Abstract
A colon lipoma is a remarkably rare tumor. In most cases, the tumors are asymptomatic and small in size, need to be differentiated from malignant tumors, and do not need any special treatment. Selection of the right surgical strategy depends on the status of bowel, as well as the size and the location of tumor. We encountered two patients with giant submucosal lipomas that had induced intussusceptions: one with a lipoma in the transverse colon and the other with a lipoma in the ascending colon. The diagnoses were made by using histological examinations. We report the clinical features, diagnoses, and treatments of, as well as our experience with, these two uncommon cases, and we present a review of the literature on this subject.
Keywords: Colon, Intussusception, Laparoscopy, Lipoma
INTRODUCTION
A lipoma of the colon is a relatively rare, benign tumor. It has a reported incidence ranging between 0.2% and 4.4% and is the third most common benign tumor of the colon, following hyperplastic and adenomatous polyps [1]. The tumor is located in the right colon in 65% of the cases [2]. Most colonic lipomas are asymptomatic and need no treatment. However, about 30% reach 2 cm or larger in size and may produce symptoms such as anemia, abdominal pain, constipation, diarrhea, bleeding, or intussusception [3]. In this case report, we present one case of a giant transverse colonic lipoma causing a transverse colo-colonic intussusception and one case of a cecal lipoma causing an ileo-colic intussusception.
CASE REPORTS
Case 1
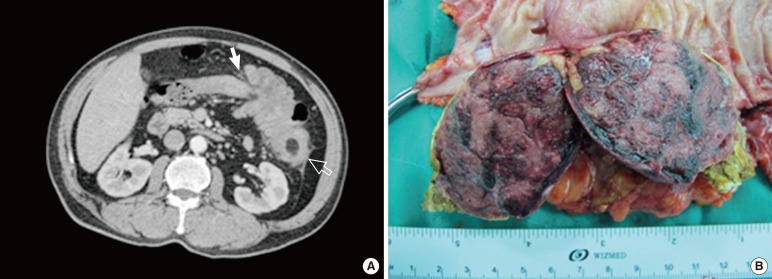
A 50-year-old male patient visited Gyeongsang National University Hospital because of a palpable mass on the left upper quadrant and intermittent abdominal pain which has started seven days earlier. His medical history was nonspecific, and he was hemodynamically stable. Detailed laboratory studies produced results within normal limits, including complete peripheral blood cell counts and blood biochemistry. However, the carcinoembryonic antigen level was not checked. The abdominal computed tomography (CT) scan was checked. A concentrically layered mass was shown at the middle transverse colon and extended to the distal transverse colon along the shortened transverse colon. About a 6-cm × 5-cm low-density mass on the distal transverse colon was observed on the CT scan (Fig. 1A). Colonoscopy was not performed because of complete colonic obstruction due to the intussusception. He was deemed to require surgery, which led to a transverse colonic segmental resection. In the excised colonic specimen, a polypoid mass of around 6.5 cm × 4 cm × 4.5 cm rising from the submucosal layer was observed, and the cross section of this mass was dark brown (Fig. 1B). The frozen biopsy confirmed that the tumor was benign. On microscopic examination, the mass consisted of matured fatty cells, and there was no evidence of malignancy; thus, the mass was diagnosed as a submucosal lipoma. After the surgery, the patient was discharged without any complications.
Fig. 1.
(A) Abdominal computed tomography findings show a transverse colonic intussusception (white arrow) and a 6-cm × 5-cm well-defined low-density mass (empty arrow) in the distal T-colon, suggesting a colo-colic intussusception caused by a lipoma. (B) Gross findings. The mass is confined to the submucosa, and the cut surface appears dark brown and septated.
Case 2
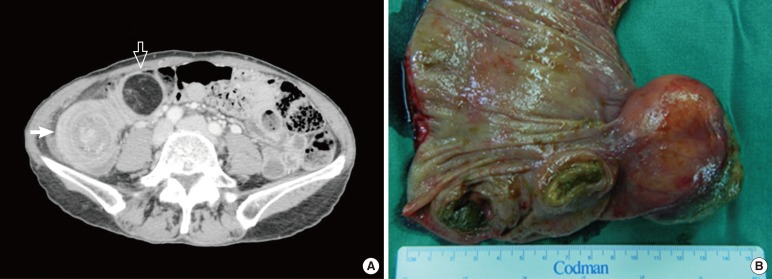
A 54-year-old woman visited an Emergency Department with severe abdominal pain in the right lower quadrant and vomiting. On her past medical history, an asymptomatic 2-cm-sized lipoma had been found incidentally during colonoscopy 4 months earlier. The current pain had started two days earlier when she had undergone a follow-up colonoscopy. Elective surgery was planned because the size of the lipoma had increased to 4 cm. She was hemodynamically stable. Preoperative laboratory findings were normal. About a 5.5-cm × 4-cm low-density mass on the proximal ascending colon was observed on the CT scan (Fig. 2A). A laparoscopy-assisted right hemicolectomy was performed. In the excised colonic specimen, a polypoid mass of around 6 cm × 4 cm × 3.5 cm rising from the submucosal layer was observed (Fig. 2B). The frozen biopsy confirmed that the tumor was benign, and the pathologic report was a submucosal lipoma. After surgery, the patient was discharged without any complications.
Fig. 2.
(A) Abdominal computed tomography findings show a concentric multilayered mass (white arrow) at the proximal A-colon and a 5.5-cm × 4-cm low-density mass (empty arrow), suggesting an ileo-colic intussusception caused by a lipoma. (B) Gross findings. A polypoid submucosal mass is identified in the proximal A-colon.
DISCUSSION
Most colonic lipomas, which often occur in elderly women, have small sizes and occur mainly in the cecum and the ascending colon [3]. The most common age is the fifth or the sixth decade of life. Most colonic lipomas are shown as single lesions, but multiple lipomas are noted in 10%-20% of cases. The most frequent type of colonic lipoma is a submucosal lipoma with a sessile or pedunculate appearance. The rest, less than 10%, are subserosal lipomas. In general, colonic lipomas do not cause symptoms and, therefore, are usually detected incidentally during colonoscopy, surgery and/or autopsy. When reported at autopsy, the incidence of colonic lipomas ranges from 0.035% to 4.4% [4].
Only 25% of patients with colonic lipomas develop symptoms. The common symptoms of colon lipomas include abnormal bowel habits, abdominal pain, diarrhea, rectal bleeding, abdominal discomfort and melena. Episodes of intussusception or intestinal obstruction can also be seen in patients with larger lipomas. Sometimes a colonic lipoma may also cause massive lower gastrointestinal bleeding [5]. The size of the lipoma is a predictor of the symptoms. As is widely accepted, lipomas larger than 20 mm in diameter are likely to be symptomatic [3]. Furthermore, for a lipoma with a maximum diameter of 85 mm to be asymptomatic is quite unusual [6].
Diagnosing a lipoma preoperatively is quite difficult because of the lack of specific symptoms and physical signs. Thus, asymptomatic lipomas are found incidentally during colonoscopy or a CT scan. A barium enema may demonstrate a filling defect, and the lesion may exhibit a lobulated appearance [4]. However, this phenomenon is nonspecific. In colonoscopy, three signs may contribute to the diagnosis: the "cushion sign" (probing the polyp with a closed biopsy forceps will often yield a pillow-like indentation), the "tenting effect" (grasping the overlying mucosa with biopsy forceps presents a tent-like appearance), and the "naked fat sign" (biopsies may result in an extrusion of yellowish fat) [7]. Biopsy by colonoscopy is not recommended in patients suspected of having a lipoma because the lesion is beneath the normal mucosa and because a biopsy often cannot promote a diagnosis. A biopsy cannot completely exclude the possibility of malignancy. The exact diagnosis still mainly relies on an intra- or postoperative pathology examination. In addition, biopsy may increases the risks of bleeding and perforation; furthermore, there was a case report that biopsy promoted colitis [6].
A patient with an asymptomatic colonic lipoma with a size smaller than 2 cm needs regular follow-up, but a resection is unnecessary. A symptomatic lipoma or asymptomatic lipoma larger than 2 cm in size should be considered for resection by endoscopic removal or surgical resection. With the advancement of colonoscopy, the endoscopic cautery snare resection of colonic lipomas has become popular and has been proven to be a safe therapeutic method, especially for small lesions. However, some studies have demonstrated that endoscopic removal increases the risks of bleeding and perforation [8]. The removal of colonic lipomas with the assistance of laparoscopy has also been reported [9]. In our first case, we tried to operate using a laparoscopic technique, but switched to an open procedure because of the bulky mass-like lesion and severe edema of the large bowel. However, in our second case, reduction was possible by using laparoscopic instruments because of less bowel edema. Laparoscopic surgery has advantages compared to open surgery for the patient's recovery [10]. Thus, we recommend that a laparoscopic procedure be tried first.
Several surgical methods, such as local excision through a small incision into a colon, segmental resection of the colon, and a hemicolectomy, can be used to treat a colonic lipoma. We can select an appropriate procedure based on the existence or nonexistence of an intussusception and on the size and the location of the lipoma. Although lipomas are benign tumors, the malignancy-free resection margin needs to be immediately checked in the operating room by using a frozen biopsy in order to confirm that the tumor is indeed benign. In our cases, frozen biopsies confirmed that both tumors were lipoma. However, if malignancy is not excluded by the frozen biopsy, the surgical procedure should be extended to a lymph-node dissection and a radical colon resection.
Footnotes
No potential conflict of interest relevant to this article is reported.
References
- 1.Vecchio R, Ferrara M, Mosca F, Ignoto A, Latteri F. Lipomas of the large bowel. Eur J Surg. 1996;162:915–919. [PubMed] [Google Scholar]
- 2.Rogers SO, Jr, Lee MC, Ashley SW. Giant colonic lipoma as lead point for intermittent colo-colonic intussusception. Surgery. 2002;131:687–688. doi: 10.1067/msy.2002.116409. [DOI] [PubMed] [Google Scholar]
- 3.Rogy MA, Mirza D, Berlakovich G, Winkelbauer F, Rauhs R. Submucous large-bowel lipomas--presentation and management. An 18-year study. Eur J Surg. 1991;157:51–55. [PubMed] [Google Scholar]
- 4.Ryan J, Martin JE, Pollock DJ. Fatty tumours of the large intestine: a clinicopathological review of 13 cases. Br J Surg. 1989;76:793–796. doi: 10.1002/bjs.1800760809. [DOI] [PubMed] [Google Scholar]
- 5.Rodriguez DI, Drehner DM, Beck DE, McCauley CE. Colonic lipoma as a source of massive hemorrhage: report of a case. Dis Colon Rectum. 1990;33:977–979. doi: 10.1007/BF02139110. [DOI] [PubMed] [Google Scholar]
- 6.Zhang H, Cong JC, Chen CS, Qiao L, Liu EQ. Submucous colon lipoma: a case report and review of the literature. World J Gastroenterol. 2005;11:3167–3169. doi: 10.3748/wjg.v11.i20.3167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Beer RA, Shinya H. Colonic lipomas: an endoscopic analysis. Gastrointest Endosc. 1975;22:90–91. doi: 10.1016/s0016-5107(75)73710-0. [DOI] [PubMed] [Google Scholar]
- 8.Raju GS, Gomez G. Endoloop ligation of a large colonic lipoma: a novel technique. Gastrointest Endosc. 2005;62:988–990. doi: 10.1016/j.gie.2005.08.018. [DOI] [PubMed] [Google Scholar]
- 9.Scoggin SD, Frazee RC. Laparoscopically assisted resection of a colonic lipoma. J Laparoendosc Surg. 1992;2:185–189. doi: 10.1089/lps.1992.2.185. [DOI] [PubMed] [Google Scholar]
- 10.Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6:477–484. doi: 10.1016/S1470-2045(05)70221-7. [DOI] [PubMed] [Google Scholar]