Abstract
Dengue is the most significant arthropod-borne viral infection of humans. Persons infected with dengue viruses (DENV) have subclinical or clinically apparent infections ranging from undifferentiated fever to dengue hemorrhagic fever/shock syndrome. Although recent studies estimated that the Indian subcontinent has the greatest burden of DENV infection and disease worldwide, we do not have reliable, population-based estimates of the incidence of infection and disease in this region. The goal of this study was to follow-up a cohort of 800 children living in a heavily urbanized area of Colombo, Sri Lanka to obtain accurate estimates of the incidence of DENV infection and disease. Annual blood samples were obtained from all children to estimate dengue seroprevalence at enrollment and to identify children exposed to new DENV infections during the study year. Blood was also obtained from any child in whom fever developed over the course of the study year to identify clinically apparent DENV infections. At enrollment, dengue seroprevalence was 53.07%, which indicated high transmission in this population. Over the study year, the incidence of DENV infection and disease were 8.39 (95% confidence interval = 6.56–10.53) and 3.38 (95% confidence interval = 2.24–4.88), respectively, per 100 children per year. The ratio of clinically inapparent to apparent infections was 1.48. These results will be useful for obtaining more accurate estimates of the burden of dengue in the region and for making decisions about testing and introduction of vaccines.
Introduction
Dengue is caused by four related mosquito-borne dengue viruses (DENV1–4), which are endemic to many tropical and subtropical regions of the world. Most persons infected with DENV are asymptomatic or show development of a febrile illness known as dengue fever, but disease can be more severe and progress to dengue hemorrhagic fever and dengue shock syndrome (DHF/DSS). Infection with one DENV serotype confers protective immunity to future infections with that serotype only and these persons are susceptible to secondary infections with heterologous serotypes.1 Persons with secondary DENV infections are at a greater risk of DHF/DSS than persons having their first infection.2,3
Globally, an estimated four billion persons are at risk for DENV infection, and there are an estimated 390 million annual DENV infections and 96 million dengue cases.4 From prospective community and school-based cohort studies, it has been possible to obtain estimates for the incidence of DENV infection and disease for sites in southeast Asia5–10 and Latin America.11–13 Although dengue is emerging in the Indian subcontinent and is considered a major health issue, we do not have estimates of the true burden of DENV infection and disease in this region.
Dengue was first reported in Sri Lanka in the 1960s.14 Studies conducted during 1980–1984 showed a DENV seroprevalence of 50% among school children and an annual seroconversion rate of 10–15% among 5–7-year-old school children in Colombo, the capital of Sri Lanka.15,16 More recently, analysis of age-stratified seroprevalence data indicated that the annual seroconversion rate among children < 12 years of age in Colombo is approximately 14%.16 In the past, most dengue cases have been reported from the Colombo district and other neighboring districts in the heavily urbanized southwestern region of the country. However, over the past 10–15 years, dengue has been reported from nearly all districts of the island, and over the past two decades, the number of reported DF and DHF cases has increased by more than 10-fold.17 This increase in cases has been attributed to introduction of new genotypes of DENV, as well the expansion of the range of the virus on the island.17–19 In many ways, the changing epidemiology of dengue in Sri Lanka mirrors events in other parts of the subcontinent including India, which has also documented large increases in cases and appearance of new virus strains.20,21 We conducted a population-based study to determine the incidence of symptomatic and asymptomatic DENV infection among children living in Colombo, Sri Lanka, an urban setting of the Indian subcontinent.
Materials and Methods
Ethical approval for study.
Ethical approval for this research was obtained from the Ethical Review Committee of the Faculty of Medicine, University of Colombo, Sri Lanka, and the Institutional Research Board of the International Vaccine Institute, Seoul, South Korea. Only children whose parents or legal guardians provided written informed consent were enrolled in the study.
Study site.
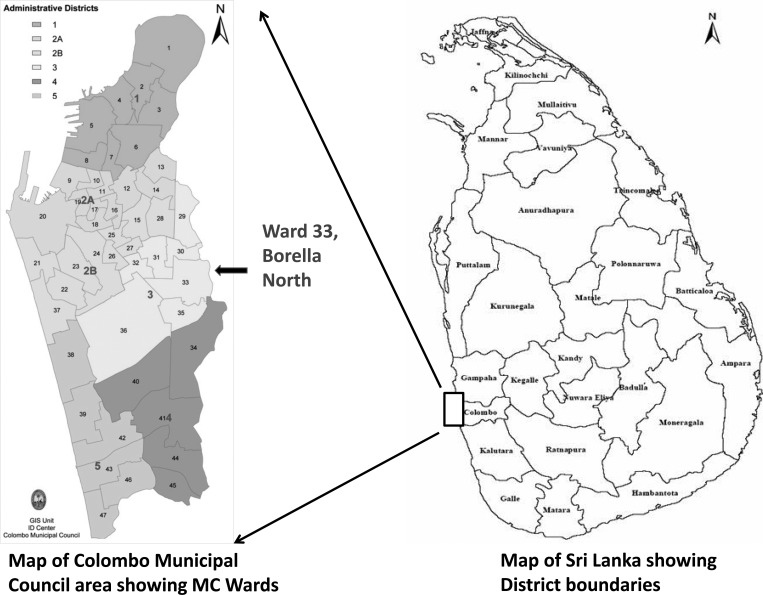
The study was conducted in the city of Colombo, the commercial capital of Sri Lanka, which has a population of 647,100 and is the most densely populated area in the country; there are 17,353 persons/km2.22 The city is divided into 47 municipal wards. Ward 33 was selected for the study because of its stable population, which reflects the socioeconomic status and demographics of the entire municipal area. Dengue is endemic to this ward, and the catchment population seeking healthcare in the tertiary care institution situated within its boundaries (Figure 1).
Figure 1.
Location of study site (Ward 33) in relation to the Colombo Municipal Council (MC) and Colombo District, Colombo, Sri Lanka.
Study population.
A prospective cohort study was conducted during November 2008–January 2010. The protocol for the study is described in detail elsewhere.23 In brief, a house-to-house census was conducted by research assistants to determine the size and obtain sociodemographic information and health-seeking patterns of the permanent resident population of children ≤ 12 years of age. A representative sample of 800 children ≤ 12 years of age was recruited for the current study. The sample size calculation was based on the ability to detect an annual incidence of dengue of 10% with an absolute precision of 3%. The estimated sample size was then inflated by 30% to allow for possible loss to follow-up during the study period. All children were enrolled in the study after written informed consent was obtained from parents/legal guardians and consent from children > 7 years of age. Each participating household was given a thermometer and each child was given an identification card with a unique study number. A febrile illness was defined as a temperature ≥ 38°C lasting ≤ 7 days in any child in the study cohort documented by a parent, research assistant, or health care professional. After assessment and treatment by a designated physician, the research assistants interviewed the patient and parent by using a standard case investigation form.
Sample collection.
Blood samples were obtained from all children at enrollment (during November 2008–January 2009) and one year after enrollment (during November 2009–January 2010) by finger prick and stored as blood spots on protein saver cards (Whatman, Piscataway, NJ and Id Biological Systems, Greeneville, SC).24,25 From children with a documented fever, whole blood was collected by venipuncture and placed in tubes containing EDTA. Some of the whole blood was used to prepare dried blood spots for serologic testing. The remaining blood was centrifuged and the plasma used for molecular diagnostic testing. Ten or more days after recovery from fever, convalescent-phase samples were collected by finger prick and stored as blood spots on protein saver cards.
DENV strains used for laboratory assays.
The World Health Organization reference DENV strains (i.e., DENV1 West Pac 74, DENV2 S-16803, DENV3 CH54389, and DENV4 TVP-360) were used for preparing antigen and infectious stocks for serologic assays. These reference viruses were initially obtained from Dr. Robert Putnak (Walter Reed Army Institute of Research, Silver Spring, MD). Infectious stocks of virus were prepared by using the C6/36 mosquito cell line, and dengue antigens were harvested from Vero cells as described.26
Molecular detection of DENV.
Plasma obtained during the acute phase of the febrile illness was tested by reverse transcription–polymerase chain reaction (RT-PCR) to detect and serotype DENVs as described.17
Detection of IgM and IgG against DENV in dried blood spots.
Antibodies were eluted from dried blood spots by submerging the filter paper in phosphate-buffered saline and incubating at 37°C for 2.5 hours. The final volume of the eluted antibody was adjusted to obtain a 1:50 or 1:100 dilution of the original blood volume applied to the filter paper. A recent report validated the use of dried blood spots for dengue serologic analysis.27
We performed dengue IgM capture enzyme-linked immunosorbent assay (ELISA) as described,28 except that monoclonal antibody (MAb) 4G2 against flavivirus, followed by enzyme-conjugated goat anti-mouse IgG to detect captured DENV antigen. In brief, 96-well plates were coated (overnight at 4°C) with 100 μL/well (1 ng/μL) of goat anti-human IgM (Sigma, St. Louis, MO) at a concentration of 0.1 mol/L in carbonate buffer, pH 9.6. Plates were washed three times in Tris-buffered saline containing 0.2% Tween 20 (TBST) and blocked with 200 μL/well of 1 × Tris-buffered saline containing 0.05% Tween 20 and 3% nonfat dry milk. Paired serum samples were tested on the same plate. Diluted serum (1:50) was loaded in duplicate and incubated (37°C for 1 hour) to capture IgM. Unbound antibody was washed, and wells were successively incubated with DENV antigen (mixture of serotypes DEN1–4), mouse anti-flavivirus 4G2 MAb, and human-absorbed alkaline phosphatase (AP)–conjugated goat anti-mouse IgG (Sigma). Optical density (OD) was measured at 405 nm after final incubation with AP substrate.
Dengue IgG ELISA was performed as described.29 Plates were coated overnight (4°C) with 100 μL/well of mouse anti-flavivirus 4G2 MAb at a concentration of 0.1 mol/L in carbonate buffer, pH 9.6, and then washed three times in TBST. Plates were then blocked with standard diluents and successively incubated (37°C for 1 hour) with DEN1–4 antigen, diluted serum (1:100) in duplicate wells, and AP-conjugated goat anti-human IgG (Fc portion). Three washings with TBST were conducted between incubations. Plates were read at 405 nm after a final incubation with AP substrate (15 minutes at room temperature in the dark).
Measurement of DENV neutralizing antibodies.
The presence of DENV neutralizing antibody was determined by using a flow cytometry–based neutralization assay with U937 monocytic cells stably transfected with dendritic cell-specific intercellular adhesion molecule-3-grabbing non-integrin as described.30 This flow cytometery–based neutralization test has comparable specificity to the conventional dengue plaque-reduction neutralization test and does not detect antibodies against Japanese encephalitis virus (Broadwater A, de Silva AM, unpublished data).30 Blood samples were serially diluted (four-fold dilutions starting at 1:40 and ending at 1:10,240) and the serum dilution that neutralized 50% of the viruses was calculated by nonlinear, dose-response regression analysis with Prism 4.0 software (GraphPad Software, Inc., San Diego, CA).
Determination of dengue serostatus at study enrollment.
DENV serostatus (DENV naive or immune) at enrollment was determined by using a dengue IgG immunoassay. An OD value ≥ 0.3 were considered dengue antibody positive. During the study period, primary infections were defined as dengue-naive children at enrollment who had had an infection. Secondary infections were defined as dengue-immune children at enrollment who had had an infection.
Laboratory criteria for diagnosis of new DENV infections.
A laboratory-confirmed clinically apparent dengue case was defined as a child who had a febrile illness and showed positive results in at least two of the three diagnostic assays (PCR, increasing levels of IgM and/or IgG in paired acute-phase and convalescent-phase blood samples). In the few cases in which there was only an acute-phase blood sample, the diagnosis was based on RT-PCR testing only. To detect clinically inapparent infections, paired baseline and end-of-year blood samples from all children were tested by IgG immunoassay. Dengue-naive children at enrollment (391 children) who seroconverted over the study year (baseline sample seronegative and end-of-year sample seropositive [≥ 0.3 OD units]) were classified as primary infections. Classification of these cases as primary infections was confirmed by neutralization testing of selected samples. The DENV-immune children at enrollment (441 children) who had increasing levels of IgG against DENV by the end of the year (≥ 0.1 OD units) were initially classified as secondary infections. However, neutralization testing indicated that when samples were collected 12 months apart, the IgG ELISA had poor specificity for detecting secondary infections (Corbett KS and others, unpublished data). Therefore, we tested paired baseline and end-of-year samples from all children who were dengue immune at enrollment for the presence of neutralizing antibodies against each of the four serotypes.
To establish criteria for defining secondary infections by using paired samples obtained 12 months apart, we used a test set of eight symptomatic secondary cases (detected by PCR and serologic analysis performed on samples collected within one month of acute infection). Only half (4 of 8) of the cases had a ≥ 4-fold increase, and all (8/8) of the cases had a ≥ 2-fold increase in neutralizing antibody levels when paired baseline and end-of-year samples from these children were tested. Therefore, children who had ≥ 2 fold increases in levels of neutralizing antibodies to one or more serotypes by the end of the year were designated as secondary infections. Samples were tested at least twice and only paired samples that displayed a reproducible two-fold increase were included as new secondary infections. Inapparent cases were defined as children who had not been identified as a clinical dengue case over the study year but still seroconverted by IgG immunoassay (primary infections) or had increasing levels of neutralizing antibodies (secondary infections) by the end of the study year.
Results
During November 2008–February 2009, a total of 800 children between 0–12 years of age were enrolled in the study from ward 33 (Figure 1); these children were representative of the age and demographic distribution of the 2,527 children known to be permanent resident of the ward. Only one child was lost to follow-up during the study period.
The dengue seroprevalence at enrollment was determined by testing all children by ELISA for IgG against DENV (Table 1). To confirm that IgG seropositivity was caused by dengue infection and not exposure to related Japanese encephalitis virus, which is also present in Sri Lanka, all IgG-positive samples were tested for DENV-neutralizing antibodies. Most (96%) of IgG-positive serum samples also neutralized DENV, indicating that in this population the results of the IgG ELISA reflected dengue seroprevalence. The overall dengue seroprevalence was 53% at enrollment (Table 1). The age specific seroprevalence steadily increased with age from a low of 22% in the youngest (< 1 year) age group to a high of 74.26% in the oldest (10–12 years) age group (Table 1).
Table 1.
Age-specific dengue seroprevalence in children, Sri Lanka*
| Age group (years) | No. children | No. seropositive by IgG ELISA | No. seropositive confirmed by dengue neutralization test | Seroprevalence (%) |
|---|---|---|---|---|
| < 1 | 51 | 12 | 11 | 21.57 |
| 1–3 | 196 | 71 | 67 | 34.18 |
| 4–6 | 191 | 105 | 100 | 52.36 |
| 7–9 | 225 | 150 | 145 | 64.44 |
| 10–12 | 136 | 103 | 101 | 74.26 |
| Total | 799 | 441 | 424 | 53.07 |
Dengue seroprevalence at the beginning of study (baseline) was determined by screening all serum samples by dengue IgG enzyme-linked immunosorbent assay (ELISA) and then testing the positive samples by dengue neutralization test.
A total of 681 fever episodes were detected among the 799 children, indicating that on average each child reported 0.9 fever episodes over one person-year of follow-up (Table 2). Dengue was laboratory confirmed for 3.9% (27 of 681) of the fever episodes (Table 2); no child had more than one episode of dengue fever over the course of the study. Therefore, the incidence of clinically apparent dengue in the cohort was 3.38 cases/100 children/year (Table 2). When combined with the clinically inapparent infections, the total incidence of DENV infection was 8.39 cases/100 children (Table 2). The highest incidence of infection and disease was in children 1–3 years of age. The overall ratio of inapparent to apparent infections was 1.48. We used a two-fold instead of a four-fold increase in neutralizing antibody levels to identify new secondary infections because a four-fold increase had poor sensitivity for paired samples collected 12 months apart. It is possible that the two-fold increase reduces specificity and leads to a modest overestimation of true incidence.
Table 2.
Age-specific fever episodes and incidence of dengue infection and illness in children, Sri Lanka*
| Age (years) | No. children | Fever episodes | New dengue infections | Incidence of infection per 100 children | Incidence of disease per 100 children | |||
|---|---|---|---|---|---|---|---|---|
| Total | Mean/child | Total | Inapparent | Apparent | ||||
| < 1 | 51 | 31 | 0.6 | 1 | 0 | 1 | 1.96 (0.05–10.45) | 1.96 (0.05–10.45) |
| 1–3 | 196 | 252 | 1.3 | 27 | 15 | 12 | 13.78 (9.28–19.41) | 6.12 (3.20–10.45) |
| 4–6 | 191 | 174 | 0.9 | 13 | 11 | 2 | 6.81 (3.67–11.36) | 1.05 (0.13–3.73) |
| 7–9 | 225 | 137 | 0.6 | 15 | 6 | 9 | 6.67 (3.78–10.76) | 4.00 (1.85–7.46) |
| 10–12 | 136 | 87 | 0.6 | 11 | 8 | 3 | 8.09 (3.25–16.03) | 2.21 (0.46–6.31) |
| Total | 799 | 681 | 0.9 | 67 | 40 | 27 | 8.39 (6.56–10.53) | 3.38 (2.24–4.88) |
Values in parentheses are 95% confidence intervals. Clinically apparent dengue infections were diagnosed by performing paired serologic analysis and polymerase chain reaction on acute-phase and convalescent-phase serum samples obtained from febrile children. Total dengue infections over the study year were detected by testing paired baseline and end of year samples by IgG enzyme-linked immunosorbent assay and neutralization test. Children who were infected but not identified as having apparent cases were designated as having inapparent cases.
Of the 67 new apparent and inapparent DENV infections, 35 were primary infections and 32 were secondary infections (Table 3). As might be expected, the ratio of primary to secondary infections decreased with age from 3 in the youngest (< 1 year) age group to 0.75 in the oldest (10–12 years) age group. The ratios of inapparent to apparent infections were not statistically significantly different (P > 0.1) between primary and secondary infections (Table 3).
Table 3.
Dengue disease outcome in children exposed to primary or secondary infections, Sri Lanka
| Infection, no. | Disease | ||
|---|---|---|---|
| Inapparent | Apparent | Inapparent:apparent ratio | |
| Primary, 35 | 20 | 15 | 1.33 |
| Secondary, 32 | 20 | 12 | 1.67 |
| Total, 67 | 40 | 27 | 1.48 |
The prevalence of each DENV serotype during the study year was estimated by identifying the serotypes responsible for primary infections (Supplemental Table 1). DENV2 was the most common serotype (49%) followed by DENV3 (27%), DENV1 (23%), and DENV4 (3%). The number of persons with monospecific neutralizing antibodies to each serotype at enrollment into the study was used to estimate the prevalence of each serotype in this population before the start of our study (Supplemental Table 1). This analysis showed that DENV2 (43%) and DENV3 (29%) were more common than DENV1 (9%) and DENV4 (12%) in the period preceding the study.
Discussion
Over the past two decades, dengue has emerged as a major health problem in the Indian subcontinent.20,21 Dengue epidemics in the region have been linked to more intense transmission, expansion of the range of the virus, and introduction of new strains.17–21 Most estimates of dengue incidence in the region are based on hospital-based studies and nationally reported cases, which grossly underestimate the true burden of disease and infection.31 We followed a cohort of 799 children in Colombo, Sri Lanka, and estimated the incidence of infection and disease to be 8.39 and 3.38 cases/100 children, respectively. The ratio of clinically inapparent to apparent infections was 1.48, which indicated that for every apparent infection there were approximately 1.5 inapparent infections in children. This high intensity of transmission was also supported by the seroprevalence data, which showed a gradually increasing prevalence with age that ranged from 22% in the youngest age group to 74% in the oldest age group. The four DENV serotypes were circulating in this population before and during our study; serotypes 2 and 3 were more prevalent than serotypes 1 and 4 (Supplemental Table 1). Our study establishes a rigorously measured, accurate burden of dengue infection and disease among children living in an urban area of Sri Lanka.
Recently, we used dengue seroprevalence data from this cohort to model the rate of primary infections in dengue-naive children.16 Using a catalytic model, we estimated the incidence of primary infection to be 14.1% per year (95% confidence interval [CI] = 12.7–15.6%), which is higher than the incidence of 8.39% (95% CI = 6.56–10.53%) observed for total infections (primary and secondary infections). A more legitimate comparison would be to compare the model based estimate for primary infections with the incidence of primary infections in our cohort. The incidence of primary infection noted in the current study was 9.8% (95% CI = 6.80–12.80%), which is closer to the model-based estimate of 14.1% per year (95% CI = 12.7–15.6%). A previous study of school children in Colombo over a five-year period during 1980–1985 estimated the incidence of new infections to range between 10.78 and 18.54 cases/100 children in different years.15 Collectively, these findings demonstrate intense transmission of dengue among children in Colombo.
Our current estimate for disease (3.38 cases/100 children < 12 years of age) is 14-fold higher than the reported national incidence of the disease (0.23/100 persons) among persons < 15 years of age in 2010 in Sri Lanka, which is based on the passive national surveillance system (Epidemiology Unit, Ministry of Health). Based on national surveillance for 2010, the disease estimates for children < 15 years of age in the Colombo district and the Colombo Municipality (study area) (Figure 1) were 0.64 and 1.61 cases/100 persons, respectively. Thus, as expected, the passive national program underreports the true burden of disease in Sri Lanka. Recent studies in Southeast Asia have estimated expansion factors of 8.9 and 9.6 when comparing national data with true disease incidence for Thailand and Cambodia, respectively.7,32 Moreover, a recent study of the global burden of dengue estimated that there are three times as many infections and dengue cases compared with cases reported to the World Health Organization.4
For most regions in the world with endemic dengue transmission, we do not have accurate estimates of infection and disease because of the cost and infrastructure required to conduct cohort studies. The most comprehensive cohort studies on dengue in Southeast Asia have been conducted in Thailand where the incidence of infection has ranged between 2% and 15% depending on the year and location of the study.5,6,8,33,34 Studies in Puerto Rico, Nicaragua, and Peru have documented incidences that range between 1.34% and 12% depending on the year and location.11,12 Thus, the intensity of dengue transmission among children in Colombo (8.14%) is similar to transmission documented in other cohort studies conducted in Southeast Asia and Latin America. The ratio of inapparent to apparent infections has also been estimated in different regions of the world. In southeast Asia, the ratio has ranged from 3:1 to 1:1, whereas in Latin America the ratio has ranged from 3:1 to 18:1, indicating that infections in Southeast Asia5,6,8 are more likely to lead to clinically apparent cases than infections in Latin America.11,12 The data we report indicate that the situation in Colombo Sri Lanka with a ratio of 1.5:1 is more similar to the situation in Southeast Asia.
The current study was not designed to test hypotheses about risk factors for DHF/DSS because our cohort of 799 children is too small to detect significant numbers of DHF/DSS cases. We did not observe any significant differences in the ratio of inapparent to apparent cases between primary and secondary cases. However, it is premature to conclude from these data that risk of developing a clinically apparent infection is the same in primary and secondary cases because the study was only powered to detect a large difference in risk after primary and secondary infection. Other studies have documented that children exposed to primary and secondary infections have a similar risk of developing clinically apparent infections.6
It is well documented that the incidence of infection and disease can vary from year to year and our data were collected over a single year only. Our study was confined to a relatively small area and our results may not be generalizable to children in other parts of the city and country. Thus, studies such as this have to be conducted in other parts of the country over a longer period to understand how the incidence of infection and disease vary by location and over time. Dengue vaccines are currently being tested in different regions of the world.35 It is important that trials also be conducted in the Indian subcontinent given the heavy burden of disease and the distinct strains of DENV circulating in the region. The results of the current study will be useful for designing vaccine trials in southern Asia and for making decisions about how best to introduce vaccines.
Supplementary Material
Footnotes
Financial support: This study was supported by the Pediatric Dengue Vaccine Initiative through grant no. 23197 and partially supported by the National Institutes of Health (University of North Carolina Virology Training Grant T32AI007419 and Initiative for Minority Student Development grant no. 5R25GM055336 to Kizzmekia S. Corbett).
Authors' addresses: Hasitha Tissera, Epidemiology Unit, Ministry of Health, Colombo, Sri Lanka, E-mail: dr_korelege@yahoo.co.uk. Ananda Amarasinghe, Epidemiology Unit, Ministry of Health, Colombo, Sri Lanka, and International Vaccine Institute, Pediatric Dengue Vaccine Initiative, Seoul, South Korea, E-mail: ana_amarasinghe@yahoo.co.uk. Aruna Dharshan De Silva, Genetech Research Institute, Colombo, Sri Lanka, E-mail: dslv90@yahoo.com. Pradeep Kariyawasam, Colombo Municipal Council, Public Health Department, Colombo, Sri Lanka, E-mail: munici@slt.lk. Kizzmekia S. Corbett and Aravinda M. de Silva, Department of Microbiology and Immunology, University of North Carolina, Chapel Hill, NC, E-mails: kscorbet@email.unc.edu and aravinda_desilva@med.unc.edu or desilva@med.unc.edu. Leah Katzelnick, Department of Zoology, University of Cambridge, Cambridge, United Kingdom, E-mail: lck33@cam.ac.uk. Clarence Tam, London School of Hygiene and Tropical Medicine, London, United Kingdom, E-mail: clarence.tam@lshtm.ac.uk. G. William Letson, Center for Global Public Health, Colorado School of Public Health, Aurora, CO, E-mail: bwletson@gmail.com. Harold S. Margolis, Dengue Branch, Centers for Disease Control and Prevention, San Juan, PR, E-mail: hsm1@cdc.gov.
References
- 1.Wahala WM, Silva AM. The human antibody response to dengue virus infection. Viruses. 2011;3:2374–2395. doi: 10.3390/v3122374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Halstead SB. Dengue. Lancet. 2007;370:1644–1652. doi: 10.1016/S0140-6736(07)61687-0. [DOI] [PubMed] [Google Scholar]
- 3.Rothman AL. Immunity to dengue virus: a tale of original antigenic sin and tropical cytokine storms. Nat Rev Immunol. 2011;11:532–543. doi: 10.1038/nri3014. [DOI] [PubMed] [Google Scholar]
- 4.Bhatt S, Gething PW, Brady OJ, Messina JP, Farlow AW, Moyes CL, Drake JM, Brownstein JS, Hoen AG, Sankoh O, Myers MF, George DB, Jaenisch T, Wint GR, Simmons CP, Scott TW, Farrar JJ, Hay SI. The global distribution and burden of dengue. Nature. 2013;496:504–507. doi: 10.1038/nature12060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Endy TP, Anderson KB, Nisalak A, Yoon IK, Green S, Rothman AL, Thomas SJ, Jarman RG, Libraty DH, Gibbons RV. Determinants of inapparent and symptomatic dengue infection in a prospective study of primary school children in Kamphaeng Phet, Thailand. PLoS Negl Trop Dis. 2011;5:e975. doi: 10.1371/journal.pntd.0000975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Endy TP, Chunsuttiwat S, Nisalak A, Libraty DH, Green S, Rothman AL, Vaughn DW, Ennis FA. Epidemiology of inapparent and symptomatic acute dengue virus infection: a prospective study of primary school children in Kamphaeng Phet, Thailand. Am J Epidemiol. 2002;156:40–51. doi: 10.1093/aje/kwf005. [DOI] [PubMed] [Google Scholar]
- 7.Vong S, Goyet S, Ly S, Ngan C, Huy R, Duong V, Wichmann O, Letson GW, Margolis HS, Buchy P. Under-recognition and reporting of dengue in Cambodia: a capture-recapture analysis of the National Dengue Surveillance System. Epidemiol Infect. 2012;140:491–499. doi: 10.1017/S0950268811001191. [DOI] [PubMed] [Google Scholar]
- 8.Yoon IK, Rothman AL, Tannitisupawong D, Srikiatkhachorn A, Jarman RG, Aldstadt J, Nisalak A, Mammen MP, Jr, Thammapalo S, Green S, Libraty DH, Gibbons RV, Getis A, Endy T, Jones JW, Koenraadt CJ, Morrison AC, Fansiri T, Pimgate C, Scott TW. Underrecognized mildly symptomatic viremic dengue virus infections in rural Thai schools and villages. J Infect Dis. 2012;206:389–398. doi: 10.1093/infdis/jis357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sabchareon A, Sirivichayakul C, Limkittikul K, Chanthavanich P, Suvannadabba S, Jiwariyavej V, Dulyachai W, Pengsaa K, Margolis HS, Letson GW. Dengue infection in children in Ratchaburi, Thailand: a cohort study. I. Epidemiology of symptomatic acute dengue infection in children, 2006–2009. PLoS Negl Trop Dis. 2012;6:e1732. doi: 10.1371/journal.pntd.0001732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tien NT, Luxemburger C, Toan NT, Pollissard-Gadroy L, Huong VT, Van Be P, Rang NN, Wartel TA, Lang J. A prospective cohort study of dengue infection in schoolchildren in Long Xuyen, Viet Nam. Trans R Soc Trop Med Hyg. 2010;104:592–600. doi: 10.1016/j.trstmh.2010.06.003. [DOI] [PubMed] [Google Scholar]
- 11.Balmaseda A, Standish K, Mercado JC, Matute JC, Tellez Y, Saborio S, Hammond SN, Nunez A, Aviles W, Henn MR, Holmes EC, Gordon A, Coloma J, Kuan G, Harris E. Trends in patterns of dengue transmission over 4 years in a pediatric cohort study in Nicaragua. J Infect Dis. 2010;201:5–14. doi: 10.1086/648592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Morrison AC, Minnick SL, Rocha C, Forshey BM, Stoddard ST, Getis A, Focks DA, Russell KL, Olson JG, Blair PJ, Watts DM, Sihuincha M, Scott TW, Kochel TJ. Epidemiology of dengue virus in Iquitos, Peru 1999 to 2005: interepidemic and epidemic patterns of transmission. PLoS Negl Trop Dis. 2010;4:e670. doi: 10.1371/journal.pntd.0000670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ramos MM, Arguello DF, Luxemburger C, Quinones L, Munoz JL, Beatty M, Lang J, Tomashek KM. Epidemiological and clinical observations on patients with dengue in Puerto Rico: results from the first year of enhanced surveillance, June 2005–May 2006. Am J Trop Med Hyg. 2008;79:123–127. [PubMed] [Google Scholar]
- 14.Vitarana T. Viral diseases in Sri Lanka: a national overview. In: Mackenzie JS, editor. Viral Diseases in Southeast Asia and the Western Pacific. London: Academic Press; 1982. pp. 198–204. [Google Scholar]
- 15.Messer WB, Vitarana UT, Sivananthan K, Elvtigala J, Preethimala LD, Ramesh R, Withana N, Gubler DJ, De Silva AM. Epidemiology of dengue in Sri Lanka before and after the emergence of epidemic dengue hemorrhagic fever. Am J Trop Med Hyg. 2002;66:765–773. doi: 10.4269/ajtmh.2002.66.765. [DOI] [PubMed] [Google Scholar]
- 16.Tam CC, Tissera H, de Silva AM, De Silva AD, Margolis HS, Amarasinge A. Estimates of dengue force of infection in children in Colombo, Sri Lanka. PLoS Negl Trop Dis. 2013;7:e2259. doi: 10.1371/journal.pntd.0002259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kanakaratne N, Wahala WM, Messer WB, Tissera HA, Shahani A, Abeysinghe N, de-Silva AM, Gunasekera M. Severe dengue epidemics in Sri Lanka, 2003–2006. Emerg Infect Dis. 2009;15:192–199. doi: 10.3201/eid1502.080926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Messer WB, Gubler DG, Harris E, Sivananthan K, de Silva AM. Emergence and global spread of a dengue serotype 3, subtype III virus. Emerg Infect Dis. 2003;9:800–809. doi: 10.3201/eid0907.030038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tissera HA, Ooi EE, Gubler DJ, Tan Y, Logendra B, Wahala WM, de Silva AM, Abeysinghe MR, Palihawadana P, Gunasena S, Tam CC, Amarasinghe A, Letson GW, Margolis HS, De Silva AD. New dengue virus type 1 genotype in Colombo, Sri Lanka. Emerg Infect Dis. 2011;17:2053–2055. doi: 10.3201/eid1711.101893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chakravarti A, Arora R, Luxemburger C. Fifty years of dengue in India. Trans R Soc Trop Med Hyg. 2012;106:273–282. doi: 10.1016/j.trstmh.2011.12.007. [DOI] [PubMed] [Google Scholar]
- 21.Raheel U, Faheem M, Riaz MN, Kanwal N, Javed F, Zaidi N, Qadri I. Dengue fever in the Indian subcontinent: an overview. J Infect Dev Ctries. 2011;5:239–247. doi: 10.3855/jidc.1017. [DOI] [PubMed] [Google Scholar]
- 22.Anonymous . Population and Housing Data, City of Colombo (Colombo Municipal Council), Sri Lanka. Census of Population and Housing 2001. Colombo, Sri Lanka: Census Department; 2001. [Google Scholar]
- 23.Tissera HA, Amarasinghe A, De Silva AM, Tam CC, De Silva AD, Letson GW, Margolis HS. Surveillance of Dengue in a Community Cohort in Metropolitan Colombo, Sri Lanka: Methods and Study Population. Geneva: World Health Organization, Bulletin 91; 2013. [Google Scholar]
- 24.Snijdewind IJ, van Kampen JJ, Fraaij PL, van der Ende ME, Osterhaus AD, Gruters RA. Current and future applications of dried blood spots in viral disease management. Antiviral Res. 2012;93:309–321. doi: 10.1016/j.antiviral.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 25.Balmaseda A, Saborio S, Tellez Y, Mercado JC, Perez L, Hammond SN, Rocha C, Kuan G, Harris E. Evaluation of immunological markers in serum, filter-paper blood spots, and saliva for dengue diagnosis and epidemiological studies. J Clin Virol. 2008;43:287–291. doi: 10.1016/j.jcv.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 26.Wahala WM, Kraus AA, Haymore LB, Accavitti-Loper MA, de Silva AM. Dengue virus neutralization by human immune sera: role of envelope protein domain III-reactive antibody. Virology. 2009;392:103–113. doi: 10.1016/j.virol.2009.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Anders KL, Nguyet NM, Quyen NT, Ngoc TV, Tram TV, Gan TT, Tung NT, Dung NT, Chau NV, Wills B, Simmons CP. An evaluation of dried blood spots and oral swabs as alternative specimens for the diagnosis of dengue and screening for past dengue virus exposure. Am J Trop Med Hyg. 2012;87:165–170. doi: 10.4269/ajtmh.2012.11-0713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kuno G, Gomez I, Gubler DJ. Detecting artificial anti-dengue IgM immune complexes using an enzyme-linked immunosorbent assay. Am J Trop Med Hyg. 1987;36:153–159. doi: 10.4269/ajtmh.1987.36.153. [DOI] [PubMed] [Google Scholar]
- 29.Chungue E, Marche G, Plichart R, Boutin JP, Roux J. Comparison of immunoglobulin G enzyme-linked immunosorbent assay (IgG-ELISA) and haemagglutination inhibition (HI) test for the detection of dengue antibodies. Prevalence of dengue IgG-ELISA antibodies in Tahiti. Trans R Soc Trop Med Hyg. 1989;83:708–711. doi: 10.1016/0035-9203(89)90404-5. [DOI] [PubMed] [Google Scholar]
- 30.Kraus AA, Messer W, Haymore LB, de Silva AM. Comparison of plaque- and flow cytometry-based methods for measuring dengue virus neutralization. J Clin Microbiol. 2007;45:3777–3780. doi: 10.1128/JCM.00827-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Beatty ME, Stone A, Fitzsimons DW, Hanna JN, Lam SK, Vong S, Guzman MG, Mendez-Galvan JF, Halstead SB, Letson GW, Kuritsky J, Mahoney R, Margolis HS. Best practices in dengue surveillance: a report from the Asia-Pacific and Americas Dengue Prevention Boards. PLoS Negl Trop Dis. 2010;4:e890. doi: 10.1371/journal.pntd.0000890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wichmann O, Yoon IK, Vong S, Limkittikul K, Gibbons RV, Mammen MP, Ly S, Buchy P, Sirivichayakul C, Buathong R, Huy R, Letson GW, Sabchareon A. Dengue in Thailand and Cambodia: an assessment of the degree of underrecognized disease burden based on reported cases. PLoS Negl Trop Dis. 2011;5:e996. doi: 10.1371/journal.pntd.0000996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Thai KT, Binh TQ, Giao PT, Phuong HL, Hung LQ, Nam NV, Nga TT, Groen J, Nagelkerke N, de Vries PJ. Seroprevalence of dengue antibodies, annual incidence and risk factors among children in southern Vietnam. Trop Med Int Health. 2005;10:379–386. doi: 10.1111/j.1365-3156.2005.01388.x. [DOI] [PubMed] [Google Scholar]
- 34.Tran HP, Adams J, Jeffery JA, Nguyen YT, Vu NS, Kutcher SC, Kay BH, Ryan PA. Householder perspectives and preferences on water storage and use, with reference to dengue, in the Mekong Delta, southern Vietnam. In Health. 2010;2:136–142. doi: 10.1016/j.inhe.2009.12.007. [DOI] [PubMed] [Google Scholar]
- 35.Sabchareon A, Wallace D, Sirivichayakul C, Limkittikul K, Chanthavanich P, Suvannadabba S, Jiwariyavej V, Dulyachai W, Pengsaa K, Wartel TA, Moureau A, Saville M, Bouckenooghe A, Viviani S, Tornieporth NG, Lang J. Protective efficacy of the recombinant, live-attenuated, CYD tetravalent dengue vaccine in Thai schoolchildren: a randomised, controlled phase 2b trial. Lancet. 2012;380:1559–1567. doi: 10.1016/S0140-6736(12)61428-7. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.