Abstract
Background
Although some clinical reports suggest patient-specific instrumentation in TKA may improve alignment, reduce surgical time, and lower hospital costs, it is unknown whether it improves pain- and function-related outcomes and gait.
Questions/purposes
We hypothesized that TKA performed with patient-specific instrumentation would improve patient-reported outcomes measured by validated scoring tools and level gait as ascertained with three-dimensional (3-D) analysis compared with conventional instrumentation 3 months after surgery.
Methods
We randomized 40 patients into two groups using either patient-specific instrumentation or conventional instrumentation. Patients were evaluated preoperatively and 3 months after surgery. Assessment tools included subjective functional outcome and quality-of-life (QOL) scores using validated questionnaires (New Knee Society Score© [KSS], Knee Injury and Osteoarthritis Outcome Score [KOOS], and SF-12). In addition, gait analysis was evaluated with a 3-D system during level walking. The study was powered a priori at 90% to detect a difference in walking speed of 0.1 m/second, which was considered a clinically important difference, and in a post hoc analysis at 80% to detect a difference of 10 points in KSS.
Results
There were improvements from preoperatively to 3 months postoperatively in functional scores, QOL, and knee kinematic and kinetic gait parameters during level walking. However, there was no difference between the patient-specific instrumentation and conventional instrumentation groups in KSS, KOOS, SF-12, or 3-D gait parameters.
Conclusions
Our observations suggest that patient-specific instrumentation does not confer a substantial advantage in early functional or gait outcomes after TKA. It is possible that differences may emerge, and this study does not allow one to predict any additional variances in the intermediate followup period from 6 months to 1 year postoperatively. However, the goals of the study were to investigate the recovery period as early pain and functional outcomes are becoming increasingly important to patients and surgeons.
Level of Evidence
Level I, therapeutic study. See the Instructions to Authors for a complete description of levels of evidence.
Introduction
Knee function and survivorship after TKA are dependent on many factors, including patient selection, three-dimensional (3-D) alignment of the components, ligament balancing, effective rehabilitation, and management of patient expectations [14, 21, 22, 32, 33, 35, 42, 61]. Coronal, sagittal, and rotational plane outliers have been shown to be associated with inferior function after TKA [3, 6, 11, 13, 15, 33, 37, 38, 46, 52, 53, 55, 61, 63, 65]. As such, attempts have been made to improve frontal and sagittal alignment in TKA using multiple 3-D preoperative and intraoperative tools. New innovations such as patient-specific instrumentation have been introduced. The basic premise of these systems is to limit coronal, sagittal, and rotational plane outliers while reducing surgical time.
Patient-specific instrumentation uses preoperative imaging (plain radiographs, CT, and/or MRI) to manufacture cutting blocks through rapid prototyping specific to a patient’s anatomy. The patient-specific instrumentation guides are applied directly to position the tibial and femoral cutting guides without any violation of the intramedullary canal. As such, the purported benefits include a decrease in operative time, decrease in blood loss, improved functional recovery, decrease in instrument trays, and the ability to preoperatively plan a patient’s component size, position, and alignment [10, 41]. Disadvantages include increased cost and time for imaging and instrument fabrication and a learning curve for the surgeon.
Although multiple studies have investigated alignment, operative time, and cost with patient-specific instrumentation [29, 34, 44, 45, 48, 61], to our knowledge, there is only one available study regarding whether the technology improves patient-reported outcomes or gait [49]. Moreover, no randomized clinical trial has investigated patients’ objective functional outcome parameters with comprehensive gait analysis during the early rehabilitation period after TKA with patient-specific instrumentation. Although long-term survivorship is of interest, early pain relief and improved functional outcomes have become increasingly important to patients and surgeons, particularly with the popularization of minimally invasive surgical (MIS) techniques [17–19, 40, 48]. In addition, literature regarding MIS has shown that tools used to analyze pain and functional outcomes during the early recovery period are sensitive [16, 20, 25, 27, 47] . Because some authors have reported a decrease in operative time and blood loss with patient-specific instrumentation [10, 41], we hypothesized that the use of patient-specific instrumentation in TKA potentially could improve early pain and functional outcomes, and this could be appropriately measured.
As such, the goals of the current study were to compare (1) patient-reported outcomes scores (New Knee Society Score© [KSS], Knee Injury and Osteoarthritis Outcome Score [KOOS], and SF-12), and (2) gait parameters at 3 months after surgery between patients operated on with patient-specific instrumentation versus conventional instrumentation.
Patients and Methods
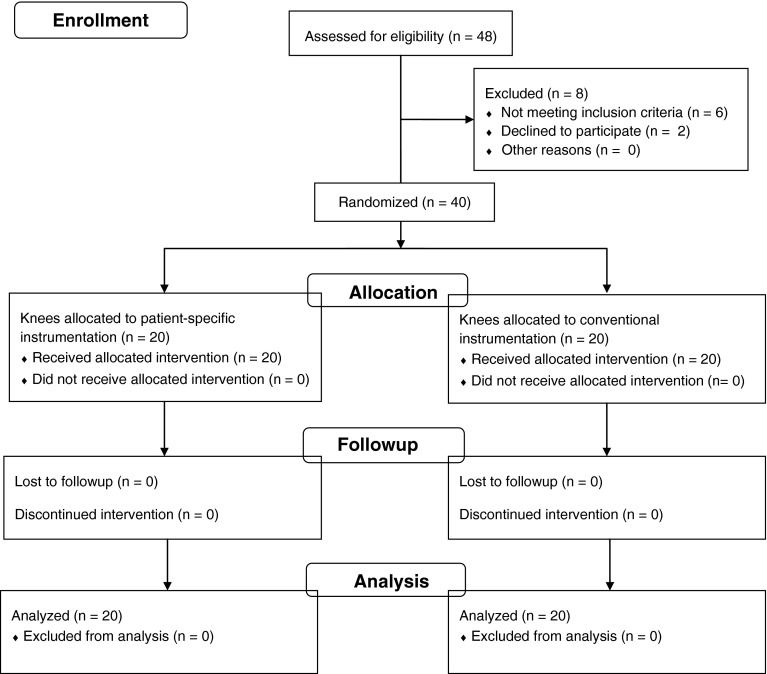
In this randomized controlled trial, 40 patients (20 in each group) undergoing unilateral primary TKA at our institution between September 2012 and January 2013 by the two senior authors (JNAA, SP) were recruited (Fig. 1). Patients were included if they (1) had severe, symptomatic knee arthritis [2]; (2) were between 50 and 85 years old; (3) were willing to wait 6 to 8 weeks before surgery; and (4) were accepting of new technology. Exclusion criteria included metallic hardware within 10 cm of the knee, any other previous knee surgery that could lead to an artifact effect on imaging, or prior THA. All patients who met the criteria were invited to participate; the 40 who agreed to participate represented 84% (40 of 48) of the patients we approached. The study was approved by our institution’s ethics committee before initiation. All patients provided informed consent.
Fig. 1.
A flow diagram [39] shows the patients’ enrollment, allocation, followup, and analysis. (Diagram adapted from Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux PJ, Elbourne D, Egger M, Altman DG; Consolidated Standards of Reporting Trials Group. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol. 2010;63:e1–37.)
We previously reported the main elements of the study design and radiographic results of these patients [47]. We found the radiographic alignment to be no different between the two study groups (Table 1) [47]. Briefly, patients were randomized to either the patient-specific instrumentation or conventional instrumentation group by the hospital’s informatics department using a systematic sampling method. The randomization protocol was not revealed to the authors, who received the information in the office regarding the group to which the patient was assigned in sealed, numbered envelopes approximately 6 to 8 weeks before the scheduled surgery. The randomization process matched patients for age within 5 years, sex, BMI ± 3 kg/m2, preoperative diagnosis, and operative side treated (Table 1).
Table 1.
Preoperative demographic and radiographic data
| Variable | Patient-specific instrumentation | Conventional instrumentation | p value |
|---|---|---|---|
| (n = 20) | (n = 20) | ||
| Age (years)* | 71 (61–81) | 71 (55–83) | 0.645 |
| Sex ratio (female:male) | 12:8 | 12:8 | – |
| Body mass index (kg/m2)* | 28.3 (20.3–36) | 30 (24–41) | 0.123 |
| Side (left/right) | 12/8 | 12/8 | – |
| ROM (degrees)* | 110 (95–125) | 113 (80–125) | 0.719 |
| Flexion contracture (degrees)* | 6 (0–10) | 6 (0–20) | 0.918 |
| Charnley classification | |||
| A | 17 | 16 | – |
| B1 | 3 | 3 | – |
| B2 | 0 | 0 | – |
| C | 0 | 1 | – |
| Preoperative alignment | |||
| Varus | 14 | 16 | – |
| Valgus | 4 | 2 | – |
| Neutral | 2 | 2 | – |
| Postoperative alignment | |||
| Hip-knee angle (degrees)* | 179 (171–185) | 178.3 (171–180) | 0.942 |
| Frontal femoral component angle (degrees)* | 90.1 (84–98) | 89.8 (87–97) | 0.409 |
| Frontal tibial component angle (degrees)* | 89.1 (85–96) | 88.6 (85–91) | 0.472 |
| Tibial slope (degrees)* | 5.9 (3–9) | 5.85 (4–8) | 0.607 |
* Values are represented as mean (range); the remaining values are expressed as number of patients.
For the patients allocated to the patient-specific instrumentation group, MRI was obtained after randomization but 6 to 8 weeks before surgery. All patients had their MRI completed on the same machine (Philips® Intera 1.5 Tesla; Koninklijke Philips NV, Best, The Netherlands) in the hospital’s department of radiology using a standardized protocol validated by the protocol manufacturer (Materialise®, Leuven, Belgium). For every patient, the protocol included images were acquired from the hip, knee (between 80 and 120 sections), and ankle. All identifying information was removed from the images and they were uploaded to a dedicated online management system. After segmentation, the engineers planned the TKA and submitted it to the surgeon. Based on the clinical examination and standing full-length hip-to-ankle radiographs, the plan was scrutinized and modified by the surgeon to set the appropriate depth of the distal femoral and tibial cuts, flexion of the femoral implant, and slope of the tibial plateau. The rotation of the femoral implant was based on the transepicondylar axis and never changed in this study. The tibial rotation was modified to be referenced from the anterior tibial tuberosity, fitting the anterior cortex [1, 4, 26, 30]. Before approval, the flexion and extension spaces were equalized. After this in-depth review by the surgeon, rapid prototyping and computer-assisted design and manufacturing technology were used to create the patient-specific instrumentation jigs.
The surgical exposure through a standard medial parapatellar arthrotomy was identical for both groups. For patients randomized to the patient-specific instrumentation group, after exposure of the knee, the patient-specific instrumentation jigs were carefully positioned over previously cleaned and dried articular surfaces, ensuring an accurate fit. Subsequently, guided by the patient-specific instrumentation jig, drill holes and pins were placed in the cartilage surfaces, which then determined the orientation of standard cutting guides. For patients randomized to the conventional instrumentation group, a traditional extramedullary guide was used for the tibia and an intramedullary rod for the femur. The remaining procedure in both groups was completed as per our standard protocol [9]. The patella was resurfaced systematically in both groups. All patients received the identical cemented high-flex mobile-bearing posterior-stabilized prosthesis (Negev® LPS-Flex mobile; Zimmer; Warsaw, IN, USA) [7, 8]. In both groups, no tourniquet was used and patients received the identical postoperative pain and blood management protocols [19, 26]. In addition, the same postoperative rehabilitative protocol was used for all patients.
There were no instances in which a patient’s procedure was converted from patient-specific instrumentation to conventional instrumentation. However, there were intraoperative modifications of the plan for patients in the patient-specific instrumentation group. Three patients required an additional distal femoral resection of 2 mm and two patients required additional tibial resection of 2 mm (25% of cases required modification). This was based on intraoperative judgment by the operative surgeon.
Subjective and objective functional results were analyzed preoperatively and 3 months postoperatively using the (1) KSS, (2) KOOS, and (3) SF-12 [27, 43, 54, 62, 64]. Gait parameters were analyzed in our institutional gait laboratory. The laboratory is fitted with the 3-D Vicon® system (Viton, Denver, CO, USA), six cameras, and two AMTI® force platforms (Advanced Mechanical Technology Inc, Watertown, MA, USA) to calculate spatiotemporal parameters (speed, pace, stride length), kinematics (knee angles), and kinetics (joint power). The acquisition was performed according to the “plug-in-gait” protocol. Thirteen passive markers were used: four segmental markers at the thighs and shins, two at the anterosuperior iliac spines, one at the first sacral vertebra, two at the lateral malleolus, and two on the first metatarsal head. Our analysis was done over a distance of 8 m with two force platforms at 4 m.
The groups were similar regarding age, sex, BMI, side of procedure, preoperative ROM, Charnley classification, and preoperative alignment (Table 1).
Statistical Methods
The a priori sample size calculation was based on a difference in walking speed of 0.1 m/second being associated with a clinically important difference in patients’ perception [50, 51, 64]. Assuming the variability in walking speed would be 0.13 m/second (which is similar to those reported in other studies investigating outcomes after TKA) [57, 64], a power of 90%, and a significance level of 5%, the required sample size was 18 patients in each group [57, 64]. A post hoc power analysis found that with the numbers available and our data distribution we had 80% power to detect a difference of 10 points in KSS.
Data that are descriptive statistics are presented as mean ± SD. Statistical analysis was performed with SPSS® 12.0 (IBM Corporation, Somers, NY, USA). Student’s paired t-tests were used for intragroup comparison of two variables and two-sample t-tests were used for intergroup comparisons of two variables.
Results
Patient-Reported Outcome Measures
At 3 months postoperatively, there were no differences in the new KSS, KOOS, or SF-12 between the patient-specific instrumentation and conventional TKA groups (p = 0.09–0.95) (Table 2). At 3 months postoperatively, all scores increased in the conventional group compared with that group’s preoperative scores, except for the KOOS sport component and SF-12 mental component subscale (p = 0.008 to p < 0.0001) (Table 3). Likewise, all scores were increased in the patient-specific instrumentation group at 3 months compared with preoperatively, except the expectation score of the new KSS and the sports and quality-of-life components of the KOOS (p = 0.017 to p < 0.0001) (Table 3).
Table 2.
Comparison of postoperative functional scores between groups
| Score (points) | 3 months postoperative | ||
|---|---|---|---|
| Patient-specific instrumentation | Conventional instrumentation | p value | |
| New Knee Society Knee Score | |||
| Objective knee score (/100) | 80 ± 7 | 82 ± 7 | 0.39 |
| Satisfaction score (/40) | 27 ± 7 | 29 ± 6 | 0.38 |
| Expectation score (/15) | 10 ± 3 | 14 ± 3 | 0.09 |
| Functional activity score (/100) | 61 ± 12 | 61 ± 13 | 0.91 |
| KOOS | |||
| Pain (/100) | 35 ± 12 | 34 ± 12 | 0.95 |
| Symptoms (/100) | 37 ± 10 | 37 ± 8 | 0.92 |
| ADL (/100) | 49 ± 15 | 48 ± 13 | 0.91 |
| Sports (/100) | 26 ± 18 | 25 ± 17 | 0.91 |
| QOL (/100) | 28 ± 13 | 27 ± 10 | 0.83 |
| SF-12 | |||
| Physical Subscale (/100) | 35 ± 8 | 35 ± 6 | 0.84 |
| Mental Subscale (/100) | 57 ± 8 | 58 ± 10 | 0.85 |
Values are mean ± SD; KOOS = Knee Injury and Osteoarthritis Outcome Score; ADL = activities of daily living; QOL = quality of life.
Table 3.
Comparison of preoperative and postoperative functional scores
| Score (points) | Patient-specific instrumentation | Conventional instrumentation | ||||
|---|---|---|---|---|---|---|
| Preoperative | 3 months postoperative | p value | Preoperative | 3 months postoperative | p value | |
| New Knee Society Knee Score | ||||||
| Objective knee score (/100) | 53 ± 13 | 80 ± 7 | < 0.0001* | 51 ± 13 | 82 ± 7 | < 0.0001* |
| Satisfaction score (/40) | 18 ± 6 | 27 ± 7 | < 0.0001* | 18 ± 7 | 29 ± 6 | < 0.0001* |
| Expectation score (/15) | 8 ± 3 | 10 ± 3 | 0.157 | 9 ± 3 | 14 ± 3 | 0.008* |
| Functional activity score (/100) | 35 ± 14 | 61 ± 12 | < 0.0001* | 32 ± 14 | 61 ± 13 | < 0.0001* |
| KOOS | ||||||
| Pain (/100) | 22 ± 11 | 35 ± 12 | 0.003* | 23± 10 | 34 ± 12 | 0.001* |
| Symptoms (/100) | 21 ± 8 | 37 ± 10 | < 0.0001* | 22 ± 6 | 37 ± 8 | < 0.0001* |
| ADL (/100) | 34 ± 15 | 49 ± 15 | 0.004* | 33 ± 12 | 48 ± 13 | 0.0004* |
| Sports (/100) | 18 ± 12 | 26 ± 18 | 0.119 | 17 ± 13 | 25 ± 17 | 0.128 |
| QOL (/100) | 21 ± 11 | 28 ± 13 | 0.075 | 20 ± 8 | 27 ± 10 | 0.003* |
| SF-12 | ||||||
| Physical subscale (/100) | 29 ± 7 | 35 ± 8 | 0.015* | 28 ± 12 | 35 ± 6 | 0.001* |
| Mental subscale (/100) | 50 ± 9 | 57 ± 8 | 0.017* | 51 ± 10 | 58 ± 10 | 0.062 |
Values are mean ± SD; * statistically significant findings; KOOS = Knee Injury and Osteoarthritis Outcome Score; ADL = activities of daily living; QOL = quality of life.
Gait Analysis
Three months after surgery, there were no differences in the analyzed gait parameters between the two groups, including spatiotemporal (double limb support, single limb support, walking speed, cadence, stride length) and kinematics/kinetics (knee varus angle, knee valgus angle, knee varus moment, knee valgus moment, knee power generation, ankle power generation) parameters (p > 0.05) (Table 4). At 3 months postoperatively, several spatiotemporal (single limb support, walking speed, cadence, and stride) gait parameters improved compared with preoperatively in the conventional instrumentation group (p = 0.02 to p < 0.0001) (Table 5). However, no gait parameters related to kinematics/kinetics (knee varus angle, knee varus moment, knee valgus angle, knee valgus moment, knee power generation, ankle power generation) improved (p = 0.07 to 0.48) (Table 5). For the patient-specific instrumentation group, at 3 months postoperatively, three spatiotemporal parameters improved (walking speed, cadence, and stride length) (p = 0.04 to p < 0.0001) and five kinematics/kinetics parameters improved (knee virus angle, knee varus moment, knee valgus angle, knee valgus moment, ankle power generation) (p = 0.03 to 0.004) (Table 5).
Table 4.
Comparison of postoperative gait during level walking (between groups)
| Parameter | Patient-specific instrumentation | Conventional instrumentation | p value |
|---|---|---|---|
| Spatiotemporal | |||
| Double limb support (%) | 45 (28–90) | 43 (28–58) | > 0.05 |
| Single limb support (%) | 44 (34–74) | 43 (30–54) | > 0.05 |
| Walking speed (m/second) | 0.75 (0.28–1) | 0.76 (0.5–1.1) | > 0.05 |
| Cadence (steps/m) | 93 (54–117) | 95 (75–122) | > 0.05 |
| Stride length (m) | 0.95 (0.6–1.16) | 0.96 (0.1–1.16) | > 0.05 |
| Kinematics/kinetics | |||
| Knee varus angle (degrees) | 6.3 (−6 to 16) | 6 (−3 to 16) | > 0.05 |
| Knee valgus angle (degrees) | −4.5 (−17 to 5) | −5.8 (−12 to 4) | > 0.05 |
| Knee varus moment (Nm/kg) | 0.4 (0.2–0.7) | 0.38 (0.1–0.7) | > 0.05 |
| Knee valgus moment (Nm/kg) | −0.05 (−0.2 to 0) | −0.1 (−0.2 to 0) | > 0.05 |
| Knee power generation (W/kg) | 0.2 (0.02–0.5) | 0.2 (0.01–0.7) | > 0.05 |
| Ankle power generation (W/kg) | 2.3 (0.4–3.6) | 2.2 (0.9–4.1) | > 0.05 |
Values are represented as mean (range).
Table 5.
Comparison of preoperative and postoperative gait during level walking
| Parameter | Patient-specific instrumentation | Conventional instrumentation | ||||
|---|---|---|---|---|---|---|
| Preoperative | Postoperative | p value | Preoperative | Postoperative | p value | |
| Spatiotemporal | ||||||
| Double limb support (%) | 49 (38–90) | 45 (28–90) | 0.2 | 47 (40–70) | 43 (28–58) | |
| Single limb support (%) | 40 (30–70) | 44 (34–74) | 0.2 | 39 (28–50) | 43 (30–54) | 0.02 |
| Walking speed (m/second) | 0.65 (0.18–0.9) | 0.75 (0.28–1) | 0.04 | 0.63 (0.5–0.78) | 0.76 (0.5–0.11) | 0.004 |
| Cadence (steps/m) | 64 (35–90) | 93 (54–117) | < 0.0001 | 66 (38–90) | 95 (75–122) | < 0.0001 |
| Stride length (m) | 0.83 (0.5–1) | 0.95 (0.6–1.16) | 0.005 | 0.81 (0.5–1) | 0.96 (0.1–1.16) | 0.003 |
| Kinematics/kinetics | ||||||
| Knee varus angle (degrees) | 9.8 (−2.8 to 20) | 6.3 (−6 to 16) | 0.03 | 9.25 (−3 to 20) | 6 (−3 to 16) | 0.07 |
| Knee valgus angle (degrees) | −8 (−20 to 1.4) | −4.5 (−17 to 5) | 0.2 | −7.95 (−13 to 0) | −5.8 (−12 to 4) | |
| Knee varus moment (Nm/kg) | 0.5 (0.31–0.79) | 0.4 (0.2–0.7) | 0.004 | 0.48 (0.3–0.8) | 0.38 (0.1–0.7) | 0.13 |
| Knee valgus moment (Nm/kg) | −0.12 (−0.29 to 0.019) | −0.05 (−0.2 to 0) | 0.34 | −0.12 (−0.25 to 0.01) | −0.1 (−0.2 to 0) | 0.51 |
| Knee power generation (W/kg) | 0.13 (0.02–0.8) | 0.2 (0.02–0.5) | 0.29 | 0.163 (0.02–0.8) | 0.2 (0.01–0.7) | 0.48 |
| Ankle power generation (W/kg) | 1.56 (0.06–2.8) | 2.3 (0.4–3.6) | 0.005 | 1.85 (0.06–4) | 2.2 (0.9–4.1) | 0.28 |
Values are represented as mean (range).
At most recent followup, there were three complications in the patient-specific instrumentation group and none in the conventional instrumentation group. Two patients in the patient-specific instrumentation group had postoperative flexion contractures between 5° and 10°. Both patients had a preoperative flexion contracture. Neither required any additional intervention. One patient in the patient-specific instrumentation group had preoperative patellar subluxation that continued postoperatively.
Discussion
Patient-specific instrumentation is a tool in the orthopaedic armamentarium with limited clinical, radiographic, and cost-effectiveness data. Although proponents of patient-specific instrumentation contend that it improves alignment, reduces costs, and improves operating room efficiency [24, 41, 44, 56], the many well-designed comparative trials have revealed no improvement in alignment, no reduction in overall cost, and no global savings in time when the entire process is analyzed [12, 25, 29, 31, 44, 45, 58, 59]. Even more concerning, there are few data regarding the functional results and gait parameters associated with this technology [49]. We hypothesized that the use of patient-specific instrumentation in TKA could improve early subjective and objective functional outcomes. As such, the goals of the current study were to compare (1) patient-reported outcomes scores, and (2) gait parameters between patients operated on with patient-specific instrumentation versus conventional instrumentation at 3 months postoperative. In this randomized clinical trial comparing patient-specific instrumentation versus conventional instrumentation, we found no benefit in pain or function and no comparative improvement in gait parameters when patient-specific instrumentation was compared with conventional TKA.
There are limitations to our study. Foremost, the sample size is small with 20 patients per group. However, the a priori power analysis suggested our sample size was adequate to identify a clinically important difference in gait speed, and the randomized study design helped ensure similarity between the two populations at baseline, further mitigating this limitation. Second, the study focused on only the first 3 months postoperatively, and the results cannot be extrapolated to longer-term followup. However, it was our intention to focus on the immediate postoperative rehabilitative period. Moreover, some studies on MIS have shown that patient-reported outcome measure and gait analysis tools are sensitive at detecting changes during the early recovery period [16, 20, 25, 27, 48]. Finally, as with all motion analysis studies, there are intrinsic limitations that include variability in gait measurements owing to body anthropometrics and independent skin motion, definition of the neutral position, and time and expense of gait analysis [64, 66].
To our knowledge, this is the only investigation to study multiple patient-reported outcomes of patient-specific instrumentation, and the only study to complete a gait analysis. Thienpont et al. [60] retrospectively reported on 10 patients who were treated with patient-specific instrumentation for extraarticular deformities and found improvements in KSS and Oxford knee scores. However, there was no control group and such improvements would be expected even without the use of patient-specific instrumentation. Pietsch et al. [49] completed a randomized clinical trial of 80 patients divided into groups with conventional instrumentation and with patient-specific instrumentation. They found no difference in the KSS at 3 months. However, the KOOS, SF-12, and gait parameters were not analyzed.
To our knowledge, no published study is dedicated to gait performance analysis after patient-specific instrumented TKA with comparison to conventional TKA. As such, no true assessment can be made with the literature. Gait analysis objectively documents comprehensive joint mechanics after TKA, particularly on knee loading and function with pathologic conditions [28, 64]. In our study, spatiotemporal parameters, kinematics, and kinetics were improved in both groups during level walking. The knee varus angle and moment were decreased, highlighting correction of the frontal plane deformity after TKA. Our findings are in accordance with those of previous studies that showed normalization of the knee varus angle and moment after TKA regardless of approach or instrumentation used [5, 23, 36, 64].
Five of our 20 patients in the patient-specific instrumentation group required intraoperative modification of the plan. This was surprising given that we specifically performed a thorough review before fabrication of the patient-specific instrumentation jigs knowing that previous studies had shown a similar rate [47, 59]. However, this may be attributable to the substantial difference in our experience with the two approaches (i.e., conventional instrumentation performed in thousands of cases versus patient-specific instrumentation in hundreds of cases). Although we were past the learning curve when the study was initiated, patient-specific instrumentation is not our standard of care.
Patient-specific instrumentation did not confer an advantage in early functional or gait outcomes 3 months after TKA as assessed by the KSS, KOOS, SF-12, and comprehensive gait analysis. However, it is possible that differences may emerge, and this study does not allow one to predict any additional variances in the intermediate followup period from 6 months to 1 year postoperatively. Although patient-specific instrumentation has a role in certain cases, such as for patients with intramedullary hardware or extraarticular deformities, its widespread use is debatable. In addition to longer followup of patient-reported outcomes and the gait analysis, long-term survivorship analyses are needed.
Acknowledgments
We acknowledge Damien Girard MD (Department of Orthopedic Surgery, Institute for Locomotion, Aix-Marseille University, Marseille), Guillaume Gauthier MS (Center of Motion and Gait Analysis, Department of Pediatric Orthopedic Surgery, Tim one Hospital, Marseille), and Elisabeth Castanet MS (Center of Motion and Gait Analysis, Department of Pediatric Orthopedic Surgery, Tim one Hospital, Marseille), for their assistance.
Footnotes
The institution of one or more of the authors (MPA) has received funding from Biomet (Warsaw, IN, USA), DePuy (Warsaw, IN, USA), Stryker (Mahwah, NJ, USA), and Zimmer (Warsaw, IN, USA). One author certifies that he (J-NAA), or a member of his immediate family has received between USD 100,000 and USD 1,000,000 from Zimmer Inc (royalties and consultant). One author certifies that he (SP), or a member of his immediate family, has received between USD 100,000 and USD 1,000,000 from Zimmer Inc (development of educational programs).
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA- approval status, of any drug or device prior to clinical use.
This work was performed at Aix-Marseille University, Marseille, France.
References
- 1.Aglietti P, Sensi L, Cuomo P, Ciardullo A. Rotational position of femoral and tibial components in TKA using the femoral transepicondylar axis. Clin Orthop Relat Res. 2008;466:2751–2755. doi: 10.1007/s11999-008-0452-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ahlback S. Osteoarthrosis of the knee: a radiographic investigation. Acta Radiol Diagn (Stockh). 1968:Suppl 277:7–72. [PubMed]
- 3.Akagi M, Matsusue Y, Mata T, Asada Y, Horiguchi M, Iida H, Nakamura T. Effect of rotational alignment on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res. 1999;366:155–163. doi: 10.1097/00003086-199909000-00019. [DOI] [PubMed] [Google Scholar]
- 4.Akagi M, Mori S, Nishimura S, Nishimura A, Asano T, Hamanishi C. Variability of extraarticular tibial rotation references for total knee arthroplasty. Clin Orthop Relat Res. 2005;436:172–176. doi: 10.1097/01.blo.0000160027.52481.32. [DOI] [PubMed] [Google Scholar]
- 5.Alnahdi AH, Zeni JA, Snyder-Mackler L. Gait after unilateral total knee arthroplasty: frontal plane analysis. J Orthop Res. 2011;29:647–652. doi: 10.1002/jor.21323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anouchi YS, Whiteside LA, Kaiser AD, Milliano MT. The effects of axial rotational alignment of the femoral component on knee stability and patellar tracking in total knee arthroplasty demonstrated on autopsy specimens. Clin Orthop Relat Res. 1993;287:170–177. [PubMed] [Google Scholar]
- 7.Argenson JN, Parratte S, Ashour A, Komistek RD, Scuderi GR. Patient-reported outcome correlates with knee function after a single-design mobile-bearing TKA. Clin Orthop Relat Res. 2008;466:2669–2676. doi: 10.1007/s11999-008-0418-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Argenson JN, Parratte S, Ashour A, Saintmard B, Aubaniac JM. The outcome of rotating-platform total knee arthroplasty with cement at a minimum of ten years of follow-up. J Bone Joint Surg Am. 2012;94:638–644. doi: 10.2106/JBJS.K.00263. [DOI] [PubMed] [Google Scholar]
- 9.Argenson JN, Parratte S. Flecher X [Minimally invasive total knee arthroplasty][in French] Rev Chir Orthop Reparatrice Appar Mot. 2005;91:28–30. doi: 10.1016/S0035-1040(05)84502-7. [DOI] [PubMed] [Google Scholar]
- 10.Ast MP, Nam D, Haas SB. Patient-specific instrumentation for total knee arthroplasty: a review. Orthop Clin North Am. 2012;43:e17–e22. doi: 10.1016/j.ocl.2012.07.004. [DOI] [PubMed] [Google Scholar]
- 11.Bargren JH, Blaha JD, Freeman MA. Alignment in total knee arthroplasty: correlated biomechanical and clinical observations. Clin Orthop Relat Res. 1983;173:178–183. [PubMed] [Google Scholar]
- 12.Barrett W, Hoeffel D, Dalury D, Mason JB, Murphy J, Himden S. In-vivo alignment comparing patient specific instrumentation with both conventional and computer assisted surgery (CAS) instrumentation in total knee arthroplasty. J Arthroplasty. 2014;29:343–347. doi: 10.1016/j.arth.2013.06.029. [DOI] [PubMed] [Google Scholar]
- 13.Bellemans J, Robijns F, Duerinckx J, Banks S, Vandenneucker H. The influence of tibial slope on maximal flexion after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2005;13:193–196. doi: 10.1007/s00167-004-0557-x. [DOI] [PubMed] [Google Scholar]
- 14.Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, Faris GW, Davis KE. Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res. 2004;428:26–34. doi: 10.1097/01.blo.0000148578.22729.0e. [DOI] [PubMed] [Google Scholar]
- 15.Berger RA, Crossett LS, Jacobs JJ, Rubash HE. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res. 1998;356:144–153. doi: 10.1097/00003086-199811000-00021. [DOI] [PubMed] [Google Scholar]
- 16.Bertsch C, Holz U, Konrad G, Vakili A. Oberst M [Early clinical outcome after navigated total knee arthroplasty: comparison with conventional implantation in TKA: a controlled and prospective analysis][in German] Orthopade. 2007;36:739–745. doi: 10.1007/s00132-007-1122-3. [DOI] [PubMed] [Google Scholar]
- 17.Bonutti PM, Zywiel MG, McGrath MS, Mont MA. Surgical techniques for minimally invasive exposures for total knee arthroplasty. Instr Course Lect. 2010;59:83–91. [PubMed] [Google Scholar]
- 18.Bonutti PM, Zywiel MG, Seyler TM, Lee SY, McGrath MS, Marker DR, Mont MA. Minimally invasive total knee arthroplasty using the contralateral knee as a control group: a case-control study. Int Orthop. 2010;34:491–495. doi: 10.1007/s00264-009-0775-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bonutti PM, Zywiel MG, Ulrich SD, McGrath MS, Mont MA. Minimally invasive total knee arthroplasty: pitfalls and complications. Am J Orthop (Belle Mead NJ). 2010;39:480–484. [PubMed] [Google Scholar]
- 20.Cheng T, Pan XY, Mao X, Zhang GY, Zhang XL. Little clinical advantage of computer-assisted navigation over conventional instrumentation in primary total knee arthroplasty at early follow-up. Knee. 2012;19:237–245. doi: 10.1016/j.knee.2011.10.001. [DOI] [PubMed] [Google Scholar]
- 21.Choong PF, Dowsey MM, Stoney JD. Does accurate anatomical alignment result in better function and quality of life? Comparing conventional and computer-assisted total knee arthroplasty. J Arthroplasty. 2009;24:560–569. doi: 10.1016/j.arth.2008.02.018. [DOI] [PubMed] [Google Scholar]
- 22.Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty. 2009;24(6 suppl):39–43. doi: 10.1016/j.arth.2009.04.034. [DOI] [PubMed] [Google Scholar]
- 23.Hatfield GL, Hubley-Kozey CL. Astephen Wilson JL, Dunbar MJ. The effect of total knee arthroplasty on knee joint kinematics and kinetics during gait. J Arthroplasty. 2011;26:309–318. doi: 10.1016/j.arth.2010.03.021. [DOI] [PubMed] [Google Scholar]
- 24.Heyse TJ, Tibesku CO. Improved femoral component rotation in TKA using patient-specific instrumentation. Knee. 2014;21:268–271. doi: 10.1016/j.knee.2012.10.009. [DOI] [PubMed] [Google Scholar]
- 25.Howell SM, Hodapp EE, Kuznik K, Hull ML. In vivo adduction and reverse axial rotation (external) of the tibial component can be minimized. Orthopedics. 2009;32:319. doi: 10.3928/01477447-20090501-04. [DOI] [PubMed] [Google Scholar]
- 26.Huddleston JI, Scott RD, Wimberley DW. Determination of neutral tibial rotational alignment in rotating platform TKA. Clin Orthop Relat Res. 2005;440:101–106. doi: 10.1097/01.blo.0000185448.43622.77. [DOI] [PubMed] [Google Scholar]
- 27.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 28.Kaufman KR, Hughes C, Morrey BF, Morrey M, An KN. Gait characteristics of patients with knee osteoarthritis. J Biomech. 2001;34:907–915. doi: 10.1016/S0021-9290(01)00036-7. [DOI] [PubMed] [Google Scholar]
- 29.Klatt BA, Goyal N, Austin MS, Hozack WJ. Custom-fit total knee arthroplasty (OtisKnee) results in malalignment. J Arthroplasty. 2008;23:26–29. doi: 10.1016/j.arth.2007.10.001. [DOI] [PubMed] [Google Scholar]
- 30.Lemaire P, Pioletti DP, Meyer FM, Meuli R, Dorfl J, Leyvraz PF. Tibial component positioning in total knee arthroplasty: bone coverage and extensor apparatus alignment. Knee Surg Sports Traumatol Arthrosc. 1997;5:251–257. doi: 10.1007/s001670050059. [DOI] [PubMed] [Google Scholar]
- 31.Lombardi AV, Jr, Berend KR, Adams JB. Patient-specific approach in total knee arthroplasty. Orthopedics. 2008;31:927–930. doi: 10.3928/01477447-20080901-21. [DOI] [PubMed] [Google Scholar]
- 32.Longstaff LM, Sloan K, Stamp N, Scaddan M, Beaver R. Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. J Arthroplasty. 2009;24:570–578. doi: 10.1016/j.arth.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 33.Lotke PA, Ecker ML. Influence of positioning of prosthesis in total knee replacement. J Bone Joint Surg Am. 1977;59:77–79. [PubMed] [Google Scholar]
- 34.Lustig S, Scholes CJ, Oussedik SI, Kinzel V, Coolican MR, Parker DA. Unsatisfactory accuracy as determined by computer navigation of VISIONAIRE patient-specific instrumentation for total knee arthroplasty. J Arthroplasty. 2013;28:469–473. doi: 10.1016/j.arth.2012.07.012. [DOI] [PubMed] [Google Scholar]
- 35.Mahoney OM, Kinsey TL. 5- to 9-year survivorship of single-radius, posterior-stabilized TKA. Clin Orthop Relat Res. 2008;466:436–442. doi: 10.1007/s11999-007-0070-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mandeville D, Osternig LR, Lantz BA, Mohler CG, Chou LS. The effect of total knee replacement on the knee varus angle and moment during walking and stair ascent. Clin Biomech (Bristol, Avon). 2008;23:1053–1058. [DOI] [PubMed]
- 37.Matsuda S, Miura H, Nagamine R, Urabe K, Hirata G, Iwamoto Y. Effect of femoral and tibial component position on patellar tracking following total knee arthroplasty: 10-year follow-up of Miller-Galante I knees. Am J Knee Surg. 2001;14:152–156. [PubMed] [Google Scholar]
- 38.Miller MC, Berger RA, Petrella AJ, Karmas A, Rubash HE. Optimizing femoral component rotation in total knee arthroplasty. Clin Orthop Relat Res. 2001;392:38–45. doi: 10.1097/00003086-200111000-00005. [DOI] [PubMed] [Google Scholar]
- 39.Moher D, Hopewell S, Schulz KF, Montori V, Gotzsche PC, Devereaux PJ, Elbourne D, Egger M, Altman DG; Consolidated Standards of Reporting Trials Group. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomised trials. J Clin Epidemiol. 2010;63:e1–37. [DOI] [PubMed]
- 40.Mont MA, Zywiel MG, McGrath MS, Bonutti PM. Scientific evidence for minimally invasive total knee arthroplasty. Instr Course Lect. 2010;59:73–82. [PubMed] [Google Scholar]
- 41.Nam D, McArthur BA, Cross MB, Pearle AD, Mayman DJ, Haas SB. Patient-specific instrumentation in total knee arthroplasty: a review. J Knee Surg. 2012;25:213–219. doi: 10.1055/s-0032-1319785. [DOI] [PubMed] [Google Scholar]
- 42.Ng VY, DeClaire JH, Berend KR, Gulick BC, Lombardi AV., Jr Improved accuracy of alignment with patient-specific positioning guides compared with manual instrumentation in TKA. Clin Orthop Relat Res. 2012;470:99–107. doi: 10.1007/s11999-011-1996-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Noble PC, Scuderi GR, Brekke AC, Sikorskii A, Benjamin JB, Lonner JH, Chadha P, Daylamani DA, Scott WN, Bourne RB. Development of a new Knee Society scoring system. Clin Orthop Relat Res. 2012;470:20–32. doi: 10.1007/s11999-011-2152-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nunley RM, Ellison BS, Ruh EL, Williams BM, Foreman K, Ford AD, Barrack RL. Are patient-specific cutting blocks cost-effective for total knee arthroplasty? Clin Orthop Relat Res. 2012;470:889–894. doi: 10.1007/s11999-011-2221-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nunley RM, Ellison BS, Zhu J, Ruh EL, Howell SM, Barrack RL. Do patient-specific guides improve coronal alignment in total knee arthroplasty? Clin Orthop Relat Res. 2012;470:895–902. doi: 10.1007/s11999-011-2222-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Olcott CW, Scott RD. The Ranawat Award: femoral component rotation during total knee arthroplasty. Clin Orthop Relat Res. 1999;367:39–42. doi: 10.1097/00003086-199910000-00005. [DOI] [PubMed] [Google Scholar]
- 47.Parratte S, Blanc G, Boussemart T, Ollivier M, Le Corroller T, Argenson JN. Rotation in total knee arthroplasty: no difference between patient-specific and conventional instrumentation. Knee Surg Sports Traumatol Arthrosc. 2013;21:2213–2219. doi: 10.1007/s00167-013-2623-8. [DOI] [PubMed] [Google Scholar]
- 48.Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am. 2010;92:2143–2149. doi: 10.2106/JBJS.I.01398. [DOI] [PubMed] [Google Scholar]
- 49.Pietsch M, Djahani O, Hochegger M, Plattner F, Hofmann S. Patient-specific total knee arthroplasty: the importance of planning by the surgeon. Knee Surg Sports Traumatol Arthrosc. 2013;21:2220–2226. doi: 10.1007/s00167-013-2624-7. [DOI] [PubMed] [Google Scholar]
- 50.Purser JL, Weinberger M, Cohen HJ, Pieper CF, Morey MC, Li T, Williams GR, Lapuerta P. Walking speed predicts health status and hospital costs for frail elderly male veterans. J Rehabil Res Dev. 2005;42:535–546. doi: 10.1682/JRRD.2004.07.0087. [DOI] [PubMed] [Google Scholar]
- 51.Redelmeier DA, Bayoumi AM, Goldstein RS, Guyatt GH. Interpreting small differences in functional status: the Six Minute Walk test in chronic lung disease patients. Am J Respir Crit Care Med. 1997;155:1278–1282. doi: 10.1164/ajrccm.155.4.9105067. [DOI] [PubMed] [Google Scholar]
- 52.Rhoads DD, Noble PC, Reuben JD, Mahoney OM, Tullos HS. The effect of femoral component position on patellar tracking after total knee arthroplasty. Clin Orthop Relat Res. 1990;260:43–51. [PubMed] [Google Scholar]
- 53.Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement: its effect on survival. Clin Orthop Relat Res. 1994;299:153–156. [PubMed] [Google Scholar]
- 54.Roos EM, Toksvig-Larsen S. Knee injury and Osteoarthritis Outcome Score (KOOS): validation and comparison to the WOMAC in total knee replacement. Health Qual Life Outcomes. 2003;1:17. doi: 10.1186/1477-7525-1-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sharkey PF, Hozack WJ, Rothman RH, Shastri S, Jacoby SM. Insall Award paper: why are total knee arthroplasties failing today? Clin Orthop Relat Res. 2002;404:7–13. doi: 10.1097/00003086-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 56.Silva A, Sampaio R, Pinto E. Patient-specific instrumentation improves tibial component rotation in TKA. Knee Surg Sports Traumatol Arthrosc. 2014;22:636–642. doi: 10.1007/s00167-013-2639-0. [DOI] [PubMed] [Google Scholar]
- 57.Smith AJ, Lloyd DG, Wood DJ. A kinematic and kinetic analysis of walking after total knee arthroplasty with and without patellar resurfacing. Clin Biomech (Bristol, Avon). 2006;21:379–386. [DOI] [PubMed]
- 58.Spencer BA, Mont MA, McGrath MS, Boyd B, Mitrick MF. Initial experience with custom-fit total knee replacement: intra-operative events and long-leg coronal alignment. Int Orthop. 2009;33:1571–1575. doi: 10.1007/s00264-008-0693-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Stronach BM, Pelt CE, Erickson J, Peters CL. Patient-specific total knee arthroplasty required frequent surgeon-directed changes. Clin Orthop Relat Res. 2013;471:169–174. doi: 10.1007/s11999-012-2573-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Thienpont E, Paternostre F, Pietsch M, Hafez M, Howell S. Total knee arthroplasty with patient-specific instruments improves function and restores limb alignment in patients with extra-articular deformity. Knee. 2013;20:407–411. doi: 10.1016/j.knee.2013.07.001. [DOI] [PubMed] [Google Scholar]
- 61.Victor J, Dujardin J, Vandenneucker H, Arnout N, Bellemans J. Patient-specific guides do not improve accuracy in total knee arthroplasty: a prospective randomized controlled trial. Clin Orthop Relat Res. 2014;472:263–271. doi: 10.1007/s11999-013-2997-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 63.Wasielewski RC, Galante JO, Leighty RM, Natarajan RN, Rosenberg AG. Wear patterns on retrieved polyethylene tibial inserts and their relationship to technical considerations during total knee arthroplasty. Clin Orthop Relat Res. 1994;299:31–43. [PubMed] [Google Scholar]
- 64.Wegrzyn J, Parratte S, Coleman-Wood K, Kaufman KR, Pagnano MW. The John Insall award: no benefit of minimally invasive TKA on gait and strength outcomes: a randomized controlled trial. Clin Orthop Relat Res. 2013;471:46–55. doi: 10.1007/s11999-012-2486-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Yoshii I, Whiteside LA, White SE, Milliano MT. Influence of prosthetic joint line position on knee kinematics and patellar position. J Arthroplasty. 1991;6:169–177. doi: 10.1016/S0883-5403(11)80013-6. [DOI] [PubMed] [Google Scholar]
- 66.Yu B, Kienbacher T, Growney ES, Johnson ME, An KN. Reproducibility of the kinematics and kinetics of the lower extremity during normal stair-climbing. J Orthop Res. 1997;15:348–352. doi: 10.1002/jor.1100150306. [DOI] [PubMed] [Google Scholar]