Abstract
Shared sanitation is defined as unimproved because of concerns that it creates unsanitary conditions; this policy is being reconsidered. We assessed whether sharing a toilet facility was associated with an increased prevalence of diarrhea among children < 5 years of age. We use data from Demographic and Health Surveys conducted in 51 countries. Crude and adjusted prevalence ratios (PRs) for diarrhea, comparing children from households that used a shared facility with children from households that used a non-shared facility, were estimated for each country and pooled across countries. Unadjusted PRs varied across countries, ranging from 2.15 to 0.65. The pooled PR was 1.09; differences in socioeconomic status explained approximately half of this increased prevalence (adjusted PR = 1.05). Shared sanitation appears to be a risk factor for diarrhea although differences in socioeconomic status are important. The heterogeneity across countries, however, suggests that the social and economic context is an important factor.
Introduction
Diarrheal disease is a major cause of morbidity and mortality, particularly in low- and middle-income countries.1 Inadequate sanitation, water, and hygiene are the most significant risk factors for diarrheal disease and are responsible for an estimated 1.9 million deaths worldwide.2 Since the adoption of the Millennium Development Goals (MDGs), access to improved sanitation has increased around the globe. However, approximately 37% of the world's population (2.5 billion persons) still lacks access to improved sanitation.3 This finding includes an estimated 761 million persons who rely on public or other shared sanitation facilities.
To track changes in water and sanitation, including progress towards international targets such as the MDGs, The World Health Organization and the United Nations Children's Fund created the Joint Monitoring Program (JMP) for Water Supply and Sanitation. Apart from monitoring, the JMP was tasked with creating a uniform definition of improved and unimproved sanitation to be used across countries. The JMP definition of improved sanitation currently includes flush or pour-flush toilets, pit latrines with a slab, ventilated improved pit latrines, and composting toilets, and unimproved sanitation includes open defecation, pit latrines without a slab, buckets, hanging toilets or latrines, or a flush/pour flush toilet that flushes to an unsanitary destination.3 Because of concerns about cleanliness and accessibility, facilities that are shared by two or more households are classified as unimproved, regardless of the level of technology used.3
Recently, the JMP's Task Force on Sanitation proposed a change in this policy that would allow sanitation facilities to be considered as improved, and therefore scored toward the MDG and other international sanitation targets, provided they meet the other criteria and are shared by no more than 5 households or 30 persons, whichever is fewer.4 In 2010, an estimated 11% of the world's population used a shared facility that would otherwise be considered improved, and that percentage is increasing.3 There is relatively little evidence, however, on whether and at what circumstances sharing sanitation facilities actually poses a health risk to those that use them. Also, public latrines are considered by some to be the only viable option in many urban slums.3,5–7
Because of this trend towards shared sanitation, more empirical data are needed to determine whether such facilities increase the risk of disease, and if so, to quantify that risk, identify the causal pathway and explore ways of mitigating it. A recent systematic review has reported that shared sanitation may be a risk factor for diarrhea and other adverse health outcomes when compared with individual household latrines.8 The review identified eight studies (two cross-sectional and six case-control); shared sanitation was the focus in only two of these studies,9,10 and the others simply reported statistical associations with little to no mention of potential mechanisms. Although these studies report an association between shared sanitation and diarrhea, the review noted substantial deficiencies in the quality of methods used in most studies, including the failure to account for some potential sources of confounding, unclear comparisons, and failure to distinguish between different types of sanitation technology and ownership.
The objective of our study was to determine whether the prevalence of diarrhea is higher among those that share a toilet facility compared with those that use a facility that is not shared. We used data from 51 low- and middle-income countries that represent much of the developing world. We also define shared sanitation three ways. Finally, we rigorously assessed the extent to which confounding plays a role in the association between sharing and diarrhea.
Methods
We use data from the Demographic and Health Surveys (DHSs) (measuredhs.com) completed during 2001–2011. Surveys completed before 2001 were excluded. As a result, our findings will better reflect current circumstances and be more able to inform an ongoing policy debate. To achieve a representative sample at the subnational level, these cross-sectional surveys use a two-stage stratified random sample of households. Countries are divided into enumeration areas (clusters), and then households are randomly selected within each cluster with a different probability of selection within different clusters. The surveys ask a variety of questions about demographics, reproductive health, and child health. For countries that had multiple surveys in this period, we use only the most recent one to prevent overrepresentation of single countries. We selected the 51 recent surveys from low- and middle-income countries that included data on disease outcome, exposure, and potential confounders (Table 1).
Table 1.
Summary statistics of all children < 5 years of age by country
| Country (year) | Sample size | Prevalence of diarrhea (%) | No toilet facility (%) | Improved toilet facility (%)* | Shared toilet facility (%)† | Shared with > 5 households (%)‡ |
|---|---|---|---|---|---|---|
| All countries | 435,205 | 14.3 | 30.9 | 45.1 | 29.9 | 22.2 |
| Africa | 220,000 | 15.4 | 32.1 | 31.5 | 41.8 | 24.2 |
| Benin (2006) | 14,270 | 9.2 | 68.6 | 18.1 | 69.5 | 56.1 |
| Burkina Faso (2010) | 13,487 | 14.9 | 68.1 | 25.1 | 51.0 | 14.0 |
| Burundi (2011) | 7,147 | 25.2 | 3.0 | 40.0 | 15.9 | 9.0 |
| Cameroon (2011) | 9,932 | 21.8 | 8.4 | 53.9 | 29.4 | 18.9 |
| Republic of Congo (2005) | 4,047 | 14.1 | 11.9 | 17.1 | 60.6 | – |
| Democratic Republic of Congo (2007) | 7,678 | 16.5 | 11.6 | 37.2 | 55.3 | – |
| Ethiopia (2003) | 10,441 | 13.6 | 43.1 | 12.6 | 27.7 | 19.0 |
| Ghana (2008) | 2,733 | 20.1 | 27.6 | 60.5 | 87.3 | 80.8 |
| Guinea (2005) | 5,316 | 16.4 | 30.1 | 25.4 | 60.8 | – |
| Kenya (2009) | 5,533 | 16.8 | 18.1 | 39.9 | 49.4 | 29.0 |
| Lesotho (2010) | 3,322 | 11.4 | 41.8 | 31.7 | 36.2 | 34.2 |
| Liberia (2007) | 4,930 | 20.8 | 59.8 | 23.5 | 76.0 | 64.3 |
| Madagascar (2009) | 11,444 | 8.4 | 49.9 | 3.9 | 63.8 | 15.2 |
| Malawi (2010) | 17,966 | 17.6 | 11.1 | 11.8 | 42.8 | 7.0 |
| Mali (2006) | 12,070 | 13.6 | 19.8 | 20.4 | 45.0 | 3.2 |
| Namibia (2007) | 4,238 | 13.4 | 58.1 | 37.8 | 25.2 | 36.5 |
| Niger (2006) | 7,922 | 21.3 | 80.5 | 8.8 | 39.3 | 41.9 |
| Nigeria (2008) | 24,733 | 10.4 | 30.7 | 51.8 | 40.2 | 41.8 |
| Rwanda (2011) | 8,330 | 13.1 | 1.3 | 72.9 | 19.7 | 5.4 |
| Sao Tome and Principe (2009) | 1,807 | 15.9 | 62.1 | 37.7 | 20.3 | 34.4 |
| Senegal (2011) | 11,060 | 21.1 | 19.1 | 55.8 | 24.3 | 8.6 |
| Sierra Leone (2008) | 4,783 | 13.6 | 23.9 | 39.7 | 77.6 | 35.1 |
| Swaziland (2007) | 2,325 | 14.3 | 22.0 | 28.7 | 33.6 | 30.5 |
| Tanzania (2010) | 6,995 | 14.9 | 18.9 | 14.8 | 30.6 | 13.5 |
| Uganda (2011) | 7,015 | 24.1 | 11.1 | 29.8 | 39.7 | 23.3 |
| Zambia (2007) | 5,582 | 15.8 | 27.4 | 30.8 | 40.1 | 9.9 |
| Zimbabwe (2011) | 4,894 | 13.6 | 32.2 | 57.1 | 47.5 | 17.8 |
| Latin America and the Caribbean | 75,910 | 16.1 | 18.0 | 66.1 | 17.9 | 8.5 |
| Bolivia (2008) | 8,135 | 26.2 | 32.5 | 37.9 | 33.7 | 10.3 |
| Colombia (2010) | 17,220 | 12.7 | 8.4 | 85.1 | 13.3 | – |
| Dominican Republic (2007) | 10,285 | 14.8 | 5.8 | 90.2 | 18.0 | – |
| Guyana (2009) | 2,027 | 10.1 | 1.4 | 87.8 | 13.6 | 3.6 |
| Haiti (2006) | 5,358 | 24.4 | 41.1 | 24.7 | 49.7 | 12.8 |
| Honduras (2006) | 10,198 | 16.0 | 21.9 | 58.5 | 15.2 | 2.0 |
| Nicaragua (2001) | 6,536 | 13.0 | 22.2 | 27.9 | 8.6 | – |
| Peru (2008) | 16,151 | 13.8 | 17.9 | 78.9 | 13.7 | 7.7 |
| Southeast Asia | 85,276 | 10.7 | 46.5 | 43.2 | 25.1 | 22.0 |
| Bangladesh (2007) | 5,201 | 10.1 | 8.6 | 37.6 | 45.1 | 11.2 |
| India (2006) | 45,144 | 8.9 | 62.3 | 34.3 | 32.5 | 25.2 |
| Indonesia (2007) | 17,292 | 13.8 | 25.1 | 56.0 | 14.1 | 45.0 |
| Maldives (2009) | 3,678 | 4.5 | 0.7 | 96.9 | 2.1 | 22.6 |
| Nepal (2011) | 4,754 | 13.9 | 48.8 | 43.6 | 30.9 | 6.9 |
| Timor-Leste (2010) | 9,207 | 15.6 | 37.5 | 50.5 | 16.9 | 4.5 |
| Western Pacific | 13,837 | 12.4 | 40.3 | 56.2 | 24.5 | 7.5 |
| Cambodia (2011) | 7,670 | 15.0 | 61.6 | 36.1 | 19.7 | 7.5 |
| Philippines (2008) | 6,167 | 9.1 | 12.9 | 82.0 | 27.3 | – |
| Eastern Mediterranean | 33,605 | 14.4 | 11.7 | 83.6 | 7.0 | 1.6 |
| Egypt (2008) | 9,992 | 8.4 | 0.4 | 99.5 | 5.7 | 1.6 |
| Jordan (2007) | 9,791 | 15.9 | 0.0 | 99.5 | 3.1 | – |
| Morocco (2004) | 5,746 | 11.9 | 20.8 | 78.6 | 7.9 | – |
| Pakistan (2007) | 8,076 | 21.6 | 32.6 | 49.3 | 15.5 | – |
| Europe | 6,577 | 8.2 | 0.0 | 84.2 | 6.3 | 20.4 |
| Albania (2009) | 1,562 | 5.4 | 0.0 | 93.8 | 2.2 | 0.0 |
| Armenia (2010) | 1,433 | 8.7 | 0.0 | 77.9 | 1.4 | 9.2 |
| Azerbaijan (2006) | 2,116 | 10.7 | 0.1 | 80.7 | 10.0 | 24.6 |
| Moldova (2005) | 1,466 | 7.1 | 0.0 | 85.3 | 9.6 | – |
Based on the Joint Monitoring Program categorization, but ignoring sharing.
Among households that have a sanitation facility.
Among households with a shared sanitation facility. – = data not collected.
For any children less than five years of age in the household, the caretaker reported whether said child had diarrhea in the past two weeks. Each caretaker also reported the type of toilet facility that the household uses. For each survey, we classified each potential response as being improved or unimproved based on the definitions provided by the JMP but ignoring sharing.3 Responses considered to be improved were then further classified based on whether the facility used flush technology, yielding three categories: unimproved facility, improved latrine, and improved flush or pour-flush toilet. Caretakers then reported whether their facility was shared by other households. We used this information to create three measures of sharing. First, a binary definition of sharing was used, where a toilet facility was classified as shared if more than one household used it. Those with no facility were excluded. We then accounted for the number of households that share the facility, creating three exposure categories: 1) facilities that are not shared, 2) facilities shared by five or fewer households, and 3) facilities shared by more than five households. Again, those with no facility were excluded. The data describing the number of households sharing, however, was only available in 40 of the 51 surveys (Table 1). Finally, we use the sanitation ladder of the JMP, which was composed of four categories: 1) no facility, 2) unimproved facility, 3) shared but otherwise improved facility, and 4) improved facility that is not shared. Log-binomial regression, accounting for complex sampling strategy, was used to generate the unadjusted (crude) and adjusted prevalence ratios (PRs) and 95% confidence intervals (CIs) for diarrhea. The prevalence ratios represent the relative difference in diarrhea prevalence comparing children from households with a shared facility compared with children from households with a facility that is not shared.
Households that use a shared sanitation facility are likely different in many respects than households that have their own facility. To account for these differences, we made a list of potential confounding variables to include in the analysis. Characteristics of the household assessed were type of sanitation facility (unimproved, improved latrine, improved flush or pour-flush toilet; improved being defined by JMP, but ignoring sharing), improved water source (as defined by JMP), household ownership of assets (electricity, radio, television, refrigerator, bicycle, motorcycle/scooter, car/truck, improved cooking fuel, and improved floor surface), urban/rural residence, the mother's age, the mother's educational attainment, the highest level of education in the household, and number of children less than five 5 years of age in the household. Characteristics of the child assessed were age, sex, vaccination status, and whether the child had a health card. The DHS includes many more variables, but we selected this group because each captures a different aspect of socioeconomic status. We chose this list of confounders a priori and analyzed each of them individually and in groups to assess their impact on the prevalence ratio(s) for shared sanitation and diarrhea. For the sake of parsimony, we only included variables that made a substantial impact on the PR in our final model, namely the type of sanitation facility (unimproved facility, improved latrine, or improved flush toilet), mother's age and education, the highest level of education in the household, and household ownership of assets.
We conducted country-specific and pooled analyses. In the pooled analyses, surveys were combined by the World Health Organization–defined regions of the world (Africa, Latin America and the Caribbean, Southeast Asia, Western Pacific, Eastern Mediterranean, and Europe), and dummy variables for each survey were included. Because of geographic proximity and the small number of countries in the Western Pacific region, Southeast Asia and Western Pacific were combined as a single region. Because they contained relatively fewer countries, the Eastern Mediterranean and Europe regions were also combined. This change resulted in four distinct regions. We analyzed the data stratified by region to detect any regional patterns or differences. We also conducted an overall pooled analysis by using data from all 51 surveys along with survey fixed effects. All data management and analysis was conducted using STATA 11.2 (StataCorp LP, College Station, TX).
Results
There were 435,205 children less than five years of age included in the analysis (Table 1). Of these children, 30.9% were from households with no sanitation facility. Of children from households with a facility, 45.1% were from households with a facility that was improved (ignoring sharing), and 29.9% were from households that used a shared facility. The amount of sharing varied substantially across countries. The lowest level of sharing was in Armenia (1.4% of those with a facility) and the highest was in Ghana (87.3%). When all 51 surveys were combined, the overall prevalence of diarrhea was 14.3%. Diarrhea prevalence varied substantially across countries from 4.5% in Maldives to 26.2% in Bolivia.
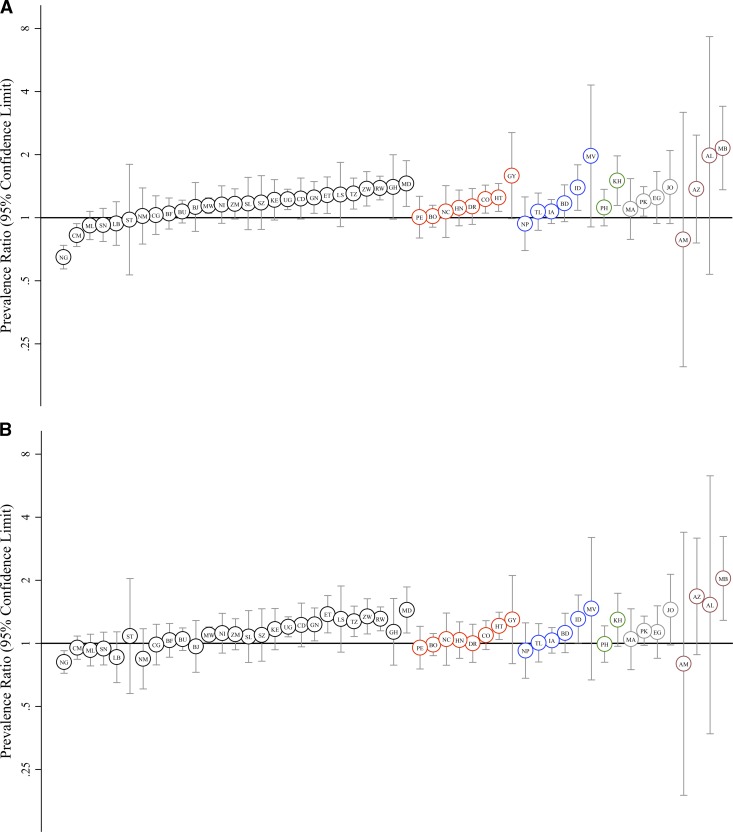
In most countries, the prevalence of diarrhea was higher among households that used a shared toilet facility (Figure 1). This effect of sharing, however, varied across countries. The point estimates of the unadjusted PRs ranged from 0.65 (Nigeria) to 2.15 (Moldova), although only 16 of the 51 unadjusted PRs were significantly different from 1. After adjusting for confounders, many of the point estimates moved towards the null, but some did not. The adjusted PRs ranged from 0.80 (Armenia) to 2.04 (Moldova). There was an apparent clustering of countries in West Africa that showed protective effects, particularly Nigeria, Cameroon, Mali, Senegal, and Liberia. To highlight this geographic pattern, we present the Africa and global estimates with and without West Africa in Table 2.
Figure 1.
Crude and adjusted prevalence ratios for diarrhea comparing those with shared toilet facilities with those with non-shared facilities. Presented for each Demographic and Health Survey (n = 51) conducted during 2001–2011. A, Crude prevalence ratios and 95% confidence intervals. B, Adjusted prevalence ratios and 95% confidence intervals.
Table 2.
Effect of shared sanitation pooled across countries*
| Region and subset of countries | Crude PR (95% CI) | Adjusted† PR (95% CI) |
|---|---|---|
| Africa | 1.07 (1.03–1.10) | 1.05 (1.01–1.09) |
| West Africa‡ | 0.89 (0.84–0.94) | 0.91 (0.86–0.97) |
| Excluding West Africa‡ | 1.19 (1.14–1.25) | 1.15 (1.11–1.21) |
| Latin America and the Caribbean | 1.11 (1.04–1.19) | 1.03 (0.97–1.10) |
| Southeast Asia and Western Pacific | 1.16 (1.06–1.26) | 1.09 (1.01–1.19) |
| Eastern Mediterranean and Europe | 1.26 (1.11–1.42) | 1.20 (1.06–1.36) |
| All regions combined | 1.09 (1.06–1.12) | 1.05 (1.02–1.08) |
| Excluding West Africa‡ | 1.17 (1.14–1.21) | 1.11 (1.08–1.15) |
Shown are prevalence ratios (PRs) and 95% confidence intervals (CIs) for diarrhea for comparisons of households with shared toilet facilities with households with facilities that are not shared. Data were obtained from 51 Demographic and Health Surveys during 2001–2011.
Adjusted for type of facility (flush toilet, improved latrine, unimproved latrine) mother's age, mother's educational attainment, highest level of education in the households, and asset ownership.
West Africa is defined as Benin, Burkina Faso, Cameroon, Ghana, Guinea, Mali, Nigeria, Senegal, and Sierra Leone.
We observed 9% higher prevalence among households that used a shared toilet facility (Crude PR =1.09, 95% CI = 1.06–1.12) when pooling the data across all 51 counties (Table 2). In absolute terms, this finding represents a prevalence difference of 1.2 (95% CI = 0.8–1.6) percentage points. Adjusting for confounding attenuated the effect (adjusted PR = 1.05, 95% CI = 1.02–1.08). This relationship was consistent across three of the four regions. Only the Latin America and Caribbean region differed, where adjusting for confounding eliminated the effect. In the Eastern Mediterranean and Europe region, we observed the largest harmful effect (adjusted PR =1.20, 95% CI = 1.06–1.36). The level of attenuation after adjustment for confounding differed slightly by region. The estimates did not appear to differ when stratified by urban and rural areas.
As mentioned above, there was substantial heterogeneity among countries within each region (Figure 1). This heterogeneity is best illustrated in Africa (Figure 1 and Table 3). The pooled prevalence ratio for a number of countries within Africa are either protective (Nigeria, Cameroon, Mali, Senegal, and Liberia: adjusted PR = 0.86, 95% CI = 0.80–0.93) or exhibit no effect (Sao Tome and Principe, Namibia, Congo, Burkina Faso, and Burundi). In the remaining subsets of countries in Africa, those that use a shared toilet had a 10–32% higher prevalence of diarrhea than those that do not use a shared toilet (Table 3). The countries in Africa that showed a protective effect are all located in West Africa. The patterns within other regions of the world appear similar. In Europe, there was a large degree of heterogeneity between and within countries, possibly attributable to small sample size.
Table 3.
Heterogeneity of the effect of sharing within Africa*
| Countries | Crude PR (95% CI) | Adjusted† PR (95% CI) |
|---|---|---|
| Nigeria, Cameroon, Mali, Senegal, Liberia | 0.82 (0.76–0.88) | 0.86 (0.80–0.93) |
| Sao Tome and Principe, Namibia, Congo, Burkina Faso, Burundi | 1.05 (0.96–1.15) | 1.00 (0.92–1.10) |
| Benin, Malawi, Niger, Zambia, Sierra Leone | 1.15 (1.07–1.23) | 1.10 (1.03–1.18) |
| Swaziland, Kenya, Uganda, Democratic Republic of Congo, Guinea | 1.23 (1.12–1.34) | 1.19 (1.09–1.30) |
| Ethiopia, Lesotho, Tanzania, Zimbabwe, Rwanda, Ghana, Madagascar | 1.35 (1.25–1.45) | 1.32 (1.22–1.42) |
Countries are grouped based on quintiles of the crude prevalence ratio (PR). Shown are PRs and 95% confidence intervals (CIs) for diarrhea for comparisons of households with shared toilet facilities with households with facilities that are not shared.
Adjusted for type of facility (flush toilet, improved latrine, unimproved latrine) mother's age, mother's educational attainment, highest level of education in the household, and asset ownership.
The second way in which we examined the impact of sharing on prevalence was by stratifying exposure by those that share with five or fewer households and those that share with more than five households. These data were available for only 40 of the 51 surveys (Table 1). Except for Africa, the regional estimates were not statistically significant after adjustment for confounders (Table 4). Each sharing category had an increased prevalence compared with the not shared reference group, but the prevalence of diarrhea was not statistically different when we compared a facility that is shared by fewer than five households with a facility that is shared with by five or more households. Only in Southeast Asia, Western Pacific, Eastern Mediterranean, and Europe did there appear to be a dose-response relationship. In other regions, the prevalence of diarrhea did not differ based on the number of households sharing. Therefore, the stratified data provide little evidence for a dose response relationship and no support for a threshold of households for which sharing does not present an increased risk of diarrhea.
Table 4.
Number of households sharing a toilet facility and prevalence ratios for diarrhea among children < 5 years of age*
| Region | Sharing category† | Crude PR (95% CI) | Adjusted‡ PR (95% CI) |
|---|---|---|---|
| Africa | With ≤ 5 households | 1.06 (1.02–1.10) | 1.04 (1.00–1.08) |
| With > 5 households | 1.01 (0.95–1.08) | 1.02 (0.95–1.09) | |
| West Africa§ | With ≤ 5 households | 0.88 (0.82–0.94) | 0.89 (0.83–0.95) |
| With > 5 households | 0.81 (0.73–0.90) | 0.87 (0.79–0.96) | |
| Excluding West Africa§ | With ≤ 5 households | 1.20 (1.15–1.25) | 1.15 (1.10–1.20) |
| With > 5 households | 1.20 (1.10–1.31) | 1.17 (1.08–1.28) | |
| Latin America and the Caribbean | With ≤ 5 households | 1.09 (1.00–1.18) | 1.04 (0.95–1.13) |
| With > 5 households | 1.10 (0.88–1.38) | 1.01 (0.81–1.26) | |
| Southeast Asia and Western Pacific | With ≤ 5 households | 1.13 (1.03–1.25) | 1.08 (0.98–1.18) |
| With > 5 households | 1.27 (1.05–1.55) | 1.21 (0.99–1.46) | |
| Eastern Mediterranean and Europe | With ≤ 5 households | 1.25 (0.93–1.67) | 1.15 (0.85–1.54) |
| With > 5 households | 1.48 (0.67–3.29) | 1.36 (0.63–2.94) | |
| All regions combined | With ≤ 5 households | 1.08 (1.04–1.11) | 1.04 (1.00–1.07) |
| With > 5 households | 1.05 (0.99–1.12) | 1.03 (0.97–1.09) | |
| Excluding West Africa§ | With ≤ 5 households | 1.16 (1.12–1.21) | 1.10 (1.07–1.15) |
| With > 5 households | 1.20 (1.12–1.30) | 1.14 (1.06–1.23) |
Data were obtained from 40 Demographic and Health Surveys during 2001–2011. PR = prevalence ratio; CI = confidence interval.
Reference category is those that use a not shared facility.
Adjusted for type of facility (flush toilet, improved latrine, unimproved latrine) mother's age, mother's education, highest level of education in the household, and ownership of assets.
West Africa is defined as Benin, Burkina Faso, Cameroon, Ghana, Guinea, Mali, Nigeria, Senegal, and Sierra Leone.
The sanitation ladder of JMP is another useful way to examine the impact of sharing on prevalence. By using this classification, we found that households that share sanitation facilities that are otherwise improved can be compared with those that use improved facilities that are not shared. When all 51 surveys are pooled, sharing appeared to be harmful even when the facility was improved (Table 5). The prevalence of diarrhea was 10% lower among households that used a non-shared improved facility compared with facilities that were shared but otherwise improved (crude PR = 0.90, 95% CI = 0.87–0.93). Adjusting for confounding modestly attenuated that effect (adjusted PR = 0.95, 95% CI = 0.91–0.99). The strongest effect observed was the in Eastern Mediterranean and Europe (adjusted PR = 0.83, 95% CI = 0.72–0.94) and Africa when West Africa was excluded (adjusted PR = 0.81, 95% CI = 0.75–0.87). In Latin America and the Caribbean and Southeast Asia and Western Pacific the adjusted effect was not significant.
Table 5.
Sanitation ladder and diarrhea*
| Region | Sanitation ladder category | Crude PR (95% CI) | Adjusted† PR (95% CI) |
|---|---|---|---|
| Africa | No facility | 1.06 (1.01–1.11) | 0.95 (0.90–1.00) |
| Unimproved facility (shared or not shared) | 1.03 (0.98–1.08) | 0.96 (0.92–1.01) | |
| Shared facility (otherwise improved) | 1.00 (Ref.) | 1.00 (Ref.) | |
| Improved facility (not shared) | 0.93 (0.88–0.98) | 0.95 (0.90–1.00) | |
| West Africa‡ | No facility | 1.14 (1.07–1.23) | 0.98 (0.91–1.05) |
| Unimproved facility (shared or not shared) | 1.18 (1.10–1.27) | 1.05 (0.98–1.13) | |
| Shared facility (otherwise improved) | 1.00 (Ref.) | 1.00 (Ref.) | |
| Improved facility (not shared) | 1.11 (1.03–1.20) | 1.10 (1.02–1.19) | |
| Excluding West Africa‡ | No facility | 0.97 (0.91–1.04) | 0.91 (0.84–0.98) |
| Unimproved facility (shared or not shared) | 0.91 (0.85–0.97) | 0.88 (0.82–0.93) | |
| Shared facility (otherwise improved) | 1.00 (Ref.) | 1.00 (Ref.) | |
| Improved facility (not shared) | 0.78 (0.72–0.83) | 0.81 (0.75–0.87) | |
| Latin America and the Caribbean | No facility | 1.24 (1.14–1.35) | 1.12 (1.03–1.22) |
| Unimproved facility (shared or not shared) | 1.13 (1.03–1.24) | 1.09 (0.99–1.19) | |
| Shared facility (otherwise improved) | 1.00 (Ref.) | 1.00 (Ref.) | |
| Improved facility (not shared) | 0.88 (0.81–0.95) | 0.96 (0.89-1.04) | |
| Southeast Asia and Western Pacific | No facility | 1.07 (0.98–1.17) | 1.04 (0.94–1.14) |
| Unimproved facility (shared or not shared) | 1.02 (0.90–1.14) | 0.99 (0.88–1.12) | |
| Shared facility (otherwise improved) | 1.00 (Ref.) | 1.00 (Ref.) | |
| Improved facility (not shared) | 0.90 (0.82–0.98) | 0.95 (0.87–1.04) | |
| Eastern Mediterranean and Europe | No facility | 0.85 (0.73–0.98) | 0.81 (0.69–0.94) |
| Unimproved facility (shared or not shared) | 0.75 (0.63–0.89) | 0.75 (0.63–0.89) | |
| Shared facility (otherwise improved) | 1.00 (Ref.) | 1.00 (Ref.) | |
| Improved facility (not shared) | 0.78 (0.69–0.90) | 0.83 (0.72–0.94) | |
| All regions combined | No facility | 1.08 (1.04–1.12) | 0.99 (0.95–1.02) |
| Unimproved facility (shared or not shared) | 1.03 (0.99–1.07) | 0.98 (0.94–1.02) | |
| Shared facility (otherwise improved) | 1.00 (Ref.) | 1.00 (Ref.) | |
| Improved facility (not shared) | 0.90 (0.87–0.93) | 0.95 (0.91–0.99) | |
| Excluding West Africa‡ | No facility | 1.04 (1.00–1.09) | 0.98 (0.94–1.03) |
| Unimproved facility (shared or not shared) | 0.97 (0.92–1.01) | 0.94 (0.90–0.98) | |
| Shared facility (otherwise improved) | 1.00 (Ref.) | 1.00 (Ref.) | |
| Improved facility (not shared) | 0.83 (0.80–0.87) | 0.89 (0.85–0.93) |
Prevalence ratios (PRs) and 95% confidence intervals (CIs) for diarrhea by level of the Joint Monitoring Program Sanitation Ladder. Data were obtained from 51 Demographic and Health Surveys during 2001–2011. Ref. = referent.
Adjusted for mother's age, mother's educational attainment, highest level of education in the households, and asset ownership.
West Africa is defined as Benin, Burkina Faso, Cameroon, Ghana, Guinea, Mali, Nigeria, Senegal, and Sierra Leone.
The results are less consistent when we compared sharing (otherwise improved) with no facility or unimproved facility (shared or not shared) (Table 5). Whereas the Eastern Mediterranean and Europe showed a protective effect for no facility and unimproved facility (adjusted PR = 0.81, 95% CI = 0.69–0.94 and adjusted PR = 0.75, 95% CI = 0.63–0.89, respectively), the other regions either did not have significant results (Southeast Asia and Western Pacific), was protective in one category (Africa), or was harmful in one category (Latin America and the Caribbean).
Discussion
Our global pooled analysis shows that there was an increased prevalence of diarrhea associated with shared sanitation. This finding is consistent with those of the few studies that have been conducted,9–16 although the effect we observed was more modest and attenuated after adjusting for confounding. However, we also report a high level of between-country heterogeneity, which limits the ability to make inferences from our pooled estimates or from the pooled estimates from previous studies.
One strength of our study was the ability to look at differences across a wide array of countries. In most countries, sharing appears to be harmful. However, in Nigeria and Cameroon, sharing appears to be protective, and in many other countries there was no difference in diarrhea prevalence attributable to sharing. These findings are consistent with the recent systematic review that found that sharing latrines was associated with increased risk (although not always significant) of diarrhea in 10 countries but protective in 1 country (Bangladesh).8 Other research has shown substantial differences among countries in the effectiveness of water, sanitation, and hygiene interventions to prevent disease.17 Such variability between countries, and possibly within countries, makes a single, uniform, global policy particularly difficult. Future research is needed to elucidate circumstances under which sharing is more harmful.
Confounding appears to play an important role in the relationship between shared sanitation and diarrheal disease. Country-specific and pooled prevalence ratios were substantially attenuated when socioeconomic indicators were included in the models. Because households that share are generally of a lower socioeconomic status than those that do not share, they are at increased risk of diarrhea because of poverty in general, not necessarily because of sharing.18 These lower-income households are more likely to have inadequate hygiene practices and consume contaminated food. The type of toilet facility (unimproved latrine, improved latrine, or flush toilet) also explained some of the observed association between shared sanitation and diarrhea but was less important than the socioeconomic variables. In this dataset, shared facilities were less likely to be improved than non-shared facilities, and less likely to use flush technology if improved. The results shown in Table 5, which directly account for type of facility, show similar levels of increased prevalence associated with sharing. Although confounding explains some of observed difference it does not explain all of the differences. Furthermore, the importance of confounding varied across regions, greater in Southeast Asia and Western Pacific, as well as in the Americas than in Africa, the Eastern Mediterranean, and Europe.
In many countries, the adverse effect of sharing was strong even after adjusting for confounding. For example, in Madagascar the prevalence of diarrhea was 44% higher (95% CI = 12–86%) among those with shared facilities than among those with facilities that were not shared, after controlling for socioeconomic variables. In such settings, shared toilets may contribute to the transmission of diarrheal disease. Further research is necessary to substantiate these findings, evaluating whether and to what extent shared sanitation actually increases the risk of disease. Stronger study designs using incidence of diarrhea will enable more robust causal inference in this regard. It is also important to identify the mechanism of transmission and how this can be mitigated. Transmission could be occurring because shared facilities, particularly those that are communally owned, may be more difficult to clean and maintain. Often, some type of institution is required to keep the public facility in good operating condition.5–7,19–21 When such institutions are insufficient or lacking, the quality of the facility is affected. Also, shared facilities of all types may be overused and increase the amount of epidemiologic contact between users. Other than cleanliness, persons may periodically choose to practice open defecation, or some other less hygienic means of excrement disposal, when shared facilities are deemed unsafe or inconvenient because of distance or long lines. Shared latrines may also fill up more rapidly and require more frequent emptying, which raises additional concerns about unsafe sludge management, creating another source of exposure.
In some countries, sharing appears to be protective, a seemingly counterintuitive result. The protective effect was particularly strong in Nigeria, where the prevalence ratio was substantially protective even after adjusting for confounding. Cameroon also initially showed a protective effect, but it was substantially attenuated after adjusting for confounders. Other countries, namely Mali, Senegal, and Liberia, showed a modest protective effect. Interestingly, these countries are clustered in West Africa, and countries in sub-Saharan Africa generally show benign to harmful effects. Further research is necessary to confirm the validity of this protective effect and, if so, the reasons therefor.
The nature of shared sanitation is often different between rural and urban areas.3 Sharing in rural areas is often characterized by sharing with a few neighbors or relatives. In urban areas, particularly in urban slums, many of the shared facilities may be public and used by a large number of households. Unfortunately, the DHS data do not allow enough geographic resolution to differentiate between urban slums and other urban areas, which may explain why we did not detect a difference in the effect of shared sanitation between urban and rural areas.
Our study design has other limitations. It is well documented that using a two-week recall period understates disease status, resulting in bias. Some studies22–24 have suggested that a two-day or three-day recall period will minimize this bias, but Arnold and others25 reported that one week is optimal when accounting for bias and variance. Although the two-week recall period used in the DHS is not ideal, any bias in our results should be towards the null, as long as disease misclassification is unrelated to exposure. Second, like any cross-sectional study, causal inference is limited. Reverse causation seems unlikely in this situation, but we cannot rule out residual confounding. However, the DHS collect many potential confounding variables that we were able to use in these analyses. In particular, we were able to examine how much of the potential increase in harmful effect measured in the analysis was caused by confounding by socioeconomic status and how much was likely caused by an actual increase risk when sharing sanitation. Additional information on handwashing, hygiene practices, and food contamination would enhance these analyses. Also, diarrheal diseases are often seasonal. Cross-sectional studies are unable to detect seasonal trends. Even so, for season to be a confounder, it would need to be associated with exposure (sharing) and not just outcome. In addition, the DHS relies on self-reporting of shared sanitation. A compound may be made up of several households of the same family sharing the same facility. In such situations, sharing (and the number of households sharing) may be underreported.
These results provide additional evidence that shared sanitation is generally a risk factor for diarrhea among children. As a result, our results provide support for the existing policy of the JMP to treat shared sanitation as unimproved. However, our results also provide no evidence of a minimum threshold of households that can share a latrine without increasing the risk. Thus, our findings provide no support for the proposed change in the JMP policy that would encourage sharing of latrines by treating latrines shared among five or fewer households as improved.
At the same time, there are settings in which the relationship is neutral, and in a few it appears to be protective. This heterogeneity among countries suggests that the specific social and economic context matters. Because the number of shared latrines is large and likely to increase, particularly in urban settings, it is important to ascertain under what circumstances sharing can be undertaken safely. Also, because the overall increase in prevalence is modest, shared sanitation could potentially be a low cost intervention. Although shared facilities are clearly not optimal, for the same cost, higher coverage rates could be achieved with shared sanitation compared with private facilities. The higher coverage rates achieved could offset any losses to effectiveness.
One clear conclusion from this analysis is that confounding likely plays an important role in the association between sharing and diarrhea. Adjusting for socioeconomic status attenuates the estimated harmful effect of sharing, suggesting that alternative transmission pathways accounts for some of the differences. However, adjusting for socioeconomic status does not account for all of the differences observed, suggesting that shared sanitation may contribute to the transmission of diarrheal diseases caused by issues of cleanliness and maintenance, overuse, or caused by users occasionally opting for less hygienic means of excreta disposal. Future research should attempt to identify the circumstances that make sharing harmful or protective, better understand confounding and its role, and seek to elucidate the mechanism through which sharing could increase the risk of diarrhea. This information will be crucial to help inform policy decisions.
Footnotes
Financial support: This study was supported by the National Institutes of Health (grant R01-AI050038).
Disclosure: None of the authors have any competing financial interests.
Authors' addresses: James A. Fuller and Joseph N. S. Eisenberg, Department of Epidemiology, University of Michigan School of Public Health, Ann Arbor, MI, E-mails: jafuller@umich.edu and jnse@umich.edu. Thomas Clasen and Marieke Heijnen, Department of Disease Control, London School of Hygiene and Tropical Medicine, London, United Kingdom, E-mails: thomas.clasen@lshtm.ac.uk and marieke.heijnen@lshtm.ac.uk.
References
- 1.Black RE, Cousens S, Johnson HL, Lawn JE, Rudan I, Bassani DG, Jha P, Campbell H, Walker CF, Cibulskis R, Eisele T, Liu L, Mathers C. Child Health Epidemiology Reference Group of WHO and UNICEF, 2010. Global, regional, and national causes of child mortality in 2008: a systematic analysis. Lancet. 375:1969–1987. doi: 10.1016/S0140-6736(10)60549-1. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization Global Health Observatory Data Repository. 2013. http://apps.who.int/gho/data/node.country Available at. Accessed July 12, 2013.
- 3.UNICEF and World Health Organization . Progress on Drinking Water and Sanitation: 2012 Update. Geneva: World Health Organization; 2012. [Google Scholar]
- 4.UNICEF and World Health Organization . Post-2015 Proposal for Sanitation Targets and Indicators. Geneva: World Health Organization; 2012. [Google Scholar]
- 5.Schouten MA, Mathenge RW. Communal sanitation alternatives for slums: a case study of Kibera, Kenya. Phys Chem Earth. 2010;35:815–822. [Google Scholar]
- 6.Wegelin-Schuringa M, Kodo T. Tenancy and sanitation provision in informal settelements in Nairobi: revisiting the public latrine option. Environ Urban. 1997;9:181–190. [Google Scholar]
- 7.Nelson KL, Murray A. Sanitation for unserved populations: technologies, implementation challenges, and opportunities. Annu Rev Environ Resour. 2008;33:119–151. [Google Scholar]
- 8.Heijnen M, Cumming O, Peletz R, Chan GKS, Brown J, Baker K, Clasen T. Shared sanitation versus individual household latrines: a systematic review of health outcomes. PLoS ONE. 2014;9:e93300. doi: 10.1371/journal.pone.0093300. Published April 17, 2014, doi:10.1371/journal.pone.0093300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baker KK, O'Rielly CE, Mintz ED, Farag T, Nasrin D, Panchalingham S, Blackwelder W, Wu Y, Nataro JP, Kotloff KL, Alonso P, Breiman RF, Sur D, Faruque ASG, Zaidi A, Saha D, Sow SO, Levine MM. The risk of moderate and severe diarrhea in children less than five years old is increased among families who share a sanitation facility. Paper presented at the 60th Annual Meeting of the American Society of Tropical Medicine and Hygiene; December 4–8; Philadelphia, PA, United States. 2011. [Google Scholar]
- 10.Khan MU. Limitation of communal latrines in changing the prevalence of parasites and diarrhoeal attack rate in Dhaka peri-urban slums. Environ Pollut. 1987;47:187–194. doi: 10.1016/0269-7491(87)90209-0. [DOI] [PubMed] [Google Scholar]
- 11.Chakraborty AK, Das JC. Comparative study of incidence of diarrhea among children in two different environmental situations in Calcutta. Indian Pediatr. 1983;20:907–913. [PubMed] [Google Scholar]
- 12.Brooks JT, Shapiro RL, Kumar L, Wells JG, Phillips-Howard PA, Shi YP, Vulule JM, Hoekstra RM, Mintz E, Slutsker L. Epidemiology of sporadic bloody diarrhea in rural western Kenya. Am J Trop Med Hyg. 2003;68:671–677. [PubMed] [Google Scholar]
- 13.Shultz A, Omollo JO, Burke H, Qassim M, Ochieng JB, Weinberg M, Feiken DR, Breiman RF. Cholera outbreak in Kenyan refugee camp: risk factors for illness and importance of sanitation. Am J Trop Med Hyg. 2009;80:640–645. [PubMed] [Google Scholar]
- 14.Sobel J, Gomes TA, Ramos RT, Hoekstra M, Rodrigue D, Rassi V, Griffin PM. Pathogen-specific risk factors and protective factors for acute diarrheal illness in children aged 12–59 months in Sao Paulo, Brazil. Clin Infect Dis. 2004;38:1545–1551. doi: 10.1086/420822. [DOI] [PubMed] [Google Scholar]
- 15.Ghosh S, Sengupta PG, Mandal SK, Manna B, Sikder SN, Sirkar BK. Maternal behaviour and feeding practices as determinants of childhood diarrhoea: Some observations amongst rural Bengalese mothers. Indian J Public Health. 1994;38:77–80. [PubMed] [Google Scholar]
- 16.Tuttle J, Ries AA, Chimba RM, Perera CU, Bean NH, Griffin PM. Antimicrobial-resistant epidemic Shigella dysenteriae type 1 in Zambia: modes of transmission. J Infect Dis. 1995;171:371–375. doi: 10.1093/infdis/171.2.371. [DOI] [PubMed] [Google Scholar]
- 17.Whittington D, Jeuland M, Barker K, Yuen Y. Setting priorities, targeting subsidies among water, sanitation, and preventive health interventions in developing countries. World Dev. 2012;40:1546–1568. [Google Scholar]
- 18.Blakely T, Hales S, Kieft C, Wilson N, Woodward A. The global distribution of risk factors by poverty level. Bull World Health Organ. 2005;83:118–126. [PMC free article] [PubMed] [Google Scholar]
- 19.Isunju JB, Schwartz K, Schouten MA, Johnson WP, van Dijk MP. Socio-economic aspects of improved sanitation in slums: a review. Public Health. 2011;125:368–376. doi: 10.1016/j.puhe.2011.03.008. [DOI] [PubMed] [Google Scholar]
- 20.Katukiza AY, Ronteltap M, Oleja A, Niwagaba CB, Kansiime F, Lens PN. Selection of sustainable sanitation technologies for urban slums: a case of Bwaise III in Kampala, Uganda. Sci Total Environ. 2010;409:52–62. doi: 10.1016/j.scitotenv.2010.09.032. [DOI] [PubMed] [Google Scholar]
- 21.Kulabako RN, Nalubega M, Wozei E, Thunvik R. Environmental health practices, constraints and possible interventions in peri-urban settlements in developing countries: a review of Kampala, Uganda. Int J Environ Health Res. 2010;20:231–257. doi: 10.1080/09603120903545745. [DOI] [PubMed] [Google Scholar]
- 22.Ramakrishnan R, Venkatarao T, Koya PK, Kamaraj P. Influence of recall period on estimates of diarrhoea morbidity in infants in rural Tamilnadu. Indian J Public Health. 1999;43:136–139. [PubMed] [Google Scholar]
- 23.Feikin DR, Audi A, Olack B, Bigogo GM, Polyak C, Burke H, Williamson J, Breiman RF. Evaluation of the optimal recall period for disease symptoms in home-based morbidity surveillance in rural and urban Kenya. Int J Epidemiol. 2010;39:450–458. doi: 10.1093/ije/dyp374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zafar SN, Luby SP, Mendoza C. Recall errors in a weekly survey of diarrhoea in Guatemala: determining the optimal length of recall. Epidemiol Infect. 2010;138:264–269. doi: 10.1017/S0950268809990422. [DOI] [PubMed] [Google Scholar]
- 25.Arnold BF, Galiani S, Ram PK, Hubbard AE, Briceño B, Gertler PJ, Colford JM., Jr Optimal recall period for caregiver-reported illness in risk factor and intervention studies: a multicountry study. Am J Epidemiol. 2013;177:361–370. doi: 10.1093/aje/kws281. [DOI] [PubMed] [Google Scholar]