Abstract
Ischemic preconditioning is a form of intrinsic cardioprotection where an episode of sublethal ischemia protects against subsequent episodes of ischemia. Identifying a clinical biomarker of preconditioning could have important clinical implications, and prior work has focused on the electrocardiographic ST segment. However, the electrophysiology biomarker of preconditioning is increased action potential duration (APD) shortening with subsequent ischemic episodes, and APD shortening should primarily alter the T wave, not the ST segment. We translated findings from simulations to canine to patient models of preconditioning to test the hypothesis that the combination of increased [delta (Δ)] T wave amplitude with decreased ST segment elevation characterizes preconditioning. In simulations, decreased APD caused increased T wave amplitude with minimal ST segment elevation. In contrast, decreased action potential amplitude increased ST segment elevation significantly. In a canine model of preconditioning (9 mongrel dogs undergoing 4 ischemia-reperfusion episodes), ST segment amplitude increased more than T wave amplitude during the first ischemic episode [ΔT/ΔST slope = 0.81, 95% confidence interval (CI) 0.46–1.15]; however, during subsequent ischemic episodes the T wave increased significantly more than the ST segment (ΔT/ΔST slope = 2.43, CI 2.07–2.80) (P < 0.001 for interaction of occlusions 2 vs. 1). A similar result was observed in patients (9 patients undergoing 2 consecutive prolonged occlusions during elective percutaneous coronary intervention), with an increase in slope of ΔT/ΔST of 0.13 (CI −0.15 to 0.42) in the first occlusion to 1.02 (CI 0.31–1.73) in the second occlusion (P = 0.02). This integrated analysis of the T wave and ST segment goes beyond the standard approach to only analyze ST elevation, and detects cellular electrophysiology changes of preconditioning.
Keywords: acute myocardial infarction, electrocardiology, electrophysiology, quantitative modeling
in patients with acute myocardial infarction, a primary therapeutic goal is protection of the area at risk that remains in potentially reversible ischemia, to minimize infarct size and maximize ventricular function (30). Ischemic preconditioning is a form of intrinsic cardioprotection where an episode of sublethal ischemia protects against subsequent episodes of ischemia (30). Identifying electrocardiographic (ECG) signs of preconditioning at the time of patient presentation could have clinical importance in guiding decisions for cardioprotective interventions.
The cellular electrophysiological effects of acute myocardial ischemia have been characterized in experimental studies and integrated in computer simulation models to demonstrate the effect of individual metabolic and ion current changes on the cellular action potential (AP) (27). The principal AP changes (and associated extracellular electrogram changes) occurring during acute ischemia are depolarization of the resting membrane potential (causing TQ segment depression that appears as ST segment elevation), delayed initiation and decreased rate of rise in the AP upstroke (causing increased R wave amplitude), decrease of the AP amplitude (causing ST segment elevation), and shortening of AP duration (APD) (causing increased T wave amplitude) (19, 20). Experimental and simulation studies have shown that changes in extracellular potassium and pH, along with opening of ATP-dependent potassium channels (KATP), can account for the AP changes that occur in acute ischemia (15, 42).
Thus far, clinical studies of preconditioning have focused primarily on ST segment deviation, showing that, during serial ischemia and reperfusion episodes, there is less ST elevation with subsequent occlusions (8, 9, 22, 23, 31). However, APD shortening, which has been demonstrated to increase with preconditioning, results in increased T wave amplitude assuming there are no major delays in depolarization (15, 20).
The purpose of this study was to identify a translational electrophysiological basis for ischemic preconditioning from the basic cellular level to patient ECGs. Therefore, we developed the hypothesis that the combination of increasing T wave amplitude (ΔT) with decreasing ST elevation (ΔST) during subsequent occlusions characterizes ischemic preconditioning in simulations, canine experiments, and patients. This combination was reflected in the ratio between ΔT and ΔST.
MATERIALS AND METHODS
All experiments involving the use of laboratory animals conform to the guidelines of the American Physiological Society and the standards in the Guide for the Care and Use of Laboratory Animals, DHEW Publ. No. NIH 85–23, revised 1985. ECGs from patients were obtained from the STAFF III database, originally acquired at the Charleston Area Medical Center and approved by the institutional review board (33, 34).
Simulation model.
The simulation program ECGSIM (www.ecgsim.org) version 2.2.1 was used in this study (47). ECGSIM is a software for computer simulations used in research and in education that uses the equivalent surface source model to compute ECG signals on the body surface, as well as electrograms on both the endocardium and epicardium (13, 32, 45, 46, 47). Ischemia was simulated by altering combinations of APD and AP amplitude in a similar fashion as in a prior study on ischemia with ECGSIM (12).
The ECGSIM “normal male” model was used with default parameters. Next, the changes were applied to a 5-cm area around a reference node (ECGSIM index no. 3) on the anterior left ventricular wall near the first left anterior descending (LAD) diagonal artery. The magnitude of the changes decreased linearly from the reference node to zero at the edge of the 5-cm area. The reference node in baseline conditions depolarizes at 47 ms, repolarizes at 308 ms (APD of 261 ms), and has an AP amplitude of 100 mV (−85-mV resting potential, +15-mV plateau potential during depolarization). Lead V3 was chosen because changes in the selected ischemic zone have a maximal effect on that lead.
ECG simulation of preconditioning.
Experimental epicardial monophasic action potential (MAP) changes during ischemic preconditioning from the prior publication by Shattock et al. (41) were inputted into ECGSIM to simulate human ECGs during preconditioning. That prior study included eight open-chested pigs (20–25 kg body wt) that underwent two cycles of 8 min of LAD coronary artery occlusion (distal to the second major diagonal branch) and 8 min of reperfusion before 60 min of ischemia and 2 h of reperfusion. MAPs were recorded within the ischemic zone via a suction electrode. The authors reported the mean APD and ST segment change at each minute during 8 min of ischemia for each of the three cycles. In ECGSIM, APD was shortened proportionally to the APD changes reported, the plateau potential was reduced by 5 mV for every minute of occlusion down to −5 mV (extrapolated from experimental results from Cinca et al.), and the resting potential was adapted to have the same electrogram ST changes measured by Shattock et al. (7, 41). One ECG was simulated for each minute of occlusion, and the ECG lead V3 was analyzed to measure ST and T amplitudes.
ECG changes in canine model of preconditioning.
Body surface ECGs were analyzed from dogs undergoing a preconditioning protocol previously performed by Murry et al. (30). The methods of these studies were described in prior publications (11, 30, 48). In summary, nine mongrel dogs underwent four cycles of 5 min of occlusion of the left circumflex coronary artery followed by 5 min of reperfusion. Continuously recorded ECGs were analyzed in lead II every 30 s during each occlusion. The ECGs were scanned with a resolution of 600 dpi. ECGScan (AMPS LLC, Montichiari, Italy) was used to create digital XML-file ECGs. The digital ECGs were analyzed with CalECG (AMPS) (3, 4). At each time point of 30 s, two consecutive beats were analyzed to obtain a representative beat. ST- and T wave amplitudes were measured from baseline (PR segment) to the peak of the R wave, ST-J point, and the peak of the T wave. The PR segment was chosen as baseline as opposed to the TP segment because the T and P waves merged at faster heart rates (6). When biphasic, the highest positive deflection amplitude of the T wave was measured. If the T wave was completely negative, the negative peak was used. ΔST and ΔT were measured in reference to the time immediately before each occlusion.
ECG changes in human model of preconditioning.
ECGs were analyzed from the subset of nine patients in the STAFF-III database with two or more occlusions of ≥2 min in the same location of the LAD (33, 34). The STAFF-III database includes patients referred for elective balloon PCI at Charleston Area Medical Center (Charleston, WV) from 1995 to 1996. In some patients in this database two consecutive occlusions were performed. Digital 12-lead ECGs were recorded continuously (Siemens-Elema, Solna, Sweden) at baseline and during the procedure. ECGs were analyzed with custom software in Matlab, version R2008a (Mathworks Massachusetts) as previously described (26, 29, 36). The changes in amplitude of the ST segment and T wave (measured from PR segment) were calculated in reference to the time immediately before each occlusion. Of leads V2-V4, the single lead with the highest ST segment change during the first occlusion was chosen for analysis.
Statistical analysis.
Linear regression analysis was used to assess the relationship between ΔT and ΔST during each occlusion in the animal and human studies. The slope of the relationship with the corresponding 95% confidence interval (CI) was reported. Change in slope during subsequent occlusions was assessed by interaction analyses. Two-sided P values <0.05 were considered significant. Statistical analyses were performed using Stata 11 (StataCorp).
RESULTS
Simulation of human ECGs.
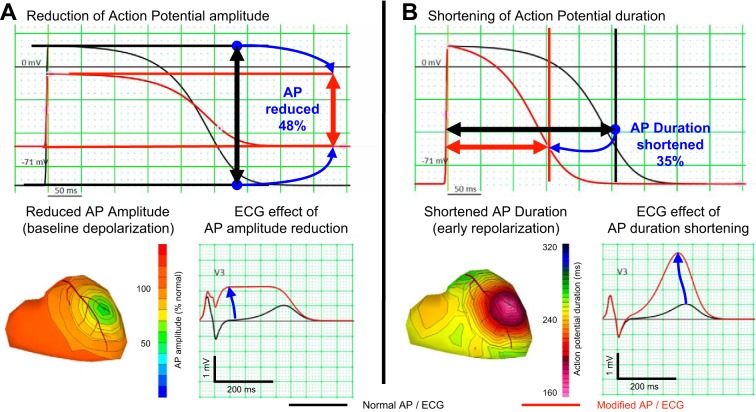
Simulated body surface ECGs resulting from changes in APs during ischemia are presented in Fig. 1. Altering the cellular APs in ECGSIM revealed that in leads above the ischemic zone (i.e., V2-V4), reduced AP amplitude led to a flattened, elevated ST segment with minimal T wave amplitude increase (Fig. 1A). Shortened APD caused tall peaked T waves with no change in the ST-J point amplitude (Fig. 1B).
Fig. 1.
Simulation of individual aspects of ischemia. A: reduction of action potential amplitude. B: shortening of action potential duration. Each panel shows, on the top, the action potential at baseline (black) and after the changes are applied. The part on bottom depicts the extent of the changes on the heart model on the left and the resulting electrocardiogram (ECG) on the right, both at baseline condition (black) then after changes (red). ECG, electrocardiogram; AP, action potential.
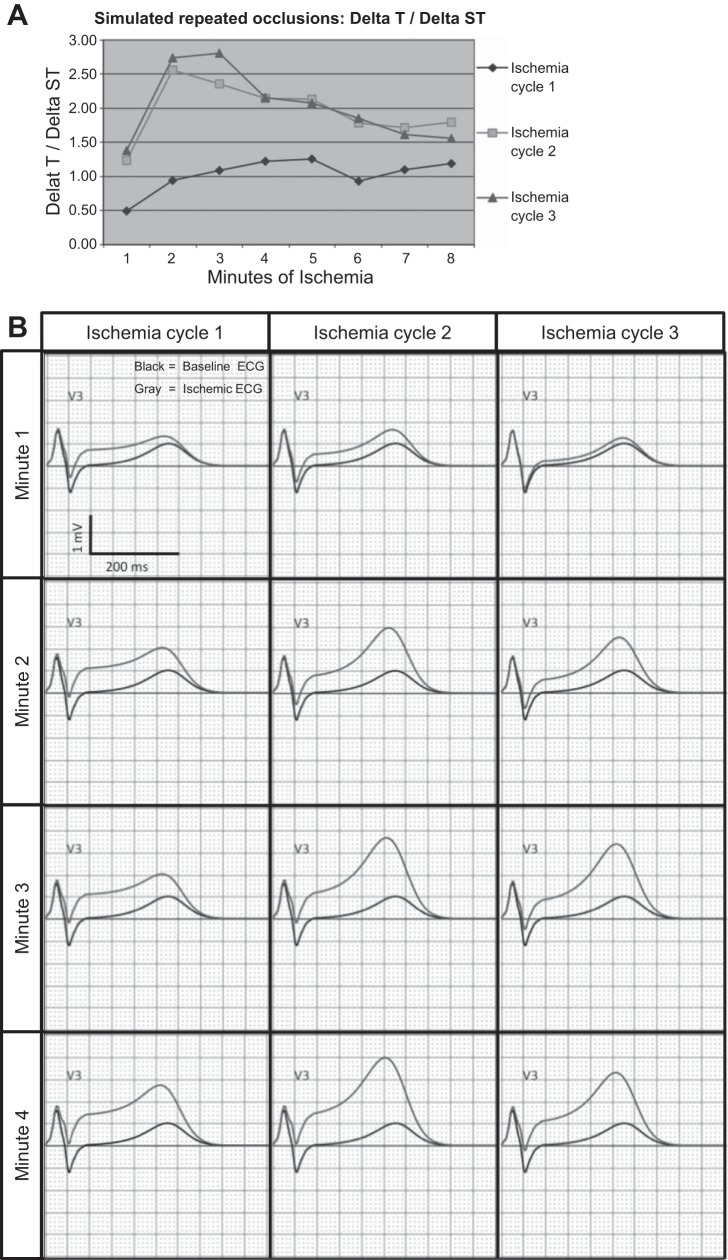
Simulations of human ECGs during preconditioning are shown in Fig. 2. During the first occlusion, the ST-J point amplitude increased significantly more than the T wave amplitude (Fig. 2, A and B), resulting in a flattened ST segment with minimal increase in T wave amplitude. However, in occlusion 2 (Fig. 2, A and C), this reversed and the T wave amplitude increased more than the ST-J point amplitude. ECG changes during occlusion 3 were almost identical to occlusion 2 (Fig. 2, A and D).
Fig. 2.
Transition of electrophysiological changes during subsequent occlusions in porcine simulation experiments. A: ΔT/ΔST in three subsequent cycles of ischemia. Ischemia cycle 1 causes an increase in ΔST-amplitude with less increase of ΔT wave amplitude, whereas the second and third ischemia cycles show a reversed relation. Accompanying body-surface ECGs (B) are shown for each minute of ischemia with specific changes in ST-amplitude and T wave amplitude. Black lines represent the baseline ECG. Gray lines represent the ischemia ECG.
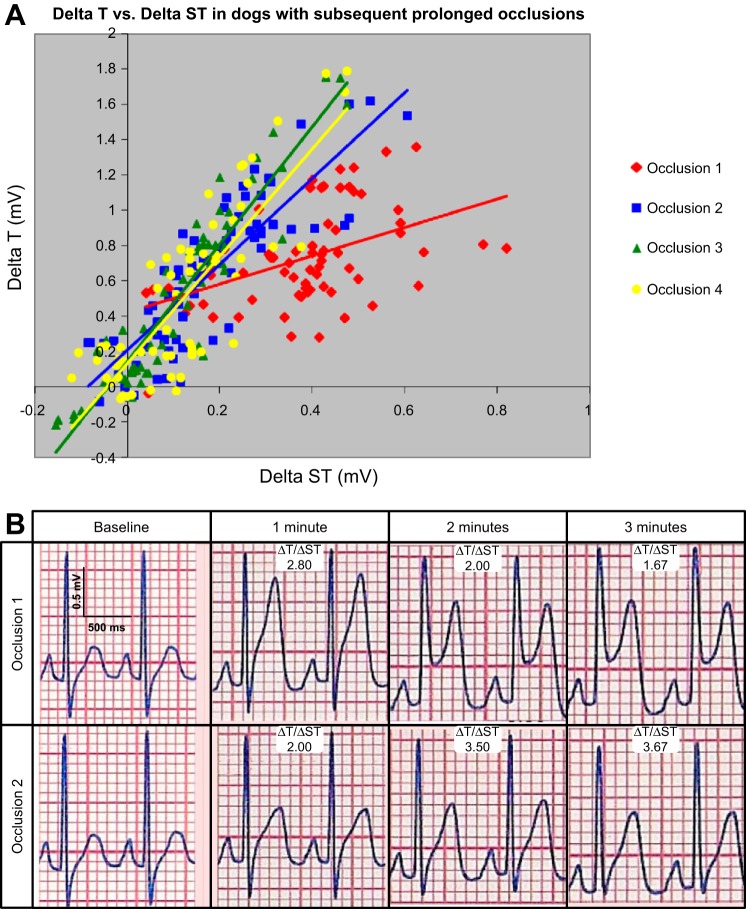
ECG measurements of experimental ischemic preconditioning in canine hearts.
During the first occlusion in the canine experiments (Fig. 3), ST-J point and T wave amplitudes behaved in line with the simulation experiments. A rapid increase of ST-J point amplitude during the 1st min of occlusion 1 was accompanied with minimal increase in the T wave amplitude (ΔT/ΔST slope = 0.81, 95% CI 0.46–1.15). This relationship reversed during the second occlusion with an increase in slope of ΔT/ΔST to 2.43 (95% CI 2.07–2.80), indicating that the T wave increased significantly more than the ST segment. This varied on an individual basis as to whether the increasing ratio was due to a greater amount of T wave increase, a lesser amount of ST segment increase, or both. ΔT/ΔST stabilized in occlusions 3 and 4 (occlusion 3 slope 3.33, 95% CI 3.00–3.66 and occlusion 4 slope 3.02, 95% CI 2.51–3.53). There was a significant interaction between the slope from occlusion 1 and each of the subsequent occlusions (P < 0.001 for all). Among occlusions 2, 3, and 4, there was an interaction between occlusions 2 and 3 (P = 0.001), but not for the other comparisons.
Fig. 3.
A: ΔT vs. ΔST in subsequent occlusions in canine preconditioning experiments. An increase in ΔT/ΔST is graphed in four subsequent occlusions during canine preconditioning. Occlusions 2-4 show a significant increase in ΔT (ΔT > ΔST) compared with occlusion 1 (P < 0.001). B: example body-surface ECGs are presented for occlusion 1 and 2 in one canine subject. There is a large amount of ST elevation and high T wave amplitude during occlusion 1. During occlusion 2, there is greater T wave amplitude increase relative to the amount of ST elevation, reflecting a greater ΔT-to-ΔST ratio.
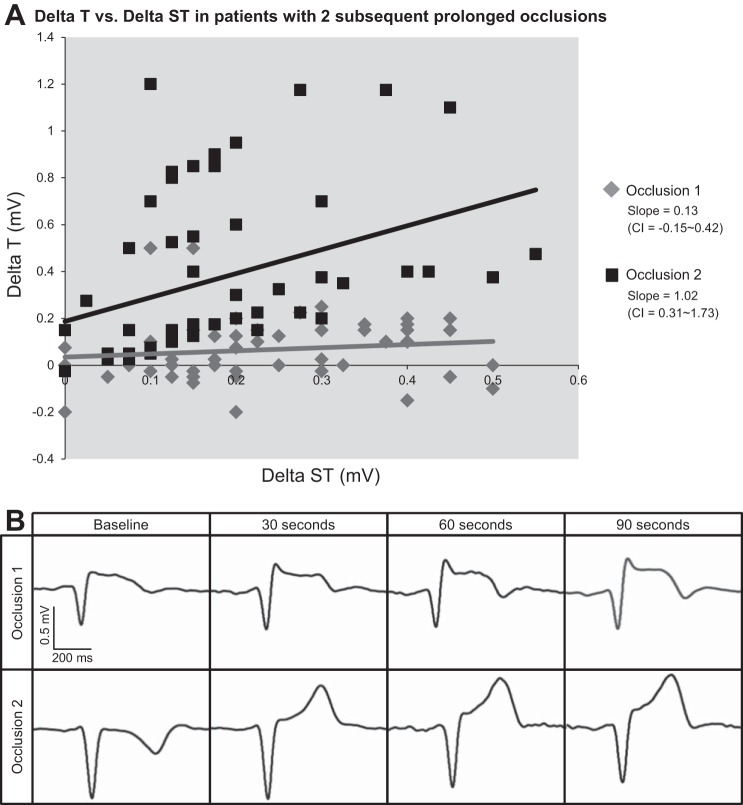
ECG measurements of ischemic preconditioning in patients.
In the patients undergoing two balloon occlusions of the LAD artery for ≥2 min (Fig. 4), similar patterns were observed as in the porcine and canine experiments. In all nine patients, ST-J point amplitude increased rapidly during the first occlusion with less increase in T wave amplitude. During occlusion 1, the slope between the ΔT wave amplitude and the ΔST-J point amplitude was 0.13 (95% CI −0.15 to 0.42), indicative of a greater increase in ST-J point amplitude than T wave amplitude. However, during the second occlusion, the slope between ΔT wave amplitude and ΔST-J point amplitude increased to 1.02 (95% CI 0.31–1.73) (P = 0.02 for interaction of occlusions 2 vs. 1). As in the canine experiments, this varied on an individual basis as to whether the increasing ΔT-to-ΔST ratio with preconditioning was due to a greater amount of T wave increase, a lesser amount of ST segment increase, or both.
Fig. 4.
A: ΔT vs. ΔST in a human preconditioning study with two subsequent occlusions. In line with observations from porcine simulation and canine experiments, a significant increase in ΔT vs. ΔST is observed in occlusion 2 compared with occlusion 1 during human preconditioning (P = 0.02). B: example ECGs of two subsequent occlusions are presented below. There is a more rapid increase in ΔT/ΔST during the second occlusion compared with the first occlusion. Although the R wave increases in occlusion 1 in this particular example, which was not the case during occlusion 2, this pattern of R wave change was not uniform throughout all patients.
DISCUSSION
The objective of this study was to test the hypothesis that the combination of an increase in T wave amplitude with decreasing ST elevation characterizes ischemic preconditioning from the cellular level in hearts of experimental animals to patient ECGs. To our knowledge, this is the first study that combines the electrophysiological processes of ischemic preconditioning in simulations, canine experiments, and a human study. Human ECGs during preconditioning were simulated by inputting AP values reported from a previous porcine experiment into a human heart and torso model (ECGSIM). We demonstrated that reduction of the AP amplitude leads to increase of the ST-J point amplitude on the body-surface ECG with minor increase of T wave amplitude. During subsequent occlusions (after preconditioning has occurred), there is more APD shortening, which in general caused an increase in T wave amplitude with less ST segment elevation as confirmed in both canine and human experiments in this study. Of note, the T wave amplitude in leads above the ischemic area is largely determined by the relative repolarization time of the ischemic area compared with the surrounding myocardium, with earlier repolarization in the ischemic area causing tall T waves and delayed repolarization in the ischemic area causing inverted T waves. Thus, if large delays in depolarization occur, then shortened APD will not result in increased T wave amplitudes. This may explain some of the interindividual variability.
Physiological relevance.
The basis for changes in the APs during ischemia have been investigated extensively. Schulz et al. found during a preconditioning protocol in swine that KATP are activated and result in increased APD shortening and significant reduction of infarct size. Mitochondrial KATP is activated by numerous metabolic processes, of which anoxia, ischemia-induced fall of intracellular ATP concentration, activation of adenosine A1 receptors, and lactate have been reported to be the most significant (16, 37, 38, 39, 43, 44). Blockade of KATP led to normal APD and no reduction of infarct size (39). This finding was confirmed by a study reported by Gross and Auchampach (16). Furthermore, Sanada et al. found that mitochondrial and sarcolemmal KATP channels play independent roles in limiting infarct size by ischemic preconditioning (37, 38).
The importance and pathophysiological basis of tall T waves is not well established. Tall peaked T waves in the absence of ST elevation have long been associated with early ischemia, and their presence has been shown to indicate a good prognosis following acute coronary occlusion (43, 44). In the late 1970s, Kleber et al. made direct simultaneous measurements of APs and extracellular electrograms on the heart surface and showed that the polarity of the local T wave was dependent on the time of repolarization of the ischemic cells relative to repolarization of surrounding normal tissue (19). Early repolarization in the ischemic area from shortened APD caused tall, peaked T waves, whereas late repolarization caused negative T waves (19). Miller and Geselowitz extended those results with computer simulations to show that those AP changes had the same effect on 12-lead body surface ECG leads that were directly over the ischemic zone (27). We confirmed the finding that tall peaked T waves may be caused by reduced APD using the computer simulation program ECGSIM (47).
Severe ischemia can affect the duration and terminal portion of the QRS complex. Weston et al. showed that QRS duration increased significantly with higher magnitudes of ST elevation in canine hearts subjected to severe ischemia, whereas QRS duration prolongation decreased in preconditioned canine hearts as shown by Weston et al. and Floyd et al. (11, 48). This may also occur in patients (10).
Species variability.
Our experiments are based on the premise that the biology of the ischemic process is similar in living myocardium of large mammalian hearts, such as the porcine and canine heart, as well as the human heart. In particular, the metabolic and electrophysiological features of ischemia are similar among these species as is the fact that each can be preconditioned with ischemia (35). However, proximal occlusion of a large coronary artery usually produces larger infarcts in the porcine than the canine heart, due to an increase in ischemic arterial flow provided by small arterial collateral connections that are common in dog hearts and absent in pig hearts. Proximal occlusion of a major coronary artery in the pig heart results in a transmural infarct involving 95% or more of the arterial bed supplied by this vessel, whereas a similar result is found in only 10% of dog hearts and occurs in the hearts that have few or no collaterals (18). The impact of collaterals, if they are abundant, is to slow the rate at which necrosis develops as well as the extent of the necrosis. The collateral flow converts a transmural area of severe ischemia in the heart to one localized in the subendocardial myocardium and sometimes midmyocardium as well. The resultant infarction is limited to this region because collateral flow is great enough to prevent death in the epicardial and a variable portion of the midmyocardial region. The surviving reversibly injured tissue in the epicardial region is ischemic and acontractile, but is not sufficiently ischemic to die.
The heart of an average young human adult has few significant collateral connections and is much more like a porcine than a canine heart. However, when coronary artery disease becomes marked and diffuse, collaterals develop in humans (35). Thus, a human heart with severe coronary artery disease is more analogous to the heart of a dog than to that of the pig. By lessening the severity of ischemia, these collaterals have significant beneficial effects relative to e.g., mortality, extent of infarction, and development of cardiac failure. However, as long as flow is diminished enough to make the tissue ischemic, collaterals do not impact the effects of ischemia on metabolism or electrophysiology. Unfortunately, there is no easy ethical way to study this collateral flow in the human heart. The easiest way to demonstrate collaterals is by injection studies of hearts removed at autopsy. Nevertheless, the fact that subendocardial infarcts are common in human hearts with extensive coronary artery disease and uncommon in the pig hearts is a finding best explained by collateral flow (18, 35).
Clinical significance.
Identifying patients with a preconditioning state may have implications for treatment decisions of patients with acute myocardial infarction. In the past 15 years, ST segment, T wave, and QRS changes have been incorporated into ECG scoring systems to rate the severity and acuteness of ischemia (1, 5, 40, 49). Sclarovsky et al. and Birnbaum et al. labeled tall T waves without any ST elevation as a sign of less severe ischemia (5, 40). The authors attributed this effect to better collateral circulation. In the light of the present study, these patients may have had intrinsic cardioprotection by preconditioning. Sclarovsky et al. and Birnbaum et al. have shown that patients with tall T waves without any ST elevation have good prognosis, which would likely be attributable to less severe ischemia due to either collaterals or intrinsic cardioprotection, or a combination of both. In addition, Anderson et al. and Wilkins et al. labeled tall T waves as a sign of early ischemia using a scoring system based on normal distribution of the T wave amplitude; however, they did not explain the tall T waves etiology on a cellular AP basis (1, 49). In the present study, in particular by simulating cellular APs in preconditioning, we have shown that one of the earliest signs of ischemia is reduction of APD, leading to an increase in T wave amplitude.
The results of this study reveal a potential ECG biomarker for identifying patients with a state of cardioprotection, which, after further investigation, might influence early decision-making regarding the treatment strategy for ST elevation myocardial infarction (STEMI) patients (2). According to current guidelines, primary PCI should be performed to restore coronary blood flow. Thrombolysis is the second choice as a revascularization therapy because coronary reflow is slower than with PCI and because the inciting pathophysiological process (including plaque rupture, intramural hemorrhage, dissection, and spasm) is not adequately treated (17, 24, 44a). In the present day, PCI is widely available in the Western World; however, rural areas and developing countries have less access to primary PCI centers. It is possible that the presence of intrinsic cardioprotection could influence the decision for transfer to a PCI center. This requires further study.
Preconditioning in dogs delays the onset of myocardial necrosis (30). If preconditioning can be directly translated to humans, infarcts developing in an area that was associated previously with ischemia would result in that myocardium dying more slowly than myocardium not previously exposed to ischemia. As a result, there may be increased time available to salvage the ischemic living myocardium. Also, infarcts preceded by intermittent coronary spasm or thrombosis, alleviated by spontaneous thrombolysis, might develop at a slower rate, which creates time for initiating the earliest possible treatment. It should be emphasized that ischemic preconditioning only delays the onset of lethal necrosis, but does not prevent infarction if reperfusion is not achieved. Only early reperfusion reduces infarct size and the risk of fatal arrhythmia (18, 35). Indeed, in a retrospective analysis of the Thrombolysis in Myocardial Infarction-IV trial, Kloner et al. found that preinfarction angina was associated with smaller infarct size and better in-hospital outcome, which they hypothesized was due to preconditioning (21).
Limitations.
This study was limited by the small number of patients, and thus the clinical applicability of findings should be viewed as preliminary. However, the concordance of significant findings between simulations, preclinical experiments and clinical studies, despite and respecting the individual differences between the three populations, supports that increasing T wave amplitude with decreasing ST elevation characterizes ischemic preconditioning. The use of simulations comes with a certain degree of uncertainty, due to the limited amount of knowledge about the individual subject's electrophysiology and to the limits of the simulation environment. In this regard educated estimations had to be made to define details such as location of the ischemic area, the decrease of the depolarization plateau, and how measurements on a porcine heart could be translated to a human model. However, if a single simulated measurement may be unreliable, the trends emerging from multiple simulations are likely to represent a realistic behavior, in particular when in agreement with other experimental data.
Although there is physiological variability in T wave amplitude among leads and patients, normal limits have been well defined in the literature, and clinically used ECG scoring systems have been developed and validated taking this physiological T wave amplitude variability into account (1, 5, 14, 25, 40, 49). Despite the fact that short (2- to 4-min) periods of transmural ischemia are not frequently seen at the time point of patient presentation, recognition of cardioprotection could have clinical importance in the setting of preinfarction angina, which has been documented in the literature (21). At this time it is unknown if our observed changes in the ΔT-to-ΔST ratio persist during prolonged ischemia. This should be the subject of future investigations. Also, future research should extend the observations in patients undergoing elective PCI to patients presenting with STEMI.
In conclusion, the body surface ECG is a biomarker of heart pathophysiology, and quantitative analysis of the ECG can be used to predict changes at the cellular level. Through a combination of simulation, preclinical, and clinical studies, we demonstrated that increasing T wave amplitude with decreased ST elevation characterizes ischemic preconditioning. This integrated ECG analysis goes beyond the standard approach to only analyze ST elevation, which has been shown to be a poor marker of preconditioning. Further research is needed to determine if this ECG sign of preconditioning could help guide reperfusion treatment decisions.
GRANTS
The development of computerized methods to facilitate in accurate data acquisition was previously supported by project TEC2010-19410 and by Ramón y Cajal program (to E. P. Pueyo), Spain. Data collection for the STAFF III dataset was supported by the American Heart Association, Durham, NC, to M. Ringhorn (account 5-21628). The canine experiments were supported by a series of grants from the National Heart, Lung, and Blood Institute. The final grants were HL-23138 and HL-27416. This project was supported in part by the Food and Drug Administration's Critical Path Initiative, and appointments to the Research Participation Program at the Center for Drug Evaluation and Research and Center for Devices and Radiological Health administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and the U.S. Food and Drug Administration.
DISCLOSURES
The mention of commercial products, their sources, or their use in connection with material reported herein is not to be construed as either an actual or implied endorsement of such products by the Department of Health and Human Services.
AUTHOR CONTRIBUTIONS
Author contributions: L.P.B.M. and D.G.S. conception and design of research; L.P.B.M., R.B.J., M.R., S.G.W., and D.G.S. performed experiments; L.P.B.M., L.G., E.P.P., D.R., R.B.J., M.R., S.G.W., G.S.W., and D.G.S. analyzed data; L.P.B.M., L.G., E.P.P., D.R., R.B.J., M.R., S.G.W., G.S.W., and D.G.S. interpreted results of experiments; L.P.B.M. and D.G.S. prepared figures; L.P.B.M. and D.G.S. drafted manuscript; L.P.B.M., L.G., E.P.P., D.R., R.B.J., M.R., S.G.W., G.S.W., and D.G.S. edited and revised manuscript; L.P.B.M., L.G., E.P.P., D.R., R.B.J., M.R., S.G.W., G.S.W., and D.G.S. approved final version of manuscript.
REFERENCES
- 1.Anderson ST, Wilkins M, Weaver WD, Selvester RH, Wagner GS. Electrocardiographic phasing of acute myocardial infarction. J Electrocardiol Suppl 25: 3–5, 1992 [DOI] [PubMed] [Google Scholar]
- 2.Antman EM, Hand M, Armstrong PW, Bates ER, Green LA, Halasyamani LK, Hochman JS, Krumholz HM, Lamas GA, Mullany CJ, Pearle DL, Sloan MA, Smith SC, Jr, Anbe DT, Kushner FG, Ornato JP, Pearle DL, Sloan MA, Jacobs AK, Adams CD, Anderson JL, Buller CE, Creager MA, Ettinger SM, Halperin JL, Hunt SA, Lytle BW, Nishimura R, Page RL, Riegel B, Tarkington LG, Yancy CW. 2007 focused update of the ACC/AHA 2004 guidelines for the management of patients with ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 51: 210–247, 2008 [DOI] [PubMed] [Google Scholar]
- 3.Badilini F, Erdem T, Zareba W, Moss AJ. ECGScan: a method for conversion of paper electrocardiographic printouts to digital electrocardiographic files. J Electrocardiol 38: 310–318, 2005 [DOI] [PubMed] [Google Scholar]
- 4.Badilini F, Sarapa N. Implications of methodological differences in digital electrocardiogram interval measurement. J Electrocardiol 39: S152–S156, 2006 [DOI] [PubMed] [Google Scholar]
- 5.Birnbaum Y, Sclarovsky S, Blum A, Mager A, Gabbay U. Prognostic significance of the initial electrocardiographic pattern in a first acute anterior wall myocardial infarction. Chest 103: 1681–1687, 1993 [DOI] [PubMed] [Google Scholar]
- 6.Chhabra L, Spodick DH. Ideal isoelectric reference segment in pericarditis: a suggested approach to a commonly prevailing clinical misconception. Cardiology 122: 210–212, 2012 [DOI] [PubMed] [Google Scholar]
- 7.Cinca J, Janse MJ, Candell J, Valle V, Durrer D. Mechanism and time course of the early electrical changes during acute coronary artery occlusion. An attempt to correlate the early ECG changes in man to the cellular electrophysiology in the pig. Chest J 77: 499–505, 1980 [DOI] [PubMed] [Google Scholar]
- 8.Cribier A, Korsatz L, Koning R, Rath P, Gamra H, Stix G, Merchant S, Chan C, Letac B. Improved myocardial ischemic response and enhanced collateral circulation with long repetitive coronary occlusion during angioplasty: a prospective study. J Am Coll Cardiol 20: 578–586, 1992 [DOI] [PubMed] [Google Scholar]
- 9.Deutsch E, Berger M, Kussmaul WG, Hirshfeld JW, Jr, Herrmann HC, Laskey WK. Adaptation to ischemia during percutaneous transluminal coronary angioplasty. Clinical, hemodynamic, and metabolic features. Circulation 82: 2044–2051, 1990 [DOI] [PubMed] [Google Scholar]
- 10.Edwards RJ, Redwood SR, Lambiase PD, Tomset E, Rakhit RD, Marber MS. Antiarrhythmic and anti-ischaemic effects of angina in patients with and without coronary collaterals. Heart 88: 604–610, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Floyd JS, Maynard C, Weston P, Johanson P, Jennings RB, Wagner GS. Effect of ischemic precondtioning and arterial collateral flow ST-segment elevation and QRS complex prolongation in a canine model of acute coronary occlusion. J Electrocardiol 42: 19–26, 2008 [DOI] [PubMed] [Google Scholar]
- 12.Galeotti L, Strauss DG, Ubachs JF, Pahlm O, Heiberg E. Development of an automated method for display of ischemic myocardium from simulated electrocardiograms. J Electrocardiol 42: 204–212, 2009 [DOI] [PubMed] [Google Scholar]
- 13.Galeotti L, van Dam PM, Loring Z, Chan D, Strauss DG. Evaluating strict and conventional left bundle branch block criteria using electrocardiographic simulations. Europace 15: 1816–1821, 2013 [DOI] [PubMed] [Google Scholar]
- 14.Gambill CL, Wilkins ML, Haisty WK, Jr, Anderson ST, Maynard C, Wagner NB, Selvester RH, Wagner GS. T wave amplitudes in normal populations. J Electrocardiol 28: 191–197, 1995 [DOI] [PubMed] [Google Scholar]
- 15.Gettes LS, Cascio WE. Effect of acute ischaemia on cardiac electrophysiology. In: The Heart and Cardiovascular System, edited Fozzard HA. New York, NY: Raven, 1992, p. 2021–2054 [Google Scholar]
- 16.Gross GJ, Auchampach JA. Blockade of ATP-sensitive potassium channels prevents myocardial preconditioning in dogs. Circ Res 70: 223–233, 1992 [DOI] [PubMed] [Google Scholar]
- 17.Hedström E, Engblom H, Frogner F, Aström-Olsson K, Ohlin H, Jovinge S, Arheden H. Infarct evolution in man studied in patients with first-time coronary occlusion in comparison to different species: implications for assessment of myocardial salvage. J Cardiovasc Magn Reson 11: 38–48, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jennings RB. Historical perspective on the pathology of myocardial ischemia/reperfusion injury. Circ Res 113: 428–438, 2013 [DOI] [PubMed] [Google Scholar]
- 19.Kléber AG, Janse MJ, van Capelle FJ, Durrer D. Mechanism and time course of S-T and T-Q segment changes during acute regional myocardial ischemia in the pig heart determined by extracellular and intracellular recordings. Circ Res 42: 603–613, 1978 [DOI] [PubMed] [Google Scholar]
- 20.Kleber AG, Janse M. Ischemia-related changes in repolarization. In: Cardiac Repolarization: Bridging Basic and Clinical Science (Contemporary Cardiology), edited by Gussak I. Totowa, NJ: Humana, 2003, p. 153–167 [Google Scholar]
- 21.Kloner RA, Shook T, Przyklenk K, Davis VG, Junio L, Matthews RV, Burstein S, Gibson M, Poole WK, Cannon CP, McGabe CH, Braunwald E. Previous angina alters in-hospital outcome in TIMI 4. A clinical correlate to preconditioning? Circulation 91: 37–45, 1995 [DOI] [PubMed] [Google Scholar]
- 22.Leesar MA, Stoddard M, Ahmed M, Broadbent J, Bolli R. Preconditioning of human myocardium with adenosine during coronary angioplasty. Circulation 95: 2500–2507, 1997 [DOI] [PubMed] [Google Scholar]
- 23.Leesar MA, Stoddard MF, Manchikalapudi S, Bolli R. Bradykinin-induced preconditioning in patients undergoing coronary angioplasty. J Am Coll Cardiol 34: 639–650, 1999 [DOI] [PubMed] [Google Scholar]
- 24.Llevadot J, Giugliano RP, McCabe CH, Cannon CP, Antman EM, Murphy S, Gibson CM. Degree of residual stenosis in the culprit coronary artery after thrombolytic administration (Thrombolysis In Myocardial Infarction [TIMI] trials). Am J Cardiol 85: 1409–1413, 2000 [DOI] [PubMed] [Google Scholar]
- 25.Macfarlane PW, Oosterom A, Pahlm O, Kligfield P, Janse M, Camm J. Appendix 1: adult normal limits. In: Comprehensive Electrocardiology, edited by Macfarlane PW. London, UK: Springer-Verlag, 2011, p. 2057–2126 [Google Scholar]
- 26.Martínez JP, Almeida R, Olmos S, Rocha AP, Laguna P. A wavelet-based ECG delineator: Evaluation on standard databases. IEEE Trans Biomed Eng 51: 570–581, 2004 [DOI] [PubMed] [Google Scholar]
- 27.Miller WT, 3rd, Geselowitz DB. Simulation studies of the electrocardiogram. II. Ischemia and infarction. Circ Res 43: 315–323, 1978 [DOI] [PubMed] [Google Scholar]
- 29.Moody G, Mark R. Development and evaluation of a 2-lead ECG analysis program. Proc Comput Cardiol, IEEE Computer Society Press, p. 39–44, 1982 [Google Scholar]
- 30.Murry CE, Jennings RB, Reimer KA. Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium. Circulation 74: 1124–1136, 1986 [DOI] [PubMed] [Google Scholar]
- 31.Nakagomi A, Saito T, Kimura Y, Tamura Y, Miura M. Altered electrical and metabolic response of reperfused myocardium to ischaemia after recovery from preceding ischaemia: evidence for ischaemia sensitised myocardium. Cardiovasc Res 27: 571–577, 1993 [DOI] [PubMed] [Google Scholar]
- 32.Patuwo T, Wagner GS, Ajijola O. Comparison of Teaching Basic Electrocardiographic Concepts with and without ECGSIM: An Interactive Program for Electrocardiography. Durham, NC: Computers in Cardiology, Duke University, 2007 [Google Scholar]
- 33.Pettersson J, Carro E, Edenbrandt L, Maynard C, Pahlm O, Ringborn M, Sörnmo L, Warren SG, Wagner GS. Spatial, individual and temporal variation of the high-frequency QRS-amplitudes in the 12 standard electrocardiographic leads. Am Heart J 139: 352–358, 2000 [DOI] [PubMed] [Google Scholar]
- 34.Pettersson J, Pahlm O, Carro E, Edenbrandt L, Ringborn M, Sörnmo L, Warren SG, Wagner GS. Changes in High-Frequency QRS components are more sensitive than ST-segment deviation for detecting acute coronary artery occlusion. J Am Coll Cardiol 36: 1827–1834, 2000 [DOI] [PubMed] [Google Scholar]
- 35.Reimer KA, Jennings Myocardial Ischemia RB. Hypoxia, infarction. In: The Heart and Cardiovascular System, edited Fozzard HA. New York, NY: Raven, 1992, p. 1875–1973 [Google Scholar]
- 36.Ringborn M, Romero D, Pueyo E, Pahlm O, Wagner GS, Laguna P, Platonov PG. Evaluation of depolarization changes during acute myocardial ischemia by analysis of QRS slopes. J Electrocardiol 44: 416–424, 2011 [DOI] [PubMed] [Google Scholar]
- 37.Sanada S, Kitakaze M, Asanuma H, Harada K, Ogita H, Node K, Takashima S, Sakata Y, Asakura M, Shinozaki Y, Mori H, Kuzuya T, Hori M. Role of mitochondrial and sarcolemmal KATP channels in ischemic preconditioning of the canine heart. Am J Physiol Heart Circ Physiol 280: H256–H263, 2001 [DOI] [PubMed] [Google Scholar]
- 38.Sanada S, Komuro I, Kitakaze M. Pathophysiology of myocardial reperfusion injury: preconditioning, postconditioning and translational aspects of protective measures. Am J Physiol Heart Circ Physiol 301: H1723–H1741, 2011 [DOI] [PubMed] [Google Scholar]
- 39.Schulz R, Rose J, Heusch G. Involvement of activation of ATP-dependent potassium channels in ischemic preconditioning in swine. Am J Physiol Heart Circ Physiol 267: H1341–H1352, 1994 [DOI] [PubMed] [Google Scholar]
- 40.Sclarovsky S, Mager A, Kusniec J, Rechavia E, Sagie A, Bassevich R, Strasberg B. Electrocardiographic classification of acute myocardial ischemia. Isr J Med Sci 26: 525–531, 1990 [PubMed] [Google Scholar]
- 41.Shattock MJ, Lawson CS, Hearse DJ, Downey JM. Electrophysiological characteristics of repetitive ischemic preconditioning in the pig heart. J Mol Cell Cardiol 28: 1339–1347, 1996 [DOI] [PubMed] [Google Scholar]
- 42.Shaw RM, Rudy Y. Electrophysiologic effects of acute myocardial ischemia. A mechanistic investigation of action potential conduction and conduction failure. Circ Res 80: 124–138, 1997 [DOI] [PubMed] [Google Scholar]
- 43.Shaw RM, Rudy Y. Electrophysiologic effects of acute myocardial ischemia: a theoretical study of altered cell excitability and action potential duration. Cardiovasc Res 35: 256–272, 1997 [DOI] [PubMed] [Google Scholar]
- 44.Tan HL, Mazón P, Verberne HJ, Sleeswijk ME, Coronel R, Opthof T, Janse MJ. Ischaemic preconditioning delays ischaemia induced cellular electrical uncoupling in rabbit myocardium by activation of ATP sensitive potassium channels. Cardiovasc Res 27: 644–651, 1993 [DOI] [PubMed] [Google Scholar]
- 44a.Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC), and the European Association for Cardio-Thoracic Surgery (EACTS); European Association for Percutaneous Cardiovascular Interventions (EAPCI), Wijns W, Kolh P, Danchin N, Di Mario C, Falk V, Folliguet T, Garg S, Huber K, James S, Knuuti J, Lopez-Sendon J, Marco J, Menicanti L, Ostojic M, Piepoli MF, Pirlet C, Pomar JL, Reifart N, Ribichini FL, Schalij MJ, Sergeant P, Serruys PW, Silber S, Sousa Uva M, Taggart D. Guidelines on Myocardial Revascularization. Eur Heart J 31: 2501–2555, 2010 [DOI] [PubMed] [Google Scholar]
- 45.Van Dam PM, Oostendorp TF, van Oosterom A. Interactive Simulation of the Activation Sequence: Replacing Effect by Cause. Hang Zou, China: Computers in Cardiology, IEEE Computer Society Press, 2011 [Google Scholar]
- 46.van Huysduynen BH, Swenne CA, Bax JJ, Bleeker GB, Draisma HH, van Erven L, Molhoek SG, van de Vooren H, van der Wall EE, Schalij MJ. Dispersion of repolarization in cardiac resynchronization therapy. Heart Rhythm 2: 1286–1293, 2005 [DOI] [PubMed] [Google Scholar]
- 47.Van Oosterom A, Oostendorp TF. ECGSIM: an interactive tool for studying the genesis of QRST waveforms. Heart 90: 165–168, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Weston P, Johanson P, Schwartz LM, Maynard C, Jennings RB, Wagner GS. The value of both ST-segment and QRS complex changes during acute coronary occlusion for prediction of reperfusion-induced myocardial salvage in a canine model. J Electrocardiol 40: 18–25, 2007 [DOI] [PubMed] [Google Scholar]
- 49.Wilkins ML, Pryor AD, Maynard C, Wagner NB, Elias WJ, Litwin PE, Pahlm O, Selvester RH, Weaver WD, Wagner GS. An electrocardiographic acuteness score for quantifying the timing of a myocardial infarction to guide decisions regarding reperfusion therapy. Am J Cardiol 75: 617–620, 1995 [DOI] [PubMed] [Google Scholar]