Abstract
Background
Threshold and subthreshold forms of generalized anxiety disorder (GAD) are highly prevalent and impairing conditions among adults. However, there are few general population studies that have examined these conditions during the early life course. The primary objectives of this study were to: (1) examine the prevalence, and sociodemographic and clinical characteristics of threshold and subthreshold forms of GAD in a nationally representative sample of US youth; and (2) test differences in sociodemographic and clinical characteristics between threshold and subthreshold forms of the disorder.
Method
The National Comorbidity Survey-Adolescent Supplement is a nationally representative face-to-face survey of 10123 adolescents 13 to 18 years of age in the continental USA.
Results
Approximately 3% of adolescents met criteria for threshold GAD. Reducing the required duration from 6 months to 3 months resulted in a 65.7% increase in prevalence (5.0%); further relaxing the uncontrollability criterion led to an additional 20.7% increase in prevalence (6.1%). Adolescents with all forms of GAD displayed a recurrent clinical course marked by substantial impairment and co-morbidity with other psychiatric disorders. There were few significant differences in sociodemographic and clinical characteristics between threshold and subthreshold cases of GAD. Results also revealed age-related differences in the associated symptoms and clinical course of GAD.
Conclusions
Findings demonstrate the clinical significance of subthreshold forms of GAD among adolescent youth, highlighting the continuous nature of the GAD construct. Age-related differences in the associated symptoms and clinical course of GAD provide further support for criteria that capture variation in clinical features across development.
Keywords: Adolescents, children, epidemiology, generalized anxiety disorder, subthreshold
Introduction
A wealth of research has demonstrated that generalized anxiety disorder (GAD) is a fairly common and impairing condition (for reviews, see Kessler & Wittchen, 2002; Wittchen, 2002; Lieb et al. 2005; Beesdo et al. 2009). Across epidemiological surveys worldwide, lifetime prevalence estimates range from 1.8% to 6.9% among adults (Lieb et al. 2005) and from 0.3% to 5.8% among youth (Beesdo et al. 2009; Merikangas et al. 2010). General population samples across age groups have also shown that GAD is marked by relatively high rates of psychiatric co-morbidity and disability (Lieb et al. 2005; Beesdo et al. 2010; Kessler et al. 2012b).
Despite scientific consensus regarding the scale and burden of GAD in the general population (Kessler & Wittchen, 2002; Wittchen, 2002; Lieb et al. 2005; Beesdo et al. 2010), the diagnostic threshold of GAD continues to pose challenges for investigators and practitioners. For example, data indicate that nearly three-quarters of adults and one-quarter of youth who present for treatment due to clinically significant worry fail to meet GAD criteria by a single criterion, resulting in an anxiety disorder not otherwise specified (NOS) diagnosis (Lawrence & Brown, 2009; Comer et al. 2012a). Because NOS diagnoses are frequently excluded from clinical investigation (Fairburn & Bohn, 2005), relegation to this category may obstruct evidence-based treatment attempts. Further, investigations that have examined the application of less restrictive diagnostic thresholds, including lowering the required duration from 6 months to 3 months and/or 1 month (Kendler et al. 1992; Carter et al. 2001; Hoyer et al. 2002; Kessler et al. 2005b; Angst et al. 2006; Ruscio et al. 2007; Lee et al. 2009; Andrews & Hobbs, 2010) or omitting the requirement of excessiveness and/or uncontrollability of worry (Ruscio et al. 2005; Andrews & Hobbs, 2010), have had relatively little impact on the demographic and clinical features of cases. Thus, there is abundant evidence that the strict application of GAD diagnostic criteria may discount a sizeable proportion of individuals who are functionally impaired and phenotypically similar to individuals who meet full criteria for the disorder.
While the subthreshold concept of GAD has received substantial attention among adults, much less work has focused on this concept during the early life course. To date, only one study of which we are aware has examined both threshold and subthreshold forms of GAD in a young community-based cohort (Beesdo-Baum et al. 2011). Results of this investigation indicated that youth with subthreshold GAD defined by a 3-month duration continued to display elevated psychiatric co-morbidity and disability relative to unaffected youth. Thus far, however, no nationally representative studies of youth have also provided a comprehensive examination of the uncontrollability and associated symptom criteria – two criteria that gained particular interest in the revision process for the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) (Andrews et al. 2010; Andrews & Hobbs, 2010; Hallion & Ruscio, 2013). Indeed, definitional changes under consideration included a shorter required duration (3 months versus 6 months), exclusion of the ‘uncontrollability’ criterion, and reductions in the array of potential associated symptoms, requiring one of either restlessness or muscle tension. The recent rejection of these proposed changes exemplifies some of the uncertainty that has surrounded establishing an appropriate clinical threshold for the disorder. Yet, there remains a noteworthy lack of information on subthreshold manifestations of GAD in young people.
Related, few studies have examined the clinical features and characteristics of threshold GAD in community samples of youth (Andrews et al. 2010). Therefore, relatively little is known about the associated symptoms and clinical course of GAD among adolescents in the general population, and even less is known about how these characteristics may vary across development. Available data from clinical studies suggest that the associated symptoms of GAD differ across age groups (Tracey et al. 1997; Pina et al. 2002). Further, whereas a number of clinical and general population studies have indicated that GAD displays a fairly chronic and persistent course among adults (Kessler & Wittchen, 2002; Wittchen, 2002), community studies of youth reveal only moderate persistence and stability of the disorder across time (Bittner et al. 2007; Angst et al. 2009; Beesdo-Baum et al. 2011; Kessler et al. 2012a). Thus, despite evidence of age-related differences in the associated symptoms and clinical course of GAD, no studies have examined how these characteristics may vary among youth in the adolescent age range.
The goals of the current study were to: (1) examine the prevalence, and sociodemographic and clinical characteristics of threshold and subthreshold forms of GAD in a nationally representative sample of US youth; and (2) test differences in sociodemographic and clinical characteristics between threshold and sub-threshold forms of the disorder. In consideration of work that has found associated symptoms and course characteristics to vary across development (Tracey et al. 1997; Pina et al. 2002; Beesdo-Baum et al. 2011), we also investigated differences in these features across age for all forms of GAD.
Method
Sample and procedure
The National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) is a nationally representative face-to-face survey of 10123 adolescents aged 13–18 years in the continental USA. Information concerning the sampling strategy, participation rates and instruments in the NCS-A can be found in greater detail elsewhere (Kessler et al. 2009; Merikangas et al. 2009). The survey was carried out in a dual-frame sample that included a household subsample (n=879) and a school subsample (n=9244). The adolescent response rate of the combined subsamples was 82.9%. Minor differences in sample and population distributions of census sociodemographic and school characteristics were corrected with post-stratification weighting (Kessler et al. 2009).
One parent/parent surrogate of each participating adolescent was mailed a self-administered questionnaire (SAQ) to collect information on adolescent mental/physical health and other family- and community-level factors. The full SAQ was completed by 6483 parents. All recruitment and consent procedures were approved by the human subjects committees of Harvard Medical School and the University of Michigan.
Measures
Diagnostic assessment
Adolescents were administered a modified World Health Organization Composite International Diagnostic Interview Version 3.0, a fully structured interview of Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) diagnoses (Kessler & Ustun, 2004). Specific details concerning the diagnostic assessment can be found in previous reports (Merikangas et al. 2011; Burstein et al. 2012). Definitions of all psychiatric disorders adhered to DSM-IV criteria; however, diagnostic hierarchy rules were not applied to permit examinations of overlap between GAD and other disorders.
GAD definitions
Adolescents who endorsed DSM-IV/5 GAD criteria, including excessive anxiety or worry, occurring more days than not for at least 6 months, about more than one event or activity, were defined as threshold GAD cases (GAD-6mo). Subthreshold definitions of GAD included: (1) GAD-3mo, for which episode duration was relaxed to at least 3 months; and (2) GAD-3mo, no uncontrollability (GAD-3mo/NOU), for which duration was relaxed to at least 3 months and the uncontrollability criterion was not applied. For the purposes of conducting statistical comparisons between threshold and subthreshold forms of GAD, comparable mutually exclusive groups were also created: (1) GAD-3-5mo cases endorsed symptoms for durations of at least 3 months and less than 6 months; and (2) GAD-3-5mo, no uncontrollability (GAD-3-5mo/NOU) cases endorsed symptoms for durations of at least 3 months and less than 6 months and the uncontrollability criterion was not applied. Past-year cases of threshold and subthreshold GAD included adolescents who met specified criteria and also endorsed extensive or impairing symptoms in the past 12 months.
Clinical features
Associated symptoms
Adolescents were asked if they often experienced any associated symptoms during episodes of worry, including: restlessness, getting easily fatigued, difficulty concentrating, irritability, muscle tension, and sleep disturbance. Associated symptoms were summed to reflect the number of associated symptoms present in each adolescent. Given recent interest in limiting the array of associated symptoms to restlessness and muscle tension (Andrews & Hobbs, 2010), these two symptoms were also examined in isolation.
Course characteristics
Course characteristics included age-of-onset information, obtained from adolescents using an assessment procedure created to enhance retrospective recall (Knauper et al. 1999) and the prevalence ratio (past year of lifetime). Adolescents were also asked about episodes of GAD that were of at least 1 month in duration, including the number of past-year episodes, the number of lifetime episodes, and the longest lifetime episode. The proportion of time in episode since onset was also calculated using this information.
Severity and impairment
Several indices of severity and impairment were included in the current study: ‘severe cases’, defined by higher thresholds that required endorsement of ‘severe’ or ‘very severe’ distress and ‘a lot’ or ‘extreme’ impairment in daily activities (Merikangas et al. 2010); ‘past-year impairment’, derived from the maximum degree of disability adolescents reported at home, school/work, in their family relations, or social life, ranging from 0 to 10 (Leon et al. 1997); ‘days out of role’, estimated from the total number of days in the past year that adolescents were completely unable to function because of their worry; ‘GAD treatment contact’, for which adolescents endorsed seeking professional treatment for GAD (e.g. from psychologists, counselors, or other healing professionals); ‘other anxiety treatment contact’, for which adolescents endorsed seeking professional treatment for any other anxiety disorder; and ‘any lifetime treatment’, for which adolescents endorsed receiving services for any emotional or behavioral problem (e.g. mental health specialty, general medical, or school services). More detailed information about treatment contact and the types of services assessed has been described elsewhere (Merikangas et al. 2011).
Statistical analysis
All statistical analyses were completed in the SAS software package version 9.3 (SAS Institute Inc., USA; SAS Institute, 2008). Cross-tabulations were used to calculate estimates of prevalence and clinical features and means were used for continuous clinical characteristics. Age-specific incidence curves were generated using the Kaplan–Meier method. Multivariate logistic regression analysis was performed to examine sociodemographic correlates of the prevalence of GAD definitions. Regression models of associated symptom and course characteristics adjusted for significant sociodemographic characteristics; regression models of indices of severity and impairment and psychiatric co-morbidity adjusted for all significant sociodemographic variables and other psychiatric disorders simultaneously. Adjusted odds ratios (aORs) were the exponentiated values of multivariate logistic regression coefficients. 95% Confidence intervals (95% CIs) of aORs were calculated based on design-adjusted variances. The design-adjusted Wald χ2 test or F test was used to examine differences between threshold and subthreshold definitions of GAD. Statistical significance was based on two-sided tests evaluated at the 0.05 level of significance.
Results
Prevalence and sociodemographic correlates
The lifetime prevalence and sociodemographic correlates of GAD are presented by threshold and sub-threshold definitions in Table 1. Approximately 3.0% of adolescents met criteria for GAD-6mo in their lifetime, whereas 5.0% of adolescents were affected with GAD-3mo and 6.1% of adolescents were affected with GAD-3mo/NOU. Thus, relaxing the required duration of GAD resulted in a 65.7% increase in prevalence and further relaxing the uncontrollability criterion resulted in an additional 20.7% increase in prevalence.
Table 1.
Prevalence and sociodemographic characteristics of threshold and subthreshold GAD
| Characteristics | GAD definition
|
|||||
|---|---|---|---|---|---|---|
| GAD-6mo (n=284)
|
GAD-3mo (n=463)
|
GAD-3mo/NOU (n=545)
|
||||
| % (S.E.) | aOR (95% CI)a | % (S.E.) | aOR (95% CI)a | % (S.E.) | aOR (95% CI)a | |
| Total | 3.03 (0.38) | – | 5.02 (0.49) | – | 6.06 (0.51) | – |
| Sex | ||||||
| Male | 1.86 (0.32) | 1.00 | 3.28 (0.42) | 1.00 | 4.60 (0.49) | 1.00 |
| Female | 4.25 (0.67) | 2.26 (1.44–3.57) | 6.85 (0.87) | 2.11 (1.48–3.02) | 7.59 (0.88) | 1.66 (1.23–2.25) |
| Wald | 12.42 (0.0004) | 16.75 (<0.0001) | 10.89 (0.0010) | |||
| Age | ||||||
| 13–14 years | 1.36 (0.36) | 1.00 | 2.66 (0.41) | 1.00 | 3.71 (0.48) | 1.00 |
| 15–16 years | 3.75 (0.62) | 2.65 (1.47–4.77) | 6.12 (0.85) | 2.26 (1.52–3.35) | 6.97 (0.82) | 1.89 (1.36–2.62) |
| 17–18 years | 4.37 (0.56) | 3.26 (1.86–5.72) | 6.83 (0.83) | 2.65 (1.83–3.83) | 8.17 (1.03) | 2.31 (1.64–3.25) |
| Wald | 16.97 (0.0002) | 29.21 (<0.0001) | 27.53 (<0.0001) | |||
| Race/ethnicity | ||||||
| Non-Hispanic white | 3.54 (0.50) | 1.00 | 5.40 (0.63) | 1.00 | 6.34 (0.73) | 1.00 |
| Hispanic | 1.86 (0.40) | 0.57 (0.36–0.91) | 3.67 (0.56) | 0.73 (0.50–1.05) | 4.71 (0.54) | 0.76 (0.54–1.07) |
| Non-Hispanic black | 2.70 (0.59) | 0.81 (0.48–1.37) | 4.94 (0.71) | 0.97 (0.74–1.29) | 6.04 (0.75) | 0.97 (0.72–1.32) |
| Other | 1.74 (0.30) | 0.54 (0.37–0.80) | 4.21 (1.15) | 0.84 (0.45–1.56) | 6.17 (1.61) | 1.03 (0.57–1.87) |
| Wald | 14.34 (0.0025) | 3.93 (0.2694) | 2.91 (0.4058) | |||
| Poverty index ratio | ||||||
| >6 | 2.73 (0.42) | 1.00 | 4.98 (0.58) | 1.00 | 5.59 (0.58) | 1.00 |
| ≤6 | 3.68 (0.56) | 1.40 (0.99–1.96) | 5.89 (0.74) | 1.22 (0.95–1.57) | 7.07 (0.79) | 1.32 (1.04–1.66) |
| ≤3 | 3.15 (0.82) | 1.28 (0.79–2.08) | 4.60 (0.85) | 0.98 (0.66–1.46) | 5.52 (0.93) | 1.05 (0.72–1.53) |
| ≤1.5 | 2.14 (0.50) | 0.92 (0.50–1.72) | 3.82 (0.56) | 0.84 (0.58–1.22) | 5.64 (0.65) | 1.11 (0.80–1.53) |
| Wald | 6.37 (0.0949) | 6.45 (0.0915) | 6.55 (0.0877) | |||
GAD, Generalized anxiety disorder; DSM, Diagnostic and Statistical Manual of Mental Disorders; GAD-6mo, cases met DSM-IV/5 GAD criteria; GAD-3mo, duration was relaxed to at least 3 months; GAD-3mo/NOU, duration was relaxed to at least 3 months and uncontrollability criterion was not applied; S.E., standard error; aOR, adjusted odds ratio; CI, confidence interval.
aORs and 95% CIs include all sociodemographic predictors.
The prevalence of GAD-6mo was significantly associated with sex, such that female adolescents were twice as likely to be affected with this condition relative to male adolescents (aOR=2.26, 95% CI 1.44–3.57). GAD-6mo also increased uniformly with age, demonstrating a 3-fold increase from the youngest to the oldest age group (aOR=3.26, 95% CI 1.86–5.72). Similar sociodemographic correlates were also observed for subthreshold forms of GAD, and effects were comparable in magnitude and direction. Of exception, race/ethnicity was significantly associated only with GAD-6mo, with both Hispanic adolescents (aOR=0.57, 95% CI 0.36–0.91) and adolescents of other racial/ethnic minority groups (aOR=0.54, 95% CI 0.37–0.80) being less likely to meet criteria relative to non-Hispanic white adolescents. Paralleling these results, there were no differences between mutually exclusive GAD groups in sociodemographic correlates including sex, age or poverty. However, adolescents of other racial/ethnic minority groups were more likely to be affected with either subthreshold form of GAD (GAD-5mo or GAD-5mo/NOU) relative to non-Hispanic white adolescents (all p<0.05; online Supplementary Table S1).
Associated symptom and course characteristics
The associated symptom and course characteristics of GAD among threshold and subthreshold cases are presented in Table 2. Among GAD-6mo cases, the most frequently endorsed associated symptom was poor concentration (83.4%), followed by irritability (71.5%) and restlessness (71.3%). By contrast, the least commonly endorsed associated symptom was muscle tension (46.7%). Nearly one-quarter of adolescents who met all other criteria for GAD-6mo failed to endorse either restlessness or muscle tension. Relative to GAD-6mo cases, frequencies of associated symptoms among cases with subthreshold forms of GAD were fairly similar. However, examination of differences in associated symptoms across mutually exclusive definitions of GAD indicated that a higher proportion of GAD-3-5mo cases endorsed restlessness relative to GAD-6mo cases (aOR=3.00, 95% CI 1.54–5.85; online Supplementary Table S2).
Table 2.
Associated symptoms and course characteristics of GAD among threshold and subthreshold cases
| GAD definition
|
|||
|---|---|---|---|
| GAD-6mo (n=284) | GAD-3mo (n=463) | GAD-3mo/NOU (n=545) | |
| Associated symptoms | |||
| Restlessness, % (S.E.) | 71.30 (4.42) | 76.81 (2.95) | 74.93 (2.77) |
| Easily fatigued, % (S.E.) | 55.78 (3.46) | 57.72 (3.55) | 57.57 (3.70) |
| Difficulty concentrating, % (S.E.) | 83.41 (3.05) | 83.88 (2.17) | 82.94 (2.77) |
| Irritable, % (S.E.) | 71.51 (4.16) | 72.88 (2.79) | 71.53 (2.64) |
| Muscle tension, % (S.E.) | 46.74 (3.47) | 46.54 (2.79) | 45.07 (2.73) |
| Sleep disturbance, % (S.E.) | 70.05 (3.04) | 70.06 (2.51) | 70.83 (2.54) |
| Either restlessness or muscle tension, % (S.E.) | 77.83 (3.47) | 82.59 (2.34) | 82.03 (2.14) |
| One symptom, % (S.E.) | 7.02 (2.64) | 5.30 (1.63) | 4.73 (1.43) |
| Two symptoms, % (S.E.) | 12.49 (2.41) | 13.13 (1.61) | 14.65 (1.86) |
| Three symptoms, % (S.E.) | 13.90 (3.09) | 14.21 (2.95) | 16.23 (3.02) |
| Four symptoms, % (S.E.) | 29.11 (4.82) | 25.51 (3.53) | 23.68 (3.32) |
| Five symptoms, % (S.E.) | 17.60 (2.66) | 20.11 (2.47) | 19.44 (2.38) |
| Six symptoms, % (S.E.) | 19.89 (3.17) | 21.74 (2.62) | 21.27 (2.31) |
| Mean number of symptoms (S.E.) | 3.97 (0.14) | 4.07 (0.10) | 4.02 (0.09) |
| Course characteristics | |||
| Median age at onset, years (S.E.) | 11.83 (0.35) | 11.96 (0.36) | 11.94 (0.35) |
| Prevalence ratio, % (S.E.) | 53.92 (4.08) | 53.36 (4.03) | 50.09 (3.11) |
| Mean number of past-year episodes (S.E.)a | 2.13 (0.17) | 2.20 (0.12) | 2.35 (0.13) |
| Mean number of lifetime episodes (S.E.)a | 6.86 (0.73) | 6.13 (0.54) | 6.84 (0.97) |
| Mean longest lifetime episode, months (S.E.)a | 43.37 (6.31) | 27.47 (4.50) | 27.61 (4.01) |
| Mean time in episode since onset, months (S.E.)a | 65.72 (4.25) | 49.14 (3.66) | 49.57 (2.92) |
GAD, generalized anxiety disorder; DSM, Diagnostic and Statistical Manual of Mental Disorders; GAD-6mo, cases met DSM-IV/5 GAD criteria; GAD-3mo, duration was relaxed to at least 3 months; GAD-3mo/NOU, duration was relaxed to at least 3 months and uncontrollability criterion was not applied; S.E., standard error.
An episode was defined as at least 1 month in duration.
With reference to course characteristics, the median age of onset of GAD-6mo was approximately 12 years of age (median=11.83 years). The condition displayed a moderate level of persistence, with past-year GAD-6mo being present in a little over half of youth who had experienced the disorder in their lifetime (n=169, 53.9%). On average, adolescents who had met criteria for GAD-6mo experienced two episodes of at least 1 month’s duration in the past year (mean=2.13 episodes) and approximately seven episodes of at least 1 month’s duration in their lifetime (mean=6.86 episodes), with their longest lifetime episode being greater than 3 years (mean=43.37 months).
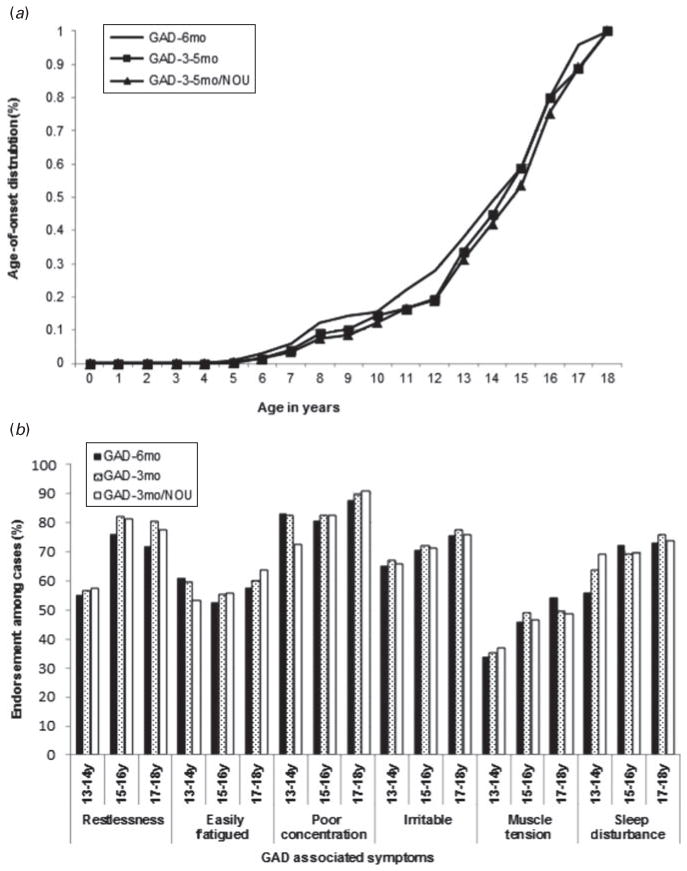
Examination of differences in course characteristics across mutually exclusive definitions of GAD yielded several significant effects. There were significant differences in the survival functions across groups (see Fig. 1a), indicating that youth with GAD-6mo had a younger age of onset (median=11.83 years) than did youth with GAD-3-5mo (median=13.00 years; log-rank test: Wald , p <0.0001) and youth with GAD-3-5mo/NOU (median=13.00 years; log-rank test: Wald , p<0.0001). Thus, although some cases developed GAD as early as 6 years of age, the incidence increased sharply after age 10 years among threshold GAD cases, and after age 12 years among subthreshold GAD cases. In addition, youth with subthreshold forms of GAD displayed shorter lifetime episodes and spent a smaller proportion of their time in episode, while experiencing a greater number of past-year and lifetime episodes, relative to GAD-6mo (all p<0.0001; online Supplementary Table S2).
Fig. 1.
(a) Standardized cumulative lifetime prevalence of threshold and subthreshold forms of generalized anxiety disorder (GAD). (b) Associated symptom endorsement among GAD threshold and subthreshold cases by adolescent age group. GAD-6mo, cases met Diagnostic and Statistical Manual of Mental Disorders (DSM)-IV/5 GAD criteria; GAD-3-5mo, duration was ≥3 months and <6 months; GAD-3-5mo/NOU, duration was ≥3 months and <6 months and uncontrollability criterion was not applied; GAD-3mo, duration was relaxed to at least 3 months; GAD-3mo/NOU, duration was relaxed to at least 3 months and uncontrollability criterion was not applied; y, years.
There were also a number of significant differences in associated symptoms and course characteristics by adolescent age group (see Fig. 1b and online Supplementary Table S3). The most consistent effects across age were observed for restlessness and the number of associated symptoms. In particular, among both GAD-3mo and GAD-3mo/NOU cases, a significantly lower proportion of the 13- to 14-year age group endorsed restlessness (56.8% and 57.5%, respectively) relative to the 15- to 16-year age group (82.2% and 81.5%, respectively) and the 17- to 18-year age group (80.5% and 77.4%, respectively; all p<0.01). Further, among both GAD-3mo and GAD-3mo/NOU cases, the 13- to 14-year age group endorsed fewer associated symptoms (mean=3.6) than did the 15- to 16-year age group (mean=4.1) and the 17- to 18-year age group (mean=4.3; all p<0.05). With respect to course characteristics, there were significant differences in the survival functions across age groups for all forms of GAD, indicating a linear effect whereby earlier ages of onset were observed among younger cohorts (all p’s< 0.0001). Further, among all forms of GAD, the youngest adolescents had a significantly greater number of episodes of at least 1 month in duration in the past year relative to older adolescents, suggesting episodes that occurred with greater frequency (all p’s<0.05).
Severity and impairment
Indices of severity and impairment among the three mutually exclusive GAD groups are displayed in Table 3. On average, adolescents with GAD-6mo reported a degree of disability in the moderate to severe range (mean=6.94) and indicated being totally unable to function for approximately 7 days out of the last calendar year (mean=7.37 days). Despite this, only a little over one-third of these adolescents had sought treatment for the disorder in their lifetime (37.25%). In general, indices of severity and impairment were slightly lower in magnitude among sub-threshold cases. However, there were few significant differences between threshold and subthreshold forms of GAD, indicating comparable levels of clinical severity and disability across the three groups. Of exception, the GAD-3-5mo/NOU cases were less likely to obtain treatment for GAD than were the GAD-6mo cases (aOR=0.46, 95% CI 0.23–0.89). Conversely, a significantly greater number of days out of role was observed among GAD-3-5mo (mean =8.23 days) and GAD3-5mo/NOU cases (mean=7.50 days) relative to GAD-6mo cases (both p<0.05). Further demonstrating the clinical significance of sub-threshold forms of GAD, cases uniformly displayed significantly higher ratings across almost all indices of severity and impairment relative to unaffected adolescents (all p<0.05; online Supplementary Table S4).
Table 3.
Severity and impairment across GAD mutually exclusive groupsa
| Severity and impairment | GAD mutually exclusive definition
|
Comparisons of mutually exclusive GAD groups
|
|||
|---|---|---|---|---|---|
| Weighted rate
|
Adjusted odds ratio (95% CI)
|
||||
| GAD-6mo (n=284) | GAD-3–5mo (n=179) | GAD-3–5mo/NOU (n=214) | GAD-3–5mo v. GAD-6mo | GAD-3–5mo/NOU v. GAD-6mo | |
| Severe cases, % (S.E.) | 42.04 (4.25) | 35.62 (5.71) | 32.45 (5.64) | 0.82 (0.45–1.49) | 0.76 (0.41–1.40) |
| Wald | 0.43 (0.5112) | 0.79 (0.3742) | |||
| Mean past-year impairment (S.E.) | 6.94 (0.21) | 6.50 (0.53) | 6.52 (0.49) | – | – |
| Wald F1 (p) | 2.56 (0.1178) | 0.44 (0.5098) | |||
| Mean days out of role (S.E.) | 7.37 (1.60) | 8.23 (2.69) | 7.50 (2.46) | – | – |
| Wald F1 (p) | 13.81 (0.0006) | 6.05 (0.0185) | |||
| GAD treatment contact, % (S.E.) | 37.25 (3.37) | 22.34 (4.46) | 18.61 (3.85) | 0.56 (0.28–1.12) | 0.46 (0.23–0.89) |
| Wald | 2.67 (0.1021) | 5.37 (0.0205) | |||
| Other anxiety treatment contact, % (S.E.) | 26.13 (2.75) | 17.20 (4.44) | 15.03 (3.86) | 0.71 (0.33–1.53) | 0.57 (0.31–1.05) |
| Wald | 0.77 (0.3807) | 1.34 (0.2478) | |||
| Any lifetime treatment, % (S.E.) | 53.69 (3.74) | 46.16 (5.21) | 42.22 (4.95) | 0.90 (0.53–1.53) | 0.79 (0.48–1.30) |
| Wald | 0.16 (0.6898) | 0.85 (0.3570) | |||
GAD, Generalized anxiety disorder; CI, confidence interval; DSM, Diagnostic and Statistical Manual of Mental Disorders; GAD-6mo, cases met DSM-IV/5 GAD criteria; GAD-3-5mo, duration was ≥3 months and <6 months; GAD-3-5mo/NOU, duration was ≥3 months and <6 months and uncontrollability criterion was not applied; S.E., standard error.
Regression models controlled for all significant sociodemographic predictors (sex, age, race) and other psychiatric disorders (but the disorder of interest).
Psychiatric co-morbidity
The lifetime co-morbidity of GAD with other psychiatric disorders is presented by threshold and subthres-hold definitions in Table 4. GAD-6mo displayed significant associations only with other anxiety and mood disorders, and was most often associated with other anxiety disorders, with nearly two-thirds of these adolescents also affected with another anxiety disorder in their lifetime (65.8%). Among the anxiety disorders, GAD-6mo was most likely to be co-morbid with specific phobia (40.71%), followed by separation anxiety disorder (20.95%), posttraumatic stress disorder (PTSD) (20.59%) and social phobia (20.08%). More than half of youth with GAD-6mo also met criteria for a mood disorder in their lifetime (58.55%).
Table 4.
Associations of threshold and subthreshold GAD with other mental disorders
| GAD definition
|
||||||
|---|---|---|---|---|---|---|
| GAD-6mo
|
GAD-3mo
|
GAD-3mo/NOU
|
||||
| % (S.E.) | aOR (95% CI)a | % (S.E.) | aOR (95% CI)a | % (S.E.) | aOR (95% CI)a | |
| Mental disorders | ||||||
| Any anxiety disorder | 65.80 (4.83) | 4.41 (2.91–6.69) | 64.27 (3.20) | 3.83 (2.68–5.47) | 61.16 (3.06) | 3.95 (2.74–5.68) |
| Specific phobia | 40.71 (2.81) | 2.15 (1.43–3.23) | 34.55 (2.10) | 1.91 (1.44–2.55) | 32.08 (2.51) | 1.76 (1.32–2.34) |
| Social phobia | 20.08 (3.82) | 2.32 (1.32–4.07) | 21.59 (2.79) | 3.00 (1.77–5.07) | 20.51 (2.58) | 2.64 (1.60–4.34) |
| Agoraphobia | 10.94 (2.58) | 1.79 (0.95–3.40) | 10.24 (2.63) | 2.03 (1.12–3.68) | 9.43 (2.28) | 1.77 (1.07–2.94) |
| Panic disorder | 10.12 (2.37) | 2.08 (0.88–4.91) | 9.67 (1.86) | 2.77 (1.44–5.33) | 9.77 (1.74) | 3.25 (1.61–6.54) |
| Separation anxiety disorder | 20.95 (4.01) | 2.90 (1.47–5.72) | 21.62 (3.08) | 2.67 (1.52–4.71) | 20.68 (2.79) | 2.70 (1.55–4.71) |
| PTSD | 20.59 (4.21) | 2.88 (1.79–4.64) | 19.70 (3.11) | 2.05 (1.31–3.20) | 18.48 (2.56) | 2.33 (1.33–4.08) |
| Any mood disorder | 58.55 (4.31) | 3.52 (1.99–6.22) | 54.02 (3.39) | 3.95 (2.75–5.66) | 51.42 (3.53) | 4.08 (2.95–5.65) |
| Major depression | 54.41 (4.51) | 2.69 (1.51–4.80) | 48.30 (3.49) | 3.02 (1.96–4.64) | 45.44 (3.38) | 2.82 (1.96–4.06) |
| Dysthymia | 22.61 (3.76) | 2.84 (1.63–4.94) | 17.46 (2.81) | 1.89 (1.15–3.12) | 17.27 (2.55) | 2.17 (1.38–3.41) |
| Bipolar disorder | 7.94 (1.71) | 0.67 (0.31–1.47) | 10.28 (1.77) | 1.59 (0.93–2.71) | 10.78 (2.16) | 2.23 (1.28–3.87) |
| Any behavior disorderb | 39.22 (6.07) | 1.40 (0.69–2.83) | 36.66 (4.19) | 1.38 (0.83–2.28) | 35.37 (3.37) | 1.18 (0.76–1.83) |
| ODDb | 22.88 (4.52) | 1.29 (0.59–2.81) | 19.62 (2.76) | 1.07 (0.61–1.87) | 19.41 (2.45) | 1.05 (0.63–1.73) |
| Conduct disorderb | 21.12 (3.68) | 0.76 (0.33–1.76) | 20.90 (3.40) | 0.99 (0.44–2.22) | 19.87 (2.88) | 0.80 (0.37–1.72) |
| ADHDb | 16.78 (2.88) | 1.57 (0.84–2.92) | 15.29 (2.05) | 1.39 (0.90–2.15) | 9.64 (1.32) | 1.47 (0.99–2.18) |
| Any substance use disorder | 23.61 (3.83) | 1.62 (0.92–2.83) | 23.06 (3.09) | 1.13 (0.69–1.86) | 24.37 (2.80) | 1.41 (0.85–2.34) |
| Alcohol use disorders | 14.58 (3.16) | 1.61 (0.61–4.24) | 16.46 (3.02) | 1.34 (0.62–2.88) | 15.63 (2.34) | 1.23 (0.58–2.18) |
| Drug use disorders | 17.26 (3.02) | 1.10 (0.49–2.47) | 18.25 (2.42) | 0.94 (0.50–1.78) | 20.35 (2.19) | 1.38 (0.86–2.24) |
GAD, Generalized anxiety disorder; DSM, Diagnostic and Statistical Manual of Mental Disorders; GAD-6mo, cases met DSM-IV/5 GAD criteria; GAD-3mo, duration was relaxed to at least 3 months; GAD-3mo/NOU, duration was relaxed to at least 3 months and uncontrollability criterion was not applied; S.E., standard error; aOR, adjusted odds ratio; CI, confidence interval; PTSD, posttraumatic stress disorder, ODD, oppositional defiant disorder; ADHD, attention deficit–hyperactivity disorder.
aORs and 95% CIs include all significant sociodemographic predictors and other psychiatric disorders (but the disorder of interest).
Reports based on parent self-administered questionnaire sample (n=6483).
Associations between subthreshold forms of GAD and other psychiatric disorders were remarkably similar to GAD-6mo and remained circumscribed to the classes of anxiety and mood disorders. However, as is shown, subthreshold forms of GAD tended to display associations with a wider range of anxiety and mood disorders and co-morbidity rates were slightly lower. Analysis of psychiatric correlates by mutually exclusive GAD groups indicated that PTSD, dysthymia and ADHD were less common among subthreshold cases relative to GAD-6mo cases, whereas the reverse was true for bipolar disorder (all p<0.05; online Supplementary Table S5).
Discussion
Summary of findings
Paralleling prior work among adults (Kessler & Wittchen, 2002; Wittchen, 2002; Lieb et al. 2005; Angst et al. 2006 2009) and a handful of studies among youth (Beesdo et al. 2009, 2010), this nationally representative study indicates that GAD is a prevalent condition among adolescents, and one that is characterized by a high degree of psychiatric co-morbidity, disability, and impairment. Furthermore, the current study provides important information on the diagnostic threshold of GAD in this young age group, highlighting both the clinical significance of subthreshold forms of GAD, as well as the continuous nature of the GAD construct. Beyond displaying similar socio-demographic and clinical correlates to adolescents who met full criteria for the disorder, adolescents with subthreshold forms of GAD experienced significantly greater impairment, disability and psychiatric co-morbidity relative to unaffected youth. Thus, given our observation of lower rates of treatment among adolescents with subthreshold forms of GAD, these data indicate that there may be a substantial number of young people who are impaired, but who are not currently recognized or treated due to failure to meet full GAD criteria. Finally, our observation of age-related differences in the associated symptoms and clinical course of GAD further highlights the need for criteria sets that are sensitive to developmental differences in symptom expression.
Prevalence and sociodemographic correlates
We found that approximately 3% of youth in the general population were affected with GAD, and 6% were affected with the broad phenotype of either threshold or subthreshold GAD at some point during their lifetime. The prevalence rate of GAD observed in this study is within the range of estimates of other community-based studies of youth (Costello et al. 1996; Beesdo et al. 2009; Merikangas et al. 2010), and indicates that even when it is narrowly defined, GAD is a relatively common condition among adolescents. Significant associations between GAD and socio-demographic characteristics including sex and age replicate past studies that have found this disorder to be disproportionately high among females (Lieb et al. 2005; Beesdo-Baum et al. 2011) and to increase in prevalence between childhood and young adulthood (Beesdo-Baum et al. 2011). Although there were no differences in the majority of sociodemographic characteristics across threshold and subthreshold definitions of GAD, adolescents of other racial/ethnic minority groups were less likely to present with threshold GAD due to a failure to meet the 6-month duration requirement. Taken together with general population studies of adults that have found lower prevalence rates of GAD among ethnic minority groups when the 6-month duration criterion is strictly applied (Grant et al. 2005; Kessler et al. 2005b), these findings suggest that individuals of certain racial/ethnic minority groups may experience shorter episodes of GAD. Thus, in addition to the numerous barriers that contribute to racial/ethnic disparities in service use (Wu et al. 2001), the failure to account for alternative manifestations of disorder among minority groups may serve as yet another obstacle.
Associated symptoms and clinical course
Several findings related to the associated symptoms and course of GAD are also noteworthy. Consistent with previous clinical studies of affected youth (Pina et al. 2002; Kendall & Pimentel, 2003; Comer et al. 2012b), in this general population sample of adolescents, poor concentration, restlessness, and irritability were the most common associated symptoms of GAD, while muscle tension was the least common symptom. Further, we found that nearly one-quarter of youth meeting all other criteria for GAD failed to endorse either restlessness or muscle tension, indicating that a substantial proportion of youth would fail to be identified if the array of associated symptoms were restricted to these domains. Thus, in line with one study of clinically referred youth (Comer et al. 2012b), the current study supports the decision to retain all associated symptoms of GAD in the DSM-5.
This decision is further justified by our observation of differences in the frequency of associated symptoms across adolescent age groups. In particular, while restlessness was one of the most common symptoms of GAD overall, it was significantly less common among younger versus older adolescents, with only about half of youth in the youngest age group endorsing this symptom. Likewise, although irritability was common among youth with GAD in the present sample of adolescents, it was relatively uncommon in a school-based sample of children between the ages of 7 and 11 years (Layne et al. 2009), suggesting that irritability may become a more prominent symptom of GAD as children enter adolescence. Finally, in agreement with prior clinical studies of youth that have found the number of associated symptoms of GAD to increase with age (Tracey et al. 1997; Kendall & Pimentel, 2003), younger adolescents had fewer associated symptoms than did older adolescents, supporting the lower threshold of only one associated symptom in children and adolescents. Such results further make a case for criteria sets that yield to age-related differences in symptom manifestation.
With regard to course characteristics, we found that youth developed GAD fairly early in adolescence, with a median age of onset of 12 years. While the age of onset revealed in this study is earlier than other studies involving adults (Kessler et al. 2005a; Beesdo et al. 2010), it is probable that this is due to the inability of the NCS-A sample to account for incident cases in adulthood. Moreover, the onset of GAD probably follows a bimodal distribution, with core periods of risk in both adolescence and adulthood (Kessler et al. 2005a; Beesdo et al. 2010). Also of interest, even in their young lifetime, affected adolescents experienced several episodes of GAD of various durations and displayed only moderate persistence of the disorder. Thus, in contrast to the chronic course of GAD that has been observed among adults (Kessler & Wittchen, 2002; Wittchen, 2002), GAD in young people may be better characterized by an episodic and/or recurrent course, as has been demonstrated by other prospective (Bittner et al. 2007; Beesdo-Baum et al. 2011) and cross-sectional studies of youth (Kessler et al. 2012a). However, it is important to note that individuals with threshold GAD displayed an earlier age of onset and longer episodes than did youth with subthreshold forms of GAD, indicating that threshold GAD may be typified by greater severity and chronicity than subthreshold GAD (Kessler et al. 2005b; Lee et al. 2009; Beesdo-Baum et al. 2011).
Severity, impairment, and psychiatric co-morbidity
In accordance with earlier general population studies of youth (Essau et al. 2000; Beesdo-Baum et al. 2011), adolescents with GAD displayed substantial impairment and disability, and high rates of co-morbidity with other psychiatric disorders. Further, consistent with numerous studies of adults (Kendler et al. 1992; Carter et al. 2001; Hoyer et al. 2002; Kessler et al. 2005b; Angst et al. 2006; Ruscio et al. 2007; Lee et al. 2009; Andrews & Hobbs, 2010) and one prior investigation including youth (Beesdo-Baum et al. 2011), our findings document the clinical significance of subthreshold forms of GAD during adolescence. In addition to demonstrating similar clinical correlates to youth who met full criteria for the disorder, adolescents with subthreshold forms of GAD exhibited significantly higher levels of impairment, disability, and psychiatric co-morbidity than did youth who were not affected with these conditions. Coupled with the higher degree of persistence experienced by adolescents with threshold GAD, such findings suggest that GAD may be conceptualized as a dimensional or continuous construct, as has been found by previous investigations (Kessler et al. 2005b; Ruscio et al. 2007; Lee et al. 2009; Beesdo-Baum et al. 2011). While the continuous nature of the condition makes the application of a dichotomous threshold challenging, it is notable that the modifications to criteria that were investigated in the current study continued to distinguish a clinically impaired subgroup of youth.
Limitations and strengths
It is necessary to consider these results in the context of several study limitations. First, the design of the NCS-A study is cross-sectional, and as such, data on course characteristics may be subject to retrospective reporting biases. Although a number of procedures were implemented to improve the accuracy of retrospective recall (Knauper et al. 1999), it is unlikely that these procedures resulted in estimates that are entirely without error. Future prospective studies that investigate threshold and subthreshold manifestations of GAD across time will provide much needed longitudinal information on the course of GAD among youth in the general population. Second, because the age of the NCS-A sample is limited to the period of adolescence, the clinical features of GAD revealed in the current study may not generalize to children of younger ages, and the age-related differences in these features are probably conservative. It will be important for additional work to investigate how clinical features of GAD may vary across the entire early life course. Finally, although this study provides data on the frequency of associated symptoms of GAD, our data do not indicate which symptoms may contribute most to a GAD diagnosis. These limitations notwithstanding, the current study is the first to examine the clinical features and characteristics of GAD in a nationally representative sample of US youth. It is also among the first to investigate the diagnostic threshold of GAD during this early developmental period. In view of the current study findings, it will be important to consider that the distress and impairment experienced by adolescents with subthreshold GAD is often comparable with that of those who meet full criteria for the disorder, and no less worthy of professional or scientific attention.
Supplementary Material
Acknowledgments
The NCS-A was carried out in conjunction with the World Health Organization World Mental Health (WMH) Survey Initiative. The views and opinions expressed in this article are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies or the US government.
The NCS-A was funded by the National Institute of Mental Health (no. ZIA MH002808-11 and no. U01-MH60220), and the National Institute of Drug Abuse (no. R01-DA016558). This work was supported by the Intramural Research Program of the National Institute of Mental Health.
Footnotes
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S0033291713002997
Declaration of Interest
None.
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
References
- Andrews G, Hobbs MJ. The effect of the draft DSM-5 criteria for GAD on prevalence and severity. Australian and New Zealand Journal of Psychiatry. 2010;44:784–790. doi: 10.3109/00048671003781798. [DOI] [PubMed] [Google Scholar]
- Andrews G, Hobbs MJ, Borkovec TD, Beesdo K, Craske MG, Heimberg RG, Rapee RM, Ruscio AM, Stanley MA. Generalized worry disorder: a review of DSM-IV generalized anxiety disorder and options for DSM-V. Depression and Anxiety. 2010;27:134–147. doi: 10.1002/da.20658. [DOI] [PubMed] [Google Scholar]
- Angst J, Gamma A, Baldwin DS, Ajdacic-Gross V, Rossler W. The generalized anxiety spectrum: prevalence, onset, course and outcome. European Archives of Psychiatry and Clinical Neuroscience. 2009;259:37–45. doi: 10.1007/s00406-008-0832-9. [DOI] [PubMed] [Google Scholar]
- Angst J, Gamma A, Bienvenu OJ, Eaton WW, Ajdacic V, Eich D, Rössler W. Varying temporal criteria for generalized anxiety disorder: prevalence and clinical characteristics in a young age cohort. Psychological Medicine. 2006;36:1283–1292. doi: 10.1017/S0033291706007938. [DOI] [PubMed] [Google Scholar]
- Beesdo K, Knappe S, Pine DS. Anxiety and anxiety disorders in children and adolescents: developmental issues and implications for DSM-V. Psychiatric Clinics of North America. 2009;32:483–524. doi: 10.1016/j.psc.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beesdo K, Pine DS, Lieb R, Wittchen HU. Incidence and risk patterns of anxiety and depressive disorders and categorization of generalized anxiety disorder. Archives of General Psychiatry. 2010;67:47–57. doi: 10.1001/archgenpsychiatry.2009.177. [DOI] [PubMed] [Google Scholar]
- Beesdo-Baum K, Winkel S, Pine DS, Hoyer J, Hofler M, Lieb R, Wittchen HU. The diagnostic threshold of generalized anxiety disorder in the community: a developmental perspective. Journal of Psychiatric Research. 2011;45:962–972. doi: 10.1016/j.jpsychires.2010.12.007. [DOI] [PubMed] [Google Scholar]
- Bittner A, Egger HL, Erkanli A, Jane Costello E, Foley DL, Angold A. What do childhood anxiety disorders predict? Journal of Child Psychology and Psychiatry. 2007;48:1174–1183. doi: 10.1111/j.1469-7610.2007.01812.x. [DOI] [PubMed] [Google Scholar]
- Burstein M, Georgiades K, Lamers F, Swanson SA, Cui L, He JP, Avenevoli S, Merikangas KR. Empirically derived subtypes of lifetime anxiety disorders: developmental and clinical correlates in U.S. adolescents. Journal of Consulting and Clinical Psychology. 2012;80:102–115. doi: 10.1037/a0026069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter RM, Wittchen HU, Pfister H, Kessler RC. One-year prevalence of subthreshold and threshold DSM-IV generalized anxiety disorder in a nationally representative sample. Depression and Anxiety. 2001;13:78–88. doi: 10.1002/da.1020. [DOI] [PubMed] [Google Scholar]
- Comer JS, Gallo KP, Korathu-Larson P, Pincus DB, Brown TA. Specifying child anxiety disorders not otherwise specified in the DSM-IV. Depression and Anxiety. 2012a;29:1004–1013. doi: 10.1002/da.21981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Comer JS, Pincus DB, Hofmann SG. Generalized anxiety disorder and the proposed associated symptoms criterion change for DSM-5 in a treatment-seeking sample of anxious youth. Depression and Anxiety. 2012b;29:994–1003. doi: 10.1002/da.21999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello EJ, Angold A, Burns BJ, Stangl DK, Tweed DL, Erkanli A, Worthman CM. The Great Smoky Mountains Study of Youth. Goals, design, methods, and the prevalence of DSM-III-R disorders. Archives of General Psychiatry. 1996;53:1129–1136. doi: 10.1001/archpsyc.1996.01830120067012. [DOI] [PubMed] [Google Scholar]
- Essau CA, Conradt J, Petermann F. Frequency, co-morbidity, and psychosocial impairment of anxiety disorders in German adolescents. Journal of Anxiety Disorders. 2000;14:263–279. doi: 10.1016/s0887-6185(99)00039-0. [DOI] [PubMed] [Google Scholar]
- Fairburn CG, Bohn K. Eating disorder NOS (EDNOS): an example of the troublesome ‘not otherwise specified’ (NOS) category in DSM-IV. Behavior Research and Therapy. 2005;43:691–701. doi: 10.1016/j.brat.2004.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Stinson FS, Dawson DA, Ruan WJ, Goldstein RB, Smith SM, Saha TD, Huang B. Prevalence, correlates, co-morbidity, and comparative disability of DSM-IV generalized anxiety disorder in the USA: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Psychological Medicine. 2005;35:1747–1759. doi: 10.1017/S0033291705006069. [DOI] [PubMed] [Google Scholar]
- Hallion LS, Ruscio AM. Should uncontrollable worry be removed from the definition of GAD? A test of incremental validity. Journal of Abnormal Psychology. 2013;122:369–375. doi: 10.1037/a0031731. [DOI] [PubMed] [Google Scholar]
- Hoyer J, Becker ES, Margraf J. Generalized anxiety disorder and clinical worry episodes in young women. Psychological Medicine. 2002;32:1227–1237. doi: 10.1017/s0033291702006360. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Pimentel SS. On the physiological symptom constellation in youth with generalized anxiety disorder (GAD) Journal of Anxiety Disorders. 2003;17:211–221. doi: 10.1016/s0887-6185(02)00196-2. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Neale MC, Kessler RC, Heath AC, Eaves LJ. Generalized anxiety disorder in women. A population-based twin study. Archives of General Psychiatry. 1992;49:267–272. doi: 10.1001/archpsyc.1992.01820040019002. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Avenevoli S, Costello EJ, Georgiades K, Green JG, Gruber MJ, He JP, Koretz D, McLaughlin KA, Petukhova M, Sampson NA, Zaslavsky AM, Merikangas KR. Prevalence, persistence, and sociodemographic correlates of DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Archives of General Psychiatry. 2012a;69:372–380. doi: 10.1001/archgenpsychiatry.2011.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Avenevoli S, Costello EJ, Green JG, Gruber MJ, Heeringa S, Merikangas KR, Pennell BE, Sampson NA, Zaslavsky AM. Design and field procedures in the US National Comorbidity Survey Replication Adolescent Supplement (NCS-A) International Journal of Methods in Psychiatric Research. 2009;18:69–83. doi: 10.1002/mpr.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Avenevoli S, Costello J, Green JG, Gruber MJ, McLaughlin KA, Petukhova M, Sampson NA, Zaslavsky AM, Merikangas KR. Severity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication Adolescent Supplement. Archives of General Psychiatry. 2012b;69:381–389. doi: 10.1001/archgenpsychiatry.2011.1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005a;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Brandenburg N, Lane M, Roy-Byrne P, Stang PD, Stein DJ, Wittchen HU. Rethinking the duration requirement for generalized anxiety disorder: evidence from the National Comorbidity Survey Replication. Psycholological Medicine. 2005b;35:1073–1082. doi: 10.1017/s0033291705004538. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Ustun TB. The World Mental Health (WMH) Survey Initiative Version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) International Journal of Methods in Psychiatric Research. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Wittchen HU. Patterns and correlates of generalized anxiety disorder in community samples. Journal of Clinical Psychiatry. 2002;63 (Suppl 8):4–10. [PubMed] [Google Scholar]
- Knauper B, Cannell CF, Schwarz N, Bruce ML, Kessler RC. Improving the accuracy of major depression age of onset reports in the US National Comorbidity Survey. International Journal of Methods in Psychiatric Research. 1999;8:39–48. [Google Scholar]
- Lawrence AE, Brown TA. Differentiating generalized anxiety disorder from anxiety disorder not otherwise specified. Journal of Nervous and Mental Disease. 2009;197:879–886. doi: 10.1097/NMD.0b013e3181c29992. [DOI] [PubMed] [Google Scholar]
- Layne AE, Bernat DH, Victor AM, Bernstein GA. Generalized anxiety disorder in a nonclinical sample of children: symptom presentation and predictors of impairment. Journal of Anxiety Disorders. 2009;23:283–289. doi: 10.1016/j.janxdis.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, Tsang A, Ruscio AM, Haro JM, Stein DJ, Alonso J, Angermeyer MC, Bromet EJ, Demyttenaere K, de Girolamo G, de Graaf R, Gureje O, Iwata N, Karam EG, Lepine JP, Levinson D, Medina-Mora ME, Oakley Browne MA, Posada-Villa J, Kessler RC. Implications of modifying the duration requirement of generalized anxiety disorder in developed and developing countries. Psychological Medicine. 2009;39:1163–1176. doi: 10.1017/S0033291708004807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leon AC, Olfson M, Portera L, Farber L, Sheehan DV. Assessing psychiatric impairment in primary care with the Sheehan Disability Scale. International Journal of Psychiatry in Medicine. 1997;27:93–105. doi: 10.2190/T8EM-C8YH-373N-1UWD. [DOI] [PubMed] [Google Scholar]
- Lieb R, Becker E, Altamura C. The epidemiology of generalized anxiety disorder in Europe. European Neuropsychopharmacology. 2005;15:445–452. doi: 10.1016/j.euroneuro.2005.04.010. [DOI] [PubMed] [Google Scholar]
- Merikangas K, Avenevoli S, Costello J, Koretz D, Kessler RC. National comorbidity survey replication adolescent supplement (NCS-A): I. Background and measures. Journal of the American Academy of Child and Adolescent Psychiatry. 2009;48:367–369. doi: 10.1097/CHI.0b013e31819996f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui LH, Benjet C, Georgiades K, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swendsen J, Avenevoli S, Case B, Georgiades K, Heaton L, Swanson S, Olfson M. Service utilization for lifetime mental disorders in U.S. adolescents: results of the National Comorbidity Survey-Adolescent Supplement (NCS-A) Journal of the American Academy of Child amd Adolescent Psychiatry. 2011;50:32–45. doi: 10.1016/j.jaac.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pina AA, Silverman WK, Alfano CA, Saavedra LM. Diagnostic efficiency of symptoms in the diagnosis of DSM-IV: generalized anxiety disorder in youth. Journal of Child Psychology and Psychiatry. 2002;43:959–967. doi: 10.1111/1469-7610.00100. [DOI] [PubMed] [Google Scholar]
- Ruscio AM, Chiu WT, Roy-Byrne P, Stang PE, Stein DJ, Wittchen HU, Kessler RC. Broadening the definition of generalized anxiety disorder: effects on prevalence and associations with other disorders in the National Comorbidity Survey Replication. Journal of Anxiety Disorders. 2007;21:662–676. doi: 10.1016/j.janxdis.2006.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruscio AM, Lane M, Roy-Byrne P, Stang PE, Stein DJ, Wittchen HU, Kessler RC. Should excessive worry be required for a diagnosis of generalized anxiety disorder? Results from the US National Comorbidity Survey Replication. Psychological Medicine. 2005;35:1761–1772. doi: 10.1017/S0033291705005908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute. SAS/STAT® User’s Guide. SAS Institute; Cary, NC: 2008. [Google Scholar]
- Tracey SA, Chorpita BF, Douban J, Barlow DH. Empirical evaluation of DSM-IV generalized anxiety disorder criteria in children and adolescents. Journal of Clinical Child Psychology. 1997;26:404–414. doi: 10.1207/s15374424jccp2604_9. [DOI] [PubMed] [Google Scholar]
- Wittchen HU. Generalized anxiety disorder: prevalence, burden, and cost to society. Depression and Anxiety. 2002;16:162–171. doi: 10.1002/da.10065. [DOI] [PubMed] [Google Scholar]
- Wu P, Hoven CW, Cohen P, Liu X, Moore RE, Tiet Q, Okezie N, Wicks J, Bird HR. Factors associated with use of mental health services for depression by children and adolescents. Psychiatric Services. 2001;52:189–195. doi: 10.1176/appi.ps.52.2.189. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.