Abstract
Objective:
To examine independent and combined associations among objectively measured movement/non-movement behaviors (moderate-to-vigorous-intensity physical activity (MVPA), total sedentary time and sleep duration) and adiposity indicators in a sample of Canadian children.
Methods:
A cross-sectional study was conducted on 507 children aged 9–11 years from Ottawa, Canada. Movement/non-movement behaviors were assessed using an Actigraph GT3X+ accelerometer over 7 days (24-h protocol). Outcomes included percentage body fat (bioelectrical impedance) and waist-to-height ratio.
Results:
After adjustment for age, sex, ethnicity, maturity offset, fast food consumption, annual household income and highest level of parental education, MVPA was inversely and sedentary time positively associated with adiposity indicators, whereas sleep duration was not. However, only MVPA remained significantly associated with adiposity indicators after additional adjustment for the other movement/non-movement behaviors. Combined associations using tertiles of the three movement/non-movement behaviors showed that higher levels of MVPA were associated with lower adiposity indicators, irrespective of total sedentary time and sleep duration.
Conclusions:
Higher levels of MVPA were associated with lower adiposity in this sample of children regardless of sedentary time and sleep duration. Although correlational in nature, these findings suggest that future efforts of obesity reduction should focus more on increasing MVPA than on reducing sedentary time or increasing sleep duration to maximize the effectiveness of interventions.
Introduction
Low levels of moderate-to-vigorous-intensity physical activity (MVPA), high levels of sedentary time, and short sleep duration have all been associated with higher levels of adiposity in many recent investigations.1, 2, 3 However, these movement/non-movement behaviors have mainly been examined in isolation of each other and with the use of suboptimal indicators of adiposity (for example, body mass index or skinfold thickness). Recent technological advances in the measurement of movement/non-movement behaviors now allow researchers to assess the full movement spectrum over 24 h with the use of a single accelerometer. The relationships among movement/non-movement behaviors (MVPA, sedentary time and sleep duration) and adiposity are understudied in children and poorly understood. A better understanding of the inter-relationships among them will aid to better tailor our interventions aimed at reducing adiposity in children.
We recently reported that low MVPA and short sleep duration were independently associated with a higher fat mass index in Danish children, and combined associations of movement/non-movement behaviors showed a synergistic effect with fat mass index.4 This study was the first to investigate MVPA, sedentary behavior and sleep using a single accelerometer worn over 24 h in children. However, the baseline examination was conducted within a nutrition intervention study, which may have influenced the results obtained. Given that the independent and combined associations between movement/non-movement behaviors and adiposity are largely unknown in children, a better understanding of these relationships may help to inform public health messages and policies aimed at addressing obesity in the pediatric population.
Therefore, the objective of this study was to examine the independent and combined relationships among objectively measured movement/non-movement behaviors (MVPA, sedentary time and sleep duration) and indicators of adiposity in a sample of Canadian children aged 9–11 years. Based on recent findings in children and youth,4, 5, 6, 7 it is hypothesized that only MVPA and sleep duration would be associated with lower adiposity indices in this sample of children regardless of their amount of sedentary behavior.
Subjects and methods
Participants
The International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE) is a multi-national, cross-sectional study conducted in 12 countries. More details on the study design and methods can be found elsewhere.8 Analyses of the present study include data from the Canadian ISCOLE site. Briefly, data were collected in 26 schools on 567 children in the 5th grade (57.1% female; 9–11 years of age) from Ottawa, Canada between September 2012 and May 2013. Schools were stratified into four groups: English Public (n=393; 69.3%), French Public (n=60; 10.6%), English Catholic (n=75; 13.2%) and French Catholic (n=39; 6.8%). All schools within each stratum were invited to participate and the first to respond were included into the study, in agreement with the rules of our research ethics boards. This project was approved by the research ethics board at the Children's Hospital of Eastern Ontario and the participating school boards. Written informed parental consent and child assent were obtained for all participants.
Assessment of physical activity, sedentary behavior and sleep
The Actigraph GT3X+ accelerometer (ActiGraph LLC, Pensacola, FL, USA) was used to objectively monitor whole-day physical activity, sedentary behavior and sleep duration.8 Children wore the device on a belt around the waist at the right mid-axillary line 24 h per day for 7 consecutive days. Children were asked to remove the device for aquatic activities and showering/bathing. Study staff instructed children on how to wear the device and conducted an in-person compliance check 2–4 days after initialization to ensure the child was following the accelerometer wear protocol. Two compliance phone calls were also made to the parents/guardians (one weekday call and one weekend call) to ensure that the device was being worn properly, and to answer any questions about the device. A valid recording for physical activity and sedentary time required at least 4 days (including at least one weekend day) of at least 10 h of wake/wear time per day.9, 10 Data were collected at a sampling rate of 80 Hz, downloaded in 1-s epochs, and were aggregated to 15-s epochs.11 MVPA was defined as ⩾574 counts per 15 s and total sedentary time as ⩽25 counts per 15 s, consistent with widely used cutoffs from Evenson et al.11 Sleep period time was obtained with the use of a fully automated algorithm for 24-h waist-worn accelerometers that was recently validated for ISCOLE.12 This new algorithm produces more precise estimates of sleep duration than previous algorithms and captures sleep period time from sleep onset to the end of sleep, including all epochs and wakefulness after onset.12 The weekly sleep averages were calculated using only days where valid sleep was accumulated (total sleep >0 min) and only for participants with at least three nights of valid sleep, including a weekend day. A total of 60 children did not provide valid accelerometry data and were excluded from the analyses; thus, 209 boys and 298 girls were included in the current cross-sectional analytical sample. Of note, descriptive characteristics of participants with incomplete accelerometer data were not significantly different than those included in the present analyses. We also collected information about screen time to explore if the associations with adiposity are different between screen-based and non-screen sedentary behaviors. Daily screen time was assessed based on the child's report of time spent in watching television, playing video/computer games or using a computer for something that is not school work related on weekdays and weekend days, and an aggregated weighted mean score over the 7 days was computed.8 Self-report methods of quantifying screen time have been reported to have acceptable reliability and validity in children.13
Assessment of adiposity indicators
A battery of anthropometric measurements was taken according to standardized procedures by trained study staff in schools during school hours.8 Height was measured without shoes using a Seca 213 portable stadiometer (Hamburg, Germany), with the participant's head in the Frankfort Plane. Height was measured with participant standing fully erect, feet together, and at the end of a deep inhalation.14 Waist circumference was measured at the end of a gentle expiration with a nonelastic tape held midway between the lower rib margin and the iliac crest.15 Each measurement was repeated, and the average used for analysis (a third measurement was obtained if the first two measurements were >0.5 cm apart and the average of the two closest measurements was used for analysis). In addition, the participant's body weight and percentage body fat (% BF) were measured using a portable Tanita SC-240 Body Composition Analyzer (Arlington Heights, IL, USA) after all outer clothing, heavy pocket items and shoes and socks were removed. Two measurements were obtained, and the average was used in analysis (a third measurement was obtained if the first two measurements were >0.5 kg or 2.0% apart, for body weight and % BF, respectively, and the closest two were averaged for analysis). The Tanita SC-240 showed acceptable accuracy for estimating % BF when compared with dual-energy X-ray absorptiometry, supporting its use in field studies.16 Body mass index (body weight (kg) per height (m2)) and waist-to-height ratio (WHtR) were also calculated. Outcome measures for the present study included % BF (an indicator of overall adiposity) and WHtR (an indicator of central adiposity). Recent investigations showed that WHtR is a useful index to identify children with high cardiometabolic risk.17, 18, 19 A WHtR cut-point ⩾0.5 is associated with increased cardiometabolic risk.
Covariates
Demographic questionnaires completed by parents were used to determine children's age, sex, ethnicity (White/Caucasian, African American, Asian, First Nations, East Indian, ‘don't know' or ‘other'), total annual family income (eight options ranging from <$14 999 to $140 000 or more) and the highest level of parental education (six options: less than high school, some high school, high school diploma/GED, diploma or 1–3 years of college, bachelor's degree or graduate degree (master's or PhD/professional degree). Biological maturity was estimated using the maturity offset method, which estimates an individual's age from peak height velocity.20 Furthermore, frequency of fast food consumption (for example, pizza, hamburgers, etc.) was self-reported by the participants as part of a larger questionnaire and was used as a proxy measure of diet quality. There were seven response options ranging from ‘never' to ‘every day, more than once'. These covariates were chosen because of their association with the exposures and/or the outcomes. Given that over-fitting can be a concern with our relatively small sample size, different analyses were conducted to assess model fit (including testing for multicollinearity) and results demonstrated that our models had good predictive performance and were not subject to over-fitting.
Statistical analysis
As there was no statistically significant sex interaction between movement/non-movement behaviors and the outcome variables, data for both sexes were pooled to maximize power. Descriptive characteristics included means for continuous variables and percentages for categorical variables. Multivariable linear regression was used to examine the independent associations between movement/non-movement behaviors (MVPA, total sedentary time, sleep duration) and adiposity indicators. All regression models included age, sex, ethnicity, maturity offset, fast food consumption, annual household income and highest level of parental education as covariates. Thereafter, we mutually adjusted the movement/non-movement behaviors for one another in the models to determine whether the associations remained statistically significant. The variance inflation factors between movement/non-movement behaviors were <5, suggesting that multicollinearity was not a problem in the models. In combined analyses, adiposity indicators were compared between tertiles of MVPA/sedentary time/sleep duration using analysis of covariance controlling for the above-mentioned covariates. Tukey post hoc tests were used to identify which groups were statistically different from one another, and we used a Bonferroni adjustment to account for multiple comparisons. A two-tailed P-value of <0.05 was considered to indicate statistical significance. All statistical analyses were performed using the JMP version 11 program (SAS Institute, Cary, NC, USA).
Results
Descriptive characteristics of the sample are shown in Table 1. Overall, 85% of children had a WHtR of <0.5, 43% had an average of ⩾60 min of MVPA per day, 45% reported ⩽2 h per day of screen time and 12% slept ⩾10 h perday. Total sedentary time represented 57% of waking hours and accelerometer wear time was on average >23 h in this sample of children.
Table 1. Descriptive characteristics of participants (n=507).
| Variable | Mean±s.d. or n (%) |
|---|---|
| Age (years) | 10.0±0.4 |
| Sex | |
| Boys | 209 (41.2) |
| Girls | 298 (58.8) |
| Ethnicity | |
| White/Caucasian | 335 (66.8) |
| African-American | 12 (2.4) |
| Asian | 50 (10.0) |
| First nations | 2 (0.4) |
| East Indian | 4 (0.8) |
| Don't know | 1 (0.2) |
| Other | 97 (19.4) |
| Body mass index (kg m−2) | 18.3±3.4 |
| Fat mass (%) | 20.6±7.5 |
| Waist circumference (cm) | 63.1±8.6 |
| Waist-to-height ratio | 0.44±0.05 |
| Moderate-to-vigorous physical activity (min per day) | 58.5±19.4 |
| Total sedentary time (min per day) | 512.8±61.4 |
| Self-reported screen time (h per day) | 2.8±1.8 |
| Sleep duration (min per day) | 544.4±50.7 |
Independent associations between movement/non-movement behaviors and adiposity indicators are shown in Table 2. All three movement/non-movement behaviors were significantly associated with % BF and WHtR in unadjusted models. After adjustment for covariates, sleep duration was no longer associated with adiposity indicators, whereas MVPA was inversely and sedentary time positively associated with % BF and WHtR. However, only MVPA remained significantly associated with adiposity indicators after additional adjustment for the other two non-movement behaviors. Exploratory analyses revealed that self-reported screen time was significantly associated with adiposity indicators in the unadjusted model only (model 1) and the associations were no longer significant after additional adjustments (models 2 and 3) (data not shown).
Table 2. Associations of objectively measured physical activity, sedentary time and sleep duration with adiposity indicators in a sample of 9–11-year-old Canadian children.
|
% Body fat |
Waist-to-height ratio |
|||||
|---|---|---|---|---|---|---|
| β | R2 | P | β | R2 | P | |
| MVPA (min per day) | ||||||
| Model 1 | −0.117 | 0.09 | <0.001 | −0.0004 | 0.02 | <0.01 |
| Model 2 | −0.060 | 0.04 | <0.001 | −0.0004 | 0.03 | <0.001 |
| Model 3 | −0.044 | 0.02 | <0.01 | −0.0003 | 0.02 | <0.01 |
| Total sedentary time (min per day) | ||||||
| Model 1 | 0.024 | 0.04 | <0.001 | 0.0001 | 0.02 | <0.01 |
| Model 2 | 0.011 | 0.01 | 0.02 | 0.00007 | 0.01 | 0.04 |
| Model 3 | −0.002 | <0.01 | 0.65 | −0.00002 | <0.01 | 0.61 |
| Sleep duration (min per day) | ||||||
| Model 1 | −0.019 | 0.02 | <0.01 | −0.0002 | 0.02 | <0.01 |
| Model 2 | −0.008 | <0.01 | 0.16 | −0.00004 | <0.01 | 0.32 |
| Model 3 | −0.006 | <0.01 | 0.25 | −0.00004 | <0.01 | 0.36 |
Abbreviation: MVPA, moderate-to-vigorous physical activity.
Model 1: unadjusted.
Model 2: adjusted for age, sex, ethnicity, maturity offset, fast food consumption, annual household income and highest level of parental education.
Model 3: adjusted for age, sex, ethnicity, maturity offset, fast food consumption, annual household income, highest level of parental education and the other two movement/non-movement behaviors.
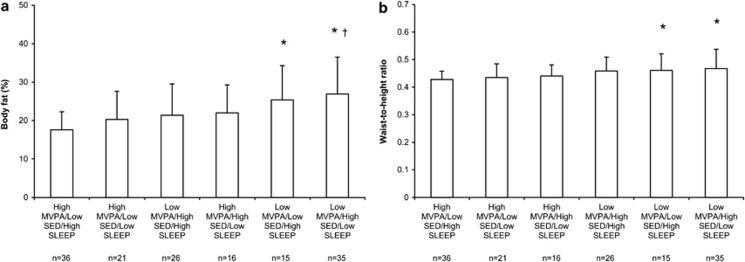
Combined associations among movement/non-movement behaviors and adiposity indicators are shown in Figure 1. Among the eight possible combinations of movement/non-movement behaviors, two groups have been removed from the analysis because they had a sample size of less than five children, thereby rendering statistical comparisons not possible. Overall, higher levels of MVPA were associated with significantly lower values of % BF and WHtR, irrespective of total sedentary time and sleep duration. Specifically, children with the least healthy pattern (that is, lower tertile of MVPA, higher tertile of sedentary time and lower tertile of sleep) have a 9.3% point higher % BF than those in the opposite tertiles. Analyses were repeated using self-reported screen time instead of objectively measured sedentary behavior and the results were not significantly different (data not shown). Of note, independent and combined associations were similar with the use of other adiposity outcomes such as body mass index Z-score or waist circumference (data not shown).
Figure 1.
Combined associations of moderate-to-vigorous-intensity physical activity (MVPA), total sedentary time (SED) and sleep duration (SLEEP) with (a) percent body fat and (b) waist-to-height ratio in 9–11-year-old Canadian children. Data are presented as means±s.d. Mean time spent in MVPA was 38.3±8.0 and 80.3±12.6 min per day in the low- and high-tertile groups, respectively. Mean time spent sedentary was 447.5±30.5 and 580.3±36.4 min per day in the low- and high-tertile groups, respectively. Mean time spent in sleeping was 487.8±32.9 and 596.2±24.3 min per day in the low- and high-tertile groups, respectively. Adiposity indicators of participants between tertiles of MVPA/SED/SLEEP were compared by ANCOVA, followed by a Tukey post hoc test to determine which groups were significantly different. The model was adjusted for age, sex, ethnicity, maturity offset, fast food consumption, annual household income and highest level of parental education. *P<0.05 vs high MVPA/low SED/high SLEEP; †P<0.05 vs high MVPA/low SED/low SLEEP.
Discussion
Overall, our results support the proposed hypothesis that higher levels of MVPA are associated with lower adiposity regardless of the amount of time spent in sedentary behaviors and asleep. In contrast, our results do not support the hypothesis that sleep duration is independently associated with adiposity in this sample of children. These findings suggest that participation in physical activity of at least moderate intensity is more important to adiposity status in childhood than total sedentary time or sleep duration. These findings further support the notion that future efforts of obesity reduction and/or prevention should focus on finding ways to increase MVPA in children.7
Our results agree with previous investigations showing that higher MVPA in children was associated with lower adiposity and better cardiometabolic health regardless of the amount of sedentary time.4, 5, 6, 7, 21 However, the present results contrast some previous observations in adults suggesting that objectively measured sedentary time is related to higher adiposity indicators and/or poorer cardiometabolic health independent of MVPA.22, 23, 24 The discrepancy in results between children and adults is still a matter of debate. Possible explanations include the fact that children are generally much healthier than adults (thereby reducing the inter-individual variability) and the fact that children generally have higher physical activity levels on a daily basis than adults (thereby confounding the associations between sedentary behaviors and cardiometabolic health outcomes). Indeed, cross-sectional associations between accelerometer-assessed sedentary time and adiposity in children are generally not present or disappear after adjusting for MVPA.5, 7, 21, 25 Future studies will be needed to better understand and elucidate the conflicting findings between children and adults.
Self-reported screen time has been reported more frequently to be associated with adiposity than objectively measured sedentary time in previous studies.5, 26, 27 This suggests that total sedentary time includes many different types of sedentary activities, some of which are possibly more deleterious than others on cardiometabolic health indicators. In this study, neither total sedentary time nor screen time was independently associated with adiposity after adjustment for MVPA. Likewise, sedentary time was not an important variable in the combined analyses, as adiposity was primarily explained by the amount of MVPA. This observation is similar to previous studies conducted in children4, 5, 6, 7, 21 and reinforces the idea that increasing children's participation in MVPA should be an important public health target to achieve. This is even more concerning given that only 7% of Canadian children and youth meet the physical activity guidelines of ⩾60 min of MVPA on a daily basis.28
Based on the fully adjusted model, 1 h per day higher MVPA was associated with a 2.6% point lower % BF (−0.044 × 60 min=2.6). Conversely, 1 h per day lower total sedentary time or 1 h per day higher sleep duration were associated with only a 0.12 and 0.36% point lower % BF in the full model. The pattern of findings for WHtR was similar to that for % BF with a similar variance explained for the full models. The magnitude of association between MVPA and adiposity is even more meaningful in the combined analysis. We observed that % BF differed by as much as 9.3% points between the two opposing groups (healthiest vs least healthy movement/non-movement behaviors). Such a large difference is clinically significant and meaningful from a public health perspective. It also agrees with a recent study using isotemporal substitution modeling in 2185 individuals showing that MVPA may be the most potent health-enhancing, time-dependent behavior, with additional benefit conferred from light-intensity activities and sleep duration when reallocated from sedentary time.29
The observation that sleep duration was not independently associated with adiposity in this sample of children is contrary to many previous observations in the field.4, 30, 31 Although sleep duration was associated with both adiposity indicators in the present study, the relationships were no longer significant after controlling for covariates. We believe that the adjustment for several important confounding factors is a strength of this study. Most previous cross-sectional studies looking at the relationship between sleep duration and adiposity adjusted for a small number of covariates but claimed that the association was ‘independent'.3 There is always the possibility of residual confounding in observational studies and the present study suggests that, at least in this sample of children, the sleep-adiposity association is explained by other factors.
Strengths of this study include objectively measured movement/non-movement behaviors monitored using a 24-h protocol in a population-based sample of children. In addition, data have been collected on other important key variables, including biological maturity, ethnicity, diet quality and socioeconomic status. However, our results need to be interpreted in light of the following limitations. First, the direction of causality cannot be determined from cross-sectional data. Second, limitations of accelerometry include the inability to accurately capture the true movement and energy expenditure of activities such as cycling, swimming and carrying loads. Consensus is also lacking on the best device to use, appropriate epoch length, importance of bouts of movement and minimum data requirements for inclusion in analyses. Third, total sedentary time measured by accelerometry does not provide information about the type of sedentary behavior or context (for example, screen-based vs non-screen sedentary behavior). Fourth, sleep duration measured with the accelerometer only provides information about sleep quantity; however, other dimensions of sleep could also be relevant and associated with adiposity (for example, sleep quality, timing, architecture, consistency and continuity). Fifth, food intake (kJ per day) was not assessed in ISCOLE and only a proxy measure of diet quality (that is, fast food consumption) was used. Finally, the external generalizability of these findings may be mainly restricted to Canadian children of Western European descent.
In conclusion, the present study provides evidence that higher levels of MVPA are associated with lower adiposity regardless of sedentary time and sleep duration. Increasing children's participation in MVPA should, thus, be an important public health target to achieve.
Acknowledgments
We thank Claire Francis, Jessica McNeil, Hadiza Amedu-Ode and Nina Azoug-Boneault for their role in data collection for the Canadian site of ISCOLE, and the Coordinating Center of ISCOLE in Baton Rouge, Louisiana, specifically Drs Peter Katzmarzyk and Timothy Church. We thank the study participants along with their parents, teachers and school principals for their involvement in the study. ISCOLE was funded by the Coca-Cola Company. The funder had no role in study design, data collection and analysis, decision to publish or preparation of this manuscript.
Author contributions
Designed research: JPC and MST; coordinated data collection: JPC, GL, CB, PB, AGL, MMB, MST; analyzed and interpreted data: JPC; discussed the analysis and interpretation of the data: GL, CB, PB, AGL, MMB, MST; wrote paper: JPC; had primary responsibility of the final content: JPC. All authors reviewed the manuscript critically and approved the final manuscript.
The authors declare no conflict of interest.
References
- Prentice-Dunn H, Prentice-Dunn S. Physical activity, sedentary behavior, and childhood obesity: a review of cross-sectional studies. Psychol Health Med. 2012;17:255–273. doi: 10.1080/13548506.2011.608806. [DOI] [PubMed] [Google Scholar]
- Tremblay MS, Colley RC, Saunders TJ, Healy GN, Owen N. Physiological and health implications of a sedentary lifestyle. Appl Physiol Nutr Metab. 2010;35:725–740. doi: 10.1139/H10-079. [DOI] [PubMed] [Google Scholar]
- Chaput JP, Tremblay A. Insufficient sleep as a contributor to weight gain: an update. Curr Obes Rep. 2012;1:245–256. [Google Scholar]
- Hjorth MF, Chaput JP, Ritz C, Dalskov SM, Andersen R, Astrup A, et al. Fatness predicts decreased physical activity and increased sedentary time, but not vice versa: support from a longitudinal study in 8- to 11-year-old children Int J Obes 2013. e-pub ahead of print 7 January 2014; doi: 10.1038/ijo.2013.229 [DOI] [PubMed]
- Chaput JP, Lambert M, Mathieu ME, Tremblay MS, O'Loughlin J, Tremblay A. Physical activity vs sedentary time: independent associations with adiposity in children. Pediatr Obes. 2012;7:251–258. doi: 10.1111/j.2047-6310.2011.00028.x. [DOI] [PubMed] [Google Scholar]
- Chaput JP, Saunders TJ, Mathieu ME, Henderson M, Tremblay MS, O'Loughlin J, et al. Combined associations between moderate to vigorous physical activity and sedentary behaviour with cardiometabolic risk factors in children. Appl Physiol Nutr Metab. 2013;38:477–483. doi: 10.1139/apnm-2012-0382. [DOI] [PubMed] [Google Scholar]
- Ekelund U, Luan J, Sherar LB, Esliger DW, Griew P, Cooper A. International Children's Accelerometry Database (ICAD) Collaborators. Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. JAMA. 2012;307:704–712. doi: 10.1001/jama.2012.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katzmarzyk PT, Barreira TV, Broyles ST, Champagne CM, Chaput JP, Fogelholm M, et al. The International Study of Childhood Obesity, Lifestyle and the Environment (ISCOLE): design and methods. BMC Public Health. 2013;13:900. doi: 10.1186/1471-2458-13-900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colley R, Gorber SC, Tremblay MS. Quality control and data reduction procedures for accelerometry-derived measures of physical activity. Health Rep. 2010;21:63–69. [PubMed] [Google Scholar]
- Trost SG, Loprinzi PD, Moore R, Pfeiffer KA. Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc. 2011;43:1360–1368. doi: 10.1249/MSS.0b013e318206476e. [DOI] [PubMed] [Google Scholar]
- Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci. 2008;26:1557–1565. doi: 10.1080/02640410802334196. [DOI] [PubMed] [Google Scholar]
- Tudor-Locke C, Barreira TV, Schuna JM, Jr, Mire EF, Katzmarzyk PT. Fully automated waist-worn accelerometer algorithm for detecting children's sleep-period time separate from 24-h physical activity or sedentary behaviors. Appl Physiol Nutr Metab. 2014;39:53–57. doi: 10.1139/apnm-2013-0173. [DOI] [PubMed] [Google Scholar]
- Lubans DR, Hesketh K, Cliff DP, Barnett LM, Salmon J, Dollman J, et al. A systematic review of the validity and reliability of sedentary behaviour measures used with children and adolescents. Obes Rev. 2011;12:781–799. doi: 10.1111/j.1467-789X.2011.00896.x. [DOI] [PubMed] [Google Scholar]
- Lohman TG, Roche AF, Martorell R.edsAnthropometric Standardization Reference Manual Human Kinetics: Champaign, IL, USA; 1988 [Google Scholar]
- World Health Organization Waist Circumference and Waist-Hip Ratio: Report of a WHO Expert ConsultationGeneva, 8–11 December 2008. World Health Organization: Geneva; 2011 [Google Scholar]
- Barreira TV, Staiano AE, Katzmarzyk PT. Validity assessment of a portable bioimpedance scale to estimate body fat percentage in white and African-American children and adolescents. Pediatr Obes. 2013;8:e29–e32. doi: 10.1111/j.2047-6310.2012.00122.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keefer DJ, Caputo JL, Tseh W. Waist-to-height ratio and body mass index as indicators of cardiovascular risk in youth. J Sch Health. 2013;83:805–809. doi: 10.1111/josh.12097. [DOI] [PubMed] [Google Scholar]
- Savva SC, Lamnisos D, Kafatos AG. Predicting cardiometabolic risk: waist-to-height ratio or BMI. A meta-analysis. Diabetes Metab Syndr Obes. 2013;6:403–419. doi: 10.2147/DMSO.S34220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maffeis C, Banzato C, Talamini G. Obesity Study Group of the Italian Society of Pediatric Endocrinology and Diabetology. Waist-to-height ratio, a useful index to identify high metabolic risk in overweight children. J Pediatr. 2008;152:207–213. doi: 10.1016/j.jpeds.2007.09.021. [DOI] [PubMed] [Google Scholar]
- Mirwald RL, Baxter-Jones ADG, Bailey DA, Beunen GP. An assessment of maturity from anthropometric measurements. Med Sci Sports Exerc. 2002;34:689–694. doi: 10.1097/00005768-200204000-00020. [DOI] [PubMed] [Google Scholar]
- Colley RC, Wong SL, Garriguet D, Janssen I, Connor Gorber S, Tremblay MS. Physical activity, sedentary behaviour and sleep in Canadian children: parent-report versus direct measures and relative associations with health risk. Health Rep. 2012;23:45–52. [PubMed] [Google Scholar]
- Henson J, Yates T, Biddle SJ, Edwardson CL, Khunti K, Wilmot EG, et al. Associations of objectively measured sedentary behaviour and physical activity with markers of cardiometabolic health. Diabetologia. 2013;56:1012–1020. doi: 10.1007/s00125-013-2845-9. [DOI] [PubMed] [Google Scholar]
- Thorp AA, Healy GN, Owen N, Salmon J, Ball K, Shaw JE, et al. Deleterious associations of sitting time and television viewing time with cardiometabolic risk biomarkers: Australian Diabetes, Obesity and Lifestyle (AusDiab) study 2004-2005. Diabetes Care. 2010;33:327–334. doi: 10.2337/dc09-0493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Healy GN, Wijndaele K, Dunstan DW, Shaw JE, Salmon J, Zimmet PZ, et al. Objectively measured sedentary time, physical activity, and metabolic risk: the Australian Diabetes, Obesity and Lifestyle Study (AusDiab) Diabetes Care. 2008;31:369–371. doi: 10.2337/dc07-1795. [DOI] [PubMed] [Google Scholar]
- Steele RM, van Sluijs EM, Cassidy A, Griffin SJ, Ekelund U. Targeting sedentary time or moderate- and vigorous-intensity activity: independent relations with adiposity in a population-based sample of 10-y-old children. Am J Clin Nutr. 2009;90:1185–1192. doi: 10.3945/ajcn.2009.28153. [DOI] [PubMed] [Google Scholar]
- Carson V, Janssen I. Volume, patterns, and types of sedentary behavior and cardio-metabolic health in children and adolescents: a cross-sectional study. BMC Public Health. 2011;4:274. doi: 10.1186/1471-2458-11-274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laurson KR, Eisenmann JC, Welk GJ, Wickel EE, Gentile DA, Walsh DA. Combined influence of physical activity and screen time recommendations on childhood overweight. J Pediatr. 2008;153:209–214. doi: 10.1016/j.jpeds.2008.02.042. [DOI] [PubMed] [Google Scholar]
- Colley RC, Garriguet D, Janssen I, Craig CL, Clarke J, Tremblay MS. Physical activity of Canadian children and youth: accelerometer results from the 2007 to 2009 Canadian Health Measures Survey. Health Rep. 2011;22:12–20. [PubMed] [Google Scholar]
- Buman MP, Winkler EA, Kurka JM, Hekler EB, Baldwin CM, Owen N, et al. Reallocating time to sleep, sedentary behaviors, or active behaviors: associations with cardiovascular disease risk biomarkers, NHANES 2005-2006. Am J Epidemiol. 2014;179:323–334. doi: 10.1093/aje/kwt292. [DOI] [PubMed] [Google Scholar]
- Chaput JP, Lambert M, Gray-Donald K, McGrath JJ, Tremblay MS, O'Loughlin J, et al. Short sleep duration is independently associated with overweight and obesity in Quebec children. Can J Public Health. 2011;102:369–374. doi: 10.1007/BF03404179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi Z, Taylor AW, Gill TK, Tuckerman J, Adams R, Martin J. Short sleep duration and obesity among Australian children. BMC Public Health. 2010;10:609. doi: 10.1186/1471-2458-10-609. [DOI] [PMC free article] [PubMed] [Google Scholar]