Abstract
Background
Total joint arthroplasty (TJA) is becoming more prevalent, with additional increases in procedure rates expected as the US population ages. Small series have suggested increased risk of periprosthetic joint infections in patients with liver cirrhosis after TJA. However, the rates of periprosthetic joint infections and use of TJA for patients with cirrhosis have not been evaluated on a larger scale.
Questions/purposes
The purposes of this study were to (1) measure the rate of periprosthetic joint infections after THAs and TKAs in patients with cirrhosis of the liver; (2) assess mortality, length of hospital stay, readmission rates, and other clinical factors among patients with cirrhosis who have had a TJA; and (3) evaluate the use of TJA in the United States among patients with liver cirrhosis during the past decade.
Methods
National and state-level databases were used to identify patients with and without liver cirrhosis who underwent TJAs. The rate of periprosthetic joint infections within 6 months was assessed using the Statewide Inpatient Database, which identified 306,946 patients undergoing THAs (0.3% with cirrhosis) and 573,840 patients undergoing TKAs (0.2% with cirrhosis). To evaluate trends in the use of TJAs, 16,634 patients with cirrhosis who underwent TJAs were identified from the Nationwide Inpatient Sample from 2000 to 2010.
Results
Periprosthetic joint infections after THA were more common in patients with cirrhosis for hip fracture (6.3% versus 1.1%; hazard ratio [HR], 5.8; p < 0.001) and nonhip fracture diagnoses (3.7% versus 0.7%; HR, 5.4; p < 0.001). Periprosthetic joint infections were more common after TKA in patients with cirrhosis (2.7% versus 0.8%; HR, 3.4; p < 0.001). Use of TJA increased faster for patients with cirrhosis than for patients without cirrhosis for THAs (140% versus 80%; p = 0.011) and TKAs (213% versus 128%; p < 0.001), and also increased faster than the general increase in use of TJAs.
Conclusions
Periprosthetic joint infections were more common among patients with cirrhosis who had TJAs. Additionally, patients with cirrhosis had longer length of hospital stay, increased costs, and higher rates of mortality, readmission, and reoperation. Finally, national use of TJAs for patients with cirrhosis has increased during the past decade.
Level of Evidence
Level III, therapeutic study. See the Instructions for Authors for a complete description of levels of evidence.
Introduction
THAs and TKAs are safe and effective procedures for the treatment of osteoarthritis [2, 15]. During the past decade in the United States, there has been a dramatic increase in the use of total joint arthroplasties (TJA) [16, 30]. Furthermore, according to projections between 2003 and 2030, the number of THAs is expected to increase by 174%, whereas TKAs are projected to increase by 673% [14]. As indications for TJA expand and medical care improves, patients undergoing TJAs are from a wider age range and have an increasing number of comorbid medical conditions [11, 14]. Because the presence of comorbid medical conditions increases the risk of adverse events and poor outcomes, as more TJAs are performed on an increasingly elderly and medically compromised population, there likely will be an increased number of postoperative complications [12, 23, 24].
The CDC recommended one-time screening for hepatitis C for all people born between 1945 and 1965 because of a disproportionately high prevalence of hepatitis C [27]. Complications of hepatitis C include liver cirrhosis, although this is more commonly caused by alcohol use [9]. Compensated cirrhosis may go undetected, but is estimated to occur in approximately 1% of the population [25]. This at-risk age group is also the primary group of patients who may elect to undergo total joint replacements during the next few decades. Patients with cirrhosis are at greater risk for surgical complications [31], partly owing to immune dysfunction [3, 22]. However, there has been little research on patients with cirrhosis undergoing orthopaedic procedures.
Current literature evaluating the results of TJA in patients with cirrhosis has been limited to small case series with groups of less than 100 patients [4, 10, 19, 20, 26]. In general these studies agreed that patients with cirrhosis had higher rates of periprosthetic joint infections, but given the small number of patients, there was limited evaluation of risk factors. Additionally, although there has been an 18% increase in hospitalizations for patients with cirrhosis during the past decade, there are no data regarding use of TJA in patients with cirrhosis [18, 28].
The purposes of our study therefore were to perform a large-scale systems-level query to (1) assess the rate of periprosthetic joint infections after THA and TKA in patients with liver cirrhosis; (2) evaluate mortality, length of hospitalization, hospital readmission rates, and other clinical factors; and (3) evaluate the use of TJA in the United States during the past decade in patients with liver cirrhosis.
Materials and Methods
Data Sources
The Nationwide Inpatient Sample (NIS) [7] and the State Inpatient Database (SID) [8] are administrative claims repositories produced annually by the Healthcare Cost and Utilization Project under the Agency for Healthcare Research and Quality. The NIS contains inpatient hospitalization information from a random sample of 20% of hospitals in the United States, weighted for generating national estimates. The SID contains inpatient records for specific participating states. Variables available in both data sets include patient demographics (ie, age, sex, and state of residence) and hospital visit information (ICD diagnosis and procedure codes, length of stay, and hospital charges). Some state databases contain identification variables that allow tracking and linking hospital admissions for the same patient with time.
The first part of our study used the SID to measure the rate of periprosthetic joint infections among patients with cirrhosis who had TJAs. We used states that allowed patient tracking, including California (2005–2011), Florida (2005–2010), Hawaii (2006–2009), North Carolina (2006–2010), Nebraska (2006–2010), New York (2006–2010), Utah (2006–2010), and Washington (2008–2009). We used the NIS from 2000 to 2010 to evaluate the national use of TJAs, length of stay, and mortality in patients with cirrhosis.
Patient Selection
From the SID and NIS datasets, we selected patients who underwent primary THAs (ICD-9 81.51) or primary TKAs (ICD-9 81.54). Patients were identified as having cirrhosis if they had a diagnosis of alcoholic cirrhosis (ICD-9 571.2), nonalcoholic cirrhosis (ICD-9 571.5), or biliary cirrhosis (ICD-9 571.6). For the longitudinal analysis, patients undergoing THAs were further grouped by whether the indication for arthroplasty was a hip fracture, as it has been suggested that these patients have worse outcomes [4].
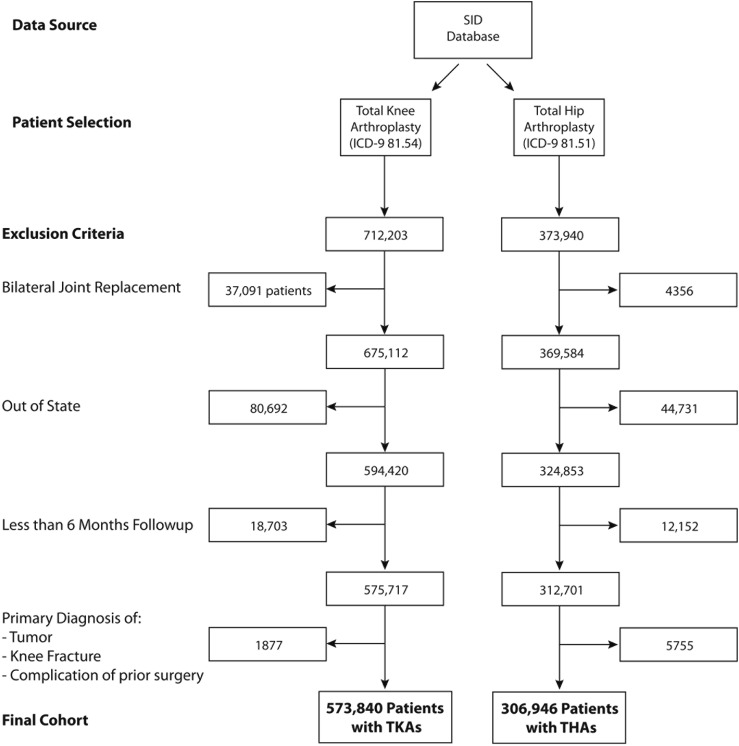
For the longitudinal analysis (first part of this study), patients were excluded if (1) they underwent bilateral joint arthroplasties; (2) their home state was different from the state where they underwent the arthroplasty; or (3) their procedure occurred during the last 6-month interval available in each data set (Fig. 1). Patients undergoing bilateral joint arthroplasties were excluded because of greater complication rates and these patients were deemed not directly comparable to patients with cirrhosis undergoing unilateral joint arthroplasties [17, 21]. Patients with different states of residence and hospitalization in the database were excluded because if complications were to occur, these patients may not return to the original state for treatment. Additionally, patients undergoing surgery during the last 6 months of each state’s available data set were excluded because there was insufficient followup time to evaluate for postoperative complications. Finally, patients with a primary diagnosis of knee fracture, tumor, or complication of a prior procedure (ICD-9 996.XX) were excluded.
Fig. 1.
Patients undergoing unilateral TKA or THA were selected from the statewide inpatient database. They were excluded if they underwent surgery out of their home state, if they did not have adequate followup (minimum, 6 months), or if they underwent joint replacement to treat tumor, infection, or a prior complication. SID = State Inpatient Database.
In total there were 306,946 patients who underwent THAs and 573,840 patients who underwent TKAs who were identified from the SID. There were 878 (0.29%) patients with cirrhosis who underwent THAs and 1231 (0.21%) patients with cirrhosis who underwent TKAs. In the NIS from 2000 to 2010, there were 2.6 million THAs and 5.2 million TKAs. Of these, there were 6890 (0.27%) patients with cirrhosis who had THAs and 9758 (0.19%) who had TKAs.
Patients with comorbid conditions that may alter the risk of infection were identified for risk stratification using the definitions of Elixhauser et al. [6]. We included other comorbid conditions that may alter the risk of infection, including hepatitis B and hepatitis C virus infection, HIV/AIDS, diabetes mellitus, rheumatoid arthritis, lupus, smoking, and obesity.
Outcome Measures
The primary outcome was periprosthetic joint infection (ICD-9 996.66 or 996.67) from the time of the procedure to 180 days after discharge. Secondary outcomes measured included all-cause mortality, blood transfusion use, length of stay, hospital charges, reoperation, and hospital readmission at 30 and 90 days after discharge. Additionally, hospital costs were estimated using the cost-to-charge ratio and adjusted for regional variations of average wages. All costs and charges were adjusted for inflation using the chained consumer price index [29] and are reported in 2010 US dollars.
Statistical Analysis
Rates of periprosthetic joint infection and hospital readmission were analyzed using a modified Kaplan-Meier time-to-failure analysis, and compared with a log-rank test. Data regarding deaths were not available as patients may die outside the hospital, and thus this information could not be incorporated in the Kaplan-Meier model. Analyses of procedure use were performed using Poisson regression. For infrequent events that occurred in groups of small size (ie, mortality in patients with cirrhosis undergoing TJA), a 3-year moving average was used to look for possible trends with time. Groups were compared using Student’s t-test for continuous variables and a chi-square test for categorical variables.
A multivariate Cox proportional hazards model was used to identify independent risk factors for periprosthetic joint infection. Other risk factors identified a priori as affecting the risk of periprosthetic joint infection also were incorporated in the model, including diabetes, peripheral vascular disease, obesity, tobacco use, and autoimmune diseases that may require immunosuppression (rheumatoid arthritis, ankylosing spondylitis, and lupus). Additionally, certain patient groups may have different levels of baseline risk, and thus risk was stratified by age, gender, arthroplasty type, hip fracture, and the number of medical comorbidities. Comparisons are reported as odds ratios (OR) or hazard ratios (HR). Results were deemed statistically significant when the p value was less than 0.05.
Results
Part I. Longitudinal Outcomes of Patients With Cirrhosis Undergoing Total Joint Arthroplasty
Patient Demographics
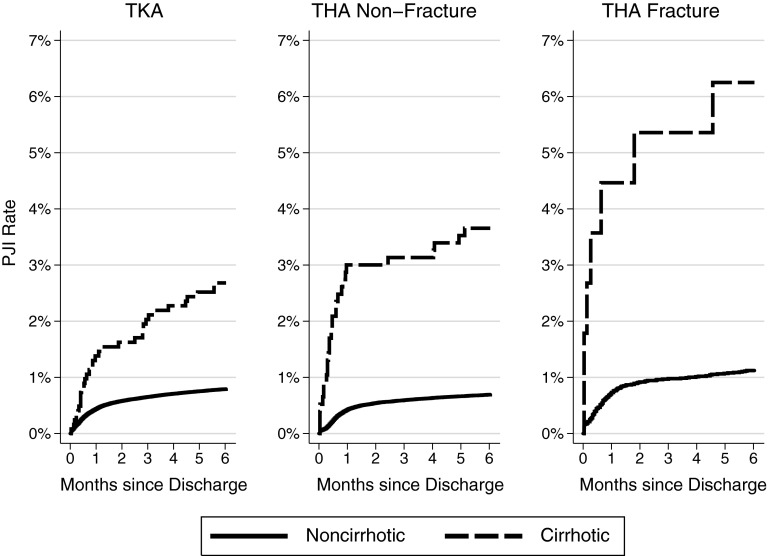
For all three groups, patients with liver cirrhosis had greater rates of periprosthetic joint infection within 180 days of the initial arthroplasty (Fig. 2). Among patients undergoing THAs, hip fracture was more common in patients with cirrhosis (12.8% versus 3.8%; OR, 3.7; p < 0.001). Among patients without hip fracture who underwent THA, the rate was increased from 0.7% to 3.7% (HR, 5.40; p < 0.001), whereas in patients with a hip fracture, it was increased from 1.1% to 6.3% (HR, 5.8; p < 0.001). Periprosthetic joint infections occurred in 0.8% of patients without cirrhosis undergoing TKAs but occurred in 2.7% of patients with cirrhosis (HR, 3.4; p < 0.001) (Table 1).
Fig. 2.
The rate of periprosthetic joint infections within 6 months of TJA was greater for patients with liver cirrhosis, with the difference most pronounced for patients undergoing THAs to treat hip fractures.
Table 1.
Infection and readmission rates at 6 months
| Outcome variable | THA (nonfracture) | THA (fracture) | TKA | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Noncirrhosis | Cirrhosis | HR | p value | Noncirrhosis | Cirrhosis | HR | p value | Noncirrhosis | Cirrhosis | HR | p value | |
| Periprosthetic infection rate | 0.69% (0.66–0.72) | 3.66% (2.54–5.25) | 5.40 | < 0.001 | 1.10% (0.95–1.33) | 6.30% (2.29–12.66) | 5.80 | < 0.001 | 0.79% (0.77–0.81) | 2.68% (1.91–3.75) | 3.41 | < 0.001 |
| Reoperation rate | ||||||||||||
| Irrigation and débridement | 1.14% | 2.87% | 2.67 | < 0.001 | 2.67% | 7.14% | 2.42 | 0.014 | 0.96% | 2.28% | 2.46 | < 0.001 |
| Resection arthroplasty | 0.18% | 1.17% | 5.87 | < 0.001 | 0.54% | 0.89% | 1.64 | 0.623 | 0.33% | 1.06% | 2.94 | < 0.001 |
| All-cause readmission | ||||||||||||
| 30 days | 4.6% | 11.0% | 2.03 | < 0.001 | 11.8% | 30.4% | 2.20 | < 0.001 | 4.6% | 10.3% | 1.83 | < 0.001 |
| 90 days | 8.9% | 18.7% | 20.7% | 42.9% | 8.8% | 17.3% | ||||||
| 180 days | 14.2% | 26.5% | 26.8% | 47.3% | 14.5% | 24.6% | ||||||
| Charge per readmission (USD)* | 41,607 ± 49,168 | 47,774 ± 63,490 | − | 0.155 | 43,323 ± 55,672 | 54,089 ± 52,657 | − | 0.204 | 35,560 ± 44,063 | 42,264 ± 67,246 | − | 0.040 |
| Cost per readmission (USD)* | 10,508 ± 10,747 | 12,433 ± 14,863 | − | 0.072 | 11,094 ± 13,599 | 15,078 ± 17,690 | − | 0.093 | 9234 ± 9982 | 10,391 ± 12,970 | − | 0.151 |
| 6-month total charges (USD)* | 58,838 ± 54,428 | 88,283 ± 116,240 | − | < 0.001 | 89,701 ± 94,394 | 155,816 ± 172,178 | − | < 0.001 | 54,785 ± 48,775 | 70,134 ± 80,892 | − | < 0.001 |
| 6-month total costs (USD)* | 12,045 ± 12,187 | 17,522 ± 22,202 | − | < 0.001 | 18,744 ± 20,710 | 32,131 ± 44,330 | − | < 0.001 | 11,232 ± 10,884 | 14,211 ± 15,706 | − | < 0.001 |
* Mean ± SD; HR = hazard ratio.
Compared with patients without cirrhosis, patients with cirrhosis had a higher likelihood of in-hospital mortality for THA (OR, 9.8; p < 0.001) and TKA (OR, 3.6; p < 0.001). Patients with cirrhosis also had longer hospital stays and were more likely to receive transfusions of blood, platelets, and coagulation factors than patients without cirrhosis. Total hospital charges and estimated costs were greater in patients with cirrhosis for THAs and TKAs (Table 2).
Table 2.
Demographic characteristics of patients undergoing total joint arthroplasty
| Patient characteristics | THA without cirrhosis | THA with cirrhosis | TKA without cirrhosis | TKA with cirrhosis |
|---|---|---|---|---|
| Patients (number) | 306,068 | 878 | 572,609 | 1,231 |
| Age ± SD (years) | 66.2 ± 12.6 | 62.3 ± 11.1* | 67.5 ± 10.4 | 64.3 ± 9.6* |
| Female (%) | 56.9% | 47.4%* | 63.3% | 54.8%* |
| Total comorbidities | 1.7 ± 1.4 | 3.8 ± 1.7* | 1.9 ± 1.4 | 3.8 ± 1.7* |
| Hip fracture (%) | 3.8% | 12.8%* | − | − |
| Insurance status | ||||
| Medicare | 55.3% | 51.3%* | 59.3% | 57.3% |
| Medicaid | 3.0% | 11.4%* | 2.7% | 7.1%* |
| Private | 38.3% | 33.9%* | 33.0% | 31.2% |
| Self-pay | 0.5% | 0.8% | 0.3% | 0.3% |
| Other | 5.9% | 6.6% | 9.9% | 8.8% |
| Length of stay (days) | 3.8 ± 2.5 | 6.0 ± 6.6* | 3.6 ± 1.9 | 4.2 ± 3.3* |
| Mortality (%) | 0.20% | 1.94%* | 0.11% | 0.41%* |
| Transfusion red blood cells | 30.29% | 47.27%* | 21.05% | 31.76%* |
| Transfusion platelets | 0.15% | 8.09%* | 0.07% | 7.47%* |
| Transfusion coagulation factors | 0.01% | 0.23%* | 0.01% | 0.16%* |
| Estimated costs (mean, 2010 US dollars) | $14,279 ± 6347 | $18,795 ± 13,447* | $13,309 ± 5306 | $14,841 ± 6792* |
| Total charges (mean, 2010 US dollars) | $55,243 ± 32,674 | $75,365 ± 67,453* | $51,121 ± 28,892 | $59,084 ± 37,388* |
* Statistical significance p < 0.05.
Reoperation also was more common in patients with cirrhosis. Rates of irrigation and débridement were greater in THAs for hip fractures (2.7% versus 7.1%; HR, 2.42; p = 0.014) and nonhip fractures (1.1% versus 2.9%; HR, 2.7; p < 0.001), and also after TKAs (1.0% versus 2.3%; HR, 2.5; p < 0.001). Resection arthroplasty was required more often for patients with cirrhosis who underwent TKAs (0.3% versus 1.1%; HR, 2.9; p < 0.001) and THAs without hip fractures (0.2% versus 1.2%; HR, 5.9; p < 0.001), whereas there was no difference in patients with hip fractures who underwent THAs (0.5% versus 0.9%; HR, 1.6; p = 0.623). When patients were readmitted for a periprosthetic joint infection, there was a higher mortality rate for patients with cirrhosis (0.7% versus 4.4%; p = 0.003).
All-cause Hospital Readmission
Patients with cirrhosis had greater all-cause hospital readmission rates at 1, 3, and 6 months. Readmission rates were higher in patients with cirrhosis and hip fractures who underwent THAs (11.8% versus 30.4%; HR, 2.2; p < 0.001) and without hip fractures (4.6% versus 11.0%; HR, 2.0; p < 0.001), and for TKAs (4.6% versus 10.3%; HR, 1.8; p < 0.001) (Table 1). The total estimated inpatient cost during 6 months was greater for all three groups for patients with cirrhosis (p < 0.001).
Multivariate Risk Model
Cirrhosis was associated with the greatest increased risk of periprosthetic joint infection (HR, 2.74; p < 0.001) (Table 3). Additionally, infection with hepatitis C increased the risk of periprosthetic joint infection, whereas HIV/AIDS showed a trend for increased risk. Hepatitis B infection, however, was not independently associated with periprosthetic joint infections. There also were multiple medical comorbidities associated with increased risk of periprosthetic joint infections.
Table 3.
Independent risk factors identified through multivariate regression*
| Risk factor | HR | 95% CI | p value |
|---|---|---|---|
| Liver cirrhosis | 2.42 | (1.87–3.12) | < 0.001 |
| Hepatitis B (no cirrhosis) | 1.22 | (0.77–1.95) | 0.401 |
| Hepatitis C (no cirrhosis) | 2.33 | (1.97–2.76) | < 0.001 |
| Diabetes | 1.32 | (1.25–1.40) | < 0.001 |
| Peripheral vascular disease | 1.34 | (1.16–1.55) | < 0.001 |
| HIV/AIDS | 1.74 | (0.96–3.17) | 0.068 |
| Smoking | 1.03 | (0.96–1.09) | 0.424 |
| Alcohol abuse | 1.64 | (1.38–1.95) | < 0.001 |
| Obesity | 1.25 | (1.17–1.33) | < 0.001 |
| Autoimmune disease (rheumatoid arthritis, lupus, ankylosing spondylitis) | 1.55 | (1.40–1.72) | < 0.001 |
* Adjusted for age, sex, procedure type (THA or TKA), hip fracture, and number of medical comorbidities; HR = hazard ratio.
Part II. National Use of TJA in Patients with Liver Cirrhosis
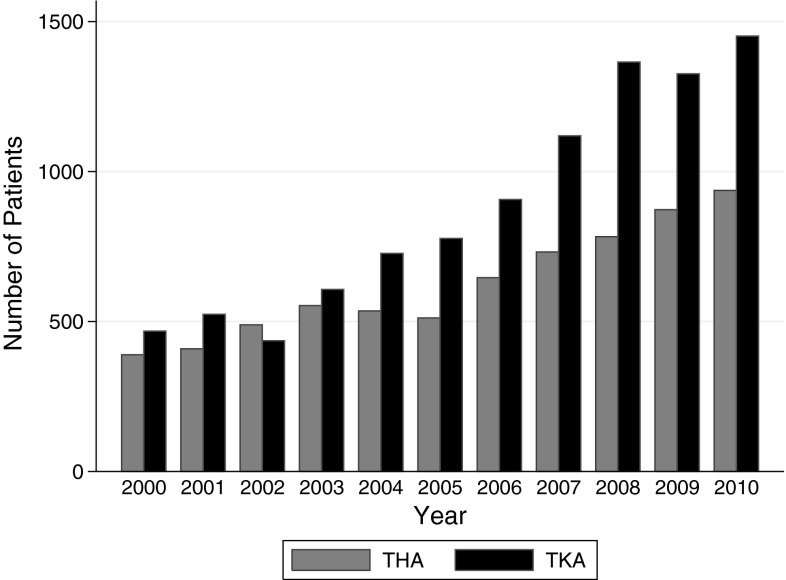
From 2000 to 2010, the number of hospital admissions in the United States for patients with cirrhosis increased by 67.1% (from 312,523 to 522,126). Hospitalizations for THA increased by 80.0% (from 168,184 to 302,838), whereas hospitalizations for TKA increased 127.9% (from 288,848 to 658,340).
During this same period, the number of patients with cirrhosis undergoing THAs increased 140.1% (from 388 to 955). The number of patients with cirrhosis undergoing TKAs increased by 213.1% (from 468 to 1465) (Fig. 3). These increases in the use of TJA were greater for patients with cirrhosis than patients without cirrhosis for THAs (p = 0.011) and TKAs (p < 0.001).
Fig. 3.
Patients with liver cirrhosis have had increased rates of TJAs during the past decade.
Overall, the length of hospital stay was greater for patients with cirrhosis (3.7 versus 4.4 days for TKA, p < 0.001; 4.0 versus 5.7 days for THA, p < 0.001). The average length of stay for all patients decreased from 2000 to 2010 for THAs (4.6 days to 3.4 days, p < 0.001) and TKAs (from 4.3 days to 3.3 days, p < 0.001). For patients with cirrhosis undergoing TKAs, the length of stay decreased from 2000 to 2010 (from 5.3 days to 3.7 days, p < 0.001), but it still was elevated compared with length of stay for patients without cirrhosis (p < 0.001).
All-cause in-hospital mortality was greater in patients with cirrhosis (0.23% versus 1.76% for THA, p < 0.001; 0.11% versus 0.34% for TKA, p = 0.002), but improved for all patients during the past decade. A 3-year moving average of mortality showed that from 2001 to 2009, mortality among patients having THAs decreased by 52.9% (from 0.34% to 0.16%, p < 0.001) and by 57.9% for TKAs (from 0.15% to 0.08%, p < 0.001). A reduction in mortality also was seen for patients with cirrhosis, decreasing by 46.7% for THAs (from 3.21% to 1.35%, p = 0.006), and 25.0% for TKAs (from 0.32% to 0.24%, p = 0.056).
Discussion
With the aging population in the United States, demand and need for TJAs will continue to increase. The prevalence of liver cirrhosis also is increasing, and the CDC now advocates one-time routine screening for hepatitis C for the baby-boomer population [27]. Current use of TJAs in patients with cirrhosis is unknown, but is important from a public health perspective to identify complication rates in patients with a severe medical comorbidity. In this study, we showed that patients with cirrhosis are at significantly greater risk of periprosthetic joint infections after TJAs, and also have longer lengths of hospitalization, increased cost of hospitalization, and higher rates of readmission, reoperation, and mortality. Our data also showed a large increase in the number of patients with cirrhosis during the past decade.
There are several limitations to our study. Because our data were derived from administrative claims data, we did not have access to laboratory results and other clinical information that would have allowed us to assess and classify the severity of cirrhosis or whether the patient was compensated or decompensated, which would help stratify patients in the cirrhosis group. Additionally, we could assess only end points that resulted in hospital admission. Although it is likely that nearly all patients with periprosthetic joint infections who present during the first 6 months would be treated on an inpatient basis [10], we are unable to identify patients who were treated conservatively as outpatients. Additionally, we could not assess certain outcomes such as overall mortality after hospital discharge as these data were not available. There is also the possibility of patient loss to followup if they moved out of the state.
In our review of the literature we identified five studies that evaluated periprosthetic joint infections after TJAs in patients with cirrhosis that combined for a total of 149 patients [4, 10, 19, 20, 26]. The reported rates of periprosthetic joint infections vary from 6% (n = 3/51)[26], 8% (n = 2/25)[20], and 10% (n = 3/30)[19], and as much as 29% (n = 2/7)[4]. The results of our study, which identified more than 2000 patients with cirrhosis, confirm that patients with cirrhosis have increased risk of periprosthetic joint infections, with 6-month rates of 2.7% for patients undergoing TKAs, 3.7% for patients with nonhip fractures undergoing THAs, and 6.3% for patients with hip fractures undergoing THAs. Although these rates may be slightly lower, this likely is attributable to differences in followup time and small sample sizes in prior studies.
Our results also showed that patients with cirrhosis had worse clinical outcomes including longer length of stay, increased transfusion requirements, higher hospital costs, and increased rates of reoperation, readmission, and mortality. This is also in agreement with prior reports. Moon et al. [19] found that patients with cirrhosis undergoing THAs had a high incidence (26.7%) of complications at 30 days with a greater risk of complications for patients with more severe grades of cirrhosis. Additionally, patients with cirrhosis had lower hip prosthesis survival rates at 5 years (77.8% versus 96.4%) [10]. Shih et al. [26] reported higher rates of complications and mortality for patients with cirrhosis undergoing TKAs than for patients without cirrhosis. Infection was the most common complication, occurring in more than 20% of patients at 42 months of followup. Bozic and Ries [1] reported that periprosthetic joint infections have been shown to cause increased use of hospital resources compared with primary arthroplasty or revision for aseptic loosening. This is confirmed with our results, as patients had higher hospital costs, higher total cost during 6 months, and increased transfusion requirements. In addition to the affect that complications have on patient quality of life, this is important in the current era of monitoring healthcare spending, and patients with cirrhosis carry significantly greater risk.
The increasing use of TJAs has been well-documented [5, 13, 14, 16]. Our study confirms this increased use, along with promising decreases in mortality and length of stay. However, the proportion of TJAs being performed on patients with cirrhosis is increasing. Although we speculate that these patients are evaluated thoroughly by a primary care provider, an orthopaedic surgeon, and an anesthesiologist before undergoing surgery, the evidence suggests that these patients who are considered stable enough for elective surgery are at a substantially elevated risk of serious postoperative complications. In our multivariate model, most patients with cirrhosis would present with a minimum of two risk factors (cirrhosis in addition to either hepatitis C or alcohol abuse) and therefore would have an almost five times higher risk of a periprosthetic joint infection compared with healthy patients.
Our study showed there is an increased risk of periprosthetic joint infection after TJA in patients with cirrhosis. Patients with cirrhosis had increased hospital stays, mortality, readmission, reoperation, and costs than did patients without cirrhosis. Thus, in light of the increasing prevalence of elective TJAs being performed in this at-risk patient population, it is important for surgeons and for patients with cirrhosis to consider the increased likelihood of postoperative complications, and for patients to improve their overall health to whatever degree is possible before surgery.
Acknowledgments
We thank Vanessa Chan MPH for help in preparing the manuscript.
Footnotes
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
References
- 1.Bozic KJ, Ries MD. The impact of infection after total hip arthroplasty on hospital and surgeon resource utilization. J Bone Joint Surg Am. 2005;87:1746–1751. doi: 10.2106/JBJS.D.02937. [DOI] [PubMed] [Google Scholar]
- 2.Chang RW, Pellisier JM, Hazen GB. A cost-effectiveness analysis of total hip arthroplasty for osteoarthritis of the hip. JAMA. 1996;275:858–865. doi: 10.1001/jama.1996.03530350040032. [DOI] [PubMed] [Google Scholar]
- 3.Christou L, Pappas G, Falagas ME. Bacterial infection-related morbidity and mortality in cirrhosis. Am J Gastroenterol. 2007;102:1510–1517. doi: 10.1111/j.1572-0241.2007.01286.x. [DOI] [PubMed] [Google Scholar]
- 4.Cohen SM, Te HS, Levitsky J. Operative risk of total hip and knee arthroplasty in cirrhotic patients. J Arthroplasty. 2005;20:460–466. doi: 10.1016/j.arth.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 5.Cram P, Lu X, Kaboli PJ, Vaughan-Sarrazin MS, Cai X, Wolf BR, Li Y. Clinical characteristics and outcomes of Medicare patients undergoing total hip arthroplasty, 1991–2008. JAMA. 2011;305:1560–1567. doi: 10.1001/jama.2011.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 7.HCUP NIS Database Documentation. Healthcare Cost and Utilization Project (HCUP). December 2013. Agency for Healthcare Research and Quality, Rockville, MD. Available at: www.hcup-us.ahrq.gov/db/nation/nis/nisdbdocumentation.jsp. Accessed March 19, 2014.
- 8.HCUP Databases. Healthcare Cost and Utilization Project (HCUP). December 2013. Agency for Healthcare Research and Quality, Rockville, MD. Available at: www.hcup-us.ahrq.gov/sidoverview.jsp. Accessed March 19, 2014.
- 9.Heidelbaugh JJ, Bruderly M. Cirrhosis and chronic liver failure: part I. Diagnosis and evaluation. Am Fam Physician. 2006;74:756–762. [PubMed] [Google Scholar]
- 10.Hsieh PH, Ueng SW, Lee MS, Shih HN, Huang KC. Prosthetic hip infection in patients with liver cirrhosis: an outcome analysis. Int J Infect Dis. 2010;14:e1054–e1059. doi: 10.1016/j.ijid.2010.06.018. [DOI] [PubMed] [Google Scholar]
- 11.Jimenez-Garcia R, Villanueva-Martinez M, Fernandez-de-Las-Penas C, Hernandez-Barrera V, Rios-Luna A, Garrido PC, de Andres AL, Jimenez-Trujillo I, Montero JS, Gil-de-Miguel A. Trends in primary total hip arthroplasty in Spain from 2001 to 2008: evaluating changes in demographics, comorbidity, incidence rates, length of stay, costs and mortality. BMC Musculoskelet Disord. 2011;12:43. doi: 10.1186/1471-2474-12-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koenig K, Huddleston JI, 3rd, Huddleston H, Maloney WJ, Goodman SB. Advanced age and comorbidity increase the risk for adverse events after revision total hip arthroplasty. J Arthroplasty. 2012;27(1402–1407):e1. doi: 10.1016/j.arth.2011.11.013. [DOI] [PubMed] [Google Scholar]
- 13.Kurtz S, Mowat F, Ong K, Chan N, Lau E, Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg Am. 2005;87:1487–1497. doi: 10.2106/JBJS.D.02441. [DOI] [PubMed] [Google Scholar]
- 14.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 15.Lavernia CJ, Guzman JF, Gachupin-Garcia A. Cost effectiveness and quality of life in knee arthroplasty. Clin Orthop Relat Res. 1997;345:134–139. [PubMed] [Google Scholar]
- 16.Losina E, Thornhill TS, Rome BN, Wright J, Katz JN. The dramatic increase in total knee replacement utilization rates in the United States cannot be fully explained by growth in population size and the obesity epidemic. J Bone Joint Surg Am. 2012;94:201–207. doi: 10.2106/JBJS.J.01958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meehan JP, Danielsen B, Tancredi DJ, Kim S, Jamali AA, White RH. A population-based comparison of the incidence of adverse outcomes after simultaneous-bilateral and staged-bilateral total knee arthroplasty. J Bone Joint Surg Am. 2011;93:2203–2213. doi: 10.2106/JBJS.J.01350. [DOI] [PubMed] [Google Scholar]
- 18.Millwala F, Nguyen GC, Thuluvath PJ. Outcomes of patients with cirrhosis undergoing non-hepatic surgery: risk assessment and management. World J Gastroenterol. 2007;13:4056–4063. doi: 10.3748/wjg.v13.i30.4056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moon YW, Kim YS, Kwon SY, Kim SY, Lim SJ, Park YS. Perioperative risk of hip arthroplasty in patients with cirrhotic liver disease. J Korean Med Sci. 2007;22:223–226. doi: 10.3346/jkms.2007.22.2.223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Orozco F, Post ZD, Baxi O, Miller A, Ong A. Fibrosis in Hhpatitis C patients predicts complications after elective total joint arthroplasty. J Arthroplasty. 2014;29:7–10. doi: 10.1016/j.arth.2013.03.023. [DOI] [PubMed] [Google Scholar]
- 21.Peak EL, Hozack WJ, Sharkey PF, Parvizi J, Rothman RH. One-stage bilateral total joint arthroplasty: a prospective, comparative study of total hip and total knee replacement. Orthopedics. 2008;31:131. doi: 10.3928/01477447-20080201-26. [DOI] [PubMed] [Google Scholar]
- 22.Rimola A, Soto R, Bory F, Arroyo V, Piera C, Rodes J. Reticuloendothelial system phagocytic activity in cirrhosis and its relation to bacterial infections and prognosis. Hepatology. 1984;4:53–58. doi: 10.1002/hep.1840040109. [DOI] [PubMed] [Google Scholar]
- 23.Schairer WW, Sing DC, Vail TP, Bozic KJ. Causes and frequency of unplanned hospital readmission after total hip arthroplasty. Clin Orthop Relat Res. 2014;472:464–470. doi: 10.1007/s11999-013-3121-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schairer WW, Vail TP, Bozic KJ. What are the rates and causes of hospital readmission after total knee arthroplasty? Clin Orthop Relat Res. 2014;472:181–187. doi: 10.1007/s11999-013-3030-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schuppan D, Afdhal NH. Liver cirrhosis. Lancet. 2008;371:838–851. doi: 10.1016/S0140-6736(08)60383-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shih LY, Cheng CY, Chang CH, Hsu KY, Hsu RW, Shih HN. Total knee arthroplasty in patients with liver cirrhosis. J Bone Joint Surg Am. 2004;86:335–341. doi: 10.2106/00004623-200402000-00017. [DOI] [PubMed] [Google Scholar]
- 27.Smith BD, Morgan RL, Beckett GA, Falck-Ytter Y, Holtzman D, Teo CG, Jewett A, Baack B, Rein DB, Patel N, Alter M, Yartel A, Ward JW; Centers for Disease Control and Prevention. Recommendations for the identification of chronic hepatitis C virus infection among persons born during 1945–1965. MMWR Recomm Rep. 2012;61(RR-4):1–32. [PubMed]
- 28.Talwalkar JA. Time trends in hospitalization and discharge status for cirrhosis and portal hypertension in the United States. Hepatology. 2010;52:1862; author reply 1863. [DOI] [PubMed]
- 29.US Department of Labor, Bureau of Labor Statistics. Consumer Price Index. Available at: http://www.bls.gov/cpi/superlink.htm. Accessed March 19, 2014,
- 30.Wolf BR, Lu X, Li Y, Callaghan JJ, Cram P. Adverse outcomes in hip arthroplasty: long-term trends. J Bone Joint Surg Am. 2012;94:e103. doi: 10.2106/JBJS.K.00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ziser A, Plevak DJ. Morbidity and mortality in cirrhotic patients undergoing anesthesia and surgery. Curr Opin Anaesthesiol. 2001;14:707–711. doi: 10.1097/00001503-200112000-00018. [DOI] [PubMed] [Google Scholar]