Abstract
Owing to the more recent positive results with the anti-CD33 immunotoxin gemtuzumab ozogamicin, therapy against acute myeloid leukemias (AMLs) targeting CD33 holds many promises. Here, CD33 and CD123 expression on AML blasts was studied by flow cytometry in a cohort of 319 patients with detailed information on French–American–British/World Health Organization (FAB/WHO) classification, cytogenetics and molecular aberrations. AMLs of 87.8% express CD33 and would therefore be targetable with anti-CD33 therapies. Additionally, 9.4% of AMLs express CD123 without concomitant CD33 expression. Thus, nearly all AMLs could be either targeted via CD33 or CD123. Simultaneous presence of both antigens was observed in 69.5% of patients. Most importantly, even AMLs with adverse cytogenetics express CD33 and CD123 levels comparable to those with favorable and intermediate subtypes. Some patient groups with unfavorable alterations, such as FMS-related tyrosine kinase 3-internal tandem duplication (FLT3-ITD) mutations, high FLT3-ITD mutant/wild-type ratios and monosomy 5 are even characterized by high expression of CD33 and CD123. In addition, blasts of patients with mutant nucleophosmin (NPM1) revealed significantly higher CD33 and CD123 expression pointing toward the possibility of minimal residual disease-guided interventions in mutated NPM1-positive AMLs. These results stimulate the development of novel concepts to redirect immune effector cells toward CD33- and CD123-expressing blasts using bi-specific antibodies or engineered T cells expressing chimeric antigen receptors.
Introduction
Acute myeloid leukemia (AML) is a very heterogeneous disease, which is characterized by the occurrence of abnormal blasts of different maturation stages in the bone marrow (BM), perturbing normal hematopoiesis. Current standard for the induction treatment of AML is a combination of cytarabine with anthracyclines, resulting in a complete remission rate of 60–80% however, 50–70% of them experience a relapse.1, 2, 3, 4 Recurrence of the disease is attributed to leukemia-initiating cells, also referred to as leukemic stem cells (LSCs), which are thought to be spared from chemotherapy and capable of reinitiating the disease.5 Thus, successful novel therapeutic strategies for the treatment of AML should aim at eradicating LSCs. In addition, alternative strategies, targeting the bulk of blasts and causing significantly fewer side effects as compared with conventional chemotherapy, are desired. Consequently, the identification of targets on the cell surface of leukemic cells, in particular LSCs, has attracted much attention.6 Among these, the CD33 and CD123 antigens are highly promising candidates for targeted therapy of AML.6
High CD33 expression on AML blasts was already reported three decades ago.7 CD33 was detected on blasts of 85–90% of patients presenting with AML as well as on normal myeloid progenitors and myelocytes.7, 8, 9, 10, 11 Interestingly, CD33 seems to be restricted to hematopoietic cells,12, 13 but absent on normal hematopoietic stem cells,14, 15, 16, 17 making it an ideal target for AML therapy. In fact, the anti-CD33 immunoconjugate gemtuzumab ozogamicin (GO; Mylotarg) was granted accelerated approval in the United States following a phase II trial reporting a 30% response rate.18, 19 However, safety concerns and initial failure to demonstrate improved efficacy led to discontinuation of commercial availability of GO.20, 21 Observed side effects were most likely caused by a dissociation of calicheamicin from the anti-CD33 monoclonal antibody.21 Subsequent clinical trials showed high efficacy of GO against acute promyelocytic leukemia (AML M3) and fractionated doses of GO in combination with chemotherapy yielded promising results in the treatment of other AML subtypes.19, 22, 23, 24, 25, 26 Moreover, multidrug resistance mechanisms were frequently observed in response to GO treatment.24, 27 Development of resistance mechanisms was reported to be reduced in preclinical studies using the anti-CD33 immunotoxin SGN-CD33A.28 Taken together, CD33 is a highly promising target in AML. Therapeutic strategies aiming at this antigen, however, need to be refined. Apart from alternative dosing regimens of GO, novel formats devoid of safety issues connected to immunotoxins, such as the recently developed bi-specific monoclonal antibodies, could increase therapeutic benefit while reducing side effects.15, 29, 30
Incorporating additional antigens, which clearly separate normal and leukemic hematopoietic stem/progenitor cells into a combined approach, could further increase efficacy and specificity of antileukemic immunotherapy. In this regard, CD123 expression was observed on cells of the myeloid lineage and on AML blasts, as well as on LSCs in 75–89% of AML patients,31, 32, 33 while being absent on normal hematopoietic stem cells.32 These observations have led to the subsequent preclinical development of antibody-based targeting strategies for CD123.34, 35 CD123 expression seems to be rather specific to hematopoietic cells, although expression on subsets of endothelial cells has been reported.36
Even though several studies have already addressed the expression of CD33 and CD123 individually in AML patient samples,7, 8, 10, 32, 33, 37 these cohorts have been rather small and restricted to subgroups with respect to French–American–British/World Health Organization (FAB/WHO) classification, cytogenetics, mutations and associated risk factors. Therefore, larger and more comprehensive studies additionally addressing the coexpression of CD33 and CD123 in AML patients are needed to set the stage for combinatorial immunotherapeutic approaches or novel trivalent constructs directing antileukemic immune effector cell activity to leukemic cells expressing these antigens.29, 38 Thus, we have analyzed the expression of CD33 in AML samples of 319 patients and CD123 alone and in combination with CD33 in AML samples of 298 of these patients by flow cytometry. In-depth analysis of CD33 and CD123 expression by AML subtypes and genetic characteristics revealed that both targets are widely expressed in AML subtypes and that their expression is equally high in patients with favorable, intermediate and poor prognosis, but particularly high in some high-risk patient groups, which are prime candidates for clinical trials.
Materials and methods
Patients
Between May 2012 and June 2013, BM (305) or peripheral blood (14) from 319 newly diagnosed AML patients (median age 63 years; range 17–88), enrolled in the Study Alliance Leukemia AML registry, was immunophenotyped in our laboratory as part of the routine diagnostic procedure for leukemias.39 These studies were approved by the ethical board of the Technische Universität Dresden. All patients gave written informed consent to participate.
Flow cytometric analysis of AML samples
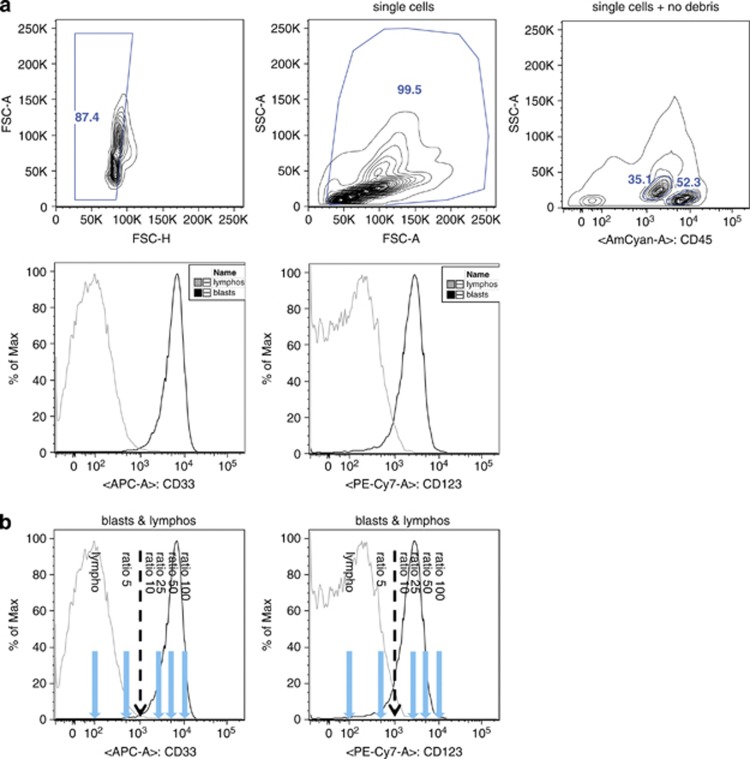
The following antibodies from the indicated suppliers were used: BD Biosciences (San Jose, CA, USA)—CD34 (8G12), CD45 (HI30), CD33 (P67.6), CD117 (104D2) and HLA-DR (L243). BioLegend (San Diego, CA, USA)—CD123 (6H6). Samples were analyzed on a FACSCanto II cytometer (BD Biosciences). Measurements and analyses were performed using FACSDiva software (BD Biosciences) and FlowJo software (Tree Star, Ashland, OR, USA). A total of 20 000 events per sample were recorded. Instrument setup including fluorescence amplification and compensation was fixed automatically applying FACSDiva compensation setup. Flow cytometer performance was checked regularly using CS&T beads (BD Biosciences). Leukemic blasts and lymphocytes were gated based on their CD45 expression and side scatter. The appropriate gate setting was verified by backgating CD34-, HLA-DR- and CD117-positive events, respectively. Blasts from AML patients were analyzed by flow cytometry (Figure 1a). The geometric mean fluorescence intensities (MFIs) of CD33 and CD123 of blasts were normalized to the MFIs of lymphocytes, which are negative for both surface markers. The resulting GeoMean ratios were applied to subsequent analyses, in which samples with a GeoMean ratio >10 were considered positive, as this represents a log-shift in the fluorescence signal compared with the negative lymphocytes (Figure 1b). For comparison, MFI ratios of CD34+ CD45dim SSClow cells of 20 healthy BM donors relative to the MFI of their lymphocytes were determined.
Figure 1.
Gating scheme of flow cytrometric analysis of CD33 and CD123 expression in AML blasts. (a) After excluding doublets and debris, lymphocytes and blasts were selected based on their SSC and CD45 expression profiles. If present, CD34 expression was used to further characterize the blast population. Thereafter, CD33 and CD123 expression was analyzed. (b) The geometric mean fluorescence intensities (MFIs) of CD33 and CD123 on blasts were normalized to the MFI of lymphocytes, which are negative for both surface markers. GeoMean ratios of 5, 10, 25, 50 and 100 are displayed in the graph together with representative FACS plots. FCS, forward scatter; SSC, side scatter.
Cytogenetic, molecular and morphologic analyses
Cytogenetic, molecular and morphologic analyses have been performed as described previously.2, 39, 40, 41, 42, 43, 44
Graphs and statistics
Graphs were prepared and statistical analyses were performed using GraphPad Prism 6 (GraphPad Software, San Diego, CA, USA). Two groups were compared with an unpaired two-tailed t-test. Multigroup comparisons were carried out with a one-way analysis of variance, followed by Tukey's multiple comparison test. Differences with a P-value of <0.05 were considered statistically significant. In the case of multigroup comparisons, multiplicity-adjusted P-values were used and reported.
Results
The majority of AMLs are positive for CD33 and CD123
In general, blast populations appeared homogenous with regard to the expression of CD33 and CD123. AML samples of 87.8% (280/319) were positive for CD33, whereas 77.9% (232/298) expressed CD123 (Figures 2a and b). Positivity for both markers was observed in 69.5% (207/298) of cases; 16.8% (50/298) of AML cases were CD33+/CD123−, whereas 9.4% (28/298) were CD33−/CD123+ (Figure 2c). The remaining 4.3% (13/298) neither expressed CD33 nor CD123. Thus, as also shown in the scatter plot in Figure 2d, CD33 and CD123 are very frequently expressed and often coexpressed on AML blasts. A significant correlation between CD33 and CD123 expression was observed according to Pearson's test (r=0.1846; P=0.0014).
Figure 2.
The majority of AMLs are positive for CD33 and CD123. (a) Pie chart showing distribution of CD33 positivity among 319 samples analyzed (GeoMean ratio blasts/lymphocytes ⩾10 was considered positive). (b) Pie chart depicting distribution of CD123 positivity among 298 samples analyzed. (c) Pie chart showing distribution of CD33 and CD123 positivity among 298 samples analyzed. (d) Scatter plot depicting distribution of CD33 and CD123 expression (GeoMean ratios blasts/lymphocytes) among 298 samples analyzed. (e) Box plots showing CD33 and CD123 expression by normal myeloid progenitors and AML blasts. P-values are based on unpaired two-tailed t-test.
Expression on AML blasts versus normal myeloid progenitors
To compare the expression of CD33 and CD123 on normal myeloid progenitor cells with AML blasts, we therefore normalized the MFI ratios of CD34+ CD45dim SSClow cells of 20 healthy BM donors to the MFI of their lymphocytes. Interestingly, leukemic blasts expressed significantly higher levels of CD33 and CD123 compared with normal myeloid progenitors (Figure 2e).
Expression of CD33 and CD123 by FAB/WHO subtype
Next, expression of CD33 and CD123 by FAB/WHO subtypes was assessed. Hundred percent of M3 and M6 AMLs were highly positive for CD33 and CD123 (Figures 3a and b and Table 1). High CD33 expression levels were observed in all AML subtypes (except for M7, N=1). FAB subtypes M2, M3, M4, M5 and M6 expressed the highest CD33 levels, whereas expression in M0, M1, M4Eo and AML subtypes with myelodysplasia-related changes (AML-MRC) was somewhat lower (Figure 3a and Table 1). When considering not the quantitative level of expression but the mere percentage of positive cases, the highest CD33 positivity of 92–100% was observed in M2, M3, M4, M4Eo and M6, whereas only 81–85% of M0 and M1 and only around 70% of M5 and AML-MRC were CD33 positive (Table 1).
Figure 3.
Expression of CD33 and CD123 by FAB/WHO subtype, cytogenetics and mutations. Box plots showing distribution of CD33 expression (a) or CD123 expression by FAB/WHO subtype (b). For further details see also Table 1. Box plots visualizing distribution of CD33 expression (c and d) or CD123 expression (e and f) based on cytogenetic features and common mutations. P-values are based on unpaired two-tailed t-test. For further details see also Table 2.
Table 1. Expression of CD33 and CD123 by FAB/WHO subtype.
| FAB/WHO subtype | Meana CD33 expression | S.d. | N | % Positive (GeoMean ratio >10) |
|---|---|---|---|---|
| CD33 | ||||
| M0 | 29.5 | 26.9 | 21 | 81.0 |
| M1 | 35.1 | 27.5 | 53 | 84.9 |
| M2 | 44.5 | 36.5 | 50 | 96.0 |
| M3 | 62.4 | 29.3 | 12 | 100.0 |
| M4 | 47.3 | 31.7 | 46 | 97.8 |
| M4Eo | 25.9 | 13.4 | 12 | 91.7 |
| M5 | 47.0 | 45.5 | 23 | 73.9 |
| M6 | 82.0 | 28.3 | 2 | 100.0 |
| M7 | 3.0 | NA | 1 | 0.0 |
| AML-MRC | 29.5 | 26.7 | 13 | 69.2 |
| CD123 | ||||
| M0 | 23.4 | 17.3 | 20 | 80.0 |
| M1 | 22.4 | 15.6 | 50 | 84.0 |
| M2 | 15.4 | 11.6 | 30 | 60.0 |
| M3 | 33.3 | 13.6 | 9 | 100.0 |
| M4 | 30.8 | 27.9 | 41 | 87.8 |
| M4Eo | 21.5 | 20.9 | 10 | 90.0 |
| M5 | 40.4 | 47.9 | 21 | 85.7 |
| M6 | 31.5 | 17.7 | 2 | 100.0 |
| M7 | 7.0 | NA | 1 | 0.0 |
| AML-MRC | 19.7 | 24.2 | 12 | 66.7 |
Abbreviations: AML, acute myeloid leukemia; FAB, French–American–British; MRC, myelodysplasia-related changes; NA, not available; WHO, World Health Organization.
Arithmetic mean of GeoMean ratios.
With regard to its levels, CD123 was highly expressed in M3, M4, M5 and M6, whereas M0, M1 and M4Eo expressed somewhat lower levels (Figure 3b and Table 1). M2 and AML-MRC had rather low CD123 levels and the only M7 sample was negative. A high percentage of CD123 positivity of 80–100% was observed in M0, M1, M3, M4, M4Eo, M5 and M6, whereas only around 60–67% of M2 and AML-MRC were CD123 positive (Table 1).
As M4 AMLs are characterized by the coexistance of a malignant monocytic population, we compared CD33 and CD123 expression in blast versus monocytic population in 23 M4 AML cases. Interestingly, the monocytic population had a significant 2.74-fold higher mean CD33 expression than the corresponding blast population, whereas there was no significant difference in CD123 expression (Supplementary Figure 1).
Expression of CD33 and CD123 by cytogenetics and molecular alterations
We further assessed the distribution of CD33 and CD123 expression based on the cytogenetic and molecular characteristics of the AML samples. Strikingly, we observed a significantly higher CD33 expression on AML blasts with FMS-related tyrosine kinase 3-internal tandem duplication (FLT3-ITD) mutations or nucleophosmin (NPM1) mutations compared with AML blasts without FLT3-ITD or NPM1 alterations (Figure 3c and Table 2). Moreover, blasts of patients with monosomy 5 showed significantly increased levels of CD33 (Figure 3d and Table 2). CD33 levels in t(15;17) blasts were nonsignificantly increased compared with negative cases, whereas t(8;21) leukemias had significantly lower CD33 expression compared with samples (Figure 3c and Table 2).
Table 2. CD33 and CD123 expression by cytogenetics and molecular alterations.
| Cytogenetics/mutation | Meana CD33 expression | S.d. | N | % Positive (GeoMean ratio >10) | P-value unpaired two-tailed t-test |
|---|---|---|---|---|---|
| CD33 | |||||
| FLT3 wt | 38.5 | 31.9 | 219 | 88.1 | |
| FLT3 mut | 55.0 | 35.6 | 58 | 93.1 | 7.19E−04 |
| NPM1 wt | 33.9 | 27.7 | 190 | 85.3 | |
| NPM1 mut | 63.3 | 37.4 | 62 | 100.0 | 2.87E−10 |
| CEBPA wt | 42.0 | 32.8 | 220 | 90.0 | |
| CEBPA mut | 32.1 | 16.1 | 14 | 92.9 | 0.26 |
| t(15;17) neg | 40.7 | 33.1 | 234 | 88.0 | |
| t(15;17) pos | 54.4 | 24.8 | 10 | 100.0 | 0.20 |
| t(8;21) neg | 41.8 | 32.8 | 242 | 88.8 | |
| t(8;21) pos | 16.2 | 9.2 | 11 | 90.9 | 0.01 |
| inv(16) neg | 41.3 | 33.1 | 241 | 88.8 | |
| inv(16) pos | 27.1 | 14.4 | 12 | 91.7 | 0.14 |
| Monosomy 5 neg | 40.0 | 32.3 | 247 | 88.7 | |
| Monosomy 5 pos | 73.0 | 35.1 | 5 | 100.0 | 0.03 |
| del(5q) neg | 41.1 | 33.1 | 235 | 88.9 | |
| del(5q) pos | 33.7 | 25.4 | 18 | 88.9 | 0.35 |
| Monosomy 7 neg | 40.7 | 32.5 | 238 | 89.1 | |
| Monosomy 7 pos | 40.4 | 35.8 | 14 | 85.7 | 0.97 |
| inv(3q) neg | 40.8 | 32.7 | 250 | 89.2 | |
| inv(3q) pos | 26.5 | 30.4 | 2 | 50.0 | NA |
| t(3;3) neg | 40.2 | 31.8 | 246 | 89.0 | |
| t(3;3) pos | 61.0 | 58.7 | 6 | 83.3 | 0.12 |
| t(6;9) neg | 40.6 | 32.8 | 250 | 88.8 | |
| t(6;9) pos | 47.0 | 8.5 | 2 | 100.0 | NA |
| t(6;11) neg | 40.7 | 32.7 | 251 | 88.8 | |
| t(6;11) pos | 41.0 | NA | 1 | 100.0 | NA |
| CD123 | |||||
| FLT3 wt | 19.8 | 14.4 | 208 | 76.9 | |
| FLT3 mut | 44.8 | 39.2 | 53 | 98.1 | 1.31E−12 |
| NPM1 wt | 20.6 | 17.2 | 179 | 76.0 | |
| NPM1 mut | 40.6 | 36.3 | 56 | 94.6 | 4.74E−08 |
| CEBPA wt | 26.3 | 26.0 | 205 | 79.0 | |
| CEBPA mut | 16.4 | 6.4 | 14 | 100.0 | 0.15 |
| t(15;17) neg | 25.3 | 25.1 | 221 | 80.1 | |
| t(15;17) pos | 33.3 | 13.6 | 9 | 100.0 | 0.34 |
| t(8;21) neg | 25.8 | 24.9 | 228 | 82.9 | |
| t(8;21) pos | 13.5 | 11.3 | 11 | 36.4 | 0.11 |
| inv(16) neg | 25.4 | 24.8 | 227 | 80.2 | |
| inv(16) pos | 21.4 | 18.8 | 12 | 91.7 | 0.58 |
| Monosomy 5 neg | 25.4 | 24.7 | 232 | 80.6 | |
| Monosomy 5 pos | 21.4 | 17.5 | 5 | 80.0 | 0.72 |
| del(5q) neg | 25.5 | 25.2 | 221 | 80.1 | |
| del(5q) pos | 21.3 | 13.4 | 18 | 83.3 | 0.48 |
| Monosomy 7 neg | 25.3 | 24.8 | 224 | 80.4 | |
| Monosomy 7 pos | 24.2 | 20.5 | 13 | 84.6 | 0.88 |
| inv(3q) neg | 25.4 | 24.6 | 235 | 80.9 | |
| inv(3q) pos | 7.5 | 4.9 | 2 | 50.0 | NA |
| t(3;3) neg | 25.6 | 24.8 | 231 | 81.0 | |
| t(3;3) pos | 14.0 | 7.2 | 6 | 66.7 | 0.26 |
| t(6;9) neg | 25.4 | 24.6 | 235 | 80.9 | |
| t(6;9) pos | 13.5 | 14.8 | 2 | 50.0 | NA |
| t(6;11) neg | 25.2 | 24.6 | 236 | 80.5 | |
| t(6;11) pos | 42.0 | NA | 1 | 100.0 | NA |
Abbreviations: CEBPA, CCAAT/enhancer-binding protein-α FLT3, FMS-related tyrosine kinase 3; mut, mutant; ITD, internal tandem duplication; NA, not available; neg, negative; NPM1, nucleophosmin; pos, positive; wt, wild type. Bold entries are statistically significant.
Arithmetic mean of GeoMean ratios.
Similarly, CD123 expression was significantly higher in AML blasts with FLT3-ITD mutations or NPM1 mutations compared with AML blasts with wild-type (wt) FLT3 or NPM1, whereas increased CD123 expression in t(15;17) samples and the lower CD123 expression in t(8;21) samples were not significant (Figure 3e and Table 2). Although blasts of most patients with monosomy 5 were CD123 positive, its expression was not as high as in the case of CD33. Interestingly, a single sample with t(6;11) showed high levels of both CD33 and CD123.
Expression of CD33 and CD123 based on FLT3 status
As blasts of patients with FLT3 mutations expressed significantly higher CD33 and CD123 protein on their cell surface than those with FLT3 wt, we dissected CD33 and CD123 expression with regard to FLT3 mutational status in greater detail. While the presence of an FLT3-ITD mutation per se is a marker for unfavorable prognosis,45 it was previously reported that, especially, a ratio of mutated FLT3 to FLT3 wt of >0.78 predicts poor outcome.42 Thus, we compared CD33 and CD123 expression in AMLs without FLT3-ITD, a mutant (mut)/wt ratio <0.78 and a ratio >0.78. Interestingly, CD33 and CD123 expression increased from wt (median 26, range 1–164) to low mut/wt ratio (median 55, range 2–103) and further to a high mut/wt ratio (median 69, range 15–148; Figure 4a). Likewise, CD123 expression increased from wt (median 16, range 2–95) to low mut/wt ratio (median 30, range 8–195) further to a high mut/wt ratio (median 46, range 11–148; Figure 4b). Because of these striking results, we analyzed additional 11 patient samples with FLT3 mut/wt ratios >0.78 from the Study Alliance Leukemia AML registry. These measurements uniformly confirmed the high CD33 and CD123 expression levels in this group (Supplementary Figure 2).
Figure 4.
Expression of CD33 and CD123 by risk group. Box plots showing expression of CD33 (a) and CD123 (b) based on FLT3 status (FLT3 wt, a mutant/wild-type ratio <0.78 and a ratio >0.78). Box plots depicting expression of CD33 (c) and CD123 (d) in AML blasts grouped by prognosis. P-values are based on one-way analysis of variance followed by Tukey's multiple comparison test.
Expression of CD33 and CD123 based on the combined FLT3-ITD and NPM1 status
It has been reported that patients with NPM1 mutation but no FLT3-ITD have a favorable prognosis.41 Thus, we compared CD33 and CD123 blast cell surface expression in this group with the other groups of patients. Patients with NPM1 mutation, irrespective of their FLT3-ITD status, had significantly higher levels of CD33 (median 59, range 10–164) than NPM1 wt/FLT3-ITD− patients (median 26, range 1–145; P-value t-test 2.96E−10; Supplementary Figure 3A). Similarly, CD123 levels were significantly higher in patients with NPM1 mutation (median 30, range 9–195) as compared with NPM1 wt/FLT3-ITD− patients (median 15, range 2–69; P-value t-test 3.84E−10; Supplementary Figure 3B).
CD33 and CD123 expression by risk group
All 236 patients with sufficient genetic information were classified into risk groups based on cytogenetic and mutation analyses according to a recommendation by the European LeukemiaNet46 with the modification that patients with an FLT3 mut/wt ratio >0.78 were added to the poor prognosis group42 (Supplementary Table 1). No significant differences were seen between the three risk groups with regard to their CD33 and CD123 levels (Figure 4c and d).
Expression of CD33 and CD123 in the CD34+ blast population only
As LSCs are contained in the CD34+CD38− or CD34+CD38+ blast population in the vast majority of AML cases,47, 48, 49, 50 we determined the expression of CD33 and CD123 in the CD34+ blast population of CD34+ leukemias as described above for overall blasts. CD34+ populations of 88.6% (249/281) of AML samples were positive for CD33, whereas 80.7% (213/264) expressed CD123 (Figures 5a and b). Positivity for both markers was observed in 73.1% (193/264) of cases, 15.5% (41/264) were CD33+/CD123−, whereas 7.6% (20/264) were CD33−/CD123+ (Figure 5c). The remaining 3.8% (10/264) neither expressed CD33 nor CD123. Thus, the blast compartment that contains LSCs expressed CD33 and/or CD123 in most AML cases.
Figure 5.
The majority of CD34+ AMLs express CD33 and CD123 in their CD34+ blast population. (a) Pie chart showing expression of CD33 in the CD34+ blast population of CD34+ leukemias (samples with a GeoMean ratio CD34+ blasts/lymphocytes ⩾10 were considered positive). (b) Pie chart depicting expression of CD123 in the CD34+ blast population of CD34+ leukemias. (c) Pie chart visualizing expression of CD33 and CD123 in the CD34+ blast population of CD34+ leukemias.
Discussion
We have analyzed the cell surface expression of CD33 and CD123 in AML blasts in a highly comprehensive manner and a larger data set compared with previous studies. We observed the expression of both markers in the vast majority of AML cases in the total blast population and in the CD34+ fraction of CD34+ AML, which is presumed to contain the LSCs in most patients.47, 48, 49 CD33 and CD123 showed a higher expression on AML blasts than on myeloid progenitors of healthy donors. The highest percentages of CD33 positivity and the highest expression levels were observed in M2, M3, M4, M5 and M6. The distribution of CD123 expression among the FAB/WHO groups was very similar to that of CD33, with the difference that CD123 expression (% and level) was lower in the M2 group. Hundred percent of M3 and M6 leukemias were CD33+ and CD123+. The fact that all M3 AMLs are CD33+ has previously been reported.11, 51 Interestingly, we observed high expression of CD33 in patients with FLT3 mut/wt ratios >0.78 and in patients with monosomy 5, with all of them being CD33+, arguing that these patients, who have a poor prognosis when treated with conventional therapy, might benefit from CD33-targeted therapies. Both groups also expressed high levels of CD123. When grouping all patients according to their prognostic outcome, no significant difference in CD33 or CD123 expression was observed between the three risk groups, suggesting that generally poor prognosis patients might profit to the same extent from targeted therapies against CD33 and CD123. While monotargeting against either CD33 or CD123 should be effective against most AML blasts and LSCs, as only around 4% of AMLs were negative for both markers, dual targeting against CD33+CD123+ double-positive cells would increase specificity and binding affinity in around 70% of cases. Our data would predict that the vast majority of patients with M3, M4, M5 and M6 leukemias would benefit from such therapies, as well as nearly all patients with FLT3-ITD and NPM1 mutations (see also Supplementary Figure), whereas M4Eo patients would benefit least from dual-targeting strategies. Such strategies can either be designed to kill only double-positive cells or to eliminate any single- and double-positive cells.52 If well tolerated, the latter strategy should be effective against 96% of AMLs. Clinical trials with GO reported high efficacy in low-risk AMLs, but not high-risk disease, which is likely explained by the preferential development of resistance mechanisms in high-risk AMLs.24, 27 Such evasion mechanisms are unlikely to occur when T cells are retargeted to leukemic cells using bi-specific antibodies. Therefore, such antibodies targeting CD33 should be more effective against high-risk leukemias as compared with GO. Moreover, targeting AMLs via cell surface proteins should be superior to targeting deregulated signaling pathways, considering the multiclonal nature of AMLs.53, 54
Of note, the definition used here for CD33 positivity of an AML sample differs from the one used in the clinic, which defines a CD33+ AML by the presence of at least 20–25% CD33+ blasts.7, 8 As the aim of this study was to quantify cell surface expression with the perspective of specific targeting, the mean expression value of the blast population is much more meaningful then the percentage of positive cells above a certain threshold. Along these lines, a recent report has described the immunophenotypic pattern of normal and malignant myeloid cells.11 However, the CD33 expression data was presented in a non-quantitative manner. Likewise, a previous study has addressed the expression of CD123 in 45 AML samples and reported its expression in all FAB subtypes, except for two cases of M7 megakaryoblastic leukemia.33 Consistently, we also observed the absence of CD123 in a single M7 sample. In contrast to our data, the corresponding data were analyzed and presented in a non-quantitative manner, which does not allow any conclusion with regard to CD123 expression levels.
In accordance with a previous report,55 we observed low CD33 expression levels in blasts of patients with t(8;21). Another recent study reported higher CD33 expression in AMLs with NPM1 mutation,56 which is confirmed by our findings. However, in the same study, no correlation between FLT3 mutations and CD33 expression was observed, which is in contrast to our results. This might be explained by the larger cohort evaluated in our study. Interestingly, Pollard et al.57 recently reported that high CD33 expression correlates with the presence of FLT3-ITD mutations in childhood AMLs. Similarly, higher CD123 expression in FLT3-ITD AMLs compared with FLT3 wt AMLs was reported previously based on flow cytometry data.58, 59 Moreover, a immunohistochemical study of CD123 expression reported correlations of CD123 expression with FLT3-ITD and NPM1 mutations, which is consistent with our data.60 Surprisingly, only 40% of AMLs were CD123+ in this study, which may be explained by the different method used to assess CD123 expression.
Highly promising results are achieved by treating chemotherapy–refractory minimal residual disease in B-cell acute lymphoblastic leukemia with the bi-specific CD3–CD19 antibody blinatumomab.61 Similarly, efficacy of bi-specific antibodies targeting AMLs via CD33 or CD123 should be assessed in patients with minimal residual disease after induction therapy. We have recently reported that NPM1 mut is suitable for detection of minimal residual disease and to be predictive of poor prognosis after relapse.40 As we have observed significantly higher CD33 and CD123 expression in AMLs with NPM1 mut as compared with those with NPM1 wt, we propose that first clinical trials should include AML patients with minimal residual disease based on positivity for NPM1 mut. Interestingly, previous studies reported the persistence of CD33 expression after relapse in CD33+ AML62, 63 and one study even reported that 45% of CD33− AML gained CD33 at relapse,63 arguing that CD33 may be an ideal target for second-line treatment, as its expression persists and might even be enhanced after chemotherapy.
Anti-CD33 therapy should efficiently target the bulk of blasts with potentially fewer side effects as compared with conventional chemotherapy. It has been debated whether or not LSCs express CD33.25 Our data on CD33 expression in the CD34+ population of CD34+ leukemias are in line with several studies, which conclude that LSCs of many AMLs express CD33 and would therefore be eradicated by anti-CD33 therapy.17, 25, 37 Likewise, our data suggest that CD123 would efficiently target blasts as well as LSCs, which is in accordance with previous reports.32, 33
In conclusion, our results suggest that tailored immunotherapies targeting CD33 and CD123 are likely to enhance treatment efficacy in the majority of AML patients.
Acknowledgments
We acknowledge the important contribution of all participating centers and physicians of the Study Alliance Leukemia registry who diagnosed patients and provided samples (see ‘Members of the Study Alliance Leukemia registry'). Support by the Flow Cytometry Service Unit of the Medizinische Klinik und Poliklinik I, University Hospital ‘Carl Gustav Carus', Technische Universität Dresden is gratefully acknowledged.
MBa, GE and AE have filed patent applications related to an antibody directed to CD33 and have founded a company. The remaining authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies this paper on Blood Cancer Journal website (http://www.nature.com/bcj)
Author contributions
AE has analyzed data and wrote the manuscript. UO acquired and analyzed data and proofread the manuscript. MK managed the data. GE, MBo, CR, MvB, MW and CT have proofread the manuscript. MvB and MW diagnosed patients. CR, CT, MBo, AF, MBa, GE and UO initiated and coordinated this study.
Supplementary Material
References
- Fernandez HF, Sun Z, Yao X, Litzow MR, Luger SM, Paietta EM, et al. Anthracycline dose intensification in acute myeloid leukemia. N Engl J Med. 2009;361:1249–1259. doi: 10.1056/NEJMoa0904544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rollig C, Bornhauser M, Thiede C, Taube F, Kramer M, Mohr B, et al. Long-term prognosis of acute myeloid leukemia according to the new genetic risk classification of the European LeukemiaNet recommendations: evaluation of the proposed reporting system. J Clin Oncol. 2011;29:2758–2765. doi: 10.1200/JCO.2010.32.8500. [DOI] [PubMed] [Google Scholar]
- Schaich M, Rollig C, Soucek S, Kramer M, Thiede C, Mohr B, et al. Cytarabine dose of 36 g/m(2) compared with 12 g/m(2) within first consolidation in acute myeloid leukemia: results of patients enrolled onto the prospective randomized AML96 study. J Clin Oncol. 2011;29:2696–2702. doi: 10.1200/JCO.2010.33.7303. [DOI] [PubMed] [Google Scholar]
- Robak T, Wierzbowska A. Current and emerging therapies for acute myeloid leukemia. Clin Ther. 2009;31 (Part 2:2349–2370. doi: 10.1016/j.clinthera.2009.11.017. [DOI] [PubMed] [Google Scholar]
- Reya T, Morrison SJ, Clarke MF, Weissman IL. Stem cells, cancer, and cancer stem cells. Nature. 2001;414:105–111. doi: 10.1038/35102167. [DOI] [PubMed] [Google Scholar]
- ten Cate B, de Bruyn M, Wei Y, Bremer E, Helfrich W. Targeted elimination of leukemia stem cells; a new therapeutic approach in hemato-oncology. Curr Drug Targets. 2010;11:95–110. doi: 10.2174/138945010790031063. [DOI] [PubMed] [Google Scholar]
- Griffin JD, Linch D, Sabbath K, Larcom P, Schlossman SF. A monoclonal antibody reactive with normal and leukemic human myeloid progenitor cells. Leuk Res. 1984;8:521–534. doi: 10.1016/0145-2126(84)90001-8. [DOI] [PubMed] [Google Scholar]
- Dinndorf PA, Andrews RG, Benjamin D, Ridgway D, Wolff L, Bernstein ID. Expression of normal myeloid-associated antigens by acute leukemia cells. Blood. 1986;67:1048–1053. [PubMed] [Google Scholar]
- Scheinberg DA, Tanimoto M, McKenzie S, Strife A, Old LJ, Clarkson BD. Monoclonal antibody M195: a diagnostic marker for acute myelogenous leukemia. Leukemia. 1989;3:440–445. [PubMed] [Google Scholar]
- Schwonzen M, Diehl V, Dellanna M, Staib P. Immunophenotyping of surface antigens in acute myeloid leukemia by flow cytometry after red blood cell lysis. Leuk Res. 2007;31:113–116. doi: 10.1016/j.leukres.2006.03.022. [DOI] [PubMed] [Google Scholar]
- Gorczyca W, Sun ZY, Cronin W, Li X, Mau S, Tugulea S. Immunophenotypic pattern of myeloid populations by flow cytometry analysis. Methods Cell Biol. 2011;103:221–266. doi: 10.1016/B978-0-12-385493-3.00010-3. [DOI] [PubMed] [Google Scholar]
- Favaloro EJ, Bradstock KF, Kabral A, Grimsley P, Zowtyj H, Zola H. Further characterization of human myeloid antigens (gp160,95; gp150; gp67): investigation of epitopic heterogeneity and non-haemopoietic distribution using panels of monoclonal antibodies belonging to CD-11b, CD-13 and CD-33. Br J Haematol. 1988;69:163–171. doi: 10.1111/j.1365-2141.1988.tb07618.x. [DOI] [PubMed] [Google Scholar]
- Hoyer JD, Grogg KL, Hanson CA, Gamez JD, Dogan A. CD33 detection by immunohistochemistry in paraffin-embedded tissues: a new antibody shows excellent specificity and sensitivity for cells of myelomonocytic lineage. Am J Clin Pathol. 2008;129:316–323. doi: 10.1309/E36008Y2H08Q1AYY. [DOI] [PubMed] [Google Scholar]
- Andrews RG, Takahashi M, Segal GM, Powell JS, Bernstein ID, Singer JW. The L4F3 antigen is expressed by unipotent and multipotent colony-forming cells but not by their precursors. Blood. 1986;68:1030–1035. [PubMed] [Google Scholar]
- Arndt C, von Bonin M, Cartellieri M, Feldmann A, Koristka S, Michalk I, et al. Redirection of T cells with a first fully humanized bispecific CD33–CD3 antibody efficiently eliminates AML blasts without harming hematopoietic stem cells. Leukemia. 2013;27:964–967. doi: 10.1038/leu.2013.18. [DOI] [PubMed] [Google Scholar]
- Robertson MJ, Soiffer RJ, Freedman AS, Rabinowe SL, Anderson KC, Ervin TJ, et al. Human bone marrow depleted of CD33-positive cells mediates delayed but durable reconstitution of hematopoiesis: clinical trial of MY9 monoclonal antibody-purged autografts for the treatment of acute myeloid leukemia. Blood. 1992;79:2229–2236. [PubMed] [Google Scholar]
- Hauswirth AW, Florian S, Printz D, Sotlar K, Krauth MT, Fritsch G, et al. Expression of the target receptor CD33 in CD34+/CD38−/CD123+ AML stem cells. Eur J Clin Invest. 2007;37:73–82. doi: 10.1111/j.1365-2362.2007.01746.x. [DOI] [PubMed] [Google Scholar]
- Bross PF, Beitz J, Chen G, Chen XH, Duffy E, Kieffer L, et al. Approval summary: gemtuzumab ozogamicin in relapsed acute myeloid leukemia. Clin Cancer Res. 2001;7:1490–1496. [PubMed] [Google Scholar]
- Sievers EL, Larson RA, Stadtmauer EA, Estey E, Lowenberg B, Dombret H, et al. Efficacy and safety of gemtuzumab ozogamicin in patients with CD33-positive acute myeloid leukemia in first relapse. J Clin Oncol. 2001;19:3244–3254. doi: 10.1200/JCO.2001.19.13.3244. [DOI] [PubMed] [Google Scholar]
- Rowe JM, Lowenberg B. Gemtuzumab ozogamicin in acute myeloid leukemia: a remarkable saga about an active drug. Blood. 2013;121:4838–4841. doi: 10.1182/blood-2013-03-490482. [DOI] [PubMed] [Google Scholar]
- Rajvanshi P, Shulman HM, Sievers EL, McDonald GB. Hepatic sinusoidal obstruction after gemtuzumab ozogamicin (Mylotarg) therapy. Blood. 2002;99:2310–2314. doi: 10.1182/blood.v99.7.2310. [DOI] [PubMed] [Google Scholar]
- Castaigne S, Pautas C, Terre C, Raffoux E, Bordessoule D, Bastie JN, et al. Effect of gemtuzumab ozogamicin on survival of adult patients with de-novo acute myeloid leukaemia (ALFA-0701): a randomised, open-label, phase 3 study. Lancet. 2012;379:1508–1516. doi: 10.1016/S0140-6736(12)60485-1. [DOI] [PubMed] [Google Scholar]
- Lo-Coco F, Cimino G, Breccia M, Noguera NI, Diverio D, Finolezzi E, et al. Gemtuzumab ozogamicin (Mylotarg) as a single agent for molecularly relapsed acute promyelocytic leukemia. Blood. 2004;104:1995–1999. doi: 10.1182/blood-2004-04-1550. [DOI] [PubMed] [Google Scholar]
- Taksin AL, Legrand O, Raffoux E, de Revel T, Thomas X, Contentin N, et al. High efficacy and safety profile of fractionated doses of Mylotarg as induction therapy in patients with relapsed acute myeloblastic leukemia: a prospective study of the alfa group. Leukemia. 2007;21:66–71. doi: 10.1038/sj.leu.2404434. [DOI] [PubMed] [Google Scholar]
- Walter RB, Appelbaum FR, Estey EH, Bernstein ID. Acute myeloid leukemia stem cells and CD33-targeted immunotherapy. Blood. 2012;119:6198–6208. doi: 10.1182/blood-2011-11-325050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnett AK, Hills RK, Hunter AE, Milligan D, Kell WJ, Wheatley K, et al. The addition of gemtuzumab ozogamicin to low-dose Ara-C improves remission rate but does not significantly prolong survival in older patients with acute myeloid leukaemia: results from the LRF AML14 and NCRI AML16 pick-a-winner comparison. Leukemia. 2013;27:75–81. doi: 10.1038/leu.2012.229. [DOI] [PubMed] [Google Scholar]
- Walter RB, Gooley TA, van der Velden VH, Loken MR, van Dongen JJ, Flowers DA, et al. CD33 expression and P-glycoprotein-mediated drug efflux inversely correlate and predict clinical outcome in patients with acute myeloid leukemia treated with gemtuzumab ozogamicin monotherapy. Blood. 2007;109:4168–4170. doi: 10.1182/blood-2006-09-047399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kung Sutherland MS, Walter RB, Jeffrey SC, Burke PJ, Yu C, Kostner H, et al. SGN-CD33A: a novel CD33-targeting antibody–drug conjugate using a pyrrolobenzodiazepine dimer is active in models of drug-resistant AML. Blood. 2013;122:1455–1463. doi: 10.1182/blood-2013-03-491506. [DOI] [PubMed] [Google Scholar]
- Arndt C, Feldmann A, von Bonin M, Cartellieri M, Ewen EM, Koristka S, et al. Costimulation improves the killing capability of T cells redirected to tumor cells expressing low levels of CD33: description of a novel modular targeting system. Leukemia. 2013;28:59–69. doi: 10.1038/leu.2013.243. [DOI] [PubMed] [Google Scholar]
- Aigner M, Feulner J, Schaffer S, Kischel R, Kufer P, Schneider K, et al. T lymphocytes can be effectively recruited for ex vivo and in vivo lysis of AML blasts by a novel CD33/CD3-bispecific BiTE antibody construct. Leukemia. 2013;27:1107–1115. doi: 10.1038/leu.2012.341. [DOI] [PubMed] [Google Scholar]
- Hwang K, Park CJ, Jang S, Chi HS, Kim DY, Lee JH, et al. Flow cytometric quantification and immunophenotyping of leukemic stem cells in acute myeloid leukemia. Ann Hematol. 2012;91:1541–1546. doi: 10.1007/s00277-012-1501-7. [DOI] [PubMed] [Google Scholar]
- Jordan CT, Upchurch D, Szilvassy SJ, Guzman ML, Howard DS, Pettigrew AL, et al. The interleukin-3 receptor alpha chain is a unique marker for human acute myelogenous leukemia stem cells. Leukemia. 2000;14:1777–1784. doi: 10.1038/sj.leu.2401903. [DOI] [PubMed] [Google Scholar]
- Munoz L, Nomdedeu JF, Lopez O, Carnicer MJ, Bellido M, Aventin A, et al. Interleukin-3 receptor alpha chain (CD123) is widely expressed in hematologic malignancies. Haematologica. 2001;86:1261–1269. [PubMed] [Google Scholar]
- Jin L, Lee EM, Ramshaw HS, Busfield SJ, Peoppl AG, Wilkinson L, et al. Monoclonal antibody-mediated targeting of CD123, IL-3 receptor alpha chain, eliminates human acute myeloid leukemic stem cells. Cell Stem Cell. 2009;5:31–42. doi: 10.1016/j.stem.2009.04.018. [DOI] [PubMed] [Google Scholar]
- Stein C, Kellner C, Kugler M, Reiff N, Mentz K, Schwenkert M, et al. Novel conjugates of single-chain Fv antibody fragments specific for stem cell antigen CD123 mediate potent death of acute myeloid leukaemia cells. Br J Haematol. 2010;148:879–889. doi: 10.1111/j.1365-2141.2009.08033.x. [DOI] [PubMed] [Google Scholar]
- Gilliet M, Conrad C, Geiges M, Cozzio A, Thurlimann W, Burg G, et al. Psoriasis triggered by toll-like receptor 7 agonist imiquimod in the presence of dermal plasmacytoid dendritic cell precursors. Arch Dermatol. 2004;140:1490–1495. doi: 10.1001/archderm.140.12.1490. [DOI] [PubMed] [Google Scholar]
- Florian S, Sonneck K, Hauswirth AW, Krauth MT, Schernthaner GH, Sperr WR, et al. Detection of molecular targets on the surface of CD34+/CD38− stem cells in various myeloid malignancies. Leuk Lymphoma. 2006;47:207–222. doi: 10.1080/10428190500272507. [DOI] [PubMed] [Google Scholar]
- Kugler M, Stein C, Kellner C, Mentz K, Saul D, Schwenkert M, et al. A recombinant trispecific single-chain Fv derivative directed against CD123 and CD33 mediates effective elimination of acute myeloid leukaemia cells by dual targeting. Br J Haematol. 2010;150:574–586. doi: 10.1111/j.1365-2141.2010.08300.x. [DOI] [PubMed] [Google Scholar]
- Oelschlaegel U, Mohr B, Schaich M, Schakel U, Kroschinsky F, Illmer T, et al. HLA-DRneg patients without acute promyelocytic leukemia show distinct immunophenotypic, genetic, molecular, and cytomorphologic characteristics compared to acute promyelocytic leukemia. Cytometry B. 2009;76:321–327. doi: 10.1002/cyto.b.20475. [DOI] [PubMed] [Google Scholar]
- Shayegi N, Kramer M, Bornhauser M, Schaich M, Schetelig J, Platzbecker U, et al. The level of residual disease based on mutant NPM1 is an independent prognostic factor for relapse and survival in AML. Blood. 2013;122:83–92. doi: 10.1182/blood-2012-10-461749. [DOI] [PubMed] [Google Scholar]
- Thiede C, Koch S, Creutzig E, Steudel C, Illmer T, Schaich M, et al. Prevalence and prognostic impact of NPM1 mutations in 1485 adult patients with acute myeloid leukemia (AML) Blood. 2006;107:4011–4020. doi: 10.1182/blood-2005-08-3167. [DOI] [PubMed] [Google Scholar]
- Thiede C, Steudel C, Mohr B, Schaich M, Schakel U, Platzbecker U, et al. Analysis of FLT3-activating mutations in 979 patients with acute myelogenous leukemia: association with FAB subtypes and identification of subgroups with poor prognosis. Blood. 2002;99:4326–4335. doi: 10.1182/blood.v99.12.4326. [DOI] [PubMed] [Google Scholar]
- Vardiman JW, Thiele J, Arber DA, Brunning RD, Borowitz MJ, Porwit A, et al. The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood. 2009;114:937–951. doi: 10.1182/blood-2009-03-209262. [DOI] [PubMed] [Google Scholar]
- Mohr B, Schetelig J, Schafer-Eckart K, Schmitz N, Hanel M, Rosler W, et al. Impact of allogeneic haematopoietic stem cell transplantation in patients with abnl(17p) acute myeloid leukaemia. Br J Haematol. 2013;161:237–244. doi: 10.1111/bjh.12253. [DOI] [PubMed] [Google Scholar]
- Kottaridis PD, Gale RE, Frew ME, Harrison G, Langabeer SE, Belton AA, et al. The presence of a FLT3 internal tandem duplication in patients with acute myeloid leukemia (AML) adds important prognostic information to cytogenetic risk group and response to the first cycle of chemotherapy: analysis of 854 patients from the United Kingdom Medical Research Council AML 10 and 12 trials. Blood. 2001;98:1752–1759. doi: 10.1182/blood.v98.6.1752. [DOI] [PubMed] [Google Scholar]
- Dohner H, Estey EH, Amadori S, Appelbaum FR, Buchner T, Burnett AK, et al. Diagnosis and management of acute myeloid leukemia in adults: recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood. 2010;115:453–474. doi: 10.1182/blood-2009-07-235358. [DOI] [PubMed] [Google Scholar]
- Eppert K, Takenaka K, Lechman ER, Waldron L, Nilsson B, van Galen P, et al. Stem cell gene expression programs influence clinical outcome in human leukemia. Nat Med. 2011;17:1086–1093. doi: 10.1038/nm.2415. [DOI] [PubMed] [Google Scholar]
- Goardon N, Marchi E, Atzberger A, Quek L, Schuh A, Soneji S, et al. Coexistence of LMPP-like and GMP-like leukemia stem cells in acute myeloid leukemia. Cancer Cell. 2011;19:138–152. doi: 10.1016/j.ccr.2010.12.012. [DOI] [PubMed] [Google Scholar]
- Taussig DC, Miraki-Moud F, Anjos-Afonso F, Pearce DJ, Allen K, Ridler C, et al. Anti-CD38 antibody-mediated clearance of human repopulating cells masks the heterogeneity of leukemia-initiating cells. Blood. 2008;112:568–575. doi: 10.1182/blood-2007-10-118331. [DOI] [PubMed] [Google Scholar]
- Taussig DC, Vargaftig J, Miraki-Moud F, Griessinger E, Sharrock K, Luke T, et al. Leukemia-initiating cells from some acute myeloid leukemia patients with mutated nucleophosmin reside in the CD34(−) fraction. Blood. 2010;115:1976–1984. doi: 10.1182/blood-2009-02-206565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis RE, Cruse JM, Webb RN, Sanders CM, Beason K. Contrasting antigenic maturation patterns in M0–M2 versus M3 acute myeloid leukemias. Exp Mol Pathol. 2007;83:269–273. doi: 10.1016/j.yexmp.2007.05.003. [DOI] [PubMed] [Google Scholar]
- Schubert I, Stein C, Fey GH. Dual-targeting for the elimination of cancer cells with increased selectivity. Antibodies. 2012;1:2–18. [Google Scholar]
- Ding L, Ley TJ, Larson DE, Miller CA, Koboldt DC, Welch JS, et al. Clonal evolution in relapsed acute myeloid leukaemia revealed by whole-genome sequencing. Nature. 2012;481:506–510. doi: 10.1038/nature10738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welch JS, Ley TJ, Link DC, Miller CA, Larson DE, Koboldt DC, et al. The origin and evolution of mutations in acute myeloid leukemia. Cell. 2012;150:264–278. doi: 10.1016/j.cell.2012.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoury H, Dalal BI, Nantel SH, Horsman DE, Lavoie JC, Shepherd JD, et al. Correlation between karyotype and quantitative immunophenotype in acute myelogenous leukemia with t(8;21) Mod Pathol. 2004;17:1211–1216. doi: 10.1038/modpathol.3800168. [DOI] [PubMed] [Google Scholar]
- De Propris MS, Raponi S, Diverio D, Milani ML, Meloni G, Falini B, et al. High CD33 expression levels in acute myeloid leukemia cells carrying the nucleophosmin (NPM1) mutation. Haematologica. 2011;96:1548–1551. doi: 10.3324/haematol.2011.043786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard JA, Alonzo TA, Loken M, Gerbing RB, Ho PA, Bernstein ID, et al. Correlation of CD33 expression level with disease characteristics and response to gemtuzumab ozogamicin containing chemotherapy in childhood AML. Blood. 2012;119:3705–3711. doi: 10.1182/blood-2011-12-398370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riccioni R, Diverio D, Riti V, Buffolino S, Mariani G, Boe A, et al. Interleukin (IL)-3/granulocyte macrophage-colony stimulating factor/IL-5 receptor alpha and beta chains are preferentially expressed in acute myeloid leukaemias with mutated FMS-related tyrosine kinase 3 receptor. Br J Haematol. 2009;144:376–387. doi: 10.1111/j.1365-2141.2008.07491.x. [DOI] [PubMed] [Google Scholar]
- Riccioni R, Pelosi E, Riti V, Castelli G, Lo-Coco F, Testa U. Immunophenotypic features of acute myeloid leukaemia patients exhibiting high FLT3 expression not associated with mutations. Br J Haematol. 2011;153:33–42. doi: 10.1111/j.1365-2141.2011.08577.x. [DOI] [PubMed] [Google Scholar]
- Rollins-Raval M, Pillai R, Warita K, Mitsuhashi-Warita T, Mehta R, Boyiadzis M, et al. CD123 immunohistochemical expression in acute myeloid leukemia is associated with underlying FLT3-ITD and NPM1 mutations. Appl Immunohistochem Mol Morphol. 2013;21:212–217. doi: 10.1097/PAI.0b013e318261a342. [DOI] [PubMed] [Google Scholar]
- Topp MS, Kufer P, Gokbuget N, Goebeler M, Klinger M, Neumann S, et al. Targeted therapy with the T-cell-engaging antibody blinatumomab of chemotherapy-refractory minimal residual disease in B-lineage acute lymphoblastic leukemia patients results in high response rate and prolonged leukemia-free survival. J Clin Oncol. 2011;29:2493–2498. doi: 10.1200/JCO.2010.32.7270. [DOI] [PubMed] [Google Scholar]
- Chevallier P, Robillard N, Ayari S, Guillaume T, Delaunay J, Mechinaud F, et al. Persistence of CD33 expression at relapse in CD33(+) acute myeloid leukaemia patients after receiving Gemtuzumab in the course of the disease. Br J Haematol. 2008;143:744–746. doi: 10.1111/j.1365-2141.2008.07153.x. [DOI] [PubMed] [Google Scholar]
- Baer MR, Stewart CC, Dodge RK, Leget G, Sule N, Mrozek K, et al. High frequency of immunophenotype changes in acute myeloid leukemia at relapse: implications for residual disease detection (Cancer and Leukemia Group B Study 8361) Blood. 2001;97:3574–3580. doi: 10.1182/blood.v97.11.3574. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.