Abstract
Extra pontine myelinolysis (EPM) is a form of osmotic demyelination syndrome, characterized by the presence of signal alterations in varied sites in the brain other than the pons. When caudate and putamen are involved, it results in a constellation of extra pyramidal signs and symptoms resembling parkinsonism. Here we report a case of this unique syndrome presenting with features of parkinsonism which was successfully treated with dopaminergic drugs.
Keywords: osmotic demyelination, cxtrapontine myelinolysis (EPM), parkinsonism, hyponatremia
Case report
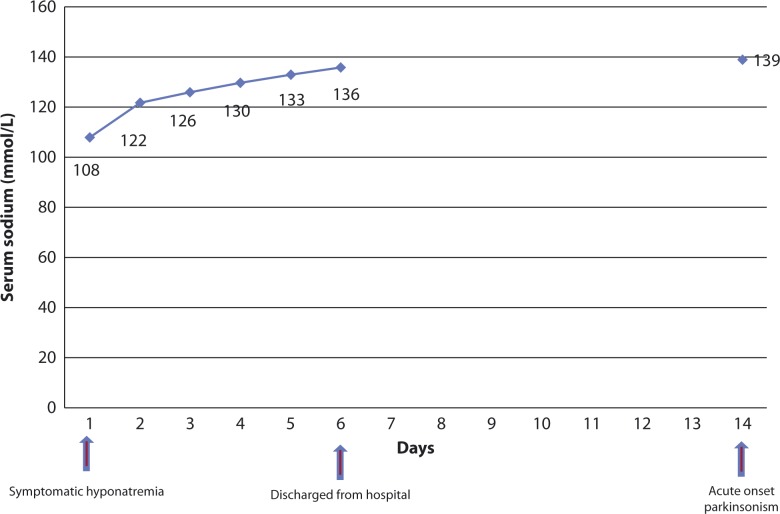
A 52-year-old gentleman, with a history of hypertension for the last two years on losartan-hydrochlorothiazide, presented with a history of slowness of all movements for last three days, including slow gait, mild tremor of both hands, slurred speech, excessive salivation and drooling. He also had difficulty in remembering recent events and a feeling of lack of interest. He was admitted two weeks prior to the onset of symptoms with recurrent vomiting and confusion. Serum Na+ level during that admission was 108 mmol/L (Fig. 1). The other electrolytes including serum K+ were normal. The patient was treated using IV fluids including 3% saline for symptomatic hyponatremia. Serum Na+ rose to 122 mmol/L on day two, becoming 130 mmol/L by day four. There was no preceding history of encephalitis or prior use of antipsychotic or antiemetic medications or any exposure to toxic substances.
Figure 1.
Changes in serum sodium with relation to the onset of symptoms of EPM.
On examination, his vitals were stable with no postural drop in blood pressure. He had an expressionless face and reduced blink rate. He was apathetic and bradyphrenic. Speech was hypophonic and saccadic eye movements were slow. Ocular fundi were normal and there were no Keyser Fleischer rings. He had cogwheel rigidity of all limbs and resting tremor of both the hands. Deep tendon reflexes were normal but plantar reflexes were extensor bilaterally. He had a short shuffling gait and moderate bradykinesia. The rest of neurological and system examinations were within normal limits.
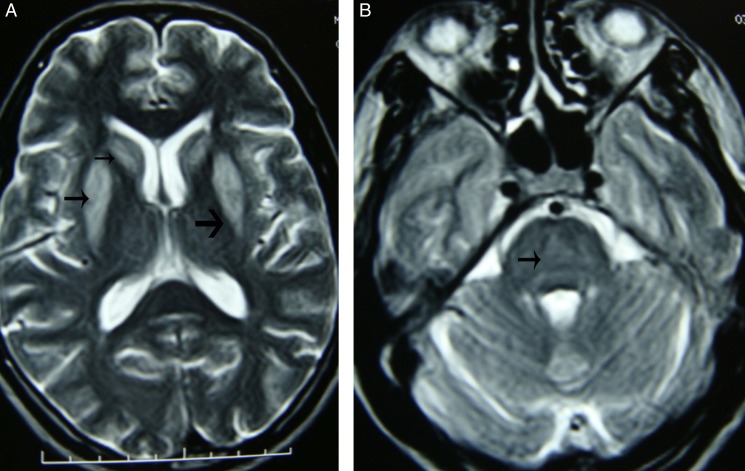
Investigations including routine hemogram, blood sugar, calcium, liver, renal function and thyroid function tests were normal. Serum Na+ was 139 mmol/L. Cerebrospinal fluid (CSF) study was unremarkable. Magnetic resonance imaging (MRI) of brain showed signal alteration involving bilateral caudate nuclei and putamen in a symmetric fashion with sparing of globus pallidus (Fig. 2: Panel A). The pons and the rest of the brain stem and cerebellum did not show any abnormality (Fig. 2: Panel B).
Figure 2.
Panel A. tbl2 weighted MRI shows symmetrical bilateral hyperintensities in caudate nucleus and putamen (small arrow) with sparing of globus pallidus (broad arrow).
The characteristic appearance on MRI, on the background history of hyponatremia with subsequent correction preceding the clinical syndrome, was diagnostic of extra pontine myelinolysis (EPM). The patient was started on levodopa/Carbidopa and Ropinirole with which he showed improvement in the period of two weeks. The treatment was continued for six months and in subsequent follow up, he had complete recovery with no residual signs and symptoms of parkinsonism. Follow up MRI could not be taken due to financial constraints of the patient.
Discussion
Osmotic demyelination syndromes (ODS) includes central pontine myelinolysis (CPM) and extra pontine myelinolysis (EPM). Isolated EPM is the least common form of ODS, (1) described in only 22% of myelinolysis syndromes. (2) One of the precipitating factors for these syndromes is the rapid osmotic shift commonly occurring during correction of sodium abnormality especially in those with severe and prolonged hyponatremia. It can also occur with normal or elevated serum sodium levels, (3) Risk factors for EPM include alcoholism, malnutrition, prolonged diuretic use (as was in this case), immunosuppression, post-liver transplant and post–urological surgery. (1,4)
It typically occurs between 7–14 days after osmotic shift with a characteristic biphasic clinical course. Initially, the patient presents with symptomatic hyponatremia which improves albeit transiently following sodium correction. This is a followed by a second phase characterized by the features of EPM. (5) Extra-pontine myelinolysis may manifest in a number of different ways, mainly presenting as mutism, catatonia, ataxia, movement disorders such as dystonia, tremor and choreoathetosis. (1) It can also affect emotional and cognitive functions.
Radiologically, EPM is characterized by bilaterally symmetrical signal changes of the caudate and putamen with sparing of the globus pallidus. In addition, the corticospinal tract, cerebellum and subcortical white matter may be affected. (1,4) It is unclear why the lesions are confined to these regions but it is postulated that the maximal admixture of grey-white matter in these regions make them more susceptible to changes in osmolality. (1) The lesions will appear hypointense on tbl1 image and hyper intense on tbl2 image; and are non-contrast enhancing. (6,7) MRI changes may be delayed and its severity is not prognostic.
Microscopically myelin alone is involved with sparing of the axons and without any obvious inflammatory infiltrate. (1,8) So, in patients with isolated EPM presenting as parkinsonism, prompt improvement is seen, if identified and treated early.
The diagnosis should be considered in a patient who has failed to recover as expected, after a severe illness requiring intravenous fluids and subsequently manifesting with movement disorders or parkinsonism, even if imaging studies are unremarkable. It should be remembered that a rise in serum sodium need not be in excess of 10 mmol/L/day for the condition to develop and there may not be a ‘safe’ limit for the rate of Na+ rise. MRI is the imaging modality of choice. Isolated EPM causing parkinsonism has good prognosis, unlike other forms of ODS.
Treatment is mainly supportive. Symptoms of parkinsonism are treated with dopaminergic drugs. (9) Isolated case reports have shown the usefulness of steroids, immunoglobulin and thyrotropin releasing hormone. (1) Few case reports and animal studies have shown benefit with the reintroduction of hyponatremia. (10) EPM, in contrast to other causes of secondary parkinsonism, responds well to treatment with dopaminergic drugs with only a few cases ending up in progressive parkinsonism. (11)
Conclusion
Osmotic demyelination is not confined to the pons alone and can present with symptoms and signs other than the classic quadriparesis and loss of consciousness. Extra pontine myelinolysis causing acute onset parkinsonism is a rare manifestation of osmotic demyelination syndrome. It occurs due to osmotic changes and can be prevented by slow correction of hyponatremia. EPM presenting as parkinsonism represents a treatable manifestation of osmotic demyelination syndrome. Clinicians should be aware of this unique condition as a reversible cause of parkinsonism.
References
- 1.Martin RJ. Central pontine and extrapontine myelinolysis: the osmotic demyelination syndromes. J Neurol Practice. 2004;75(3):iii22–iii28. doi: 10.1136/jnnp.2004.045906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gocht A, Colmant HJ. Central pontine and extrapontine myelinolysis: a report of 58 cases. Clin Neuropathol. 1987 Nov;6(6):262–270. [PubMed] [Google Scholar]
- 3.Brown WD. Osmotic demyelination disorders: central pontine and extrapontine myelinolysis. Curr Opin Neurol. 2000;13(6):691–697. doi: 10.1097/00019052-200012000-00014. [DOI] [PubMed] [Google Scholar]
- 4.Sajith J, Ditchfield A, Katifi HA. Extrapontine myelinolysis presenting as acute parkinsonism. BMC Neurol. 2006;6:33. doi: 10.1186/1471-2377-6-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ruzek KA, Campeau NG, Miller GM. Early diagnosis of central pontine myelinolysis with diffusion-weighted imaging. AJNR Am J Neuroradiol. 2004 Feb;25(2):210–213. [PMC free article] [PubMed] [Google Scholar]
- 6.Sharma P, Eesa M, Scott JN. Toxic and acquired metabolic encephalopathies: MRI appearance. AJR Am J Roentgenol. 2009 Sep;193(3):879–886. doi: 10.2214/AJR.08.2257. [DOI] [PubMed] [Google Scholar]
- 7.Seiser A, Schwarz S, Aichinger-Steiner MM, Funk G, Schnider P, Brainin M. Parkinsonism and dystonia in central pontine and extrapontine myelinolysis. J Neurol Neurosurg Psychiatry. 1998 Jul;65(1):119–121. doi: 10.1136/jnnp.65.1.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Imam YZ, Saqqur M, Alhail H, Deleu D. Extrapontine myelinolysis-induced parkinsonism in a patient with adrenal crisis. Case Rep Neurol Med. 2012;2012:327058. doi: 10.1155/2012/327058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gujjar A, Al-Mamari A, Jacob PC, Jain R, Balkhair A, Al-Asmi A. Extrapontine myelinolysis as presenting manifestation of adrenal failure: a case report. J Neurol Sci. 2010 Mar 15;290(1-2):169–171. doi: 10.1016/j.jns.2009.11.012. [DOI] [PubMed] [Google Scholar]
- 10.Oya S, Tsutsumi K, Ueki K, Kirino T. Reinduction of hyponatremia to treat central pontine myelinolysis. Neurology. 2001 Nov 27;57(10):1931–1932. doi: 10.1212/wnl.57.10.1931. [DOI] [PubMed] [Google Scholar]
- 11.Post B, van Gool WA, Tijssen MA. Transient parkinsonism in isolated extrapontine myelinolysis. Neurol Sci. 2009 Aug;30(4):325–328. doi: 10.1007/s10072-009-0088-9. [DOI] [PMC free article] [PubMed] [Google Scholar]