Abstract
Background
The rotator cuff plays a significant role in the static and dynamic stability of the glenohumeral joint. Rotator cuff tears may occur after shoulder dislocations, whether in younger athletes or older patients with age-related tendon degeneration. Untreated tears may cause persistent pain, dysfunction, instability, and degenerative changes. A thorough understanding of when to look for rotator cuff tears after shoulder dislocations and how best to manage them may decrease patients’ pain and improve function.
Questions/purposes
We systematically reviewed the available literature to better understand (1) when a rotator cuff tear should be suspected after a dislocation, (2) whether surgical or nonsurgical approaches result in better scores for pain and satisfaction in patients with rotator cuff tears resulting from shoulder dislocations, and (3) whether intraarticular lesions, rotator cuff tears, or both should be addressed when surgery is performed.
Methods
We systematically searched MEDLINE®, CINAHL, and EMBASE for studies published from 1950 to 2012. We included studies reporting outcomes after treatment in patients with rotator cuff tears and shoulder dislocations. We excluded case reports, studies without any treatment, and studies about patients treated with arthroplasty. Five Level III and six Level IV studies were ultimately selected for review.
Results
Patients with persistent pain or dysfunction after a shoulder dislocation often had a concomitant rotator cuff tear. Surgical repair resulted in improved pain relief and patient satisfaction compared to nonoperative management. Repair of the rotator cuff, along with concomitant capsulolabral lesions, helped restore shoulder stability. While these findings are based on Level III and IV evidence, better long-term studies with larger cohorts are needed to strengthen evidence-based recommendations.
Conclusions
Persistent pain and dysfunction after a shoulder dislocation should prompt evaluation of the rotator cuff, especially in contact or overhead athletes, patients older than 40 years, or those with nerve injury. Surgery should be considered in the appropriately active patient with a rotator cuff tear after dislocation. While the current literature suggests improved stability and function after surgical repair of the rotator cuff, higher-quality prospective studies are necessary to make definitive conclusions.
Introduction
The shoulder is the most mobile and least constrained joint in the human body [2]. A complex combination of static and dynamic stabilizers about the glenohumeral joint balances this inherent mobility with functional stability. A great deal of the dynamic restraint of the glenohumeral joint arises from the concavity-compression mechanism created by the rotator cuff [15, 18]. This mechanism stabilizes the shoulder at middle range of motion (ROM) when the capsulolabral structures are lax and at terminal ROM through muscle activity that limits motion and decreases strain on the glenohumeral ligaments [6, 16, 21, 27]. The shoulder muscle activity balances translational (destabilizing) forces with compressive (stabilizing) forces to maintain glenohumeral joint stability throughout its arc of motion [20, 22, 23, 25, 31].
When the active and passive restraints of the rotator cuff are lost, the shoulder may become unstable. In a cadaveric study, a 50% decrease in rotator cuff muscle activity resulted in a 50% increase in the occurrence of dislocations in all positions examined [34]. Additionally, a smaller capsulolabral (Bankart) lesion was needed to induce instability in a rotator cuff-deficient model compared to an intact rotator cuff [33].
There are similar rates of a single dislocation event among patients older or younger than 45 years [35]. After an anterior dislocation, McLaughlin [26] postulated that in younger patients the anterior capsulolabral structures most commonly fail. In elderly patients, the posterior structures are more likely to fail secondary to preexisting rotator cuff weakness. The possibility of a rotator cuff tear after an anterior dislocation was first discussed by Stevens in 1926 [36]. This posterior mechanism of instability was further popularized by Craig [7] in a reported series of patients older than 60 years with rotator cuff failure and recurrent instability after an anterior dislocation, where failure of the posterior rotator cuff tendons may account for recurrent anterior instability. The overall frequency of rotator cuff tears after an anterior dislocation ranges between 7% and 32% and rises with advancing age [5, 17, 37].
Treatment options have focused on the consequences of an instability episode. Recurrence is of primary concern after an anterior dislocation in younger patients [12–14, 36], and thus treatment is directed toward repairing the damaged capsulolabral structures to restore stability. In older patients, treatment focuses on preventing both recurrent instability and the morbidity associated with a dysfunctional rotator cuff, ranging from pain and loss of function to disabling degenerative changes [10, 24, 28].
However, several key clinical questions remain and form the basis for this systematic review of the literature: (1) When should rotator cuff pathology be suspected in patients with shoulder instability? (2) If both a cuff tear and shoulder instability are present, will pain and outcome scores improve more dramatically with surgical or nonsurgical treatments? And (3) when surgery is performed, should treatment be directed to intraarticular pathology, rotator cuff lesions, or both?
Search Strategy and Criteria
We searched MEDLINE®, CINAHL, and EMBASE databases for studies published in English between January 1950 and December 2012. Keywords used to identify relevant articles included “shoulder instability AND rotator cuff” or “shoulder dislocation AND rotator cuff” or “glenohumeral instability AND rotator cuff” or “glenohumeral dislocation AND rotator cuff”. MeSH terms were also used, including “shoulder dislocation AND rotator cuff”. The references of relevant review papers and each included article were also searched. Our initial search strategy revealed 553 articles for consideration.
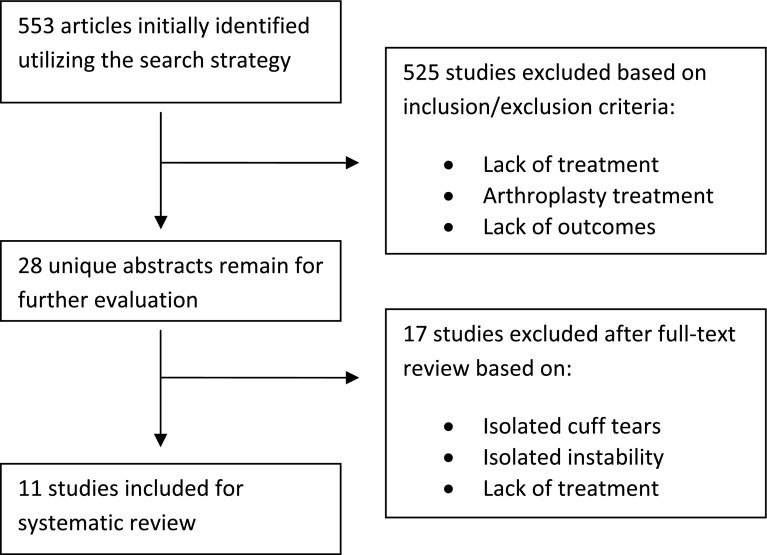
We included studies reporting outcomes (eg, pain, ROM, stability, or functional scores) after treatment for patients with rotator cuff tears and glenohumeral dislocation/instability (Fig. 1). Studies reporting two or more patients were included. Treatment options included both nonoperative management with physical therapy or operative repair or reconstruction. We excluded studies in which patients did not undergo treatment, case reports of one patient, or studies with outcomes after arthroplasty. We excluded studies of patient populations with isolated instability without rotator cuff tears or isolated cuff tears without instability/dislocation. After applying these inclusion and exclusion criteria, ultimately 11 studies were included in the systematic review [3, 8, 10, 11, 17, 27, 29, 32, 37, 38, 42] (Table 1). Five of the studies were Level III evidence [10, 17, 37, 38, 42], and the remainder represented Level IV evidence [3, 8, 11, 27, 29, 32]. Three of the studies [3, 8, 27] reported entirely on patients with combined cuff pathology and shoulder instability, and the remainder included subgroups with combined pathology. Six of the studies specifically reported on patients older than 40 years [10, 27, 29, 32, 37, 38].
Fig. 1.
A flowchart shows the selection process of studies included in the systematic review.
Table 1.
Summary of studies reviewed
| Study | Year | Injury pattern | Total number of patients | Number of patients with instability and RCT | Rotator cuff lesions | Intervention | Age (years)* | Followup (months)* | Outcome | Complications | Redislocations |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Banerjee et al. [3] | 2012 | 2 judo players with recurrent instability with PASTA, no labral lesions | 2 | 2 | Partial-thickness supraspinatus | Arthroscopic PASTA repair (Lo and Burkhart technique) | 26 and 16 | 19 (18–20) | 1st patient: 100 (C-M), 100 (Rowe) 2nd patient: 97 (C-M), 96 (Rowe) |
None | None |
| Goldberg et al. [8] | 2003 | 6 elite rugby players with instability and large cuff tears (5 diagnosed by MRI, 1 by CT arthrography) | 6 | 6 | Mean tear size: 3.8 cm (1.5–6 cm) involving supraspinatus and often infraspinatus | Open cuff repair, stabilization ~10 weeks later | 26.5 (23–29) | 34.3 (12–50) | Returned to contact sports in 9 months, ER/IR 70%/76% of normal; negative apprehension, 5/5 cuff strength | None | None |
| Hawkins et al. [10] | 1986 | Group I: anterior dislocation; age > 40 years | 39 | 35 (mostly clinical findings of RCT, 22 with positive arthrograms) | 22/26 positive arthrograms, no other information available | Nonoperative | 61.2 | 32 (24–42) | 30/39 remained symptomatic; 15 with night pain; 2/3 with impaired motion | NA | 2 patients (both with RCT) |
| Group II: dislocation; age > 40 years; persistent symptoms | 14 | 14 (clinical findings of RCT) | Of 7 RCTs undergoing surgery, defects were often large, 1 irreparable | PT (in 7); SAD, RCR (in 7) | 59.3 (40–70) | 32 (24–49) | 0/7 treated with PT had adequate pain relief or function; acceptable pain relief in 4/7 after surgery | NA | |||
| Group III: postoperative patients; age > 40 years; anterior dislocation | 8 | 2 (RCT on arthrography) | NA | Reconstruction for dislocation (and RCR when RCT present) | 45 (43–59) | 61 (41–81) | Patients with RCTs had poor function, 1/2 satisfied with pain relief | None | |||
| Hawkins et al. [11] | 1999 | Full-thickness RCT (all with clinical findings, 10 by arthrography); age < 40 years | 19 | 5 with dislocations | 6 small (< 1 cm), 5 moderate (1–3 cm), 5 large (3–5 cm), 3 massive (> 5 cm); all full-thickness | Open stabilization and RCR | 33.4 (23–40) | 68.4 (25.2–144) | All 5 had improved pain and overall clinical improvement; 5 returned to full employment, 3 to sports | None | None |
| Imhoff et al. [17] | 2010 | Anterior instability treated with arthroscopic stabilization | 190 | 15 with RCT (diagnosed at surgery) | 12 partial-thickness, 3 full-thickness | Arthroscopic capsulorraphy, 4 with mini-open RCR | 28.0 (14.4–59.2) | 37.4 (14.1–72.8) | Impairment in Rowe, C-M, ASES, 12-item questionnaire in full-thickness RCT vs partial or no tear | NA | Presence of RCT did not influence redislocation |
| Neviaser et al. [27] | 1993 | Group I: primary anterior dislocation; age > 40 years; missed RCT | 37 | 26 (diagnosed by arthrography) | 23 patients with full-thickness supraspinatus, partial-thickness infraspinatus | SAD, cuff repair (in 23) or reconstruction (in 3) | 59.8 (35–83) | 58.8 (24–132) | Dramatic pain relief, most regained full motion | NA | None |
| Group II: recurrent anterior dislocation; age > 40 years; missed RCT | 11 (diagnosed by arthrography) | All patients had subscapularis ruptures | Subscapularis repair to tuberosity | Good pain relief, regained full elevation | |||||||
| Pevny et al. [29] | 1998 | Anterior dislocation; age > 40 years | 52 | 12 (RCT diagnosed by MRI, arthrogram, or clinical findings) | NA | Nonoperative (in 6) | 56 (40–79) | 34 (24–61) | 3 of 6 had good-to-excellent outcomes | 10% adhesive capsulitis; 8% axillary palsy | None |
| RCR (in 6) | 5 of 6 had good-to-excellent outcomes | None | |||||||||
| Porcellini et al. [32] | 2006 | Recurrent instability; age > 40 years | 150 | 50 (RCT diagnosed by MRI) | 32% supraspinatus, 10% subscapularis, 8% infraspinatus, 26% combined tears | Arthroscopic Bankart repair and RCR | 48.1 (± 6.4) | 36 (24–52) | C-M: 69.4 ± 11.1; Rowe: 78.9 ± 15.2 | NA | 2 cases, treated with Bristow-Laterjet, both had irreparable cuffs |
| Simank et al. [37] | 2006 | Anterior dislocation; age > 40 years | 65 | 33 (diagnosed by ultrasonography) | 54% full-thickness; all medium to large (1–5 cm) | PT (in 18) | 59 (40.1–86.7) | 12 (minimum) | Surgically treated patients were more satisfied and had higher outcome scores | No major complications | 3 recurrences |
| NA | Mini-open RCR (in 15) | No recurrences | |||||||||
| Sonnabend [38] | 1994 | Anterior dislocation; age > 40 years; subgroup with persistent pain or weakness | 53 | 11 with RCT on arthrography | 2 with supraspinatus and infraspinatus, 3 with subscapularis | Nonoperative (in 6) | 58 | 24 (minimum) | All had weakness in forward flexion, abduction; 2 patients with pain | NA | None |
| SAD, RCR (in 5) | All virtually pain free; 4/5 regained strong forward flexion, abduction | None | |||||||||
| Voos et al. [42] | 2007 | Combined labral tear and RCT (diagnosed by MRI) | 30 | 16 with Bankart lesions | 87% with full-thickness, 13% with high-grade partial-thickness | Arthroscopic RCR and Bankart repair | 47 (36–61) | 32.4 (24–54) | L’Insalata: 95.0; ASES: 95.8 (Bankart group); 90% good-to-excellent outcomes, 77% returned to sports (all patients) | 2 recurrent RCT | None |
* Values are expressed as mean, with range in parentheses; RCT = rotator cuff tear; PASTA = partial articular surface tendon avulsion; NA = not available; PT = physical therapy; SAD = subacromial decompression; RCR = rotator cuff repair; C-M = Constant-Murley score; ER = external rotation; IR = internal rotation; ASES = American Shoulder and Elbow Society score.
Data were extracted from each included article and entered into a spreadsheet for analysis. Pertinent information extracted included author, date and journal of publication, study design (and level of evidence), patient demographics (mean age, mean followup, injury pattern, rotator cuff lesion size and location, total number of patients, and number of patients with combined instability and rotator cuff pathology), modality for diagnosis, treatment intervention, outcomes, complications, and redislocation rates. Many studies reported on outcomes in a heterogeneous population. For these studies, data for the subgroup of patients with combined instability and rotator cuff pathology were extracted. Data were also separately reported among subgroups if the patients underwent different treatment options (eg, nonoperative versus operative repair). Both authors (MMG, JKS) assessed and discussed the quality of evidence, including a risk of bias assessment for each study (Table 2).
Table 2.
Risk of bias assessment for included studies
| Risk of bias criterion | Banerjee et al. [3] | Goldberg et al. [8] | Hawkins et al. [10] | Hawkins et al. [11] | Imhoff et al. [17] | Neviaser et al. [27] | Pevny et al. [29] | Porcellini et al. [32] | Simank et al. [37] | Sonnabend [38] | Voos et al. [42] |
|---|---|---|---|---|---|---|---|---|---|---|---|
| (1) Is the outcome absent at the start of the study? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| (2) Did analyses account for clustering at the group level? | No | No | No | No | No | No | No | No | No | No | No |
| (3a) Were the outcome assessors (for the primary outcome) blind to the intervention? | No | No | No | No | No | No | No | No | No | No | No |
| (3b) Was the outcome measurement performed in the same manner with similar intensity in the groups being compared? | Yes | Yes | Not known | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| (4) Did similarly trained individuals administer the intervention across groups? | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| (5) Were the groups similar at baseline? | Yes | Yes | No | No | Yes | No | No | Yes | No | No | Yes |
| (6) Did the authors perform analyses adjusting for known confounders? | No | No | No | No | Yes | No | No | No | Yes | No | No |
Results
Patients with persistent pain or dysfunction after a shoulder dislocation often had a concomitant rotator cuff tear. Three of the included studies [10, 27, 38] reported on patients with persistent pain and weakness after shoulder dislocation. These patients remained symptomatic because of a concomitant rotator cuff tear. Reviewing these findings helps us understand when rotator cuff pathology should be suspected after a dislocation. In 1986, Hawkins et al. [10] reported on 61 patients older than 40 years after an anterior dislocation. One subgroup of 14 patients was referred to their institution because of persistent pain and weakness after a trial of physiotherapy. All patients were subsequently diagnosed with a rotator cuff tear. In 1993, Neviaser et al. [27] reported outcomes on 37 patients older than 40 years referred to the authors’ institution with a previously undiagnosed rotator cuff tear after a primary anterior dislocation. These patients were unable to elevate the arm after reduction and were unable to regain function after physiotherapy. This loss of function was mistakenly attributed to presumed axillary nerve palsy before referral to the authors. The rotator cuff tears were subsequently diagnosed after arthrographic evaluation. The mean time from dislocation to diagnosis of the cuff tear was 7.2 months. Eleven of the patients had recurrent instability at the time of evaluation, all of whom were diagnosed with a subscapularis rupture. Similarly, Sonnabend [38] in 1994 reported outcomes after anterior dislocation in patients older than 40 years. In this study, a subgroup of 13 patients had persistent pain and weakness 3 weeks after the dislocation. All 13 patients were subsequently diagnosed with rotator cuff tears. However, the remaining asymptomatic patients did not undergo further investigation, and it is unknown whether these patients had rotator cuff tears or not. The authors concluded that persistent pain and weakness after primary dislocation in this age group are indications for further evaluation. Similar presentations were noted by Goldberg et al. [8] in a series of elite young rugby players. Five of the six participants had symptoms before a catastrophic injury, including difficulty with abduction and a sensation of a “dead arm” with forceful overhead muscular activity. After the catastrophic dislocation event, all six patients presented with signs and symptoms of a rotator cuff tear, which was confirmed by either MRI with arthrography or CT arthrography. In these studies, a rotator cuff tear was diagnosed when a patient experienced persistent pain and weakness after a shoulder dislocation. The majority of these studies involved significant selection bias and did not account for potential confounding variables, and so their results should be interpreted with some caution.
Patients with a rotator cuff tear after a dislocation showed decreased pain and improved function after surgery compared to patients treated nonoperatively. Four of the studies [10, 29, 37, 38] compared outcomes in this patient population after treatment with physical therapy or surgery. In the series presented by Hawkins et al. [10], 30 of the 39 patients in the subgroup treated nonoperatively remained symptomatic. Two-thirds of these patients had persistently impaired motion. The same study compared a subgroup of 14 patients referred to their institution, one half of whom were treated nonoperatively and the other half with rotator cuff repair. None of the patients in the nonoperative group had adequate pain relief or restoration of function. Four of the seven patients undergoing surgery reported acceptable pain relief. Pevny et al. [29] similarly reported a subgroup of 12 patients with rotator cuff tears after a dislocation, one half of whom were treated nonoperatively and the other half with rotator cuff repair. After surgery, 84% of patients reported good-to-excellent results per the Rowe shoulder scale, compared to 50% in the nonoperatively managed group. Simank et al. [37] reported on 33 patients older than 40 years with rotator cuff tear after dislocation; 18 elected nonoperative management with physical therapy and 15 underwent mini-open rotator cuff repair. Instability recurred in three patients treated nonoperatively but in none after surgery. Subjective stability, adapted Constant-Murley scores, and satisfaction were significantly higher in patients receiving surgery than for patients receiving physical therapy alone. Sonnabend [38] presented a subgroup of 11 patients with rotator cuff tears after anterior dislocations; six patients were treated with physiotherapy and five underwent rotator cuff repair. All of the patients treated with physiotherapy had persistent weakness, while 80% of patients regained strong forward flexion and abduction after surgery. While many of these studies are small and retrospective in nature, the overall results suggested that patients undergoing surgery fared better than those treated nonoperatively.
Patients who underwent rotator cuff repair showed improved shoulder stability and function. All of the studies in our review included a subgroup of patients who underwent surgery. In five of these studies, a rotator cuff repair alone with or without a subacromial decompression was performed on the included patients [3, 10, 27, 29, 38]. Mean outcomes (pain relief, Rowe shoulder scores, and Constant-Murley scores) improved in all studies. In two of the studies, the absence of a capsulolabral lesion was specifically noted in all patients [3, 27]. Four of the studies specifically included patients with a capsulolabral lesion and rotator cuff tear who underwent both an anterior stabilization and rotator cuff repair [8, 11, 32, 42]. Mean outcomes (pain relief, Rowe shoulder scores, or American Shoulder and Elbow Society scores) improved in all studies, and redislocation was reported in only one study where two patients had irreparable cuff tears [32]. One study [28] included a subgroup of patients with recurrent instability before presentation and subscapularis rupture. These patients had restored stability after subscapularis repair to the lesser tuberosity. The surgeries were performed in a staged fashion in a study by Goldberg et al. [8]; open anterior stabilization was performed at a mean of 9.5 weeks after the open rotator cuff repair in all patients. Imhoff et al. [17] presented a subgroup of 15 patients with anterior capsulolabral injury and rotator cuff tears; 11 patients underwent only arthroscopic capsulorraphy and four patients underwent anterior stabilization and mini-open rotator cuff repair. They concluded that the presence of a rotator cuff tear did not influence redislocation. In all studies, pain was relieved, shoulder function was improved, and stability was restored in the majority of patients who underwent rotator cuff repair. Where a capsulolabral lesion was noted, repair of the lesion improved pain and functional outcomes. These studies, however, were retrospective and many did not include a comparison group; thus, it is difficult to draw definitive conclusions regarding treatment.
Discussion
The rotator cuff significantly contributes to the active and passive stability of the glenohumeral joint [6, 16, 20–23, 25, 27, 31]. The rotator cuff may become susceptible to injury in younger athletes who endure repetitive microtrauma to the shoulder either during overhead throwing motions or while engaging in contact sports [8, 31]. Older patients undergo age-related degenerative changes of the rotator cuff tendons [39, 40]. In either population, a single dislocation event may damage the already-weakened rotator cuff. The torn rotator cuff may cause continued dysfunction and recurrent instability after a traumatic episode; thus, prompt evaluation and appropriate treatment are necessary to ensure the best clinical outcome. To appropriately address this challenging scenario, the treating surgeon must answer several questions. We performed a systematic review of the available evidence to better understand (1) when a rotator cuff tear should be suspected after a dislocation, (2) whether nonoperative or operative treatment is more likely to restore a painless, functional shoulder, and (3) whether intraarticular lesions, rotator cuff tears, or both should be addressed when surgery is performed.
There are several limitations to our review. First, the included studies were all Level III or IV, which tend to suffer from an important component of selection bias, as surgeons may modify treatments based on patient factors or personal experience. It is difficult to draw definitive conclusions and offer concrete indications based on findings from studies of this sort alone. Additionally, the studies had relatively small sample sizes, thus limiting the statistical power. Prospective studies with larger sample sizes, ideally randomized studies further evaluating whether surgery should be performed or which surgical approach should be taken, would allow for higher-evidence-based recommendations. Further, there was a relatively large range of patient demographics, indications, treatment types, and outcomes tools utilized, which all represent sources of potential confounding. The method for diagnosing the rotator cuff tear was not standardized, which may also confound the results. Although general trends may be suggested from the outcomes of this review, it is difficult to establish definitive guidelines without a homogeneous patient population and randomization of treatment options.
Our results may help the treating surgeon understand when to evaluate the rotator cuff after a dislocation. Our findings suggest that persistent pain and weakness 2 to 3 weeks after an anterior dislocation should prompt further evaluation of the rotator cuff. Advanced imaging such as ultrasonography or MRI may be indicated to better evaluate the rotator cuff. The persistent dysfunction was often mistakenly attributed to presumed nerve palsy, resulting in delayed diagnosis of the cuff tear. Both lesions may be present after dislocation in the older patient, which Groh and Rockwood [9] described as the “terrible triad of the shoulder”. Pevny et al. [29] suggested that a rotator cuff tear should be suspected in all patients with a nerve palsy after dislocation.
Once the diagnosis of a combined instability and rotator cuff lesion is made, treatment options must be considered. Four studies in this review [10, 29, 37, 38] showed better results and improved outcomes after surgery, including better pain relief, increased function, decreased recurrence, and higher patient satisfaction. However, the decision for an individual patient to undergo surgery must be weighed against the risks of an operation. In certain patients with a balanced cuff lesion and minimal pain and without recurrent instability, nonoperative management may be considered [31]. However, in patients with persistent pain, dysfunction, and/or recurrent dislocations, surgery may improve function and result in less pain. Similarly, Bassett and Cofield [4] reported improved results with surgical repair after acute dislocations. In acute rotator cuff tears, Lahteenmaki et al. [19] reported better outcomes after early surgery compared to nonoperative management or delayed repair. Loew et al. [24] highlighted the importance of addressing rotator cuff tears after dislocations in older patients to prevent the development of persistent symptoms and secondary degenerative changes.
At the time of surgery, there often are several kinds of pathology present, and the surgeon must decide whether capsulolabral repair, rotator cuff repair, or both should be performed in patients with a rotator cuff tear after a shoulder dislocation. Before selecting a surgical treatment option, the surgeon must assess the patient’s age, functional status, time since first dislocation, capsular status, and degree of bone loss. In the majority of patients in the included studies, stability was restored and outcomes were improved with rotator cuff repair. Theoretically, restoring the concavity compression of the rotator cuff and repairing the damaged structures involved in the posterior mechanism of instability should improve outcomes. Similar to the younger population, a proportion of patients older than 40 years may have anterior capsulolabral detachment as a cause of the shoulder dislocation [1]. Thus, the anterior mechanism must also be appropriately recognized and addressed. In these cases, the rotator cuff tear may be the result of instability rather than the cause [30, 32]. Anterior stabilization and a rotator cuff repair improved outcomes in patients in whom both a capsulolabral lesion and cuff tear were present [8, 11, 32, 42]. These findings suggest that the torn rotator cuff should be repaired, and a capsulolabral lesion should be corrected where present. Although stronger evidence would be beneficial in definitively guiding treatment, this recommendation mirrors the conclusions of studies previously reported. Hawkins et al. [11] suggested combined repair of the rotator cuff tear and capsuloligamentous complex in patients younger than 40 years. Voigt and Lill [41] similarly proposed combined capsular ligament reconstruction and rotator cuff repair in patients younger than 60 years. In patients older than 60 years or with low functional demands, rotator cuff repair alone may restore stability. In a study by Goldberg et al. [8], a combined two-stage surgical approach in young elite rugby players restored stability and improved outcomes. Porcellini et al. [31, 32] utilized a combined arthroscopic anterior stabilization and rotator cuff repair to address coexisting lesions after a dislocation. In that study, the authors suggested that, whether arthroscopic or open procedures may be appropriate, the treatment for instability should guide the surgical choice.
In conclusion, the tendons of the rotator cuff play both active and passive roles in preventing glenohumeral instability. A single dislocation event can disrupt an already-weakened rotator cuff, which may be damaged from repetitive microtrauma in younger athletes or from degeneration in the elderly. A rotator cuff lesion after a dislocation must be promptly diagnosed and appropriately addressed to prevent recurrent instability and detrimental outcomes. In cases of persistent pain, loss of function, or a nerve injury after a dislocation, evaluation of the rotator cuff is warranted. If a symptomatic lesion is diagnosed, the treating surgeon should consider operative repair. Should the patient undergo surgery, addressing the rotator cuff tear and capsulolabral lesion, when present, may restore stability and improve outcomes. Further investigation, including randomized trials, should be directed toward better defining surgical indications and repair techniques for patients with a rotator cuff tear and shoulder instability.
Acknowledgments
The authors thank Tom Cichonski for his manuscript editing and technical assistance.
Footnotes
Each author certifies that he, or a member of his immediate family, has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
References
- 1.Araghi A, Prasarn M, St Clair S, Zuckerman JD. Recurrent anterior glenohumeral instability with onset after forty years of age: the role of the anterior mechanism. Bull Hosp Jt Dis. 2005;62:99–101. [PubMed] [Google Scholar]
- 2.Bahk M, Keyurapan E, Tasaki A, Sauers EL, McFarland EG. Laxity testing of the shoulder: a review. Am J Sports Med. 2007;35:131–144. doi: 10.1177/0363546506294570. [DOI] [PubMed] [Google Scholar]
- 3.Banerjee M, Bouillon B, Helm P, Akoto R, Balke M, Shafizadeh S. Recurrent anterior shoulder dislocation due to a partial-thickness articular surface supraspinatus tendon tear without capsulolabral lesion. J Shoulder Elbow Surg. 2012;21:e6–e9. doi: 10.1016/j.jse.2012.06.016. [DOI] [PubMed] [Google Scholar]
- 4.Bassett RW, Cofield RH. Acute tears of the rotator cuff: the timing of surgical repair. Clin Orthop Relat Res. 1983;175:18–24. [PubMed] [Google Scholar]
- 5.Berbig R, Weishaupt D, Prim J, Shahin O. Primary anterior shoulder dislocation and rotator cuff tears. J Shoulder Elbow Surg. 1999;8:220–225. doi: 10.1016/S1058-2746(99)90132-5. [DOI] [PubMed] [Google Scholar]
- 6.Bigliani LU, Kelkar R, Flatow EL, Pollock RG, Mow VC. Glenohumeral stability: biomechanical properties of passive and active stabilizers. Clin Orthop Relat Res. 1996;330:13–30. doi: 10.1097/00003086-199609000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Craig EV. The posterior mechanism of acute anterior shoulder dislocations. Clin Orthop Relat Res. 1984;190:212–216. [PubMed] [Google Scholar]
- 8.Goldberg JA, Chan KY, Best JP, Bruce WJ, Walsh W, Parry W. Surgical management of large rotator cuff tears combined with instability in elite rugby football players. Br J Sports Med. 2003;37:179–181; discussion 181. [DOI] [PMC free article] [PubMed]
- 9.Groh GI, Rockwood CA., Jr The terrible triad: anterior dislocation of the shoulder associated with rupture of the rotator cuff and injury to the brachial plexus. J Shoulder Elbow Surg. 1995;4:51–53. doi: 10.1016/S1058-2746(10)80008-4. [DOI] [PubMed] [Google Scholar]
- 10.Hawkins RJ, Bell RH, Hawkins RH, Koppert GJ. Anterior dislocation of the shoulder in the older patient. Clin Orthop Relat Res. 1986;206:192–195. [PubMed] [Google Scholar]
- 11.Hawkins RJ, Morin WD, Bonutti PM. Surgical treatment of full-thickness rotator cuff tears in patients 40 years of age or younger. J Shoulder Elbow Surg. 1999;8:259–265. doi: 10.1016/S1058-2746(99)90139-8. [DOI] [PubMed] [Google Scholar]
- 12.Hovelius L, Augustini BG, Fredin H, Johansson O, Norlin R, Thorling J. Primary anterior dislocation of the shoulder in young patients: a ten-year prospective study. J Bone Joint Surg Am. 1996;78:1677–1684. doi: 10.2106/00004623-199611000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Hovelius L, Eriksson K, Fredin H, Hagberg G, Hussenius A, Lind B, Thorling J, Weckstrom J. Recurrences after initial dislocation of the shoulder: results of a prospective study of treatment. J Bone Joint Surg Am. 1983;65:343–349. [PubMed] [Google Scholar]
- 14.Hovelius L, Lind B, Thorling J. Primary dislocation of the shoulder: factors affecting the two-year prognosis. Clin Orthop Relat Res. 1983;176:181–185. [PubMed] [Google Scholar]
- 15.Howell SM, Galinat BJ, Renzi AJ, Marone PJ. Normal and abnormal mechanics of the glenohumeral joint in the horizontal plane. J Bone Joint Surg Am. 1988;70:227–232. [PubMed] [Google Scholar]
- 16.Howell SM, Kraft TA. The role of the supraspinatus and infraspinatus muscles in glenohumeral kinematics of anterior should instability. Clin Orthop Relat Res. 1991;263:128–134. [PubMed] [Google Scholar]
- 17.Imhoff AB, Ansah P, Tischer T, Reiter C, Bartl C, Hench M, Spang JT, Vogt S. Arthroscopic repair of anterior-inferior glenohumeral instability using a portal at the 5:30-o’clock position: analysis of the effects of age, fixation method, and concomitant shoulder injury on surgical outcomes. Am J Sports Med. 2010;38:1795–1803. doi: 10.1177/0363546510370199. [DOI] [PubMed] [Google Scholar]
- 18.Kelkar R, Wang VM, Flatow EL, Newton PM, Ateshian GA, Bigliani LU, Pawluk RJ, Mow VC. Glenohumeral mechanics: a study of articular geometry, contact, and kinematics. J Shoulder Elbow Surg. 2001;10:73–84. doi: 10.1067/mse.2001.111959. [DOI] [PubMed] [Google Scholar]
- 19.Lahteenmaki HE, Virolainen P, Hiltunen A, Heikkila J, Nelimarkka OI. Results of early operative treatment of rotator cuff tears with acute symptoms. J Shoulder Elbow Surg. 2006;15:148–153. doi: 10.1016/j.jse.2005.07.006. [DOI] [PubMed] [Google Scholar]
- 20.Lazarus MD, Sidles JA, Harryman DT, 2nd, Matsen FA., 3rd Effect of a chondral-labral defect on glenoid concavity and glenohumeral stability: a cadaveric model. J Bone Joint Surg Am. 1996;78:94–102. doi: 10.2106/00004623-199601000-00013. [DOI] [PubMed] [Google Scholar]
- 21.Lee SB, Kim KJ, O’Driscoll SW, Morrey BF, An KN. Dynamic glenohumeral stability provided by the rotator cuff muscles in the mid-range and end-range of motion: a study in cadavera. J Bone Joint Surg Am. 2000;82:849–857. doi: 10.2106/00004623-200006000-00012. [DOI] [PubMed] [Google Scholar]
- 22.Lippitt S, Matsen F. Mechanisms of glenohumeral joint stability. Clin Orthop Relat Res. 1993;291:20–28. [PubMed] [Google Scholar]
- 23.Lippitt SB, Vanderhooft JE, Harris SL, Sidles JA, Harryman DT, 2nd, Matsen FA., 3rd Glenohumeral stability from concavity-compression: a quantitative analysis. J Shoulder Elbow Surg. 1993;2:27–35. doi: 10.1016/S1058-2746(09)80134-1. [DOI] [PubMed] [Google Scholar]
- 24.Loew M, Thomsen M, Rickert M, Simank HG. [Injury pattern in shoulder dislocation in the elderly patient] [in German] Unfallchirurg. 2001;104:115–118. doi: 10.1007/s001130050700. [DOI] [PubMed] [Google Scholar]
- 25.Matsen FA, 3rd, Harryman DT, 2nd, Sidles JA. Mechanics of glenohumeral instability. Clin Sports Med. 1991;10:783–788. [PubMed] [Google Scholar]
- 26.McLaughlin HL. Injuries of the shoulder and arm. In: McLaughlin HL, Harrison L, editors. Trauma. Philadelphia, PA: Saunders; 1959. pp. 233–296. [Google Scholar]
- 27.Neviaser RJ, Neviaser TJ, Neviaser JS. Anterior dislocation of the shoulder and rotator cuff rupture. Clin Orthop Relat Res. 1993;291:103–106. [PubMed] [Google Scholar]
- 28.Noel E, Walch G, Tebib JG. [Recurrent anterior luxation of the shoulder occurring after 40 years of age and rupture of the rotator cuff] [in French] Rev Rhum Mal Osteoartic. 1990;57:189–191. [PubMed] [Google Scholar]
- 29.Pevny T, Hunter RE, Freeman JR. Primary traumatic anterior shoulder dislocation in patients 40 years of age and older. Arthroscopy. 1998;14:289–294. doi: 10.1016/S0749-8063(98)70145-8. [DOI] [PubMed] [Google Scholar]
- 30.Porcellini G, Caranzano F, Campi F, Paladini P. Instability and rotator cuff tear. Med Sport Sci. 2012;57:41–52. doi: 10.1159/000328876. [DOI] [PubMed] [Google Scholar]
- 31.Porcellini G, Caranzano F, Campi F, Pellegrini A, Paladini P. Glenohumeral instability and rotator cuff tear. Sports Med Arthrosc. 2011;19:395–400. doi: 10.1097/JSA.0b013e31820d583b. [DOI] [PubMed] [Google Scholar]
- 32.Porcellini G, Paladini P, Campi F, Paganelli M. Shoulder instability and related rotator cuff tears: arthroscopic findings and treatment in patients aged 40 to 60 years. Arthroscopy. 2006;22:270–276. doi: 10.1016/j.arthro.2005.12.015. [DOI] [PubMed] [Google Scholar]
- 33.Pouliart N, Gagey O. Concomitant rotator cuff and capsuloligamentous lesions of the shoulder: a cadaver study. Arthroscopy. 2006;22:728–735. doi: 10.1016/j.arthro.2006.03.015. [DOI] [PubMed] [Google Scholar]
- 34.Rodosky MW, Harner CD, Fu FH. The role of the long head of the biceps muscle and superior glenoid labrum in anterior stability of the shoulder. Am J Sports Med. 1994;22:121–130. doi: 10.1177/036354659402200119. [DOI] [PubMed] [Google Scholar]
- 35.Rowe CR. Prognosis in dislocations of the shoulder. J Bone Joint Surg Am. 1956;38:957–977. [PubMed] [Google Scholar]
- 36.Shah AS, Karadsheh MS, Sekiya JK. Failure of operative treatment for glenohumeral instability: etiology and management. Arthroscopy. 2011;27:681–694. doi: 10.1016/j.arthro.2010.11.057. [DOI] [PubMed] [Google Scholar]
- 37.Simank HG, Dauer G, Schneider S, Loew M. Incidence of rotator cuff tears in shoulder dislocations and results of therapy in older patients. Arch Orthop Trauma Surg. 2006;126:235–240. doi: 10.1007/s00402-005-0034-0. [DOI] [PubMed] [Google Scholar]
- 38.Sonnabend DH. Treatment of primary anterior shoulder dislocation in patients older than 40 years of age: conservative versus operative. Clin Orthop Relat Res. 1994;304:74–77. [PubMed] [Google Scholar]
- 39.Toolanen G, Hildingsson C, Hedlund T, Knibestol M, Oberg L. Early complications after anterior dislocation of the shoulder in patients over 40 years: an ultrasonographic and electromyographic study. Acta Orthop Scand. 1993;64:549–552. doi: 10.3109/17453679308993690. [DOI] [PubMed] [Google Scholar]
- 40.Travlos J, Goldberg I, Boome RS. Brachial plexus lesions associated with dislocated shoulders. J Bone Joint Surg Br. 1990;72:68–71. doi: 10.1302/0301-620X.72B1.2298797. [DOI] [PubMed] [Google Scholar]
- 41.Voigt C, Lill H. [Shoulder instability and rotator cuff tear] [in German] Orthopade. 2009;38:70–74. doi: 10.1007/s00132-008-1356-8. [DOI] [PubMed] [Google Scholar]
- 42.Voos JE, Pearle AD, Mattern CJ, Cordasco FA, Allen AA, Warren RF. Outcomes of combined arthroscopic rotator cuff and labral repair. Am J Sports Med. 2007;35:1174–1179. doi: 10.1177/0363546507300062. [DOI] [PubMed] [Google Scholar]