Abstract
Context:
Abnormal movement patterns have been implicated in lower extremity injury. Reliable, valid, and easily implemented assessment methods are needed to examine existing musculoskeletal disorders and investigate predictive factors for lower extremity injury.
Objective:
To determine the reliability of experienced and novice testers in making visual assessments of lower extremity movement patterns and to characterize the construct validity of the visual assessments.
Design:
Cross-sectional study.
Setting:
University athletic department and research laboratory.
Patients or Other Participants:
Convenience sample of 30 undergraduate and graduate students who regularly participate in athletics (age = 19.3 ± 4.5 years). Testers were 2 experienced physical therapists and 1 novice postdoctoral fellow (nonclinician).
Main Outcome Measure(s):
We took videos of 30 athletes performing the single-legged squat. Three testers observed the videos on 2 occasions and classified the lower extremity movement as dynamic valgus, no change, or dynamic varus. The classification was based on the estimated change in frontal-plane projection angle (FPPA) of the knee from single-legged stance to maximum single-legged squat depth. The actual FPPA change was measured quantitatively. We used percentage agreement and weighted κ to examine tester reliability and to determine construct validity of the visual assessment.
Results:
The κ values for intratester and intertester reliability ranged from 0.75 to 0.90, indicating substantial to excellent reliability. Percentage agreement between the visual assessment and the quantitative FPPA change category was 90%, with a κ value of 0.85.
Conclusions:
Visual assessments were made reliably by experienced and novice testers. Additionally, movement-pattern categories based on visual assessments were in excellent agreement with objective methods to measure FPPA change. Therefore, visual assessments can be used in the clinic to assess movement patterns associated with musculoskeletal disorders and in large epidemiologic studies to assess the association between lower extremity movement patterns and musculoskeletal injury.
Key Words: movement analysis, screening, athletic injuries, knee valgus
Key Points
With training and the use of standardized techniques, both experienced and novice testers reliably classified lower extremity movement patterns based on visual assessment.
Movement-pattern category-based visual assessments were in excellent agreement with objective methods to measure changes in frontal-plane projection angle.
Visual assessment based on the methods described in this study may be used in the clinical setting, as well as in large epidemiologic studies and screening assessments for sport participation, to identify distinct categories of lower extremity movement patterns.
Abnormal movement patterns of the lower extremity have been implicated in noncontact anterior cruciate ligament (ACL) injuries1 and other musculoskeletal problems, such as patellofemoral pain2–4 and acetabular labral tears.5 In addition, correcting these abnormal movement patterns has been shown to prevent ACL injury6 and is proposed to reduce symptoms in people with preexisting pain conditions.5,7,8 Thus, assessment of lower extremity movement patterns may be a way to guide treatment of existing musculoskeletal pain problems and to identify people at risk for future injury or musculoskeletal pain. To facilitate the examination of existing musculoskeletal disorders and the investigation of predictive factors of lower extremity injury, reliable, valid, and feasible methods to assess lower extremity movement patterns are needed.
One method to assess lower extremity movement patterns is the Landing Error Scoring System (LESS).9–11 The LESS uses a standard technique to make visual assessments of movement patterns during a drop vertical jump. The LESS is reliable and valid9–11; however, the drop vertical jump is a relatively high-level activity and may not be the best way to assess movement patterns in patients with existing injury or in athletes whose sports do not involve landing from a jump. In addition, the drop vertical jump is a bilateral activity that may allow the participant to use 1 limb to compensate for the other. Visual assessment of the single-legged squat (SLSquat), a unilateral limb task, may provide an alternative to the LESS.
We have developed standardized methods using a visual assessment of the frontal-plane projection angle (FPPA) to classify the lower extremity movement pattern during an SLSquat. The FPPA is a 2-dimensional (2-D) representation of the lower extremity position12 and has been used to identify differences between men and women12 and between women with patellofemoral pain and control participants4,13 and to detect change in movement patterns after specific training.14 We established specific criteria to define the categories of lower extremity movement pattern based on the change in FPPA (FPPA change) during motion. The tester observes the angle formed between a line that bisects the thigh and a line that bisects the lower leg. During movement tests, the tester compares the FPPA at the start position with the FPPA at the end position. For example, to assess an SLSquat, the examiner compares the FPPA during the start position of single-legged stance with the end position of maximum squat depth. The difference observed in FPPA from the start to the end position can then be classified as dynamic valgus (change in the valgus direction), no change, or dynamic varus (change in the varus direction). We have used this assessment extensively in the clinical setting, but we have not assessed the rater reliability or the construct validity of our visual assessments.
The purpose of this study was to assess the intratester and intertester reliability of 3 testers (2 experienced, 1 novice) categorizing the lower extremity movement pattern demonstrated during an SLSquat. A standardized protocol was used to assess videos of healthy participants performing the SLSquat. We hypothesized that the testers, both experienced and novice, would demonstrate good to excellent reliability using the standardized methods. In addition, we used the objective measure of quantifying FPPA as described by Willson and Davis12 to determine the construct validity of our visual assessments. We hypothesized that we would see good to excellent agreement between our visual assessments and the quantitative FPPA change.
METHODS
Participants
Participants were a subset of a prospective cohort study developed to assess risk factors for athletic injury. The cohort was a convenience sample including both undergraduate and graduate students who were regularly involved in athletics. All participants were 18 years of age or older and were recruited for involvement in the longitudinal study that included a focused examination of hip range of motion and hip muscle strength, provocative tests to assess for hip joint injury, and movement-pattern assessment. As part of the study, participants were videotaped performing an SLSquat. Data collection occurred over 2 years. Volunteers with an existing injury that limited their ability to undergo the examination items were excluded. Before the study began, all participants read and signed an informed consent statement approved by the Washington University Human Research Protection Office.
Movement Task and Video-Taping Procedures
We used a standardized method to collect videos of the SLSquat. A digital camera (Cyber-Shot DSC-w100; Sony Corporation, Tokyo, Japan) was placed on a tripod at the level of the participant's knee and approximately 2 m anterior to the participant.12 The image taken included the participant's feet to the midthoracic region throughout the entire movement. To eliminate the effect of shoe wear on limb movement, participants removed their shoes before testing.
A research assistant instructed the participant in the movement and performed the video capture. The research assistant described and demonstrated the SLSquat to the participant, standing next to (rather than in front of) the participant while demonstrating the movement, so the participant could observe the appropriate depth of the squat but not the pattern of lower extremity motion in the frontal plane. The participant was instructed to start with arms across the chest and weight distributed evenly on both feet. When cued to move, the participant raised the untested limb by flexing the knee while maintaining the hip in 0° of extension. The participant then performed the SLSquat and returned to the standing position with weight distributed evenly on both feet. The participant was encouraged to squat as far as comfortably possible. If the participant did not reach at least 60° of knee flexion, as judged visually by the research assistant, he or she was instructed to increase the depth of the squat.
After instruction, participants were allowed to practice the movement until they felt comfortable with the performance. Any participant who required more than 3 repetitions for practice was allowed 2 to 3 minutes to rest before video capture. Once the participant was comfortable with the movement, 1 movement was recorded. The video was collected in the standing position with both feet on the ground, through the SLSquat movement, and back to the standing position. The recording was repeated if the participant lost balance during the movement or if the research assistant determined that the squat was not sufficiently deep. Loss of balance was defined as (1) placing the untested limb on the ground before completing the movement, (2) demonstrating extraneous movement of the upper extremities, (3) trunk lean that resulted in excessive motion of the untested limb, or (4) movement of the stance limb by sliding, hopping, or twisting the stance foot. The participant then repeated the process on the opposite limb, yielding 1 recording of 1 trial for each limb for each person.
Video Selection for Reliability
Over 6 testing sessions, 140 movements (70 participants) were collected for the ongoing longitudinal study. From the 140 videos, a second research assistant (C.K.) not involved in the original video recordings or the visual assessment selected the videos to be used for reliability testing. The research assistant had minimal knowledge of the movement patterns of interest and was instructed to select videos that included variable movements. She was also instructed to exclude a video if the squat did not appear to achieve knee flexion of 60° or the participant lost balance during the testing. A total of 30 videos of 30 participants (1 limb each) were selected for reliability testing. Of the 30 participants, 18 were male and 12 were female; average age was 19.3 ± 4.5 years and body mass index was 23.8 ± 3.6. To reduce the likelihood of tester recall, the research assistant assigned a dummy code to each video and randomly ordered the videos for each testing session. Compact discs were created and distributed to each tester along with written instructions for performing the visual assessment and a data-collection sheet for each testing session.
Testers
Three testers participated in the study. The first tester (experienced; M.H.H.) was a Board-certified clinical specialist in orthopaedic physical therapy with 13 years of clinical and research experience. The second tester (experienced; G.B.S.) was a physical therapist with 24 years of clinical and research experience specific to the lower extremity. The third tester (novice; V.G.) was a postdoctoral fellow with 4 years of research experience (only 1 year specific to musculoskeletal assessment) and no clinical background. The first and second testers were involved in development and standardization of the movement assessment. The third tester was trained by the second tester. Training included review of a written manual describing the criteria for group classification, followed by observing and discussing 8 to 10 practice videos together.
Visual-Assessment Procedures
On 2 occasions, each tester viewed the selected videos and classified the movement pattern demonstrated by each participant. To reduce the likelihood of tester recall, the testing sessions were at least 1 week apart. No discussion of the testing procedures or the classification criteria occurred during the testing.
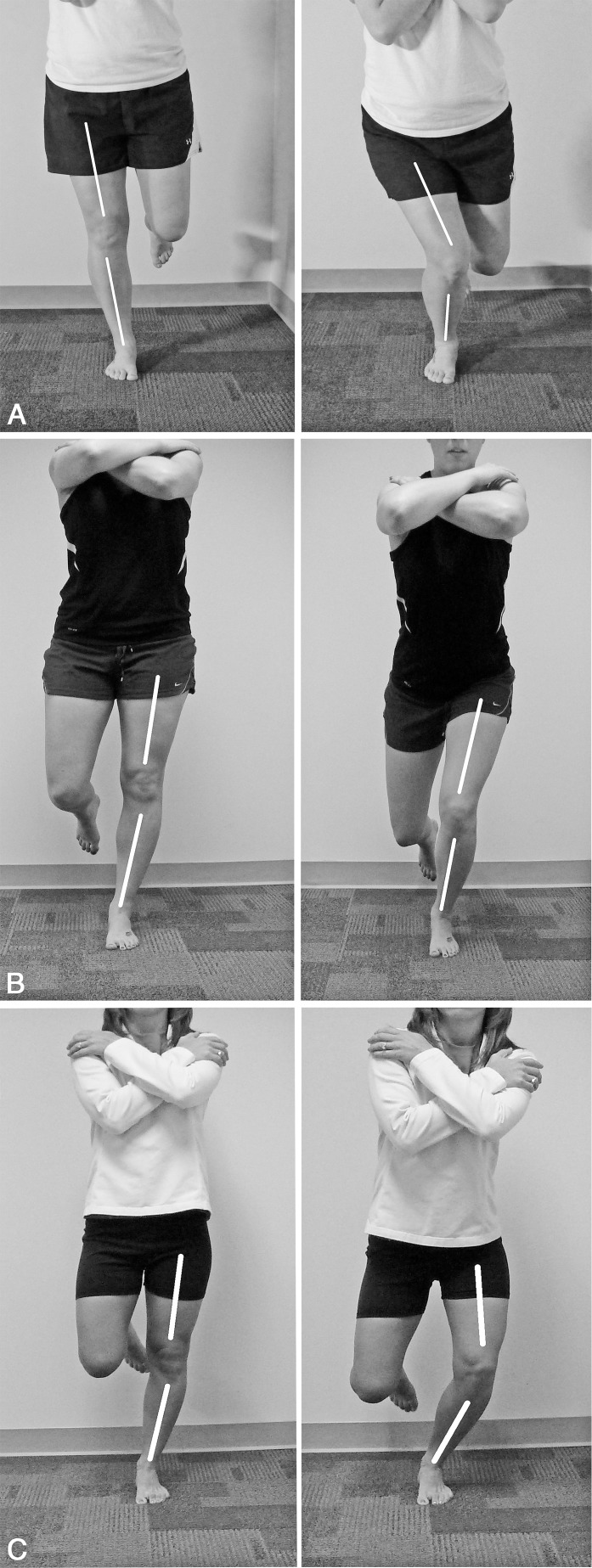
Each tester classified the movement pattern using the methods developed. For each video, she compared the FPPA in single-legged stance (start position) with the FPPA at the maximum depth of the squat movement (end position). Based on visual appraisal, the tester determined if the FPPA changed more than 10° from the start position to the end position. We used the 10° criterion because we had previously found a 10° change to be easily detectable by visual appraisal. If the angle did not change more than 10°, the movement was classified as no change. If the angle changed more than 10°, the tester also determined if the knee moved toward or away from the midline of the body. Movement toward the midline was classified as dynamic valgus, and movement away from the midline was classified as dynamic varus (Figure).
Figure.
Methods for objective measurement of the frontal-plane projection-angle (FPPA) change. We drew 2 lines to represent the FPPA: 1 bisected the thigh segment, and 1 bisected the lower leg. The angles were then measured using a protractor function in the measurement software. The FPPA change was calculated by subtracting the ending FPPA from the starting FPPA. Representative examples of the 3 lower extremity movement classifications are shown. A, Dynamic valgus: angle between the femoral bisection and lower leg bisection changed more than 10°, and the knee moved toward the midline of the body. B, No change: angle between the femoral bisection, and lower leg bisection changed less than 10° during the motion. C, Dynamic varus: angle between the femoral bisection and lower leg bisection changed more than 10°, and the knee moved away from the midline of the body.
Each tester was allowed to view each video as often as needed but was not allowed to slow down the rate of or stop the video. In addition, she was not allowed to measure the angle using imaging software or goniometric devices.
Objective Measurement Procedures
The videos were also used to obtain objective 2D measures of the FPPA change. The research assistant who selected the videos performed all measurements. Using a free and open-source media player (VLC; VideoLAN, Paris, France), we captured still frames of the video at the start and end positions. The start position was defined as the frame in which the participant had placed all body weight on the tested limb and just before the tested knee started to flex. The end position was defined as the frame in which the knee had flexed maximally and just before the tested knee started to extend.
We used SketchUp (version 7.1; Google Inc, Mountain View, CA) to measure the angles on the captured snapshots. For each start and end position, we drew 2 lines to represent the FPPA, 1 that bisected the thigh and 1 that bisected the lower leg (Figure), and measured the angle formed with the 360° protractor function. Precision was set to 0.1°. The FPPA change was determined by subtracting the starting FPPA from the ending FPPA: positive values represented movement of the knee toward the midline, and negative values represented movement of the knee away from the midline. To assess the intratester reliability of the FPPA change, 15 videos were measured a second time, 2 weeks after the first measurement session. The measurement reliability was high (intraclass correlation coefficient [2,1] = 0.98, 95% confidence interval [CI] = 0.95, 0.99), with the standard error of measurement at 1.79°. This value suggests that we can be 95% confident that the true change in FPPA angle would fall within 3.58° of the measured value.
Quantitative FPPA change based on the objective measures was categorized as follows: values less than or equal to 10° in either direction were categorized as no change, values greater than 10° in the positive direction were categorized as dynamic valgus, and values greater than 10° in the negative direction were categorized as dynamic varus. The group classification from the first session of the 2 experienced testers was used to compare the quantitative FPPA change. When the 2 testers agreed, their classification was used. In the 2 cases where they disagreed, a third expert was consulted to determine the final classification. This consensus rating is considered our best estimate of the true condition.
Statistical Analysis
Statistical analysis was completed using SAS (version 9.1 for Linux; SAS Institute Inc, Cary, NC). Descriptive statistics were calculated for demographics. Percentage of observations yielding perfect agreement (ie, percentage agreement) and weighted κ coefficients15 with 95% CIs were used to examine the intratester and intertester reliability of the visual-assessment classification and to compare the visual-assessment category with the quantitative FPPA change category based on the objective measures. We used weighted κ coefficients to represent the fraction of agreement beyond that expected by chance and to account for the magnitude of the disagreement between readings. Intratester agreement statistics compared sessions 1 and 2 for each tester. Intertester agreement statistics compared session 1 classifications across testers. A P value < .05 was considered significant.
RESULTS
Percentage agreement and tester reliability of the visual-assessment classification are provided in Table 1. Weighted κ values ranged from 0.80 to 0.90 for intratester reliability and from 0.75 to 0.90 for intertester reliability, indicating substantial to excellent reliability.16 The number of participants classified as dynamic valgus, no change, or dynamic varus for each tester's session 1 and 2 readings is shown in Table 2. The participants classified by each pair of testers are described in Table 3.
Table 1.
Intratester and Intertester Reliability for Visual Assessment of the Single-Legged Squat
| Examiners' Reliability |
Percentage Agreement (95% Confidence Interval) |
Weighted κ (95% Confidence Interval) |
| Intratester | ||
| 1 (Experienced tester) | 87 (73, 100) | 0.80 (0.61, 0.99) |
| 2 (Experienced tester) | 93 (83, 100) | 0.90 (0.77, 1.00) |
| 3 (Novice tester) | 90 (78, 100) | 0.84 (0.67, 1.00) |
| Intertester | ||
| 1 versus 2 | 93 (83, 100) | 0.90 (0.77, 1.00) |
| 1 versus 3 | 83 (68, 98) | 0.75 (0.54, 0.96) |
| 2 versus 3 | 83 (68, 98) | 0.75 (0.54, 0.96) |
Table 2.
The κ Tables for Intratester Ratingsa
| Session 1 |
Dynamic Valgus |
No Change |
Dynamic Varus |
Total |
| Tester 1 (experienced) | Session 2b | |||
| Dynamic valgus | 13 | 3 | 0 | 16 |
| No change | 1 | 10 | 0 | 11 |
| Dynamic varus | 0 | 0 | 3 | 3 |
| Total | 14 | 13 | 3 | 30 |
| Tester 2 (experienced) | Session 2 | |||
| Dynamic valgus | 15 | 1 | 0 | 16 |
| No change | 1 | 10 | 0 | 11 |
| Dynamic varus | 0 | 0 | 3 | 3 |
| Total | 16 | 11 | 3 | 30 |
| Tester 3 (novice) | Session 2 | |||
| Dynamic valgus | 18 | 3 | 0 | 21 |
| No change | 0 | 6 | 0 | 6 |
| Dynamic varus | 0 | 0 | 3 | 3 |
| Total | 18 | 9 | 3 | 30 |
Each tester viewed the videos and classified the movement pattern on 2 occasions.
Cell values are the number of participants for each pair of classifications.
Table 3.
The κ Tables for Intertester Ratingsa
| Dynamic Valgus |
No Change |
Dynamic Varus |
Total |
|
| Tester 1 (experienced) | Tester 2 (experienced)b | |||
| Dynamic valgus | 15 | 1 | 0 | 16 |
| No change | 1 | 10 | 0 | 11 |
| Dynamic varus | 0 | 0 | 3 | 3 |
| Total | 16 | 11 | 3 | 30 |
| Tester 1 (experienced) | Tester 3 (novice) | |||
| Dynamic valgus | 16 | 0 | 0 | 16 |
| No change | 5 | 6 | 0 | 11 |
| Dynamic varus | 0 | 0 | 3 | 3 |
| Total | 21 | 6 | 3 | 30 |
| Tester 2 (experienced) | Tester 3 (novice) | |||
| Dynamic valgus | 16 | 0 | 0 | 16 |
| No change | 5 | 6 | 0 | 11 |
| Dynamic varus | 0 | 0 | 3 | 3 |
| Total | 21 | 6 | 3 | 30 |
Classifications from the first session for each tester were used for intertester reliability testing.
Cell values are the number of participants for each pair of classifications.
Percentage agreement between the visual-assessment category and the quantitative FPPA change category was 90% (95% CI = 78%, 100%), with a weighted κ of 0.85 (95% CI = 0.69, 1.0; Table 4).
Table 4.
The κ Table for Comparison of Categories Based on Visual Assessment and Quantitative Frontal-Plane Projection-Angle Change
| Quantitative frontal-plane projection-angle change |
Visual Assessment (Consensus Rating) |
|||
| Dynamic Valgus |
No Change |
Dynamic Varus |
Total |
|
| Dynamic valgus | 14 | 1a | 0 | 15 |
| No change | 2b | 10 | 0 | 12 |
| Dynamic varus | 0 | 0 | 3 | 3 |
| Total | 16 | 11 | 3 | 30 |
The change value for this discrepancy is 13.4°.
The change values for these 2 discrepancies are 3.2° and 8.0°.
DISCUSSION
The goal of our study was to evaluate the reliability of experienced and novice testers in visually assessing lower extremity movement patterns during an SLSquat and to determine the construct validity of visual assessments compared with a quantitative measure of FPPA change. We hypothesized that the testers, both experienced and novice, would demonstrate good to excellent reliability using the standardized methods and that movement-pattern categories based on visual assessments would be in good to excellent agreement with categories based on the quantitative FPPA change. Both hypotheses were supported.
We have demonstrated that visual assessments can be made reliably by testers of variable experience levels when standardized methods are used. In addition, agreement between the visual assessment and the quantitative FPPA change category was substantial. The standardized criteria used during the visual assessments to determine classifications of lower extremity movement patterns require minimal training. Thus, it would be feasible to use visual assessment in the clinic to identify and treat movement-related musculoskeletal disorders and in large research studies to assess the association between lower extremity movement patterns and musculoskeletal injury.
Our study builds upon the work of previous authors17–20 who reported tester reliability of movement assessment specific to the lower extremity. Chmielewski et al18 were among the first to assess reliability in measuring the SLSquat; they reported low reliability (weighted κ = 0–0.55) among 3 experienced testers. From their experience, they hypothesized that reliability would likely improve with standardized methods that provided specific criteria to assist with decision making. We believe the standardization and inclusion of strict criteria to define each classification resulted in our high levels of agreement. The testers in our study were given standard instruction to determine FPPA (bisection of thigh and lower leg), specific timing of FPPA visualization (single-legged stance and maximum depth of squat), and quantitative value of FPPA change (10°) to make their visual assessment.
Ekegren et al21 reported substantial reliability among experienced testers assessing a different task, the drop vertical jump. They also used different criteria to classify lower extremity movement pattern. Although our measurements focused on the motion of the thigh relative to the lower leg, Ekegren et al21 used the relationship of the patella to the big toe. They classified the lower extremity movement pattern as follows: if the patella moves inward and ends up medial to the first toe, rate the individual as high risk [for ACL injury] or if the patella lands in line with the first toe, rate the individual as low risk [for ACL injury].
Similar to our study, they reported high reliability (κ coefficients = 0.75–0.85); however, we believe our methods more directly represent the relationship of the lower leg to the thigh during the SLSquat. During initial method development, we attempted to use the criteria reported by Ekegren et al.21 We found that during performance of the SLSquat, the patella would often end in line with the first toe, but the end position of the knee appeared to be in dynamic valgus. Thus, use of the patella may be appropriate for the drop vertical jump test and our methods may be more suited for visual assessment of the SLSquat.
Other authors9,11,20 have reported on the tester reliability of a score representing the combined movement pattern of the trunk, pelvis, and lower extremity. In each of these studies, explicit criteria were provided to assess the combined movement. Crossley et al20 noted substantial to excellent reliability (κ = 0.60–0.80) among experienced testers assessing an SLSquat. Padua et al9 used the LESS to assess the drop vertical jump and reported good intertester reliability (intraclass correlation coefficient [2,k] = 0.84). Although the testers observed movements of the lower extremity for the combined score, the authors did not assess their reliability in specifically judging the lower extremity movement patterns. Assessing the combined movement quality may be useful, but assessment of the lower extremity may provide more specific information for lower extremity disorders.
We demonstrated that a tester with minimal experience assessing lower extremity movement patterns can classify movements reliably if provided with training and specific criteria to determine the classifications. To our knowledge, this is the first study to report the reliability of a novice tester categorizing lower extremity movement patterns during a single-legged squat. Onate et al11 reported excellent expert-versus-novice intertester reliability using the LESS to assess a drop vertical jump, thus supporting our findings that a novice tester can reliably assess lower extremity movement patterns. Our methods may be used by coaches during preseason screening to assess movement patterns of athletes and by health care providers to identify those who may benefit from specific treatment to address impaired movement patterns. In addition, use of these methods may improve our ability to prospectively assess the relationship between movement patterns and musculoskeletal injury by increasing the number of testers available for screening studies.
The testers did not demonstrate perfect agreement in the lower extremity movement-pattern classifications. In fact, the novice tester was more likely to classify a movement pattern as dynamic valgus than the experienced testers. This observation may have important implications. If the test is used as a screening assessment to identify those athletes at risk for injury, the assessments made by the novice tester would result in a greater number of athletes identified as at risk and receiving possibly unnecessary additional training or treatment. If the risk or cost of treatment is high relative to the possible benefits, an experienced clinician may be preferred. However, the novice tester's intratester reliability was high, suggesting that novice testers may serve as the initial screeners to identify individuals to be referred to an experienced clinician for a more thorough movement-pattern assessment.
We also demonstrated that movement-pattern categories based on visual assessments are in excellent agreement with categories based on the quantitative FPPA change category. This is the first study to report on 3 movement-pattern categories. Previous authors4,19–21 have focused primarily on dynamic knee valgus as a potential risk factor for injury and labeled all other lower extremity movements as “good” or “low risk for injury.” We describe a third classification, a varus-like movement pattern that may be described as a dynamic knee varus. No studies have implicated a dynamic knee varus as a risk factor for injury, but varus alignment of the knee has been implicated in the progression of osteoarthritis.22 The association between varus alignment and osteoarthritis progression suggests that it may be important to identify dynamic knee varus as a potential risk factor that should be further explored. In addition, excluding dynamic knee varus from the “good” or “low risk for injury” categories may result in a more homogeneous group of participants who are classified as having no deviation.
Our study findings should be considered in light of several limitations. The first limitation pertains to the criteria used to determine the dynamic valgus or dynamic varus classification. We do not know if an FPPA change greater than 10° is associated directly with injury or musculoskeletal pain. Based on our clinical experience with people reporting hip or knee pain, we found that people who demonstrate dynamic valgus during an SLSquat often have increased pain with the maneuver. If the dynamic valgus is corrected, this pain is often reduced or eliminated. We therefore felt it important to standardize this test and assess its reliability and validity. As stated previously, during the development and refinement of our methods, we found that an FPPA change represented the lower extremity movement pattern we were observing clinically and that 10° was easily detected on visual assessment. Future studies with larger sample sizes, however, are needed to assess the sensitivity, specificity, and predictive values associated with our methods.
We have not validated our visual assessments using laboratory-based 3-dimensional (3-D) motion analysis, the gold standard for movement-pattern assessment. We instead compared our visual assessment with 2-D projection angles using video recordings. Projection angles, although not a direct substitute for 3-D angles,14 are correlated with 3-D angles.23 We believe our methods are a reasonable first step to validation that can be easily replicated in clinical settings that lack 3-D motion analysis. Comparison of visual assessments with 3-D motion is the focus of our next study.
We did not standardize the SLSquat for depth or speed, which is typical of clinical practice. Variations in either squat depth or speed may affect the angle changes observed and measured. The testers, however, were able to determine the classifications of the lower extremity movement patterns with substantial to excellent reliability despite this variability. This limitation is being addressed in our current study: squat depth is standardized, and the time to complete the movement is being collected as a covariate.
To assess tester reliability, we used a video recording of 1 SLSquat that could be viewed by each tester multiple times. Using a video recorder would not be feasible in clinical practice, but clinicians can use our methods for visual assessment to observe movements performed by their patients. A person's performance of the SLSquat may vary across testing sessions, resulting in different movement patterns being assessed during the two sessions, thus limiting our ability to accurately assess tester reliability. We therefore used 1 video recording so the participant's performance would remain stable across testing sessions.
We did not assess test-retest reliability by observing participants on multiple occasions. Test-retest reliability would be important, particularly if lower extremity movement assessment were to be implemented as an outcome measure for treatment. Stensrud et al19 reported fair to moderate test-retest reliability when 1 tester assessed SLSquat; however, the criteria to classify the movement pattern were not as specific as those outlined in the current study. We believe use of our standardized methods will improve upon the test-retest results previously reported. Future work will include movement testing performed by the participants on multiple occasions.
CONCLUSIONS
With training and use of standardized techniques, both experienced and novice testers can reliably classify lower extremity movement patterns based on visual assessment. Although experienced testers demonstrate higher intertester reliability, reliability between the novice and experienced testers was substantial, indicating novice testers may be used for initial screening programs. Additionally, movement-pattern-category–based visual assessments were in excellent agreement with objective methods to measure FPPA change. Visual assessment may be used in the clinic to categorize movement patterns that may be associated with musculoskeletal disorders and in large epidemiologic studies to assess the association between lower extremity movement patterns and musculoskeletal injury. Future research is needed to determine if an association exists between the identified movement patterns and musculoskeletal disorders.
ACKNOWLEDGMENTS
We recognize Shirley Sahrmann, Nancy Bloom, and Suzy Cornbleet for their assistance in concept and method development; faculty, staff, and students of the Program in Physical Therapy and Department of Orthopedic Surgery at Washington University School of Medicine for their assistance in data collection; and Rick Larsen and the Athletic Training staff at Washington University in St Louis for their assistance in participant recruitment.
FINANCIAL DISCLOSURES
This work was supported by the following grants: Dr Harris-Hayes and Ms Steger-May were supported by Grant K12HD055931 from the National Institute of Child Health and Human Development and National Institute of Neurological Disorders and Stroke and Grant 1 UL1 RR 024992-01 from the National Center for Research Resources, components of the National Institutes of Health and NIH Roadmap for Medical Research. Additional support for Dr Harris-Hayes was provided by the Program in Physical Therapy at Washington University School of Medicine. Drs Graci and Salsich were supported by Grants R15HD059080 and R15HD059080-01A1S1 from the National Institute of Child Health and Human Development. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official view of the National Center for Medical Rehabilitation Research or National Institutes of Health.
REFERENCES
- 1.Hewett TE, Myer GD, Ford KR, et al. Biomechanical measures of neuromuscular control and valgus loading of the knee predict anterior cruciate ligament injury risk in female athletes: a prospective study. Am J Sports Med. 2005;33(4):492–501. doi: 10.1177/0363546504269591. [DOI] [PubMed] [Google Scholar]
- 2.Willson JD, Binder-Macleod S, Davis IS. Lower extremity jumping mechanics of female athletes with and without patellofemoral pain before and after exertion. Am J Sports Med. 2008;36(8):1587–1596. doi: 10.1177/0363546508315592. [DOI] [PubMed] [Google Scholar]
- 3.Powers CM. The influence of altered lower-extremity kinematics on patellofemoral joint dysfunction: a theoretical perspective. J Orthop Sports Phys Ther. 2003;33(11):639–646. doi: 10.2519/jospt.2003.33.11.639. [DOI] [PubMed] [Google Scholar]
- 4.Levinger P, Gilleard W, Coleman C. Femoral medial deviation angle during a one-leg squat test in individuals with patellofemoral pain syndrome. Phys Ther Sport. 2007;8(4):163–168. [Google Scholar]
- 5.Austin AB, Souza RB, Meyer JL, Powers CM. Identification of abnormal hip motion associated with acetabular labral pathology. J Orthop Sports Phys Ther. 2008;38(9):558–565. doi: 10.2519/jospt.2008.2790. [DOI] [PubMed] [Google Scholar]
- 6.Hewett TE, Lindenfeld TN, Riccobene JV, Noyes FR. The effect of neuromuscular training on the incidence of knee injury in female athletes: a prospective study. Am J Sports Med. 1999;27(6):699–706. doi: 10.1177/03635465990270060301. [DOI] [PubMed] [Google Scholar]
- 7.Harris-Hayes M, Sahrmann SA, Norton BJ, Salsich GB. Diagnosis and management of a patient with knee pain using the movement system impairment classification system. J Orthop Sports Phys Ther. 2008;38(4):203–213. doi: 10.2519/jospt.2008.2584. [DOI] [PubMed] [Google Scholar]
- 8.Sahrmann SA. Diagnosis and Treatment of Movement Impairment Syndromes. St Louis, MO: Mosby, Inc; 2002. [Google Scholar]
- 9.Padua DA, Boling MC, Distefano LJ, Onate JA, Buetler AI, Marshall SW. Reliability of the landing error scoring system-real time, a clinical assessment tool of jump-landing biomechanics. J Sport Rehabil. 2011;20(2):145–156. doi: 10.1123/jsr.20.2.145. [DOI] [PubMed] [Google Scholar]
- 10.Padua DA, Marshall SW, Boling MC, Thigpen CA, Garrett WE, Jr, Beutler AI. The Landing Error Scoring System (LESS) is a valid and reliable clinical assessment tool of jump-landing biomechanics. Am J Sports Med. 2009;37(10):1996–2002. doi: 10.1177/0363546509343200. [DOI] [PubMed] [Google Scholar]
- 11.Onate J, Cortes N, Welch C, Van Lunen BL. Expert versus novice interrater reliability and criterion validity of the landing error scoring system. J Sport Rehabil. 2010;19(1):41–56. doi: 10.1123/jsr.19.1.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Willson JD, Ireland ML, Davis I. Core strength and lower extremity alignment during single leg squats. Med Sci Sports Exerc. 2006;38(5):945–952. doi: 10.1249/01.mss.0000218140.05074.fa. [DOI] [PubMed] [Google Scholar]
- 13.Willson JD, Davis IS. Utility of the frontal plane projection angle in females with patellofemoral pain. J Orthop Sports Phys Ther. 2008;38(10):606–615. doi: 10.2519/jospt.2008.2706. [DOI] [PubMed] [Google Scholar]
- 14.Olson TJ, Chebny C, Willson JD, Kernozek TW, Straker JS. Comparison of 2d and 3d kinematic changes during a single leg step down following neuromuscular training. Phys Ther Sport. 2011;12(2):93–99. doi: 10.1016/j.ptsp.2010.10.002. [DOI] [PubMed] [Google Scholar]
- 15.Sim J, Wright CC. The kappa statistic in reliability studies: use, interpretation, and sample size requirements. Phys Ther. 2005;85(3):257–268. [PubMed] [Google Scholar]
- 16.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 17.Eastlack ME, Arvidson J, Snyder-Mackler L, Danoff JV, McGarvey CL. Interrater reliability of videotaped observational gait-analysis assessments. Phys Ther. 1991;71(6):465–472. doi: 10.1093/ptj/71.6.465. [DOI] [PubMed] [Google Scholar]
- 18.Chmielewski TL, Hodges MJ, Horodyski M, Bishop MD, Conrad BP, Tillman SM. Investigation of clinician agreement in evaluating movement quality during unilateral lower extremity functional tasks: a comparison of 2 rating methods. J Orthop Sports Phys Ther. 2007;37(3):122–129. doi: 10.2519/jospt.2007.2457. [DOI] [PubMed] [Google Scholar]
- 19.Stensrud S, Myklebust G, Kristianslund E, Bahr R, Krosshaug T. Correlation between two-dimensional video analysis and subjective assessment in evaluating knee control among elite female team handball players. Br J Sports Med. 2011;45(7):589–595. doi: 10.1136/bjsm.2010.078287. [DOI] [PubMed] [Google Scholar]
- 20.Crossley KM, Zhang WJ, Schache AG, Bryant A, Cowan SM. Performance on the single-leg squat task indicates hip abductor muscle function. Am J Sports Med. 2011;39(4):866–873. doi: 10.1177/0363546510395456. [DOI] [PubMed] [Google Scholar]
- 21.Ekegren CL, Miller WC, Celebrini RG, Eng JJ, MacIntyre DL. Reliability and validity of observational risk screening in evaluating dynamic knee valgus. J Orthop Sports Phys Ther. 2009;39(9):665–674. doi: 10.2519/jospt.2009.3004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286(2):188–195. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- 23.McLean SG, Walker K, Ford KR, Myer GD, Hewett TE, van den Bogert AJ. Evaluation of a two dimensional analysis method as a screening and evaluation tool for anterior cruciate ligament injury. Br J Sports Med. 2005;39(6):355–362. doi: 10.1136/bjsm.2005.018598. [DOI] [PMC free article] [PubMed] [Google Scholar]