Abstract
Context:
Current holistic rehabilitation blends both physical and psychological techniques. However, validation of the usefulness of psychological strategies is limited in the literature.
Objective:
To quantify the effects of psychological strategies on both physiologic (salivary cortisol) and subjective assessments of stress.
Design:
Randomized controlled clinical trial.
Setting:
Laboratory.
Patients or Other Participants:
A total of 97 college-aged students (age = 20.65 ± 4.38 years), most with little to no experience with psychological strategies.
Intervention(s):
A 15-minute script via an iPod led the participant through visual imagery (cognitive relaxation) or deep breathing exercises (somatic relaxation) cues. The control group listened to 15 minutes of ambient nature sounds.
Main Outcome Measure(s):
Two samples (pretest, posttest) of salivary cortisol were analyzed using an enzyme immunoassay kit; the average was used for statistical analysis. Descriptive statistics and correlations were conducted to examine group differences in time of day, salivary cortisol, sex, Stress-O-Meter values, and Perceived Stress Scale scores.
Results:
Salivary cortisol levels were lower in the treatment group than the control group (F2,97 = 15.62, P < .001). Females had higher scores on both the pretest Stress-O-Meter (5.15 ± 1.796) and the Perceived Stress Scale (18.31 ± 5.833) than males (4.25 ± 1.741 and 15.272 ± 5.390, respectively).
Conclusions:
Both cognitive and somatic relaxation strategies reduced cortisol levels. Participants who received verbal guidance achieved a larger cortisol reduction. However, the change in cortisol level was uncorrelated with the change in report of acute stress; females reported higher levels of stress. Clinical implications include attention to sex when assessing stress and providing coping skills during the rehabilitation process.
Key Words: relaxation, somatic relaxation, cognitive relaxation, cortisol
Key Points:
Cognitive and somatic relaxation strategies were effective in decreasing acute stress as measured by the change in salivary cortisol.
Female college students reported higher levels of acute and chronic stress than their male counterparts.
Athletic trainers should use relaxation strategies and consider sex differences while caring for injured athletes during rehabilitation.
Sport medicine specialists acknowledge the physical and psychological aspects of injury, connecting the mind with the physical healing process.1 The education of athletic trainers includes psychological aspects2 that incorporate cognitive and somatic-based relaxation strategies.3 Cognitive strategies3 focus on thought processes (eg, imagery)4 and somatic-based strategies3 focus on body awareness and breathing (eg, progressive relaxation)5,6 to facilitate healing. Rehabilitation is a challenging time for athletes and often a time of high stress.1 Athletes can learn how to control stress,1 decrease pain,1 reduce reinjury anxiety,3 and reduce return-to-play anxiety by using sport-specific imagery that focuses on sport skills and strategies.7 Athletes can also promote positive self-talk,3 self-motivation,1 and confidence1 during all phases of the rehabilitation process3 via imagery and relaxation.8
Imagery is a cognitive and behavioral relaxation strategy. It connects the mind and body by joining emotion and perceptions with physiologic, behavioral, and psychological responses.9 Imagery encourages individuals to use all their senses to create or recreate a past, present, or future experience.5 Somatic relaxation is a psychological strategy that incorporates breathing exercises3 and is important in the healing process to help reduce muscle tension, which is associated with increased pain and inhibited healing.5 Relaxation strategies also increase blood flow to the brain and skeletal muscles to aid in healing.8 One way of examining the response to sport injury and its effects on the rehabilitation process is via cognitive appraisal models.10 Cognitive appraisal models incorporate both personal and situational factors that influence emotional and behavioral responses.10
Based on the integrated model of response to sport injury of Wiese-Bjornstal et al,10 psychological strategies potentially moderate the resulting negative emotion and behavior after injury. For example, how the athlete perceives the injury and the extent of the disability (personal and situational factors) relates to the degree of negative emotions experienced, potentially affecting healing time and adherence to rehabilitation (behavioral and emotional responses). Ultimately, the manner in which an athlete's personal and situational factors influence the behavioral and emotional responses may determine the recovery outcome. Practicing psychological strategies, including imagery and relaxation, may help rehabilitating athletes by altering their cognitive appraisal of the event, managing the stressors of recovery,9 and thereby promoting optimal healing and a timely return to play.1,10 Generally speaking, imagery and relaxation strategies have been linked to decreases in pain and reinjury anxiety and to increases in muscular strength during rehabilitation.8 These strategies have also been shown to increase overall mobility, coordination, and balance and decrease fatigue, depression, and medical costs.11
Pawlow and Jones6 showed that salivary cortisol was reduced after individuals experienced a simple relaxation exercise. In addition, Johnson12 found that relaxation techniques used during rehabilitation may assist in elevating the mood levels of competitive athletes; however, he did not objectively measure stress via cortisol levels.
Cortisol is a naturally occurring stress hormone in the human body and is associated with the flight-or-fight response.13,14 Physiologically, when an individual experiences stress, the cerebral cortex and hypothalamus initiate a reaction that releases adrenocorticotropic hormone.9,13 After stress, adrenocorticotropic hormone stimulation of the adrenal cortex13 results in release of cortisol.7 Increased cortisol has been linked to adverse health effects, including chronic stress,15 depression,13 and a suppressed immune system.16 Conversely, decreased cortisol is associated with positive mood scores9 and reduced perceived stress10 and anxiety levels.6 As a result of lower levels of stress, individuals may experience decreased pain1,4 and reinjury anxiety4 and improved healing.1
Quantifying the effects of relaxation and imagery strategies that reduce cortisol will allow us to validate the usefulness of psychological strategies for athletic training practitioners rehabilitating injured athletes. Research shows that a simple 15-minute relaxation exercise can decrease stress17 and that imagery techniques promote healing and manage pain when used during rehabilitation.1 Further investigation is needed to examine a stress biomarker (cortisol) and the use of psychological strategies during rehabilitation from athletic injury.
This research aims to enhance the implementation of psychological strategies and provides a rationale for the usefulness of imagery and relaxation as everyday tools in the athletic training room. Quantifying the effects of relaxation and imagery strategies will provide athletic training practitioners rehabilitating injured athletes with evidence-based practice. Therefore, our goals were to examine whether (1) the use of cognitive relaxation or somatic relaxation strategies decreased salivary cortisol levels, (2) a correlation exists between objective (salivary cortisol level) and subjective reports of stress (perceived stress scale14,18 and Stress-O-Meter14), and (3) perceived stress levels differ between females and males (prior research demonstrated sex differences within the rehabilitation process).
METHODS
Participants
Participants were 97 undergraduate students (age range, 18 to 46 years; mean = 20.65 ± 4.38 years) from a western university. Of the participants, 33.0% were males (n = 32) and 67.0% were females (n = 65). Most participants reported either no previous experience with guided imagery or relaxation (53.0% [n = 51]) or minimal imagery experience (40.0% [n = 39]); 7.0% (n = 7) reported moderate imagery experience, and none reported advanced imagery experience (Table 1). Data were not collected on injured athletes due to time restraints and lack of currently injured participants. The study was approved by the university's institutional review board, and participants were required to provide a signed informed consent form before data collection. All participants were randomly assigned to 1 of the following groups: cognitive treatment group, somatic treatment group, or control group. The design of this experiment was randomized, double blinded, with a control group.
Table 1.
Imagery Experience by Sex and Treatment Group
| Sex |
Treatment Group |
Imagery Experiencea |
|||
| None |
Minimal |
Moderate |
Advanced |
||
| Male (n = 32) | Cognitive intervention | 9 | 1 | 1 | 0 |
| Somatic intervention | 6 | 5 | 0 | 0 | |
| Control | 6 | 3 | 1 | 0 | |
| Female (n = 65) | Somatic intervention | 14 | 10 | 1 | 0 |
| Cognitive intervention | 10 | 10 | 3 | 0 | |
| Control | 6 | 10 | 1 | 0 | |
| Total (N = 97) | 51 | 39 | 7 | 0 | |
Imagery experience was categorized as none (0), minimal (1), moderate (2), or advanced (3).
Instrumentation
Stress-O-Meter (SOM)
The Stress-O-Meter (SOM) is a Likert scale that ranges from 1 (extremely relaxed and peaceful) to 10 (very high levels of stress). The SOM represents the individual's personal evaluation of his or her current level of stress. This measure has been widely used and has good validity and reliability.14 We used the SOM1 during the pretest survey and the SOM2 during the posttest survey.
Perceived Stress Scale (PSS)
The Perceived Stress Scale (PSS) is commonly used to evaluate an individual's chronic stress level, including thoughts and feelings over the past month.14 Participants are instructed to answer 10 questions using a scale from 0 (never) to 4 (very often). The PSS has a total of 40 possible points. A score of 0–13 is considered a low perceived stress level, 14–26 is a moderate perceived stress level, and 27–40 is a high perceived stress level. According to Olpin and Hesson,14 the PSS has strong validity and reliability and is widely used to measure chronic stress levels.
Heart Rate and Blood Pressure
Heart rate and blood pressure (HR/BP) were taken in the right arm with an automated digital blood pressure monitor (model HEM–907XL; OMRON Corporation, Kyoto, Japan). Two readings were taken 1 minute apart, and the average was recorded. This monitor meets the Association for the Advancement of Medical Instrumentation criteria, and validity and reliability have been verified.19
Psychological Strategies (Audio Script)
The cognitive relaxation treatment focused on using verbal cues through imagery as the script described a quiet forest scene and a calm lake in the mountains. A sample of audio text is “Picture a beautiful mountain scene … imagine closing your eyes and just listening, feeling the peacefulness, the restfulness of this place … let go of all your worries and tension.” The imagery script is available at http://www.rhapsody.com/artist/dr-michael-olpin/album/stress-relief-deep-relaxation-exercises and listed under “Guided Imagery—Mountain Lake.”
The somatic relaxation treatment focused on using verbal cues to relax the body and muscles through progressive relaxation. A sample of audio text is
Let your attention focus on your arms and legs … repeat to yourself “my arms and legs feel heavy” … letting your arms and legs go completely limp, be aware of the feelings of relaxation. Gently allow these feelings to spread throughout your body as you continue your slow deep breathing.
The relaxation script is available at http://www.rhapsody.com/artist/dr-michael-olpin/album/stress-relief-deep-relaxation-exercises and listed under “Autogenics.” The control treatment included nature sounds that were generated by a binaural beat program called “Presleep Induction: Calm Ocean with Occasional Seagulls Calling,” which can be found at http://itunes.apple.com/us/app/binaural-beats/id295143646?mt=8. The background nature sounds of the control treatment consisted of seagull calls, blowing breezes, and ocean waves and were deemed highly similar to the treatment conditions by 3 experts in mental-skills training. The control script did not contain verbal audio cues.
Procedures
Participants were recruited through personal contact by the principal investigator (PI) and research assistants and the use of sign-up sheets on a research board in the psychology department. Each participant was contacted using a phone script, and an official appointment was set up. Participants were reminded that they were not allowed to eat anything (including gum, mints, and candy), use tobacco products, brush their teeth, or drink anything besides water 60 minutes before their scheduled appointment at the Stress Lab. They received a reminder of their scheduled appointment 1 day before via a telephone call, e-mail, or text message (or several of these).
As participants arrived at the Stress Lab, they were asked if they followed the preparation procedure outlined above while they sat for 15 minutes to allow for HR and BP to stabilize. If they had consumed anything other than tap water or had not followed the required protocol during the prior 60 minutes (pertinent for cortisol sampling), they were asked to reschedule the appointment. Each participant was assigned a random numbered packet that included all the testing materials and a treatment group assignment. Participants completed the SOM pretest and PSS.
Before the saliva sample was collected, 2 cryogenic vials were clearly labeled with the participant's randomly assigned number, date (month/day/year), and saliva sample 1 or 2 (SS1, SS2). When taking the saliva sample from the participant, the researcher wore gloves to comply with the standards set by Occupational Safety and Health Administration. The saliva was collected by having the participant salivate into a 1-cc vial. If the participant was unable to provide a sample immediately due to dry mouth, he or she was allowed to chew a piece of plastic paraffin film to activate salivary gland secretion. If the participant was still unable to successfully salivate into the vial, the researcher used a sterile straw.
Once the saliva sample was obtained, the vial was sealed and immediately placed into a cryostorage box, which was then placed in an ultralow storage freezer (−80°C), where it remained until the cortisol was analyzed (High Sensitivity Salivary Cortisol Enzyme Immunoassay Kit; Salimetrics LLC, State College, PA). The PI or research assistant then measured the participant's HR and BP. The HR/BP machine was preset to the “typical” setting; the average of 2 HR/BP readings 1 minute apart was calculated for each participant.
Upon completion of the pretest measures, the participant was led into the main Stress Lab and seated in 1 of 2 recliners. Each participant was given a set of noise-reduction headphones and an iPod unit (4th generation; Apple, Cupertino, CA) corresponding with the randomly assigned group. The iPods were preloaded with the scripts, and each iPod was labeled A, B, or C. Neither the PI nor the participants were aware of the script assignment. The lighting in the Stress Lab was dim. The participant was instructed to follow the auditory script and wait in the chair for the PI when the script ended. Each person was asked if he or she had any questions before listening to the auditory script. After resolving any questions, the PI began playing the script, left the room, and set a timer to 15 minutes. When the script (and timer) ended, the participant was asked to sit at the processing table, where a second saliva sample (SS2), HR, and BP were taken. Each person spent approximately 60 minutes in the Stress Lab.
RESULTS
The total number of participants for this study was 97 (3 participants were excluded from the analyses because of incomplete data). Participants were randomly assigned to the cognitive treatment condition (35.1%, n = 34), the somatic treatment condition (37.1%, n = 36), or the control condition (27.8%, n = 27). Univariate normality was assessed, and the detrended normal P plots of SS1 and SS2 displayed normal distributions.20
The cortisol reduction was different between the treatment groups (F2,97 = 15.62, P < .0010). Post hoc Tukey tests revealed that together, the cognitive (−0.42433) and somatic (−0.56069) groups were different from the control group (−0.23669) but not different from each other (0.33102). Participant reports of acute stress were different from preintervention to postintervention (F2,97 = 0.693, P < .000). However, the subjective reports were uncorrelated with physiologic stress (cortisol level; Table 2).
Table 2.
Average Pretest and Posttest Scores by Sex and Treatment Group
| Sex |
Treatment Group |
Number of Participants |
Saliva Sample, μg/dL |
Heart Rate, bpma |
Blood Pressure, mm Hg (systolic)a |
Blood Pressure, mm Hg (diastolic)a |
||||
| 1 |
2 |
1 |
2 |
1 |
2 |
1 |
2 |
|||
| Male (n = 32) | Cognitive intervention | 11 | 1.246 | 1.090b | 75.5 | 73.8 | 131.1 | 128.3 | 72.2 | 70.8 |
| Somatic intervention | 11 | 1.541 | 1.236b | 74.6 | 70.5 | 127.2 | 123.2 | 73.2 | 70.9 | |
| Control | 10 | 1.295 | 1.584c | 73 | 71.4 | 128.0 | 123.5 | 75.9 | 71.1 | |
| Female (n = 65) | Cognitive intervention | 23 | 2.029 | 1.835b | 76.4 | 72.0 | 115.0 | 113.2 | 72.2 | 70.2 |
| Somatic intervention | 25 | 2.130 | 1.798b | 77.3 | 72.9 | 116.4 | 113.3 | 71.6 | 70.6 | |
| Control | 17 | 0.984 | 1.201c | 75.2 | 75.1 | 112.4 | 110.7 | 70.2 | 67.8 | |
No differences were found between groups (P > .05).
Cognitive-intervention and somatic-intervention groups were different from the control group (P > .001) but not from each other.
Cortisol level was greater in saliva sample 2 than saliva sample 1.
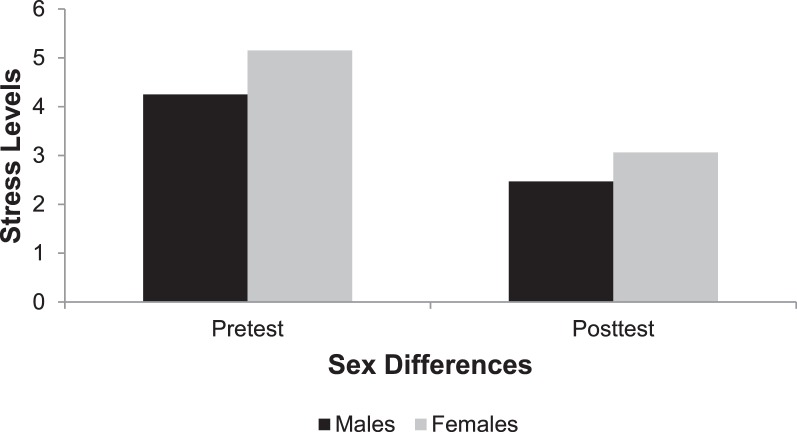
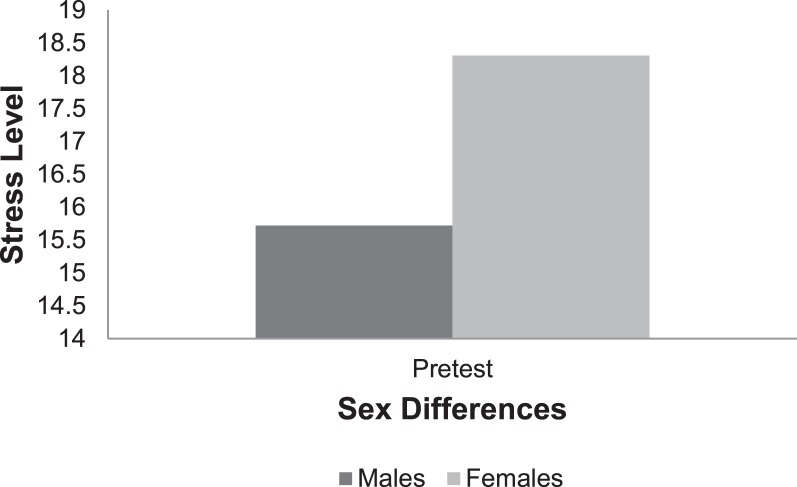
When comparing sexes, the cortisol reduction postintervention was not different (F1,96 = 2.467, P < .120). However, sex differences were evident when we compared subjective stress levels on the SOM (SOM1 = 4.86 ± 1.82 [range, 1–8], SOM2 = 2.87 ± 1.404 [range, 1–6]) and the PSS (0.038). Sex was correlated with the SOM1 (r = 0.235) and the PSS (r = 0.211) at the P < .05 level. Females reported higher scores on both the SOM1 (5.15 ± 1.796) and the PSS (18.31 ± 5.833) compared with males (SOM1 = 4.25 ± 1.741; Figure 1, and PSS = 15.272 ± 5.390; Figure 2). We used analysis of variance to assess significant differences at the P < .01 level: SOM1 and SOM2 (r = 0.693), SOM1 and PSS (r = 0.656), and SOM2 and PSS (r = 0.526).
Figure 1.
Stress-O-Meter results for pretest and posttest by sex.
Figure 2.
Perceived Stress Scale results at pretest by sex.
Time of day was correlated with SS1 (r = −0.212) and SS2 (r = −0.200) results at the 0.05 level. However, cortisol level was not correlated with time of day. No difference was noted in HR/BP across the treatment and control groups.
DISCUSSION
Our primary findings were that participants who experienced a relaxation strategy (cognitive or somatic) experienced a physiologic change in the stress hormone cortisol, and females reported higher levels of stress than their male counterparts.21 Even though nature sounds have been found to be beneficial in decreasing stress22 and increasing relaxation,23 they were not beneficial in decreasing cortisol levels in this study. In fact, the condition involving nature sounds alone actually resulted in an increase in cortisol levels. In current research,24 the easiest and most effective relaxation strategy has been identified as somatic relaxation and breath control. Our results support that finding: the somatic relaxation strategy had the greatest effect on cortisol reduction even though it was not different from the cognitive relaxation strategy.
Consistent with our study, Pawlow and Jones6 found that postintervention salivary cortisol levels were decreased after a brief 20-minute relaxation exercise and self-reported relaxation was increased. Uedo et al17 demonstrated that listening to music during a 15-minute medical procedure resulted in lower pain levels and decreased salivary cortisol levels. Athletes, particularly females, are susceptible to stress throughout practice and competition.25 We found that females reported higher scores on both the SOM1 and the PSS as compared with males on the SOM 1 and PSS. Females may report higher levels of stress than males because of physiologic differences involving the hypothalamic-pituitary-adrenal axis and the menstrual cycle.26 The hypothalamic-pituitary-adrenal axis response may affect the manner in which a female's autonomic nervous system responds to stress from work responsibilities,25,27 finances,28 marital stress,25,27 taking care of children,25 and depression.27 Given these reports of greater stress, athletic trainers and other allied health practitioners should be sensitive to the specific needs of the female athlete during rehabilitation.
No sex differences were found for the reduction in cortisol, which is consistent with the findings of Watanabe et al9 and Alderling et al.29 Even though females reported higher levels of acute and chronic stress over the past 1–30 days, their cortisol levels did not reflect their perception of chronic stress. According to Gallagher et al,30 cortisol helps to maintain normal BP and blood sugar levels and influences the way the human body regulates and metabolizes carbohydrates, fat, and protein. Higher levels of cortisol may be a precursor to numerous health concerns with adverse reactions on an individual's immune system,6,15 including fluctuations in BP31 and weight32; therefore, decreased levels of cortisol should improve an individual's immune system and result in better healing.
Athletic trainers play a key role in injury prevention during competition and rehabilitation. Just as athletes train their physical bodies for competition, they can train their minds to gain psychological health benefits.33 Relaxation and imagery strategies show positive results and, therefore, would be beneficial during rehabilitation.1 A well-balanced rehabilitation plan incorporates the mind and body to optimize healing. Injured athletes may improve their health, prevent disease, and decrease recovery time through their devotion to spirituality34 and use of cognitive and somatic relaxation strategies. Although we have addressed the usefulness of relaxation and imagery strategies to reduce cortisol levels, additional research would be beneficial to evaluate the application of psychological strategies to decrease stress in athletes as a prevention or care modality.
Clinical Implications
According to the Psychosocial Strategies and Referral2 content area developed by the Executive Council on Education, motivational techniques and psychological strategies should be implemented in the clinical setting. Those techniques and strategies include imagery, relaxation, and verbal motivations throughout the injury rehabilitation and reconditioning phases. Astin et al35 found that using psychological techniques has positive effects on health and the immune system; they also suggested that psychological control may be restored during times of physical illnesses to help limit the effect of stress on the body's immune function. As new research continues to be conducted, athletic trainers should move to incorporate this evidence-based practice into their workplace.
Limitations
When we collect data on cortisol, it is important to consider the time of day, its relation to stress, and its half-life. Research36 suggests the best time to sample cortisol is between 7:00 am and 10:00 am because of the natural circadian rhythm of cortisol, which results in hormone fluctuations throughout the day. The highest, more stable cortisol levels occur in the morning and the lowest levels occur in the evening.29,37 In our study, samples were taken from 43 of 97 participants (44.3%) between 7:00 am and 10:00 am, but time of day was not significant in relation to the cortisol level (F1,96 = 1.071, P < .396). Even though the circadian rhythm is presumed to influence hormone fluctuations throughout the day, it did not affect the morning or evening participants. The implications of this finding may allow future cortisol studies to be conducted throughout the day, not just in the morning.
The half-life of cortisol is 73 to 155 minutes,36 but this can vary due to internal stress and environmental factors. Participants remained in our laboratory for 30 to 45 minutes postintervention, yet the effect of the relaxation script may continue after their departure from the lab setting. Future researchers should retain the participants in the lab for 1 to 2 hours postintervention to study the sustained or residual effects on cortisol. The use of medications, alcohol, or an inhaler within 12 hours of salivary cortisol collection should be documented because of possible interference with cortisol levels. In addition, future investigators should aim to collect cortisol data at a consistent time point for all participants, which could minimize this limitation.
Our analysis of sex differences may have been limited by a disproportionate sample and by not taking into account the phase of the menstrual cycle. Estrogen increases from days 7 to 14 in a 28-day menstrual cycle and peaks right before ovulation, which is typically about day 14, before it decreases.13 Future authors should examine estrogen (17β estradiol) as an important biomarker in an attempt to isolate sex differences when analyzing cortisol.38 Subjective reports regarding phase of the menstrual cycle may be used in lieu of 17β estradiol levels, but the accuracy of reporting may differ. Future researchers examining the effects of relaxation strategies on reduction of cortisol would benefit by including female self-reports of their phase of the menstrual cycle as well as paying attention to the time of day when cortisol levels are checked.
CONCLUSIONS
Athletic trainers are in an ideal position to implement psychological strategies due to the proximity and frequency with which they interact with athletes. Rehabilitation of an injured athlete should focus not only on the physical healing aspect but also on psychological healing. Athletes can benefit from using cognitive and somatic-based psychological strategies throughout rehabilitation and progression to return to play. Based on the results of our study, injured athletes may be able to decrease their stress levels by using these relaxation strategies, which may positively affect their cognitive appraisals and resulting behaviors related to return to play. However, athletic trainers and other allied health care professionals should be proficient in the use of psychological assessments and strategies and sensitive to the female athlete and her increased need for coping skills to manage the stressors of life and rehabilitation.
REFERENCES
- 1.Evans L, Hare R, Mullen R. Imagery use during rehabilitation from injury. J Imagery Res Sport Phys Activity. 2006;1(1):1–19. [Google Scholar]
- 2.National Athletic Trainers' Association. Athletic Training Educational Competencies. 5th ed. Dallas, TX: National Athletic Trainers' Association; 2011. [Google Scholar]
- 3.Monsma EV. Psychological response to injury and interventions. In: Mensch JM, Miller GM, editors. The Athletic Trainer's Guide to Psychological Intervention and Referral. Thorofare, NJ: SLACK Incorporated; 2008. pp. 186–189. [Google Scholar]
- 4.Law B, Driediger M, Hall C, Forwell L. Imagery use, perceived pain, limb functioning and satisfaction in athletic injury rehabilitation. J Physiother. 2006;34(1):10–16. [Google Scholar]
- 5.Dworsky D, Krane V. Using the mind to heal the body: imagery for injury rehabilitation. 2009. http://www.appliedsportpsych.org/resource-center/injury-&-rehabilitation/articles/imagery. Accessed September 20.
- 6.Pawlow LA, Jones GE. The impact of abbreviated progressive muscle relaxation on salivary cortisol. Biol Psychol. 2002;60(1):1–16. doi: 10.1016/s0301-0511(02)00010-8. [DOI] [PubMed] [Google Scholar]
- 7.Monsma E, Mensch J, Farrol J. Keeping your head in the game: sport-specific imagery and anxiety among injured athletes. J Athl Train. 2009;44(4):410–417. doi: 10.4085/1062-6050-44.4.410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cupal D, Brewer BW. Effects of relaxation and guided imagery on knee strength, reinjury anxiety, and pain following anterior cruciate ligament reconstruction. Rehabil Psychol. 2001;46(1):28–43. [Google Scholar]
- 9.Watanabe E, Fukuda S, Hara H, Maeda Y, Ohira H, Shirakawa T. Differences in relaxation by means of guided imagery in a healthy community sample. Altern Ther Health Med. 2006;12(2):60–66. [PubMed] [Google Scholar]
- 10.Weise-Bjornstal DM, Smith AM, Shaffer SM, Morrey MA. An integrated model of response to sport-injury: psychological and sociological dynamics. J Appl Sport Psychol. 1998;10(1):46–69. [Google Scholar]
- 11.Persson AL, Veenhuizen H, Zachrison L, Gard G. Relaxation as treatment for chronic musculoskeletal pain; a systematic review of randomised controlled studies. Phys Ther Rev. 2008;13(5):355–365. [Google Scholar]
- 12.Johnson U. Short-term psychological intervention: a study of long-term-injured competitive athletes. J Sport Rehabil. 2000;9(3):207–218. [Google Scholar]
- 13.Shier D, Butler J, Lewis R. Hole's Essentials of Human Anatomy & Physiology. 10th ed. New York, NY: McGraw-Hill; 2006. [Google Scholar]
- 14.Olpin M, Hesson M. Stress Management for Life: A Research-Based, Experimental Approach. 2nd ed. Belmont, CA: Wadsworth, Cengage Learning; 2010. Self-assessment; pp. 17–19. [Google Scholar]
- 15.Innes KE, Vincent HK, Taylor AG. Chronic stress and insulin resistance-related indices of cardiovascular disease risk, part 1: neurophysiological responses and pathological sequelae. Altern Ther Health Med. 2007;13(4):46–52. [PubMed] [Google Scholar]
- 16.Segerstrom SC, Miller GE. Psychological stress and the human immune system: a meta-analytic study of 30 years of inquiry. Psychol Bull. 2004;130(4):601–630. doi: 10.1037/0033-2909.130.4.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Uedo N, Ishikawa H, Morimoto K, et al. Reduction in salivary cortisol level by music therapy during colonoscopic examination. Hepatogastroenterology. 2004;51(56):451–453. [PubMed] [Google Scholar]
- 18.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–396. [PubMed] [Google Scholar]
- 19.Ostchega Y, Nwankwo T, Sorlie PD, Wolz M, Zipf G. Assessing the validity of the OMRON HEM-907XL oscillometric blood pressure measurement device in a National Survey environment. J Clin Hypertens (Greenwich) 2010;12(1):22–28. doi: 10.1111/j.1751-7176.2009.00199.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Park HM. Univariate Analysis and Normality Test Using SAS, Stata, and SPSS. Bloomington, IN: The University Information Technology Services Center for Statistical and Mathematical Computing, Indiana University; 2008. 2011. http://www.indiana.edu/∼statmath/stat/all/normality/. Accessed February 11. [Google Scholar]
- 21.Clement D, Hamson-Utley J, Arvinen-Barrow M, Kamphoff C, Zakrajsek RA, Martin SB. College athletes expectations about injury rehabilitation with an athletic trainer. Intl J Athl Ther Train. 2012;17(4):18–27. [Google Scholar]
- 22.Alvarsson JJ, Wiens S, Nilsson ME. Stress recovery during exposure to nature sound and environmental noise. Int J Environ Res Public Health. 2010;7(3):1036–1046. doi: 10.3390/ijerph7031036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krout RE. Music listening to facilitate relaxation and promote wellness: integrated aspects of our neurophysiological responses to music. Arts Psychother. 2007;34(2):134–141. [Google Scholar]
- 24.Hanrahan SJ, Andersen MB. In: Routledge Handbook of Applied Sport Psychology: A Comprehensive Guide for Students and Practitioners. Routledge Taylor, Group; Francis., editors. New York, NY: 2010. pp. 474–488. [Google Scholar]
- 25.Wang HX, Leineweber C, Kirkeeide R, et al. Psychological stress and atherosclerosis: family and work stress accelerate progression of coronary disease in women: the Stockholm Female Coronary Angiography Study. J Intern Med. 2007;261(3):245–254. doi: 10.1111/j.1365-2796.2006.01759.x. [DOI] [PubMed] [Google Scholar]
- 26.Kajantie E, Phillips DI. The effects of sex and hormonal status on the physiological response to acute psychosocial stress. Psychoneuroendocrinology. 2006;31(2):151–178. doi: 10.1016/j.psyneuen.2005.07.002. [DOI] [PubMed] [Google Scholar]
- 27.Block JP, He Y, Zaslavsky AM, Ding L, Ayanian JZ. Psychosocial stress and change in weight among US adults. Am J Epidemiol. 2009;170(2):181–192. doi: 10.1093/aje/kwp104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lundberg U, Frankenhaeuser M. Stress and workload of men and women in high-ranking positions. J Occup Health Psychol. 1999;4(2):142–151. doi: 10.1037//1076-8998.4.2.142. [DOI] [PubMed] [Google Scholar]
- 29.Alderling M, Theorell T, Torre B, Lundberg I. The demand control model and circadian saliva cortisol variations in a Swedish population based sample (The PART study) BMC Public Health. 2006;6:288. doi: 10.1186/1471-2458-6-288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gallagher P, Leitch MM, Massey AE, McAllister-Williams RH, Young AH. Assessing cortisol and dehydroepiandrosterone (DHEA) in saliva: effects in collection methods. J Psychopharmacol. 2006;20(5):643–649. doi: 10.1177/0269881106060585. [DOI] [PubMed] [Google Scholar]
- 31.Seaward BL. Managing Stress Principles and Strategies for Health and Well-Being. Sudbury, MA: Jones & Bartlett Publishers; 2002. 3rd ed. [Google Scholar]
- 32.Adam TC, Epel ES. Stress, eating, and the reward system. Physiol Behav. 2007;91(4):449–558. doi: 10.1016/j.physbeh.2007.04.011. [DOI] [PubMed] [Google Scholar]
- 33.Greenlees I. The effect of mental skills training package on gymnasium triathlon performance. Sport Psychol. 2003;15(2):127–141. [Google Scholar]
- 34.Culliford L. Spirituality and clinical care. BMJ. 2002;325:1434. doi: 10.1136/bmj.325.7378.1434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Astin JA, Shapiro SL, Lee RA, Shapiro DH., Jr The construct of control in mind-body medicine: implications for healthcare. Altern Ther Health Med. 1999;5(2):42–47. [PubMed] [Google Scholar]
- 36.Iranmanesh A, Lizarralde G, Johnson ML, Veldhuis JD. Dynamics of 24-hour endogenous cortisol secretion and clearance in primary hypothyroidism assessed before and after partial thyroid hormone replacement. J Clin Endocrinol Metab. 1990;70(1):155–161. doi: 10.1210/jcem-70-1-155. [DOI] [PubMed] [Google Scholar]
- 37.Kalman BA, Grahn RE. Measuring salivary cortisol in the behavioral neuroscience laboratory. J Undergrad Neurosci Educ. 2004;2(2):A41–A49. [PMC free article] [PubMed] [Google Scholar]
- 38.Ahmad S, Schmolesky M, Hansen R. 5th Annual Utah Conference for Undergraduate Research. Ogden, Utah: 2011. Effect of physical exercise duration on brain derived neurotrophic factor in healthy women. Paper presented at. February 22. [Google Scholar]