Abstract
Background
Preoperative psychologic distress is considered to be a risk factor for clinical dissatisfaction stemming from persistent pain and physical limitations after elective orthopaedic procedures such as lower-extremity arthroplasty. However, the degree to which psychologic distress, specifically in the form of anxiety and depression, influences surgical results has been poorly characterized.
Questions/purposes
We analyzed the effect of preoperative psychologic distress on changes in pain, function, and quality of life 1 year after elective TKA.
Methods
In this prospective cohort study, we assessed patients who underwent TKAs in 2009 and 2010. Before surgery, patients completed the Folstein Mini Mental Test, the Hospital Anxiety and Depression Scale (HAD), The Knee Society Score©, the WOMAC quality-of-life questionnaire, and the VAS for pain. The patients were divided into two groups based on the degree of psychologic distress on the HAD Scale, and the groups were compared in terms of the above-listed clinical outcomes tools 1 year after surgery using multivariate linear models. Two hundred sixty-three patients met the inclusion criteria, and 202 (77%) completed the study protocol.
Results
The presence of preoperative psychologic distress did not influence 1-year postoperative pain assessment (average reduction in pain, 40.33; 95% CI, 36.9–43.8; p = 0.18). The only factor influencing change in pain experienced by patients was the preoperative pain recorded (R2 = 0.31; β = −0.82; p < 0.001). The patients experiencing preoperative psychologic distress obtained poorer outcomes in function (R2 = 0.16; β = −5.62; p = 0.001) and quality of life (R2 = 0.09; β = −0.46; p < 0.001) 1 year after receiving TKA.
Conclusions
The presence of preoperative psychologic distress is associated with worse 1-year outcomes for function and quality of life in patients undergoing TKA. Interventions designed to reduce psychologic distress may be indicated for patients to undergo this type of surgery, and incorporation of these data into discussions with patients may facilitate informed and shared decision making regarding the surgical treatment of knee osteoarthritis.
Level of Evidence
Level II, therapeutic study. See the Instructions for Authors for a complete description of levels of evidence.
Introduction
Joint arthroplasty is a common procedure [28, 31] and although the majority of patients receiving a TKA report an improvement in pain and function [11, 30, 42], 15% to 30% report no improvement after surgery [3, 30, 47]. Possible causes for failure of this type of surgery include infection, instability, loosening of the prosthesis, and complex regional pain syndrome. However, psychologic diagnoses including anxiety and depression have been proposed as potential risk factors for persistent pain, functional limitations, and clinical dissatisfaction after elective orthopaedic procedures [9, 39]. Psychologic distress is a term used to describe a clinical set of psychologic symptoms including anxiety, depression, and somatization [7].
The influence of psychologic distress on results of orthopaedic surgery has been studied and some of the studies have examined the effect on patients after knee and/or hip arthroplasties [2, 9, 19, 20, 22, 34, 37–39, 44]. One study found psychologic distress to be five times more common in patients on the waiting list for surgery than in the population in general [1]. Research shows that approximately 25% of patients due to receive full primary hip or knee arthroplasties experience preoperative psychologic distress [34], which may have a negative effect on preoperative and/or postoperative pain and function. Paulsen et al. [37] identified six studies [2, 9, 19, 20, 22, 44] in which psychologic state had an influence on the outcome of this type of patient and four studies [30, 34, 36, 38] in which it did not affect them. Although this literature is not yet large, it is growing, and disagreements remain regarding the degree to which psychologic distress influences patients’ pain, function, and quality of life after elective arthroplasty. Our study was designed to establish whether preoperative psychologic distress levels can predict poor outcomes in pain, function, and quality of life for patients 12 months after knee replacement surgery and, if so, to quantify the degree of this affect in a significant clinical context.
Patients and Methods
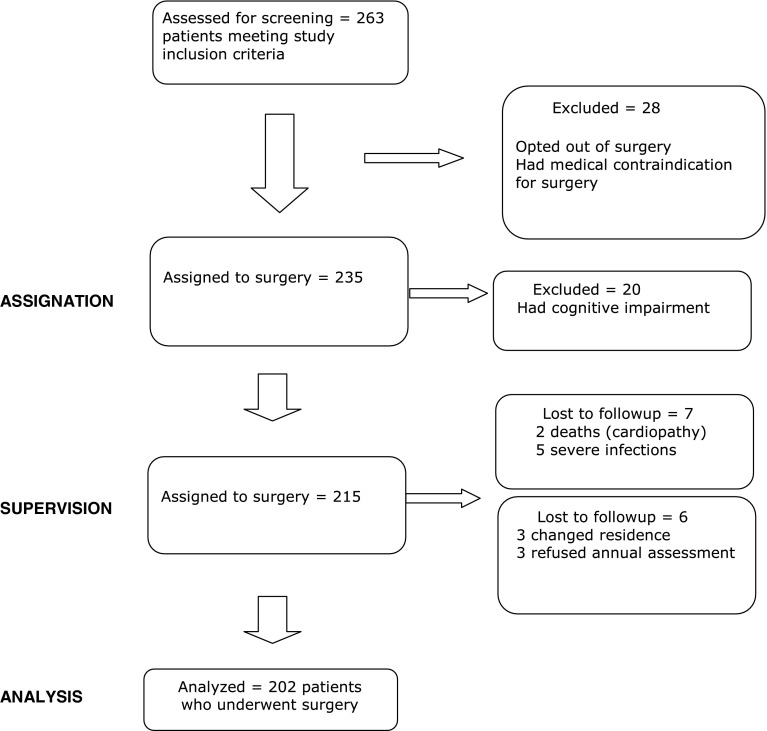
A prospective cohort study was completed of patients undergoing unilateral primary TKAs for the treatment of gonarthrosis. Patients were recruited between January and December 2009 (inclusive) and followup took place from January to December 2010 (inclusive) at the University Hospital in Guadalajara, Spain. The study was approved by the independent ethics committee at the hospital, and all patients provided agreement and consent for inclusion in the study. Two hundred sixty-three patients eligible for surgery initially were selected, and a diagnosis of osteoarthritis was made by the operating surgeon after clinical and radiographic examinations. Patients were excluded if they had a history of knee infection or if they were unable to complete the questionnaires because of cognitive or language difficulties. Two hundred thirty-five of them (89.4%) underwent surgery, and 28 (10.6%) were included in the control group because they did not want surgery or they had a medical contraindication. None refused participation at the beginning of the study. Twenty patients initially were excluded because they had dementia. Statistically significant differences between intervention and control group patients were found, resulting in the groups not being comparable. At the end of the annual evaluation two patients had died (cardiopathy), five had deep infections requiring reintervention, and six were lost to followup (three had moved and three refused annual assessment). These patients were excluded and the main analyses were performed only in the group of surgically treated patients (202 patients, 77%) (Fig. 1).
Fig. 1.
The flowchart shows the distribution of patients during the study.
With estimated postoperative success rates of 90% in the population not experiencing psychologic distress and 70% in those experiencing psychologic distress, with a power of 80%, CI of 95%, and considering the expected prevalence of psychologic distress of 25%, a sample size of 205 patients was needed for this study.
Patients with primary gonarthrosis, gonarthrosis secondary to osteonecrosis, or gonarthrosis secondary to rheumatoid arthritis based on radiographs and clinical history were eligible for inclusion. Two of the authors (AU-C, BJDT-E) obtained informed consent and patient details using a standard protocol. Patients were excluded if they had an active infection, unstable medical conditions before implant surgery, cognitive disorders (score of 26 or less in the Folstein Mini Mental Test [16]), or were non-Spanish speakers.
The two prostheses used were the standard or posterior-stabilized NexGen® total knee system (Zimmer, Warsaw, IN, USA) and the standard or posterior-stabilized Genesis II® prosthesis (Smith & Nephew, Memphis, TN, USA). No patients had a contralateral TKA within 12 months of the first procedure during the course of the study.
Sociodemographic details, height, weight, affected side, Sangha comorbidity scale [41], diagnosis, Folstein Mini Mental Test [16], Hospital Anxiety and Depression (HAD) Scale [49], The Knee Society Score© (KSS©) [27], the WOMAC quality-of-life scale [4–6], and the VAS for pain [45] were collected for all patients in the days before surgery. After the procedure, appointments were made for assessment 1 year after surgery.
The HAD [49] is a questionnaire commonly used [8, 21, 25, 39] to diagnose anxiety and/or depression in patients hospitalized in departments other than psychiatric, and it is particularly useful for somatic dysfunction, which may be biased by the symptoms of the physical condition experienced by the patient as may occur, for example, with the effect of fatigue and depression on the Beck Depression Inventory [8]. The HAD consists of 14 items, none of which make any reference to somatic symptoms, and are grouped into two subscales, one for anxiety and the other for depression. The patient must answer each item using a Likert-type scale, which sometimes refers to the intensity of symptoms and at other times to the frequency of their occurrence. The scale ranges from 0 (never, no intensity) to 3 (almost all day, very intense). The timing reference of this scale is the week before surgery. For each subscale, a score is obtained by adding that given to each of the items on the questionnaire. For both subscales, the resulting score is interpreted in line with the following criteria: 0 to 7, normal range; 8 to 10, probable case; and 11 to 21, case of anxiety or depression, therefore its use in our study to observe the existence of psychologic distress [24], as advised by Paulsen et al. [37].
The study population was divided into two retrospective cohorts—no distress and distressed, and all subsequent analyses compared the two cohorts based on pain, function, and quality of life. Initially a descriptive study was completed and it was checked using appropriate bivariate tests, whether demographic factors (age and gender), clinical factors (diagnosis, affected side, BMI, and comorbidity), or variables relating to the surgery (type of prosthesis, type of patient per the KSS©, and complications), were different in the two groups with and without psychologic distress. BMI data were used, classified as normal weight (BMI ≤ 25 kg/m2), overweight (26 < BMI < 30 kg/m2), obese (31 < BMI < 35 kg/m2), severely obese (35 < BMI < 39 kg/m2), and morbidly obese (BMI ≥ 40 kg/m2) as classified by the WHO [46].
The mean age of the group of patients undergoing surgery (202 patients) was 73 years (SD, 6.35 years). The gender distribution showed a predominance of females with 140 (69.3%). The results were similar in terms of the affected side with 104 right knees (51.5%) involved. The diagnosis was gonarthrosis in 194 patients (96%), osteonecrosis in six patients (3%), and rheumatoid arthritis in two patients (1%). The mean height of the patients was 161.28 cm (SD, 7.13 cm), and their mean weight was 78.26 kg (SD, 13.08 kg), resulting in an average BMI of 20.08 kg/m2 with a typical deviation of 4.60 kg/m2, according to the WHO BMI scale [46].
One hundred fifty-one patients (74.75%) had a comorbidity, with high blood pressure (39.1%; n = 59) being the most common. The Nexgen® prosthesis was used in 155 patients (76.7%) compared with the Genesis II® in 47 patients. One hundred fifty-seven (77.7%) posterior-stabilized prostheses and 45 (22.3%) prostheses that preserved the posterior cruciate ligament were placed. The mean hospitalization was 8.56 days (SD, 5.1 days), and the mean time to annual assessment was 371.9 days (SD, 24.7 days).
Pain
To assess pain, the KSS© was used [27], although it is not yet validated [20]. The KSS© is specific to the joint being assessed, meaning that it only reflects changes in the knee condition and not any comorbidity. The VAS for pain also assesses patient satisfaction [45]. The outcomes from the KSS© and VAS scales were assessed 1 year after surgery for patients in the distressed and nondistressed groups and compared with their preoperative figures.
Function
For function, the KSS© also was used [27]. The data obtained from the KSS© scale preoperatively and 1 year after surgery initially were used continuously and then categorized. The outcomes were classified as excellent (between 100 and 85 points), good (84-70 points), acceptable (69-60 points), and poor (less than 60 points).
Quality of Life
The assessment of patient quality of life was completed using the WOMAC questionnaire before surgery and 1 year after surgery [4–6, 14], specifically for hip and/or knee arthritis. It also was used to assess function in patients with a TKA [20, 29, 32, 34, 39]. As with the KSS©, the WOMAC is specific to the joint being assessed and does not assess any comorbidity. In addition, the data obtained from the WOMAC scales initially were used continuously and then categorized. The outcomes were classified as excellent (less than 70 points), good (70-79 points), acceptable (80-89 points), and poor (between 90 and 96 points), as higher scores on the WOMAC indicate worse pain, stiffness, and functional limitations.
Statistical Analysis
An analysis was completed using a multivariate linear regression model to assess whether the difference between the data obtained before surgery and after 1 year depended on preoperative psychologic distress, also considering the influence of variables (gender, age, type of patient as per the KSS©, comorbidity, BMI, and diagnosis), which, according to univariate analyses, or at the discretion of the investigator, may have had clinical meaning. Statistical analyses were done using Version 19 of the SPSS software (SPSS Inc, Chicago, IL, USA).
Results
All the scales examined (KSS© pain, KSS© function, WOMAC, and VAS) showed improved scores during the course of the study (Table 1). Psychologic distress also decreased at the annual assessment of the group of patients from 34.16% presurgery (n = 69) to 7.9% after surgery (n = 16). Analyzing preoperative distress such as the presence of anxiety and/or depression based on the cut-off point indicated by Zigmong and Snaith [49], the following results were obtained: 65.84% of patients (n = 133) did not have preoperative distress compared with 34.16% (n = 69) who did (Table 2). We analyzed whether preoperative and postoperative difference scales depended on anxiety, depression, or preoperative distress through a multivariate linear regression model.
Table 1.
Baseline data and comparison of difference between outcomes
| Dependent variables | No distress (n = 133) | Distress (n = 69) | Difference between groups | ||||
|---|---|---|---|---|---|---|---|
| KSS©, WOMAC, AND VAS | Baseline | Difference after 1 year | Baseline | Difference after 1 year | p value | ||
| Mean | 95% CI | Mean | 95% CI | ||||
| KSS© (pain) | 37.74 | 42.45 | (40.2–44.7) | 35.78 | 40.33 | (36.9–43.8) | 0.182 |
| VAS | 8.67 | −6.89 | (−7.1 to −6.7) | 8.60 | −6.72 | (−7.2 to −6.3) | 0.886 |
| KSS© (function) | 38.79 | 47.96 | (45.9–50.0) | 38.43 | 42.13 | (39.0–45.2) | 0.002 |
| WOMAC | 60.84 | −41.56 | (−42.6 to −40.5) | 60.55 | −39.48 | (−41.2 to −37.7) | 0.042 |
KSS = The Knee Society Score©.
Table 2.
Comparison of initial variables
| Initial variables | Not distressed (n = 133) | Distressed (n = 69) | p value | ||
|---|---|---|---|---|---|
| Number | Percent | Number | Percent | ||
| Age (mean SD) | 72 | 6.44 | 74 | 6.23 | 0.04 |
| Females | 87 | 65.4 | 53 | 76.8 | 0.07* |
| Right side affected | 64 | 48.1 | 40 | 58 | 0.12 |
| Diagnosis | |||||
| Gonarthrosis | 130 | 97.7 | 64 | 92.8 | 0.1* |
| IFC necrosis | 3 | 2.3 | 3 | 4.3 | |
| Rheumatoid arthritis | 0 | 0 | 2 | 2.9 | |
| Nexgen® total knee system | 99 | 74.4 | 56 | 81.2 | 0.19 |
| Comorbidity | 63 | 47.4 | 30 | 43.5 | 0.35 |
| Complications | 124 | 93.2 | 65 | 95.2 | 0.53 |
| BMI | |||||
| Normal | 16 | 12 | 11 | 15.9 | 0.55 |
| Overweight | 54 | 40.6 | 27 | 39.1 | |
| Obesity | 43 | 32.3 | 20 | 29 | |
| Severe obesity | 16 | 12 | 6 | 8.7 | |
| Morbid obesity | 4 | 3 | 5 | 7.2 | |
| KSS© (pain) postoperatively | |||||
| Excellent | 39 | 29.3 | 17 | 24.6 | 0.65 |
| Good | 71 | 53.4 | 35 | 50.7 | |
| Acceptable | 16 | 12 | 12 | 17.4 | |
| Poor | 7 | 5.3 | 5 | 7.2 | |
| KSS© (function) postoperatively | |||||
| Excellent | 70 | 52.6 | 29 | 42 | 0.5 |
| Good | 53 | 39.8 | 32 | 46.4 | |
| Acceptable | 6 | 4.5 | 5 | 7.2 | |
| Poor | 4 | 3 | 3 | 4.3 | |
| WOMAC postoperatively | |||||
| Excellent | 16 | 12 | 2 | 2.9 | 0.14 |
| Good | 103 | 77.4 | 56 | 81.2 | |
| Acceptable | 11 | 8.3 | 8 | 11.6 | |
| Poor | 3 | 2.3 | 3 | 4.3 | |
| VAS postoperatively | |||||
| 0 | 5 | 3.8 | 5 | 7.2 | 0.23 |
| 1 | 62 | 46.6 | 26 | 37.7 | |
| 2 | 44 | 33.1 | 24 | 34.8 | |
| 3 | 14 | 10.5 | 7 | 10.1 | |
| 4 | 7 | 5.3 | 2 | 2.9 | |
| 5 | 0 | 0 | 2 | 2.9 | |
| 6 | 0 | 0 | 1 | 1.4 | |
| 8 | 0 | 0 | 1 | 1.4 | |
| 9 | 1 | 0.8 | 1 | 1.4 | |
* Statistically significant association was observed between anxiety and gender (female) (p < 0.02) and between diagnosis of internal femoral condyle (IFC) necrosis and depression (p < 0.001); KSS© = The Knee Society Score©.
Pain
Postoperative outcome of the KSS© pain subscale depended only on the preoperative KSS© pain score (R2 = 0.313; β = −0.824; p < 0.001). Previous pain had an effect on the change observed in patients (41.72; 95% CI, 39.86–43.59). In the case of previous pain on the VAS, we found no factor influencing the outcomes. The change observed on the VAS (−6.83; 95% CI, −7.04 to −6.64) did not depend on any of the preoperative factors under study.
Function
The changes observed with the KSS© function subscale (R2 = 0.160) depended on preoperative scores (β = 0.46; p < 0.001); age (β = −0.27; p = 0.004); diagnosis which increased with the presence of a larger number of concomitant conditions (β = 3.08; p < 0.01); comorbidities (β = −2.85; p = 0.009); BMI (β = −0.09; p = 0.009); and preoperative distress (β = −5.621; p < 0.001). The greater the level of preoperative distress, the poorer the outcome on the KSS© function subscale test. In the first analysis of this analytical model, the presence of distress nullified the possible influence of anxiety and/or depression. During subsequent separate analysis, we observed that the influence of preoperative psychologic distress on the change in the KSS© function subscale was attributable to preoperative depression and not anxiety. Beta factor represents the influence of the predictor variable on the dependent variable, and its negative value indicates that as one increases, the other decreases. By linking preoperative psychologic distress with the KSS© function subscale, we observed that it had a substantial influence on it (very high beta coefficient), and that greater psychologic distress in the patients in the preoperative evaluation resulted in a lower difference in the final result and therefore less improvement (Table 3).
Table 3.
Linear regression with statistically significant values
| Dependent variables | Predictor variables | Beta coefficient | p value |
|---|---|---|---|
| Difference in KSS© pain | Preoperative KSS© pain | −0.834 | 0.001 |
| Difference in KSS© function | Preoperative KSS© function | −0.461 | 0.001 |
| Comorbidity | −2.567 | 0.009 | |
| Psychologic distress | −6.184 | 0.001 | |
| Diagnostic | 7.866 | 0.012 | |
| Age | −0.396 | 0.004 | |
| BMI | −2.020 | 0.018 | |
| Difference in WOMAC | Preoperative WOMAC | 0.536 | 0.001 |
| Psychologic distress | −2.024 | 0.028 |
KSS = The Knee Society©.
Quality of Life
The change observed on the WOMAC scale fundamentally depended on the preoperative WOMAC test score (R2 = 0.09; β = −0.46; p < 0.001) and preoperative distress score (β = −0.08; p < 0.001). Patients with preoperative psychologic distress had worse quality of life at 1 year. The greater the degree of preoperative distress, the higher the WOMAC score, and the worse the quality of life for the patient (Tables 1 and 3).
Discussion
From the results of our study, the changes in the KSS© pain subscale and VAS were not influenced by preoperative psychologic distress, however, the changes observed in the KSS© function subscale were influenced by preoperative psychologic distress (the greater the level of preoperative distress, the poorer the outcome in the KSS© function subscale test). The influence of preoperative psychologic distress on the change in the KSS© function subscale was attributable to preoperative depression and not anxiety. Finally, the change observed in the WOMAC scale fundamentally depended on the preoperative distress score: the greater the degree of preoperative distress, the higher the WOMAC score, and the worse the quality of life for the patient.
Limitations of this study include that it involved just one hospital, which reduces the possibility of generalizing results for any other country, and as all the patients assessed were white, the results cannot be generalized for patients of other ethnic origins. However, there was a low rate of withdrawal and exclusion of patients, and the bias attributable to cognitive impairment was removed. The HAD questionnaire is specifically targeted at the diagnosis of psychologic distress, and the WOMAC and KSS© at the joint studied. The diagnoses were knee osteoarthritis in 219 patients (96.5%), necrosis of the medial femoral condyle in six patients (2.6%), and rheumatoid arthritis in two patients (0.9%). Fifteen patients (9.9 %) had a valgus tibial osteotomy before the current rating, and 2.6% (n = 4) of the patients had Parkinson’s disease. There were no other musculoskeletal comorbidities or another factors such as a previous cerebrovascular accident, multiple sclerosis, or multiple trauma with long-term compromise of locomotion that would have compromised the functional status of the patients. One hundred ninety of the patients (94%) included in this study were in Category A of the KSS© (unilateral or bilateral, opposite knee successfully replaced), nine patients (4.5%) were in Category B (unilateral, other knee symptomatic), and three patients (1.5%) were in Category C (multiple arthritis or medical infirmity), so there was no significant influence of other joints in the evaluation of the surgically treated knee. Thirteen patients (8.6%) had been diagnosed, managed, and treated for depression by Psychiatry and/or Primary Care physicians. No other psychiatric conditions were evident in the patients. Although some authors [9] excluded patients receiving treatment with antidepressants or antianxiety drugs, we did not exclude these patients because they were considered to be in a stable psychologic state because of their treatment and because the relationship between preoperative psychologic complaints and postoperative function disorders would be strengthened if they were included [38]. Although a previous study [50] showed the unfavorable effect of preoperative and longstanding opioids on postoperative pain scores, the number of patients who were known to take preoperative opioids, either in a medicinal or recreational manner, was not analyzed in our study. Psychologic distress in our patients decreased from 34.16% (n = 69 patients) preoperatively to 7.9% (n = 16 patients) postoperatively. All of these patients were included in the group with psychologic distress before surgery.
The scores obtained with the HAD pointed to a diagnosis of psychologic distress as a state rather than a feature, as the patients were consulted regarding their symptoms during the 2 weeks before surgery or at the yearly assessment. Although these states may be influenced by other factors such as mourning or a previous psychologic condition, all patients were receiving treatment for any existing conditions (ongoing depression or anxiety), and questions dealing with somatic disorders were excluded. Therefore, the cause of psychologic distress in these patients was a chronic condition rather than a recent or passing event. The HAD has been used on a variable scale, proving to be a highly significant predictor of postoperative function 1 year after surgery. Its ability to provide information regarding the nature of psychologic distress is less limited than the ability of other scales and the assessment of depression, anxiety, and psychologic distress on the HAD questionnaire reduces the need to use several different formats [23, 36, 37]. The severity of preoperative pain was correlated with the severity of physical and radiographic findings as the items included in the categories of pain, ROM, stability, flexion contracture, and radiographic alignment are summed to obtain the KSS© pain subscale. The postoperative result of the KSS© pain subscale depends only on the preoperative KSS© pain subscale. Previous pain has substantial influence on the observed change in patients. No statistically significant connection was found between preoperative KSS© pain and postoperative KSS© function, unlike in other studies [12, 33, 43] in which a correlation was observed between the KSS© preoperative pain subscale and KSS© function subscale 1 year after surgery. Patients with psychologic distress did not have more pain, lesser function, or poorer quality of life before surgery than those without psychologic distress. The approach of dichotomizing the HAD scale made it possible to judge the influence of psychologic distress on the clinical affect, assessed using the KSS©, WOMAC, and VAS, and the sensitivity of the analyses proved these estimations to be reasonably reliable. It is necessary to distinguish between change (representing improvements in condition) and outcome (representing the final state) and, after analysis, the latter seems clinically more important, as change and outcome are conceptually different phenomena, as indicated by Lingard and Riddle [34]. Changes in scores seem to be affected more by preoperative psychologic distress than end scores, as there are statistically significant differences in the changes found in the scores for the distressed and nondistressed groups, and not in the final scores. No connection was established between preoperative psychologic distress and postoperative pain.
Twelve percent of the patients included in this study had postoperative pain, a percentage which falls in the reported 6% to 30% range [15, 47, 48]. Although Forsythe et al. [17] did not find any relationship between preoperative and postoperative pain, Lingard et al. [33] pointed to preoperative pain as a cause of this postsurgical pain. We concur with Lingard et al. [33], as we found a statistically significant relationship between preoperative KSS© pain and postoperative KSS© pain scores. Severe preoperative pain was a predictive factor for a poorer clinical outcome (pain) 1 year after TKA. The VAS showed a statistically significant improvement [10], although no connection was found with psychologic distress. The considerable changes found in improved pain as measured using the KSS© and VAS scales may be the reason that psychologic distress does not seem to influence this difference, and a larger sample group would have been required to show this point. The results of the KSS© pain subscale and VAS were not influenced by preoperative psychologic distress.
Some authors reported that a poorer preoperative function level is one of the causes influencing poorer postoperative function outcomes [18, 26, 33, 40], as was seen in our results. Some authors also found a statistically significant connection between psychologic distress and postoperative function outcomes [19, 34, 44], although others [36, 38] reported that there is no relationship between preoperative mental health and postoperative function outcome. As in other studies, comorbidity and preoperative BMI had a negative influence on function outcomes [19]. Age also is an influencing factor on the KSS© function subscale [15, 19, 43]. This may be attributable to the progressive loss of muscular strength, coordination, and activity levels as people grow older. Because the changes for function were not as great as the changes for pain, an influence of preoperative psychologic distress on the change 1 year after surgery could be observed.
We found only two studies [9, 38] that used specific questionnaires to assess preoperative psychologic distress and function outcomes and, although the WOMAC questionnaire can have limitations such as the ceiling or floor effect, we observed that psychologic distress had a negative effect on patients in terms of function and quality of life alone, and not in terms of their perceived pain levels. The result of the WOMAC primarily depends on the test score from the preoperative WOMAC and on preoperative psychologic distress, but does not depend on preoperative pain. Patients had a worse quality of life if they experienced higher preoperative distress and higher WOMAC score.
The only predictive factor for postoperative pain was preoperative pain, and patients in this study with preoperative psychologic distress obtained poorer outcomes for function and quality of life 1 year after surgery compared with patients without psychologic distress. The mental health of the patients with psychologic distress improved, which suggests that it is a reversible condition [34], and that it may be related to the surgical procedure. For this reason, interventions designed to reduce psychologic distress may be indicated for patients scheduled to undergo surgery, as mentioned by other authors [13, 35, 37]. This information could be beneficial to surgeons and patients when considering surgery in the current climate of financial austerity. The results of our study are consistent with the economic need to define the patients for whom arthroplasty is most likely to achieve a valid functional improvement. Incorporation of these data in discussions with patients may facilitate informed, shared decision making regarding surgical treatment of knee osteoarthritis, because it seems unwise to ignore these effects and their influence on the final results. Further investigation on a larger scale is warranted to assess the magnitude of the effect of psychologic distress and other factors on pain and function in surgical patients.
Acknowledgments
We thank the staff members of the Orthopaedics Department of Guadalajara University Hospital and Alcala University (Madrid, Spain) for participating in this project.
Footnotes
Each author certifies that he or she, or a member of his or her immediate family, has no funding or commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Guadalajara University Hospital, Guadalajara, Spain.
References
- 1.Ackerman IN, Graves SE, Wicks IP, Bennell KL, Osborne RH. Severely compromised quality of life in women and those of lower socioeconomic status waiting for joint replacement surgery. Arthritis Rheum. 2005;53:653–658. doi: 10.1002/art.21439. [DOI] [PubMed] [Google Scholar]
- 2.Ayers DC, Franklin PD, Ploutz-Snyder R, Boisvert CB. Total knee replacement outcome and coexisting physical and emotional illness. Clin Orthop Relat Res. 2005;440:157–161. doi: 10.1097/01.blo.0000185447.43622.93. [DOI] [PubMed] [Google Scholar]
- 3.Ayers DC, Franklin PD, Trief PM, Ploutz-Snyder R, Freund D. Psychological attributes of preoperative total joint replacement patients: implications for optimal physical outcome. J Arthroplasty. 2004;19(7 suppl 2):125–130. doi: 10.1016/j.arth.2004.06.019. [DOI] [PubMed] [Google Scholar]
- 4.Bellamy N. WOMAC Osteoarthritis Index: A User’s Guide. London, Canada: Victoria Hospital; 1995. [Google Scholar]
- 5.Bellamy N. The WOMAC Knee and Hip Osteoarthritis Indices: development, validation, globalization and influence on the development of the AUSCAN Hand Osteoarthritis Indices. Clin Exp Rheumatol. 2005;23(5 suppl 39):S148–S153. [PubMed] [Google Scholar]
- 6.Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 7.BenDebba M, Torgerson WS, Long DM. Personality traits, pain duration and severity, functional impairment and psychological distress in patients with persistent low back pain. Pain. 1997;72:115–125. doi: 10.1016/S0304-3959(97)00020-1. [DOI] [PubMed] [Google Scholar]
- 8.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the Hospital Anxiety and Depression Scale: an updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/S0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 9.Brander V, Gondek S, Martin E, Stulberg SD. Pain and depression influence outcome 5 years after knee replacement surgery. Clin Orthop Relat Res. 2007;464:21–26. doi: 10.1097/BLO.0b013e318126c032. [DOI] [PubMed] [Google Scholar]
- 10.Brokelman RB, Van Loon CJ, Rijnberg WJ. Patient versus surgeon satisfaction after total hip arthroplasty. J Bone Joint Surg Br. 2003;85:495–498. [PubMed] [Google Scholar]
- 11.Callahan CM, Drake BG, Heck DA, Dittus RS. Patient outcomes following tricompartmental total knee replacement: a meta-analysis. JAMA. 1994;271:1349–1357. doi: 10.1001/jama.1994.03510410061034. [DOI] [PubMed] [Google Scholar]
- 12.Caracciolo B, Giaquinto S. Self-perceived distress and self-perceived functional recovery after recent total hip and knee arthroplasty. Arch Gerontol Geriatr. 2005;41:177–181. doi: 10.1016/j.archger.2005.01.006. [DOI] [PubMed] [Google Scholar]
- 13.Damush TM, Weinberger M, Perkins SM, Rao JK, Tierney WM, Qi R, Clark DO. Randomized trial of a self-management program for primary care patients with acute low back pain: short-term effects. Arthritis Rheum. 2003;49:179–186. doi: 10.1002/art.10995. [DOI] [PubMed] [Google Scholar]
- 14.Davis ET, Lingard EA, Schemitsch EH, Waddell JP. Effects of socioeconomic status on patients’ outcome after total knee arthroplasty. Int J Qual Health Care. 2008;20:40–46. doi: 10.1093/intqhc/mzm059. [DOI] [PubMed] [Google Scholar]
- 15.Elson D, Brenkel I. Predicting pain after total knee arthroplasty. J Arthroplasty. 2006;21:1047–1053. doi: 10.1016/j.arth.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 16.Folstein MF, Folstein SE, McHugh PR. Minimental state: a practical guide for cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 17.Forsythe ME, Dunbar MJ, Hennigar AW, Sullivan MJ, Gross M. Prospective relation between catastrophic and residual pain following knee arthroplasty: two-year follow-up. Pain Res Manag. 2008;13:335–341. doi: 10.1155/2008/730951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fortin PR, Clarke AE, Joseph L, Liang MH, Tanzer M, Ferland D, Phillips C, Partridge AJ, Belisle P, Fossel AH, Mahomed N, Sledge CB, Katz JN. Outcomes of total hip and knee replacement: preoperative functional status predicts outcomes at six months after surgery. Arthritis Rheum. 1999;42:1722–1728. doi: 10.1002/1529-0131(199908)42:8<1722::AID-ANR22>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 19.Franklin PD, Li W, Ayers DC. The Chitranjan Ranawat Award: functional outcome after total knee replacement varies with patient attributes. Clin Orthop Relat Res. 2008;466:2597–2604. doi: 10.1007/s11999-008-0428-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gandhi R, Dhotar H, Razak F, Tso P, Davey JR, Mahomed NN. Predicting the longer term outcomes of total knee arthroplasty. Knee. 2010;17:15–18. doi: 10.1016/j.knee.2009.06.003. [DOI] [PubMed] [Google Scholar]
- 21.Härter M, Reuter K, Gross-Hardt K, Bengel J. Screening for anxiety, depressive and somatoform disorders in rehabilitation: validity of HADS and GHQ - 12 in patients with musculoskeletal disease. Disabil Rehabil. 2001;23:737–744. doi: 10.1080/09638280110062176. [DOI] [PubMed] [Google Scholar]
- 22.Heck DA, Robinson RL, Partridge CM, Lubitz RM, Freund DA. Patient outcomes after knee replacement. Clin Orthop Relat Res. 1998;356:93–110. doi: 10.1097/00003086-199811000-00015. [DOI] [PubMed] [Google Scholar]
- 23.Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol. 2005;44:227–239. doi: 10.1348/014466505X29657. [DOI] [PubMed] [Google Scholar]
- 24.Herrero MJ, Blanch J, Peri JM, De-Pablo J, Pintora L, Bulbena A. A validation study of the hospital anxiety and depression scale (HADS) in a Spanish population. General Hospital Psychiatry. 2003;25:277–283. doi: 10.1016/S0163-8343(03)00043-4. [DOI] [PubMed] [Google Scholar]
- 25.Herrmann C. International experiences with the Hospital Anxiety and Depression Scale: a review of validation data and clinical results. J Psychosom Res. 1997;42:17–41. doi: 10.1016/S0022-3999(96)00216-4. [DOI] [PubMed] [Google Scholar]
- 26.Holtzman J, Saleh K, Kane R. Effect of baseline functional status and pain on outcomes of total hip arthroplasty. J Bone Joint Surg Am. 2002;84:1942–1948. doi: 10.2106/00004623-200211000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the Knee Society clinical rating system. Clin Orthop Relat Res. 1989;248:13–14. [PubMed] [Google Scholar]
- 28.Iorio R, Robb WJ, Healy WL, Berry DJ, Hozack WJ, Kyle RF, Lewallen DG, Trousdale RT, Jiranek WA, Stamos VP, Parsley BS. Orthopaedic surgeon workforce and volume assessment for total hip and knee replacement in the United States: preparing for an epidemic. J Bone Joint Surg Am. 2008;90:1598–1605. doi: 10.2106/JBJS.H.00067. [DOI] [PubMed] [Google Scholar]
- 29.Jones CA, Voaklander DC, Johnston DW, Suarez-Almanzor ME. Health related quality of life outcomes after total hip and knee artrhoplasties in a community based population. J Rheumatol. 2000;27:1745–1752. [PubMed] [Google Scholar]
- 30.Jones CA, Voaklander DC, Suarez-Alma ME. Determinants of function after total knee arthroplasty. Phys Ther. 2003;83:696–706. [PubMed] [Google Scholar]
- 31.Kurtz S, Ong K, Lau E, Mowat F, Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 32.Lavernia CJ, Alcerro JC, Rossi MD. Fear in arthroplasty surgery. Clin Orthop Relat Res. 2010;468:547–554. doi: 10.1007/s11999-009-1101-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lingard EA, Katz JN, Wright EA. Sledge CB; Kinemax Outcomes Group. Predicting the outcome of total knee arthroplasty. J Bone Joint Surg Am. 2004;86:2179–2186. doi: 10.2106/00004623-200410000-00008. [DOI] [PubMed] [Google Scholar]
- 34.Lingard EA, Riddle DL. Impact of psychological distress on pain and function following knee arthroplasty. J Bone Joint Surg Am. 2007;89:1161–1169. doi: 10.2106/JBJS.F.00914. [DOI] [PubMed] [Google Scholar]
- 35.Moore JE, Von Korff M, Cherkin D, Saunders K, Lorig K. A randomized trial of a cognitive-behavioral program for enhancing back pain self care in a primary care setting. Pain. 2000;88:145–153. doi: 10.1016/S0304-3959(00)00314-6. [DOI] [PubMed] [Google Scholar]
- 36.Nilsdotter AK, Toksvig-Larsen S, Roos EM. A 5 year prospective study of patient-relevant outcomes after total knee replacement. Osteoarthritis Cartilage. 2009;17:601–606. doi: 10.1016/j.joca.2008.11.007. [DOI] [PubMed] [Google Scholar]
- 37.Paulsen MG, Dowsey MM, Castle D, Choong PF. Preoperative psychological distress and functional outcome after knee replacement. ANZ J Surg. 2011;81:681–687. doi: 10.1111/j.1445-2197.2010.05634.x. [DOI] [PubMed] [Google Scholar]
- 38.Riddle DL, Wade JB, Jiranek WA, Kong X. Preoperative pain catastrophizing predicts pain outcome after knee arthroplasty. Clin Orthop Relat Res. 2010;468:798–806. doi: 10.1007/s11999-009-0963-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Riediger W, Doering S, Krismer M. Depression and somatisation influence the outcome of total hip replacement. Int Orthop. 2010;34:13–18. doi: 10.1007/s00264-008-0688-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Salmon P, Hall GM, Peerbhoy D. Influence of the emotional response to surgery on functional recovery during 6 months after hip arthroplasty. J Behav Med. 2001;24:489–502. doi: 10.1023/A:1012275611394. [DOI] [PubMed] [Google Scholar]
- 41.Sangha O, Stucki G, Liang MH, Fossel AH, Katz JN. The Self-Administered Comorbidity Questionnaire: a new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003;49:156–163. doi: 10.1002/art.10993. [DOI] [PubMed] [Google Scholar]
- 42.Santić V, Legović D, Sestan B, Jurdana H, Marinović M. Measuring improvement following total hip and knee arthroplasty using the SF-36 Health Survey. Coll Antropol. 2012;36:207–212. [PubMed] [Google Scholar]
- 43.Singh JA, Gabriel S, Lewallen D. The impact of gender, age, and preoperative pain severity on pain after TKA. Clin Orthop Relat Res. 2008;466:2717–2723. doi: 10.1007/s11999-008-0399-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Walton MJ, Newman JH. Preoperative mental wellbeing and the outcome of knee replacement. Knee. 2008;15:277–280. doi: 10.1016/j.knee.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 45.Wewers ME, Lowe NK. A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health. 1990;13:227–236. doi: 10.1002/nur.4770130405. [DOI] [PubMed] [Google Scholar]
- 46.WHO. Physical Status: The Use and Interpretation of Anthropometry. Report of a WHO Expert Committee. WHO Technical Report Series 854. Geneva, Switzerland: World Health Organization; 1995. [PubMed]
- 47.Wylde V, Dieppe P, Hewlett S, Learmonth ID. Total knee replacement: is it really an effective procedure for all? Knee. 2007;14:417–423. doi: 10.1016/j.knee.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 48.Wylde V, Hewlett S, Learmonth D, Dieppe P. Persistent pain after joint replacement: Prevalence, sensory qualities, and postoperative determinants. Pain. 2011;152:566–572. doi: 10.1016/j.pain.2010.11.023. [DOI] [PubMed] [Google Scholar]
- 49.Zigmong AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 50.Zywiel MG, Stroh DA, Lee SY, Bonutti PM, Mont MA. Chronic opioid use prior to total knee arthroplasty. J Bone Joint Surg Am. 2011;93:1988–1993. doi: 10.2106/JBJS.J.01473. [DOI] [PubMed] [Google Scholar]