.14,15 Consideration of corneal epithelial toxicity as a result of topical anesthetic administration is of particular concern following procedures which require epithelial disruption, such as PRK. The importance of both perioperative and postoperative factors for facilitating adequate re-epithelialization and wound healing should always be thoroughly evaluated.
A limitation of this study is that patients were asked for their drop preference at one time point, ie, 30 minutes following their procedure. Our data suggest that tetracaine has a longer duration of action, and that this influenced their preference. It is unclear if patients would have still preferred tetracaine drops if they were asked either immediately after surgery or on the following day. Pain levels at these time points were assessed, and there were no significant differences between tetracaine-treated and proparacaine-treated eyes at these junctures. In addition, utilization of ketorolac preoperatively and postoperatively in the PRK group constituted a confounding variable within our study. Despite ancillary analgesic properties associated with use of ketorolac, our institutional standard of care necessitates use of this medication perioperatively. Further, post-procedural dry eye represented an additional confounding factor, as it likely influenced postoperative pain perception to an unascertainable degree.
This study suggests that while both proparacaine and tetracaine are suitable topical anesthetics for LASIK and PRK surgery, more LASIK patients prefer tetracaine. This preference exists despite the initial stinging that occurs with instillation of tetracaine.
To summarize, patients in the LASIK group described a significant decrease in pain perception 30 minutes postoperatively after intraoperative administration of tetracaine, suggesting that this drop has a longer clinical duration of action in this patient population.
Acknowledgments
This investigation was supported by the University of Utah Study Design and Biostatistics Center, with funding in part from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through grant 8UL1TR000105 (formerly UL1RR025764). Assistance with the statistical analysis was provided by Greg J Stoddard.
Footnotes
Disclosure
The authors have no financial interests to disclose in relation to this work.
References
- 1.Bartfield JM, Holmes TJ, Raccio-Robak N. A comparison of proparacaine and tetracaine eye anesthetics. Acad Emerg Med. 1994;1(4):364–367. doi: 10.1111/j.1553-2712.1994.tb02646.x. [DOI] [PubMed] [Google Scholar]
- 2.Rifkin L, Schaal S. Factors affecting patients’ pain intensity during in office intravitreal injection procedure. Retina. 2012;32(4):696–700. doi: 10.1097/IAE.0b013e3182252ad3. [DOI] [PubMed] [Google Scholar]
- 3.McCaffery M, Pasero C. Pain: Clinical Manual. St Louis, MO, USA: Mosby; 1999. [Google Scholar]
- 4.Suwalsky M, Schneider C, Norris B, et al. The local anesthetic proparacaine modifies sodium transport in toad skin and perturbs the structures of model and cell membranes. Z Naturforsch C. 2002;57(9–10):930–938. doi: 10.1515/znc-2002-9-1029. [DOI] [PubMed] [Google Scholar]
- 5.Müller LJ, Marfurt CF, Kruse F, Tervo TMT. Corneal nerves: structure, contents and function. Exp Eye Res. 2003;76:521–542. doi: 10.1016/s0014-4835(03)00050-2. [DOI] [PubMed] [Google Scholar]
- 6.Nomura K, Singer DE, Aquavella JV. Corneal sensation after topical anesthesia. Cornea. 2001;20(2):191–203. doi: 10.1097/00003226-200103000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Weiss JS, Goren MB. The effect of corneal hypesthesia on the duration of proparacaine anesthetic eyedrops. Am J Ophthalmol. 1991;112(3):326–330. doi: 10.1016/s0002-9394(14)76735-2. [DOI] [PubMed] [Google Scholar]
- 8.Shah NV, Vaddavalli PK, Chow JH, San Roman J, Shi W, Yoo SH. Prospective, double-masked, randomized trial comparing lidocaine gel to tetracaine drops in femtosecond-laser assisted LASIK. J Refract Surg. 2012;28(10):671–672. doi: 10.3928/1081597X-20121001-05. [DOI] [PubMed] [Google Scholar]
- 9.El Rami H, Fadlallah A, Fahd D, Fahed S. Patient-perceived pain during laser in situ keratomileusis: comparison of fellow eyes. J Cataract Refract Surg. 2012;38(3):453–457. doi: 10.1016/j.jcrs.2011.10.028. [DOI] [PubMed] [Google Scholar]
- 10.Cheng AC, Young AL, Law RW, Lam DS. Prospective randomized double-masked trial to evaluate perioperative pain profile in different stages of simultaneous bilateral LASIK. Cornea. 2006;25(8):919–922. doi: 10.1097/01.ico.0000226363.19054.2a. [DOI] [PubMed] [Google Scholar]
- 11.Sharma NS, Ooi JL, Figueira EC, et al. Patient perceptions of second eye clear corneal cataract surgery using assisted topical anaesthesia. Eye (Lond) 2008;22(4):547–550. doi: 10.1038/sj.eye.6702711. [DOI] [PubMed] [Google Scholar]
- 12.Nijkamp MD, Kenens CA, Dijker AJ, Ruiter RA, Hiddema F, Nuijts RM. Determinants of surgery related anxiety in cataract patients. Br J Ophthalmol. 2004;88(10):1310–1314. doi: 10.1136/bjo.2003.037788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kissner A, Spoerl E, Jung R, et al. Pharmacological modification of the epithelial permeability by benzalkonium chloride in UVA/riboflavin corneal collagen cross-linking. Curr Eye Res. 2010;35(8):715–721. doi: 10.3109/02713683.2010.481068. [DOI] [PubMed] [Google Scholar]
- 14.Peyman GA, Rahimy MH, Fernandes ML. Effects of morphine on corneal sensitivity and epithelial wound healing: implications for topical ophthalmic analgesia. Br J Ophthalmol. 1994;78(2):138–141. doi: 10.1136/bjo.78.2.138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grant RL, Acosta D. Comparative toxicity of tetracaine, proparacaine and cocaine evaluated with primary cultures of rabbit corneal epithelial cells. Exp Eye Res. 1994;58(4):469–478. doi: 10.1006/exer.1994.1040. [DOI] [PubMed] [Google Scholar]