Abstract
Context:
Some athletes ingest pickle juice (PJ) or mustard to treat exercise-associated muscle cramps (EAMCs). Clinicians warn against this because they are concerned it will exacerbate exercise-induced hypertonicity or cause hyperkalemia. Few researchers have examined plasma responses after PJ or mustard ingestion in dehydrated, exercised individuals.
Objective:
To determine if ingesting PJ, mustard, or deionized water (DIW) while hypohydrated affects plasma sodium (Na+) concentration ([Na+]p), plasma potassium (K+) concentration ([K+]p), plasma osmolality (OSMp), or percentage changes in plasma volume or Na+ content.
Design:
Crossover study.
Setting:
Laboratory.
Patients or Other Participants:
A total of 9 physically active, nonacclimated individuals (age = 25 ± 2 years, height = 175.5 ± 9.0 cm, mass = 78.6 ± 13.8 kg).
Intervention(s):
Participants exercised vigorously for 2 hours (temperature = 37°C ± 1°C, relative humidity = 24% ± 4%). After a 30-minute rest, a baseline blood sample was collected, and they ingested 1 mL/kg body mass of PJ or DIW. For the mustard trial, participants ingested a mass of mustard containing a similar amount of Na+ as for the PJ trial. Postingestion blood samples were collected at 5, 15, 30, and 60 minutes.
Main Outcome Measure(s):
The dependent variables were [Na+]p, [K+]p, OSMp, and percentage change in plasma Na+ content and plasma volume.
Results:
Participants became 2.9% ± 0.6% hypohydrated and lost 96.8 ± 27.1 mmol (conventional unit = 96.8 ± 27.1 mEq) of Na+, 8.4 ± 2 mmol (conventional unit = 8.4 ± 2 mEq) of K+, and 2.03 ± 0.44 L of fluid due to exercise-induced sweating. They ingested approximately 79 mL of PJ or DIW or 135.24 ± 22.8 g of mustard. Despite ingesting approximately 1.5 g of Na+ in the PJ and mustard trials, no changes occurred within 60 minutes postingestion for [Na+]p, [K+]p, OSMp, or percentage changes in plasma volume or Na+ content (P > .05).
Conclusions:
Ingesting a small bolus of PJ or large mass of mustard after dehydration did not exacerbate exercise-induced hypertonicity or cause hyperkalemia. Consuming small volumes of PJ or mustard did not fully replenish electrolytes and fluid losses. Additional research on plasma responses pre-ingestion and postingestion to these treatments in individuals experiencing acute EAMCs is needed.
Key Words: acetic acid, dehydration, potassium, sodium, vinegar
Key Points
Drinking 1 mL/kg body mass of pickle juice (PJ) while hypohydrated did not exacerbate exercise-induced hypertonicity or cause hyperkalemia.
Ingesting a mass of mustard with a sodium (Na+) content similar to that ingested in small volumes of PJ did not alter plasma Na+ concentration, plasma potassium (K+) concentration, plasma osmolality, or percentage changes in plasma volume or plasma Na+ content.
Consuming 1 mL/kg body mass of PJ or a mass of mustard with a similar Na+ content could not fully replace the Na+, K+, or fluid lost due to exercise-induced sweating.
Ingesting small volumes of PJ or mustard may be ineffective in alleviating exercise-associated muscle cramps by replenishing electrolytes if the cramps are due to Na+, K+, or fluid imbalances.
Some scientists1 have reported that 95% of active individuals have experienced exercise-associated muscle cramps (EAMCs) during or after exercise. Although EAMCs are prevalent, their cause remains unknown. Because EAMCs tend to occur more frequently when individuals exercise in hot, humid conditions2 and people with cramps tend to have higher sweat sodium (Na+) concentrations ([Na+]) than people without cramps (approximately 55 mmol/L [conventional unit = 55 mEq/L] versus approximately 25 mmol/L [conventional unit = 25 mEq/L], respectively),3 many athletic trainers (ATs) believe EAMCs are due to dehydration and electrolyte losses.4 The dehydration and electrolyte theory speculates EAMCs result from increased pressure on select nerve terminals due to fluid shifting out of the interstitium.5 Whereas this theory has been challenged in cohort6–8 and experimental studies,9,10 most ATs focus on fluid and electrolyte replacement when treating EAMCs.4
Some ATs have experimented with anecdotal remedies, such as ingestion of pickle juice (PJ; a salty, acidic brine used in pickling cucumbers) or mustard, for EAMCs.4,11,12 Approximately 25% (92/370) of ATs polled have used PJ to treat EAMCs, with most providing small volumes (ie, <200 mL).11 Some ATs have reported success alleviating EAMCs by instructing athletes to drink 2 ounces (60 mL) of pickle juice.13 This volume is well tolerated and does not cause gastrointestinal distress.14,15 Most11 credit the electrolytes in PJ for alleviation of EAMCs. In contrast, minimal data exist on how much mustard is given for EAMCs or what the effects of mustard ingestion are on plasma variables in exercised individuals.
Other ATs discourage drinking PJ because they believe it will exacerbate exercise-induced hypertonicity and prolong rehydration.16 Some ATs advise caution when ingesting PJ because they are concerned it will cause hyperkalemia.17 However, in recent research on euhydrated men, Miller et al14 indicated that no changes in plasma osmolality (OSMp), plasma sodium concentration ([Na+]p), plasma potassium (K+) concentration ([K+]p), or percentage changes in plasma volume occurred within 60 minutes postingestion of 1 mL/kg body mass of PJ. One limitation of this investigation14 was that blood characteristics were not measured in dehydrated individuals. Given that many athletes develop EAMCs while hypohydrated,8,18,19 determining the effects of PJ ingestion in dehydrated participants is necessary. Moreover, ingesting PJ or mustard postexercise may cause a greater change in plasma electrolytes and OSMp because plasma aldosterone levels can be elevated up to 1 hour postexercise.20
Therefore, the purpose of my study was to determine if ingesting PJ, mustard, or deionized water (DIW) while hypohydrated affects [Na+]p, [K+]p, OSMp, or percentage changes in plasma volume or Na+ content. I hypothesized that no changes in these variables would occur within 60 minutes postingestion of PJ or mustard.
METHODS
Participants
A convenience sample of 13 (7 men, 6 women) physically active,21 non–heat-acclimated individuals volunteered. Four women could not complete the study because they were nauseated postexercise. Seven men and 2 women completed testing (Table 1).
Table 1.
Demographic Characteristics and Sweat Composition (Mean ± SD)a
| Characteristic |
Total |
| Age, y | 25 ± 2 |
| Height, cm | 175.5 ± 9.0 |
| Pre-exercise body mass, kg | 78.6 ± 13.8 |
| Postexercise body mass, kg | 76.4 ± 13.7 |
| Hypohydration, % | 2.85 ± 0.62 |
| Sweat volume, L | 2.03 ± 0.44 |
| Sweat [Na+], mmol/L (mEq/L) | 48 ± 12 (48 ± 12) |
| Sweat [K+], mmol/L (mEq/L) | 4.1 ± 0.3 (4.1 ± 0.3) |
Indicates no differences existed between treatments for levels of hypohydration or sweat characteristics. Thus, the data were combined and reported descriptively.
Volunteers were excluded from participating if they self-reported neurologic, cardiovascular, or blood-borne diseases; pregnancy; a history of heat-related illness (eg, heat stroke); or food allergy to mustard or pickles. Women were tested within the follicular phase of menses to minimize the effects of hormones on electrolyte balance. Participants provided written informed consent, and the study was approved by the Institutional Review Board of North Dakota State University.
Testing Procedures
Participants reported for testing on 3 separate days. Twenty-four hours before each testing session, I gave them pretest instructions (ie, drink water consistently; avoid exercise, caffeine, and alcohol; and fast for 12 hours). They were encouraged to drink water during their fasts. The participants did not keep diet logs but were instructed to maintain a consistent dietary regimen until completion of the study. Compliance with these instructions was assessed at pretest.
They reported to a laboratory typically in the morning and voided their bladders completely. Urine specific gravity was assessed with a refractometer (model SUR-Ne; Atago USA Inc, Bellevue, WA). If hypohydrated (specific gravity > 1.020),22 participants ingested approximately 500 mL of tap water, and specific gravity was reassessed 30 minutes later. When euhydrated, they inserted a rectal thermistor (YSI 4600 Precision Thermometer with model 401 probe; Advanced Industrial Systems Inc, Prospect, KY) at least 10 cm past the anal sphincter. Rectal temperature was monitored during exercise to ensure it did not exceed 39°C; no participant exceeded this temperature during exercise. They donned heart-rate monitors (Polar Electro, Inc, Lake Success, NY) and were weighed in shorts and socks (women also wore sports bras) to the nearest hundredth of a kilogram (model DA150; Denver Instruments, Bohemia, NY).
I shaved the participants' posterior midforearms and cleaned them with deionized water (DIW). After drying the forearms, I placed sterile sweat patches (occlusive dressing and sterile gauze) over the midforearms. They entered an environmental chamber (temperature = 37°C ± 1°C, relative humidity = 24% ± 4%) and began exercising. They alternated between running and biking every 15 minutes for 60 minutes. They ran on a treadmill (model TMX425C; TrackMaster, Newton, KS) at a speed that kept their heart rates between 160 and 170 beats per minute and rode a bicycle (model 818E; Monark, Stockholm, Sweden) at an intensity that kept their heart rates between 150 and 160 beats per minute. Based on age-predicted maximums, the exercise intensity for biking and running was vigorous (77%–87% of maximal heart rate).21 Sweat patches were removed after 20 minutes. After 60 minutes of exercise, participants biked for 5 minutes at a self-selected lower intensity to cool down. They exited the environmental chamber, towel dried, voided their bladders completely, and were weighed. They reentered the environmental chamber and began the second hour of exercise using the same exercise protocol.
After completing the 2 hours of exercise, participants towel dried, voided their bladders completely, and were weighed. They removed the rectal thermistor and heart-rate monitor and sat in a climate-controlled room (temperature = 25°C, relative humidity = 16%) for 30 minutes to allow their body compartments to equilibrate.23 They remained in this position for the remainder of testing and were instructed to minimize movement. During this equilibration period, I cleaned the antecubital fossa with isopropyl alcohol and inserted a venous catheter into a superficial forearm vein. After the 30-minute equilibration period, a 5-mL blood sample was collected (−2.5-minute sample).
Participants were given 2.5 minutes to ingest 1 mL/kg body mass of chilled (6°C) PJ strained from sliced dill pickles (Pinnacle Foods Group LLC, Cherry Hill, NJ) or DIW. For the mustard trial, participants ingested a chilled mass of mustard (Classic Yellow; Reckitt Benckiser, Parsippany, NJ) containing a similar amount of Na+ as was ingested or would be ingested on each participant's PJ day. The mustard container was weighed pre-ingestion and postingestion to determine the exact amount of mustard, and hence Na+, K+, and fluid, ingested. The DIW was given as a control solution. No additional fluids were provided to the participants at any time during the experiment.
I collected 5-mL blood samples at 5, 15, 30, and 60 minutes postingestion. After collecting the last blood sample, I removed the catheter assembly and excused the participants. I instructed them to report at least 48 hours later at the same time of day for the next testing session. Testing sessions differed only in the treatment ingested. The order of treatment ingestion was counterbalanced using half of the available treatment ingestion orders so the same number of participants experienced each treatment the same number of times per testing day. Participants randomly chose a treatment ingestion order a priori.
Blood Analysis Procedures
Hematocrit and hemoglobin concentration ([Hb]) were determined immediately postcollection using whole blood. Blood for hematocrit analysis was drawn into heparinized microcapillary tubes and centrifuged at 3000 revolutions per minute (model IEC Micro-MB; International Equipment Co, Needham Heights, MA) for 5 minutes and read using a microcapillary reader (model IEC 2201; Damon/IEC, Needham Heights, MA). I determined [Hb] using the cyanomethemoglobin technique.14 Hematocrit and [Hb] were measured in triplicate and averaged to calculate percentage changes in plasma volume per Dill and Costill.24 Hematocrit, [Hb], and [Na+]p were used to estimate the percentage change in plasma Na+ content per Greenleaf et al.25 Any remaining blood not used for hematocrit and [Hb] was stored on ice until centrifugation.
After collecting the last blood sample, I centrifuged the remaining blood at 3000 revolutions per minute for 15 minutes at 3°C. Plasma was removed, analyzed for OSMp using freezing-point depression osmometry (model 3D3; Advanced Instruments Inc, Norwood, MA), and then frozen (−80°C). Samples later were thawed and analyzed in duplicate for [Na+]p and [K+]p with an ion-selective electrode analyzer (NOVA 16; Nova Biomedical, Waltham, MA).
Sweat Analysis Procedures
Sweat patches were placed in a clean test tube, immediately centrifuged at 3°C for 10 minutes at 5000 revolutions per minute, and analyzed for sweat [Na+] and sweat K+ concentration ([K+]). Sweat volume was estimated from body mass measures and corrected for urine volume produced. Given that sweat [Na+] and [K+] can be overestimated when using occlusive dressings,26,27 the sweat [Na+] and [K+] data were corrected using the equations of Baker et al26 that have high reliability (r = 0.96 for Na+ and r = 0.9 for K+) with the criterion standard of whole-body wash-down.
Treatment Solution Analysis
I analyzed PJ and DIW for [Na+], [K+], osmolality, pH (model AB15 Basic; Fisher Scientific, Pittsburgh, PA), and specific gravity. All analyses were conducted in duplicate and averaged. I used the nutrition label and a food composition table28 to determine the [Na+], [K+], and fluid content of mustard.
Statistical Analysis
Differences in blood variables between treatments over time were analyzed with separate repeated-measures analyses of variance. Geisser–Greenhouse adjustments to P values were made when sphericity was violated. When I found interactions or main level effects, I used Tukey–Kramer multiple comparison tests to identify differences between treatment conditions at each time point. The α level was set at .05. I used NCSS (version 2007; NCSS, Kaysville, UT) to analyze the data.
RESULTS
Data are reported as means ± SDs. Participants self-reported compliance with all pretesting instructions and were similarly euhydrated before testing (urine specific gravities: PJ = 1.009 ± 0.005, mustard = 1.006 ± 0.003, DIW = 1.007 ± 0.005; F2,16 = 2.5, P = .11).
Participants were similarly hypohydrated (F2,16 = 0.7, P = .52), had similar sweat [Na+] (F2,16 = 0.6, P = .55) and sweat [K+] (F2,16 = 0.5, P = .61), and lost similar volumes of sweat (F2,16 = 0.3, P = .76) during exercise on each testing day. The sweat data were combined and are reported descriptively (Table 1). They lost 97 mmol (2.2 g) of Na+ and 8.4 mmol (0.33 g) of K+ via exercise-induced sweating.
The composition of each treatment solution is provided in Table 2. Participants ingested 78.9 ± 14.2 mL of PJ, 79.1 ± 14.6 mL of DIW, and 135.24 ± 22.8 g of mustard. Thus, they ingested 1.51 ± 0.27 g, 1.49 ± 0.25 g, and 0 g of Na+ with PJ, mustard, and DIW, respectively. Participants ingested 0.06 ± 0.01 g, 0.19 ± 0.03 g, and 0 g of K+ with PJ, mustard, and DIW, respectively.
Table 2.
Treatment Solution Composition (Mean ± SD)
| Measurement |
Treatment Solution |
||
| Pickle Juiceb |
Mustard |
Deionized Waterb |
|
| Osmolality, mOsm/kg H2O | 845 ± 2 | Not measured | 0 ± 0 |
| Specific gravity | 1.018 ± 0 | Not measured | 1.0 ± 0 |
| pH | 3.68 ± 0.02 | Not measured | 5.43 ± 0.04 |
| Sodium concentration, mmol/L (mEq/L)a | 832.5 ± 10.6 (832.5 ± 10.6) | 597.8 (597.8) | Nondetectable |
| Potassium concentration, mmol/L (mEq/L)a | 18.8 ± 0.4 (18.8 ± 0.4) | 39.2 (39.2) | Nondetectable |
Indicates mustard's nutrition label was used to calculate sodium (Na+) concentration and indicated 0.011 g of Na+ in 1 g of mustard. A food composition table was used to calculate potassium (K+) concentration and indicated 0.0014 g K+ in 1 g of mustard. The Na+ and K+ concentrations for mustard in the table were calculated using these values and the information that 80% of mustard's mass is water (from food composition table).
Pickle juice and deionized water characteristics were measured in duplicate.
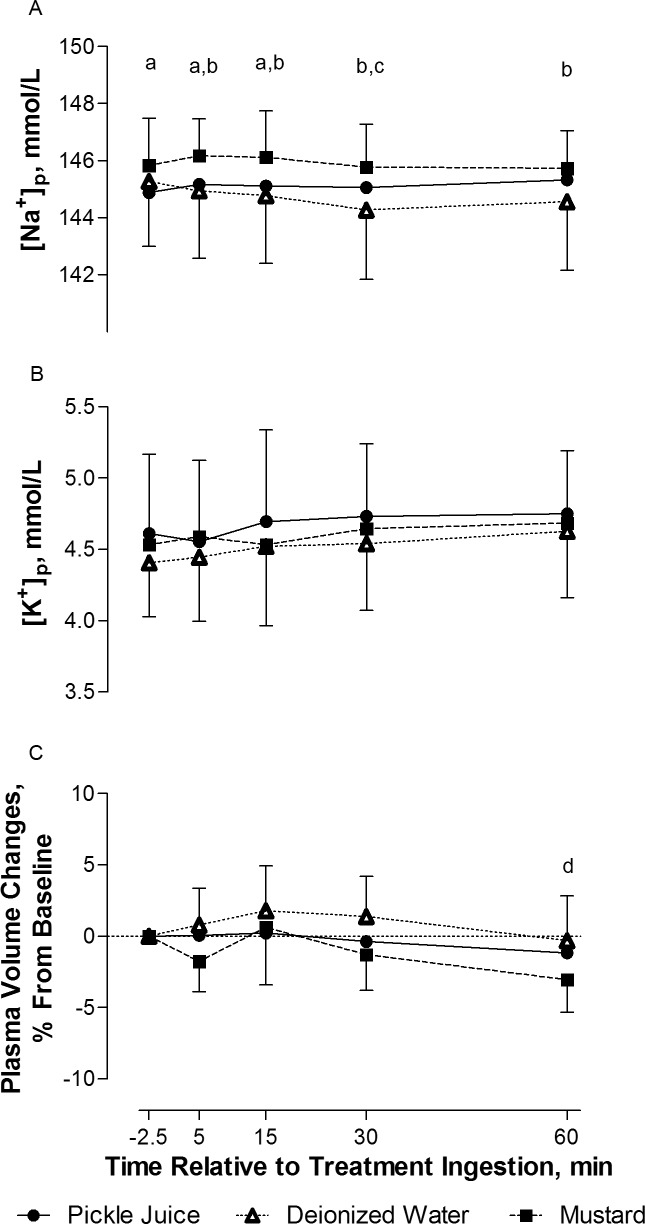
An interaction between treatment ingested and time occurred for [Na+]p (F8,64 = 2.6, P = .02; Figure 1). I did not observe differences in [Na+]p over time within the PJ or mustard trials (P > .05). After DIW ingestion, [Na+]p was lower at 30 minutes than at baseline (P < .05). The [Na+]p was lower during the PJ trial than the mustard trial at −0.5, 5, and 15 minutes postingestion (P < .05). The [Na+]p was lower in the DIW trial than in the mustard trial at 5, 15, 30, and 60 minutes postingestion (P < .05).
Figure 1.
A, Plasma sodium concentration ([Na+]p), B, plasma potassium concentration ([K+]p), and C, percentage changes in plasma volume over 60 minutes postingestion of pickle juice, deionized water, and mustard (means ± SD). a Indicates pickle juice < mustard. b Indicates deionized water < mustard. c Indicates deionized water 30 minutes < deionized water −0.5 minutes. d Indicates 60 minutes < 15 minutes (time effect). The α level was set at .05 (N = 9).
For [K+]p, no interaction effect (F8,64 = 0.7, P = .53) or main effects for treatment solution ingested (F2,16 = 1.4, P = .28) or time (F4,32 = 2.9, P = .11) were observed (Figure 1).
I did not find an interaction (F8,64 = 0.7, P = .57) or main effect for treatment ingested (F2,16 = 1.6, P = .24) for percentage changes in plasma volume (Figure 1). However, a time effect was observed (F4,32 = 4.0, P = .03): percentage changes in plasma volume were lower at 60 minutes than at 15 minutes (P < .05).
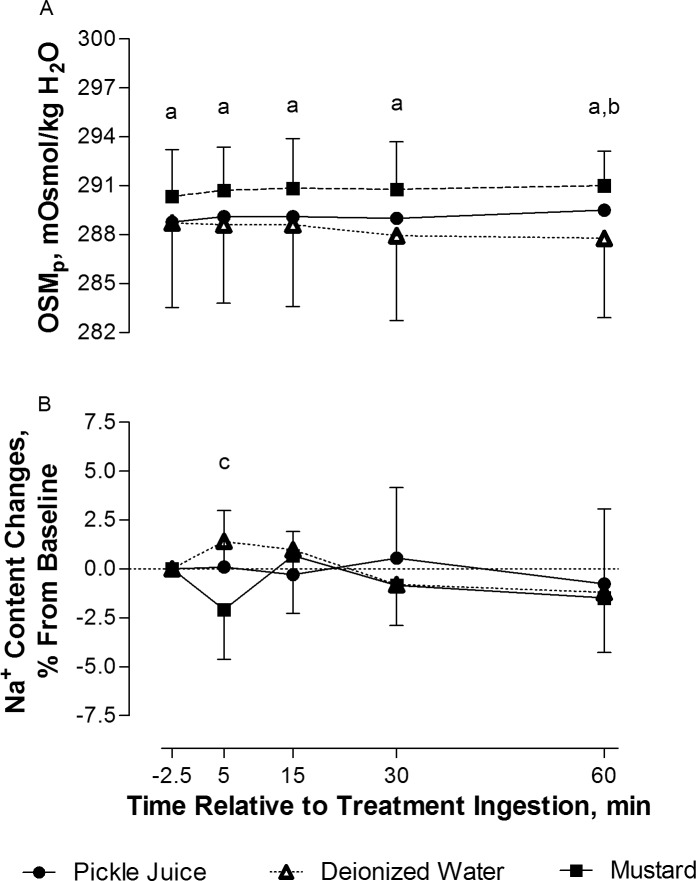
For OSMp, I observed an interaction between treatment ingested and time (F8,64 = 2.6, P = .02; Figure 2). No changes in OSMp occurred within each treatment over time (P > .05). However, OSMp was lower after PJ and DIW ingestion than after mustard ingestion at all time points (P < .05). In addition, OSMp of DIW was lower than PJ at 60 minutes (P < .05).
Figure 2.
A, Plasma osmolality ([OSMp]) and percentage changes in sodium (Na+) content compared with, B, baseline over 60 minutes postingestion of pickle juice, deionized water, and mustard (means ± SD). a Indicates pickle juice and deionized water < mustard. b Indicates deionized water < pickle juice. c Indicates deionized water > mustard. The α level was set at .05 (N = 9).
An interaction was observed for percentage changes in plasma Na+ content (F8,64 = 2.3, P = .03; Figure 2). No changes occurred within each treatment over time (P > .05). However, the percentage change in Na+ content was higher for DIW than mustard at 5 minutes postingestion (P < .05).
DISCUSSION
The 4 main points of this investigation are (1) drinking 1 mL/kg body mass of PJ did not exacerbate exercise-induced hypertonicity; (2) drinking 1 mL/kg body mass of PJ did not cause hyperkalemia; (3) ingesting a mass of mustard with a Na+ content similar to that ingested in small volumes of PJ did not alter [Na+]p, [K+]p, OSMp, or percentage changes in plasma volume or plasma Na+ content; and (4) consuming 1 mL/kg body mass of PJ or a mass of mustard with a similar Na+ content could not fully replace the Na+, K+, or fluid lost due to exercise-induced sweating. The clinical implications of these points are that ingesting small volumes of PJ or mustard may be ineffective in alleviating EAMCs by replenishing electrolytes if EAMCs are due to Na+, K+, or fluid imbalances.
Some scientists have cautioned against PJ ingestion because they believe it will increase [Na+]p and OSMp and cause a rapid plasma-volume restoration, thereby decreasing thirst and delaying rehydration.16 Despite ingesting 1.5 g of Na+ while hypohydrated, participants did not have a change in [Na+]p or OSMp at any point over the 60-minute postingestion period. Given that they ingested the treatments shortly postexercise in the heat, one can assume plasma aldosterone levels were elevated.20,29 Yet, throughout the 60-minute postingestion period, the highest OSMp and [Na+]p observed were only 0.7 mOsm/kg H2O (conventional unit = 0.7 mEq/L) and 0.4 mmol/L (conventional unit = 0.4 mEq/L), respectively, different from baseline. These data confirmed earlier observations in which [Na+]p and OSMp did not change after PJ ingestion in rested, euhydrated men.14 Furthermore, estimates of intravascular Na+ content confirmed these findings: no increases in Na+ content occurred postingestion of PJ despite participants having a 2-g deficit in Na+ at PJ ingestion. Therefore, drinking small volumes of PJ will not exacerbate exercise-induced hypertonicity up to 60 minutes postingestion.
The concern that rehydration would be impaired16 is also unnecessary for 2 reasons. First, estimates of the volume of DIW that needed to be consumed to return [Na+]p to a normal level (eg, 140 mmol/L [conventional unit = 140 mEq/L]) based on the [Na+]p data in this study indicate only an additional 62 mL of DIW would need to be consumed if PJ was ingested. Participants ingested 1 mL/kg body mass of PJ or DIW and were allowed to drink DIW ad libitum for 60 minutes.30 They consumed 167 mL more DIW ad libitum when PJ was ingested (700 ± 366 mL) than when DIW was the treatment (533 ± 337 mL). Second, percentage changes in plasma volume were minor after PJ ingestion. Whereas percentage changes in plasma volume can decrease 3% to 5% after PJ ingestion,15,31 plasma volume changes were less than 1% over 60 minutes postingestion in my study. The discrepancy likely reflects the fact that earlier investigators provided larger volumes of PJ31 to euhydrated15 rather than hypohydrated individuals. Given that minor percentage changes in plasma volume occurred, one may assume thirst would be unaffected. In fact, Hoffmann et al32 observed that the Na+ content of ingested fluid was less important than the volume of fluid ingested for inhibiting thirst in rats that were fluid deprived. Therefore, even after humans undergo intense exercise, drinking a small bolus of PJ is unlikely to delay rehydration because thirst would be unaffected.
Others17 have advised caution when ingesting PJ because they are concerned it will induce hyperkalemia. This is a concern because hyperkalemia is associated with cardiac arrhythmias33 and fatigue.34 Fowkes-Godek et al17 observed mild hyperkalemia (5.2 ± 0.2 mmol/L [conventional unit = 5.2 ± 0.2 mEq/L]) after 5 days of PJ supplementation in professional US football players compared with baseline (4.7 ± 0.5 mmol/L [conventional unit = 4.7 ± 0.5 mEq/L]). I observed no changes in [K+]p up to 60 minutes postingestion of PJ. The highest [K+]p observed was 4.75 mmol/L (conventional unit = 4.75 mEq/L), which was substantially lower than the threshold for hyperkalemia (>5 mmol/L [conventional unit >5 mEq/L]). Discrepancies are likely because of the volume and frequency of PJ ingested. Fowkes-Godek et al17 provided multiple boluses of unknown volumes of PJ over several days, whereas my participants ingested a single, small bolus postexercise. The observation of hyperkalemia after multiple boluses of PJ ingestion requires further study in which the diet, volume of PJ ingested, and exercise duration of the participants are known and controlled.
Some clinicians provide mustard for EAMCs.12 No researcher, to my knowledge, has examined the effect of ingesting mustard on [Na+]p or [K+]p. Despite the participants' ingesting 1.49 g of Na+ and 0.19 g of K+, mustard had a negligible effect on [Na+]p, [K+]p, OSMp, and percentage changes in plasma volume or Na+ content. The greatest change (0.3 mmol/L [conventional unit = 0.3 mEq/L] increase) in [Na+]p occurred at 5 minutes postingestion of mustard. This change was due to the sudden decrease in plasma volume rather than an increase in Na+ content and is likely an oropharyngeal reflex initiated by swallowing, as orophyrangeal stimulation is known to stimulate simple and complex reflexes.35 Therefore, similar arguments can be made against ingesting mustard for replenishing plasma electrolytes postexercise or using mustard as a treatment for EAMCs if EAMCs are due to electrolyte or fluid losses.
Of the ATs polled who used PJ to treat EAMCs, 64% (226/353) believed its method of action is restoration of [Na+]p or other electrolytes.11 However, ingesting these volumes of PJ cannot fully replace the Na+ or K+ lost due to exercise-induced sweating. By drinking PJ, participants replaced 4% (0.079 L/2 L) of fluid lost, 68% (1.5 g/2.2 g) of Na+ lost, and 18% (0.06 g/0.33 g) of K+ lost. Similarly, when mustard was ingested, participants replaced 6% (0.11 L/2.0 L) of fluid lost, 68% (1.5 g/2.2 g) of Na+ lost, and 58% (0.19 g/0.33 g) of K+ lost. Some athletes who develop EAMCs have higher fluid and Na+ losses than the participants in my study. Sweat rates ranging from 1.7 to 2.5 L/h and sweat [Na+] ranging from 36 to 54.6 mmol/L (conventional unit range = 36–54.6 mEq/L) have been reported in athletes with a history of cramps.3,18 Thus, for a 2-hour exercise bout, people with cramps could lose up to 5 L of fluid and 5.2 g of Na+. Therefore, if clinicians provide 80 mL of PJ postexercise, they must stress to athletes to drink copious volumes of fluid and supplement their meals with Na+ and K+. Although I did not study this possibility, athletes may be able to replace more of their Na+ and K+ lost by drinking larger volumes of PJ or eating more mustard. However, this is not advised because gastrointestinal distress has been observed when large volumes (eg, approximately 550 mL) of PJ are consumed.31 In contrast, no gastrointestinal distress occurs when participants ingest small volumes (eg, <150 mL) of PJ.14,15
One limitation and one assumption must be addressed. After reading the scientific literature, I do not know how much mustard athletes ingest for EAMCs; some researchers12 have stated athletes ingest a few 5-g packets. My participants ingested a mass of mustard containing an amount of Na+ equivalent to that ingested on the PJ day to allow between-groups comparisons and improve internal validity of the experiment. Athletes are unlikely to ingest this much mustard for EAMCs. However, the negligible changes occurring after mustard ingestion in my study suggest that eating a few mustard packets would have an even smaller effect on the intravascular space. If clinicians provide a few mustard packets, the Na+, K+, and fluid deficits likely will be higher than those I reported. My assumption in this study was that sampling from the intravascular space provides an indication of the fluid and electrolyte conditions of the interstitial space surrounding muscle fibers. Whereas the methods to obtain such measurements are technically daunting, the information would help clarify how ingestion of these treatments affects the fluid closest to the muscle.
CONCLUSIONS
Pickle juice and mustard are 2 anecdotal treatments believed to be effective for treating EAMCs by restoring plasma electrolytes; however, no appreciable changes occurred to [Na+]p, [K+]p, percentage changes in plasma Na+ content, percentage changes in plasma volume, or OSMp of hypohydrated humans within 60 minutes of PJ or mustard ingestion. Pickle juice is unlikely to exacerbate exercise-induced hypertonicity, delay rehydration, or cause hyperkalemia. Moreover, ingesting 80 mL of PJ or a mass of mustard with a similar Na+ content cannot fully replace the Na+ or K+ lost due to exercise-induced sweating. The effects of drinking multiple boluses of PJ after exercise in the heat on electrolytes are unknown and worthy of future research.
ACKNOWLEDGMENTS
I thank Jarett Peikert, LAT, ATC, for his help with data collection.
REFERENCES
- 1.Norris FH, Jr, Gasteiger EL, Chatfield PO. An electromyographic study of induced and spontaneous muscle cramps. Electroencephalogr Clin Neurophysiol. 1956;9(1):139–147. doi: 10.1016/0013-4694(57)90118-9. [DOI] [PubMed] [Google Scholar]
- 2.Cooper ER, Jr, Ferrara MS, Broglio SP. Exertional heat illness and environmental conditions during a single football season in the Southeast. J Athl Train. 2006;41(3):332–336. [PMC free article] [PubMed] [Google Scholar]
- 3.Stofan JR, Zachwieja JJ, Horswill CA, Murray R, Anderson SA, Eichner ER. Sweat and sodium losses in NCAA football players: a precursor to heat cramps? Int J Sport Nutr Exerc Metab. 2005;15(6):641–652. doi: 10.1123/ijsnem.15.6.641. [DOI] [PubMed] [Google Scholar]
- 4.Stone MB, Edwards JE, Stemmans CL, Ingersoll CD, Palmieri RM, Krause BA. Certified athletic trainers' perceptions of exercise associated muscle cramps. J Sport Rehabil. 2003;12(4):333–342. [Google Scholar]
- 5.Bergeron MF. Muscle cramps during exercise: is it fatigue or electrolyte deficit? Curr Sports Med Rep. 2008;7(4):S50–S55. [Google Scholar]
- 6.Shang G, Collins M, Schwellnus MP. Factors associated with a self-reported history of exercise-associated muscle cramps in Ironman triathletes: a case-control study. Clin J Sport Med. 2011;21(3):204–210. doi: 10.1097/JSM.0b013e31820bcbfd. [DOI] [PubMed] [Google Scholar]
- 7.Schwellnus MP, Drew N, Collins M. Increased running speed and previous cramps rather than dehydration or serum sodium changes predict exercise associated muscle cramping: a prospective cohort study in 210 Ironman triathletes. Br J Sports Med. 2011;45(8):650–656. doi: 10.1136/bjsm.2010.078535. [DOI] [PubMed] [Google Scholar]
- 8.Schwellnus MP, Nicol J, Laubscher R, Noakes TD. Serum electrolyte concentrations and hydration status are not associated with exercise associated muscle cramping (EAMC) in distance runners. Br J Sports Med. 2004;38(4):488–492. doi: 10.1136/bjsm.2003.007021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Miller KC, Knight KW, Mack GL, et al. Three percent hypohydration does not affect the threshold frequency of electrically-induced muscle cramps. Med Sci Sports Exerc. 2010;42(11):2056–2063. doi: 10.1249/MSS.0b013e3181dd5e3a. [DOI] [PubMed] [Google Scholar]
- 10.Khan SI, Burne JA. Reflex inhibition of normal cramp following electrical stimulation of the muscle tendon. J Neurophysiol. 2007;98(3):1102–1107. doi: 10.1152/jn.00371.2007. [DOI] [PubMed] [Google Scholar]
- 11.Miller KC, Knight KL, Williams RB. Athletic trainers' perceptions of pickle juice's effects on exercise associated muscle cramps. Athl Ther Today. 2008;13(5):31–34. [Google Scholar]
- 12.Williams R. Those devilish cramps. Train Condition. 2000. 10(9) http://www.momentummedia.com/articles/tc/tc1009/cramps.htm. Published December 2000. Accessed April 23, 2013.
- 13.Williams RB, Conway DP. Treatment of acute muscle cramps with pickle juice: a case report [abstract] J Athl Train. 2000;35((suppl 2)):S24. [Google Scholar]
- 14.Miller KC, Mack G, Knight KL. Electrolyte and plasma changes following ingestion of pickle juice, water, and a common carbohydrate-electrolyte solution. J Athl Train. 2009;44(5):454–461. doi: 10.4085/1062-6050-44.5.454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miller KC, Mack GW, Knight KL, et al. Reflex inhibition of electrically-induced muscle cramps in hypohydrated humans. Med Sci Sports Exerc. 2010;42(5):953–961. doi: 10.1249/MSS.0b013e3181c0647e. [DOI] [PubMed] [Google Scholar]
- 16.Dale RB, Leaver-Dunn D, Bishop P. A compositional analysis of a common acetic acid solution with practical implications for ingestion. J Athl Train. 2003;38(1):57–61. [PMC free article] [PubMed] [Google Scholar]
- 17.Fowkes-Godek S, Bartolozzi AR, Sugarman E, Peduzzi C, Hunkele T, Burkholder R. Blood electrolytes and plasma volume changes in two groups of sodium supplemented NFL players during pre-season [abstract] J Athl Train. 2006;41((suppl 2)):S60. [Google Scholar]
- 18.Bergeron MF. Heat cramps during tennis: a case report. Int J Sport Nutr. 1996;6(1):62–68. doi: 10.1123/ijsn.6.1.62. [DOI] [PubMed] [Google Scholar]
- 19.Sulzer NU, Schwellnus MP, Noakes TD. Serum electrolytes in Ironman triathletes with exercise associated muscle cramping. Med Sci Sports Exerc. 2005;37(7):1081–1085. doi: 10.1249/01.mss.0000169723.79558.cf. [DOI] [PubMed] [Google Scholar]
- 20.Takamata A, Mack GW, Gillen CM, Nadel ER. Sodium appetite, thirst, and body fluid regulation in humans during rehydration without sodium replacement. Am J Physiol. 1994;266((5 pt 2)):R1493–R1502. doi: 10.1152/ajpregu.1994.266.5.R1493. [DOI] [PubMed] [Google Scholar]
- 21.Whaley M. ACSM's Guidelines for Exercise Testing and Prescription. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2006. p. 4. [Google Scholar]
- 22.Casa DJ, Armstrong LE, Hillman SK, et al. National Athletic Trainers' Association position statement: fluid replacement for athletes. J Athl Train. 2000;35(2):212–224. [PMC free article] [PubMed] [Google Scholar]
- 23.Hagan RD, Diaz FJ, Horvath SM. Plasma volume changes with movement to supine and standing positions. J Appl Physiol. 1978;45(3):414–418. doi: 10.1152/jappl.1978.45.3.414. [DOI] [PubMed] [Google Scholar]
- 24.Dill DB, Costill DL. Calculation of percentage changes in volumes of blood, plasma, and red cells in dehydration. J Appl Physiol. 1974;37(2):247–248. doi: 10.1152/jappl.1974.37.2.247. [DOI] [PubMed] [Google Scholar]
- 25.Greenleaf JE, Van Beaumont W, Brock PJ, Morse JT, Mangseth GR. Plasma volume and electrolyte shifts with heavy exercise in sitting and supine positions. Am J Physiol. 1979;236(3):R206–R214. doi: 10.1152/ajpregu.1979.236.3.R206. [DOI] [PubMed] [Google Scholar]
- 26.Baker LB, Stofan JR, Hamilton AA, Horswill CA. Comparison of regional patch collection vs. whole body washdown for measuring sweat sodium and potassium loss during exercise. J Appl Physiol. 2009;107(3):887–895. doi: 10.1152/japplphysiol.00197.2009. [DOI] [PubMed] [Google Scholar]
- 27.Weschler LB. Sweat electrolyte concentrations obtained from within occlusive coverings are falsely high because sweat itself leaches skin electrolytes. J Appl Physiol. 2008;105(11):1376–1377. doi: 10.1152/japplphysiol.00924.2007. [DOI] [PubMed] [Google Scholar]
- 28.Sizer F, Whitney E. Nutrition: Concepts and Controversies. 9th ed. Belmont, CA: Thomson Learning Inc; 2003. pp. A1–A87. [Google Scholar]
- 29.Francesconi RP, Sawka MN, Pandolf KB. Hypohydration and heat acclimation: plasma renin and aldosterone during exercise. J Appl Physiol. 1983;55(6):1790–1794. doi: 10.1152/jappl.1983.55.6.1790. [DOI] [PubMed] [Google Scholar]
- 30.Allen S, Miller K, Albrecht J, Garden-Robinson J, Blodgett-Salafia E. Ad libitum fluid intake and plasma responses following pickle juice, hypertonic saline and deionized water ingestion. J Athl Train. 2013;48(6):734–740. doi: 10.4085/1062-6050-48.5.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miller KC, Mack GW, Knight KL. Gastric emptying after pickle juice ingestion in rested, euhydrated humans. J Athl Train. 2010;45(6):601–608. doi: 10.4085/1062-6050-45.6.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hoffmann ML, DenBleyker M, Smith JC, Stricker EM. Inhibition of thirst when dehydrated rats drink water or saline. Am J Physiol Regul Integr Comp Physiol. 2006;290(5):R1199–R1207. doi: 10.1152/ajpregu.00715.2005. [DOI] [PubMed] [Google Scholar]
- 33.Ettinger PO, Regan TJ, Oldewurtel HA. Hyperkalemia, cardiac conduction, and the electrocardiogram: a review. Am Heart J. 1974;88(3):360–371. doi: 10.1016/0002-8703(74)90473-6. [DOI] [PubMed] [Google Scholar]
- 34.Kristensen M, Juel C. Potassium-transporting proteins in skeletal muscle: cellular location and fibre-type differences. Acta Physiol (Oxf) 2010;198(2):105–123. doi: 10.1111/j.1748-1716.2009.02043.x. [DOI] [PubMed] [Google Scholar]
- 35.Miller AJ. Oral and pharyngeal reflexes in the mammalian nervous system: their diverse range in complexity and the pivotal role of the tongue. Crit Rev Oral Biol Med. 2002;13(5):409–425. doi: 10.1177/154411130201300505. [DOI] [PubMed] [Google Scholar]