Abstract
Carboplatin and paclitaxel as doublet are the standard therapeutic option for advanced stage ovarian carcinoma in the first line as well as relapse. Carboplatin with its better toxicity profile has replaced cisplatin as the first line drug. However, increase in incidence of carboplatin hypersensitivity is alarming. Severity of carboplatin hypersensitivity varies from a mild rash to life-threatening reactions. With an increase in the number of cycles the risk of hypersensitivity reactions increase, which jeopardizes the use of this highly effective drug in a significant proportion of patients. Prompt diagnosis and rapid therapeutic rescue are the key in severe life-threatening reactions. Managing patients with carboplatin hypersensitivity and planning subsequent therapy is thus a therapeutic challenge.
Keywords: Carboplatin, desensitization, hypersensitivity
INTRODUCTION
Platinum analogs have been the standard of care in management of advanced stage epithelial ovarian and fallopian tube carcinoma.[1] Platinum and taxane combination has shown a survival benefit in the firstline as well as in relapse setting.[1,2] Carboplatin being equally efficacious and with better toxicity profile has replaced cisplatin as first choice chemotherapy.[3] However, with increasing use of carboplatin, especially in relapsed settings, there is a notable increase in hypersensitivity reactions (HSRs). Severe HSRs may cause panic among nursing staff and at times can be frightening even for physicians. Further, in usual combination regimen with taxanes, differentiating acute HSR between the two is also a difficult task.
CASE SCENARIO
A 56-year-old postmenopausal woman without known comorbidities was diagnosed with Stage III C ovarian carcinoma 6 months back. She underwent four cycles of neoadjuvant chemotherapy (NACT) with paclitaxel and carboplatin. She had serological response with CA125 decreasing from 1285 U/mL to 90 U/mL post NACT. Subsequently, she underwent interval cytoreduction (R0) with histological evidence of residual viable serous adenocarcinoma and omental metastasis. She underwent three cycles of adjuvant chemotherapy with similar agents. Cycle four and five were uneventful. However, in cycle six, although paclitaxel infusion was uneventful on day 1, on day 2 immediately after starting carboplatin infusion she developed severe HSR. She developed breathlessness, chest discomfort, and flushing followed by unconsciousness. Oxygen saturation plummeted to 85% with hypotension (blood pressure [BP] –80/40 mm Hg) and tachycardia up to 125/min. Infusion was stopped immediately and she was administered intravenous (IV) injections of diphenhydramine 25 mg, hydrocortisone 100 mg, along with IV fluid (bolus normal saline), and salbutamol nebulization 2.5 mg despite of above measures she deteriorated and became pulseless with unrecordable BP. Subsequently, she received mephentermine 15 mg IV and then within a minute she regained consciousness with vital parameters returning to baseline in next few minutes. She was shifted to ward for observation and was discharged the next morning after ensuring stable general condition. Further chemotherapy was abandoned and she was suggested to be on regular follow-up.
DISCUSSION
Incidence of carboplatin induced HSR have been reported widely ranging from 1% to 35% depending upon the severity and grade.[4,5] It has been observed more frequently in women receiving carboplatin in the second line with peak incidence at median number of seven cycles.[6] These reactions could be acute, which manifests within a couple of minutes or delayed, which happens after a couple of hours or days after the inciting drug. Pattern of hypersensitivity constitutes broad spectrum, which may be varied from mild to severe life-threatening reactions. Flushing, rash, itching, diaphoresis, facial edema, fever, chills, nausea, and backache without any cardiorespiratory instability constitute mild nature of reactions, which is one end of the spectrum while hypertension/hypotension, tachycardia, breathlessness, chest pain, palpitation, altered sensorium, wheezing, stridor, laryngeal edema, shock could be serious and life-threatening. These reactions have been reported not only for IV, but also for intraperitoneal route.[7]
Exact mechanism of carboplatin induced hypersensitivity is yet to be elucidated. However, repeated exposure to low dose free platinum metal, which is present as impurity or contaminant in the drug is the likely culprit. This analogy hold true from allergic manifestation in platinum mining workers and why allergic manifestation develop after median seven cycles of carboplatin due to gradual exposure to low metal concentration. Immunologically, immediate type 1 IgE mediated HSR or anaphylactoid reaction mediated by release of vasoactive cytokines and histamines from basophils and mast cells have been postulated. Majority of carboplatin HSR have been reported after a couple of minutes to hour after the administration; however, it is not uncommon to develop a reaction within minutes of starting infusion. This is paradox of paclitaxel induced HSR which typically manifest within few drops or 10 min of infusion.
Platinum analogs have better outcomes in the second line or recurrent ovarian carcinomas with response rates up to 50-70% in platinum sensitive relapses; in.[2,8] Hence, it is pertinent to evolve strategies to counter the carboplatin HSR, which may deprive the patient of an effective drug. Lack of clinical or biochemical marker to stratify patients into high risk for HSR are yet to be defined. However, patients receiving carboplatin after 12 months of platinum free interval have much higher incidence of HSR (50%) as compared with otherwise (25%).[9] Previous history of environmental or drug allergies have been shown to increase the risk of carboplatin HSR in a study with limited sample size.[10] Several methods have been evaluated including skin testing, specific immunoglobulin levels, desensitizing, increasing infusion duration with aggressive premedication and replacing carboplatin with cisplatin with modest success.
Skin testing
Skin testing with prick or intradermal testing with stratified dilution has been useful in predicting patients likely to have HSR to carboplatin. It has high negative predictive value of more than 76% thus helpful in identify patients less likely to have a reaction.[11,12] Skin test done independently for carboplatin and cisplatin can help in identifying patients who have cross resistance to platinum analogs where cisplatin cannot be recommended. However, atypical HSR with negative skin test have been identified.[13] Limitation to skin testing is that it cannot predict the severity of reaction and correlates more with early reaction than late reaction. In a patient with recent suspicion of carboplatin hypersensitivity, it is advisable to consider skin testing. If test is positive avoid carboplatin or consider desensitization before subsequent planned dose.
Procedure
Prick test-It is done on a volar surface of forearm with a drop of carboplatin (10 mg/ml). If prick test is negative then intradermal test with 0.02 ml of 0.1 mg/ml of carboplatin is done. Concentration is increased by 10 times as long as intradermal test remains negative to a maximum of 10 mg/ml, each time on different areas of forearm. All skin tests are interpreted 15 min after application. Prick test is positive if more than 3 mm of wheal is seen, while intradermal test is positive if more than 5 mm of wheal is identified. Patch test has no value in predicting HSR.[11]
Desensitization
Patients with recent history of carboplatin HSR if re-challenged without desensitization are likely to have severe reaction in more than 75% of patient population. In one of largest series reported so far of desensitization, documented by Robinson et al.[6] 100% of patients tolerated subsequent carboplatin without any allergic reaction post IV or oral desensitization. In another series by Rose et al., rate of successful desensitization was more than 90%.[14] However, Markman suggested some reservations regarding the above finding as any significant HSR could potentially be life-threatening even after desensitization in a small group of patients and suggested alternate drugs instead of carboplatin.[15] It is recommended to formulate institutional desensitization protocols, which should be strictly followed for effective, consistent, and safe results. Commonly used methods for desensitization include:
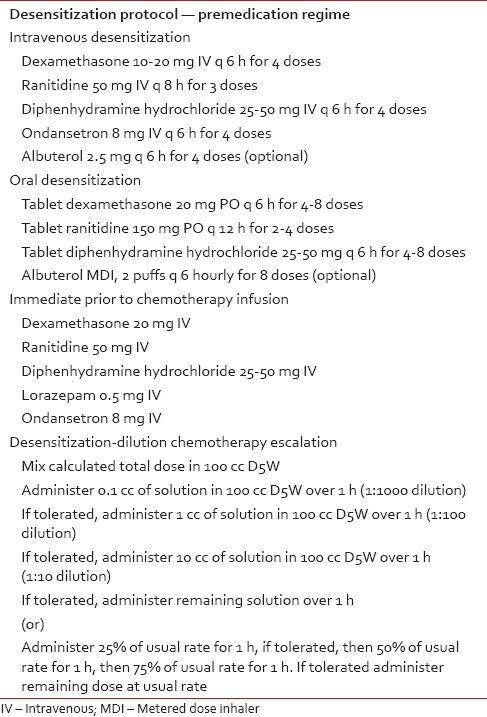
Premedication regimes,
Dilution chemotherapy escalation [Table 1], and
Increasing duration of drug infusion.
Table 1.
Desensitization protocols for carboplatin hypersensitivity reactions
Prophylactic extended infusion schedule over 3 h in a large prospective study has shown to decrease the incidence of HSR to <4% when compared to 21% in standard infusion time schedules.[16] In a patient with platinum sensitive relapse with good evidence of response during previous treatment one can consider desensitization before carboplatin as it can reduce subsequent HSR in the majority of patients.
Substituting carboplatin to cisplatin
Risk of cross sensitivity to platinum analogs is of concern in patients with HSR to carboplatin. Use of desensitization before substituting carboplatin to cisplatin is a viable option. Even without desensitization more than 75% patients do tolerate cisplatin without any HSR, however in 20% of such patients have subsequent reactions to cisplatin after 3 and 4 cycles.[17] In a small series of patients reported by MSKCC, 5 out of 7 patient successfully received cisplatin with adequate premedication and slower infusion rates.[18] Skin testing for cisplatin-carboplatin allergy is an alternate option before starting patients on cisplatin with known HSR to carboplatin. Overall, replacing cisplatin to carboplatin can be attempted preferably after desensitization with adequate premedication and slower infusion rate under strict medical supervision. Despite of above there is a small risk of cross sensitivity, hence substitution can be attempted, but with due caution.
Carboplatin hypersensitivity is one of the major clinical challenges in treating patients with relapse/recurrent ovarian malignancies. Incidence increase to more than one-third when used in the second line setting with increasing risk with each subsequent cycle. There is a paucity of data to suggest that delivering carboplatin on next rather than same day of paclitaxel affects the incidence of hypersensitivity.[8] Some of these hypersensitive reactions could be serious and life-threatening if not dealt urgently especially among less vigilant and untrained personnel. Hence, it is prudent to consider following factors in descending order of importance before deciding to continue treatment with platinum analogs.
Severity of observed reaction.
Strong evidence of current platinum responsive disease/predicted high likelihood of response.
Presence of significant comorbidity that might increase the risk of death with subsequent HSR e.g., recent Myocardial infarction, stroke, and arrhythmia.
Availability of other rational alternative therapeutic options.
Individual patient willingness to treatment with platinum in view of potential risks and possible benefits.
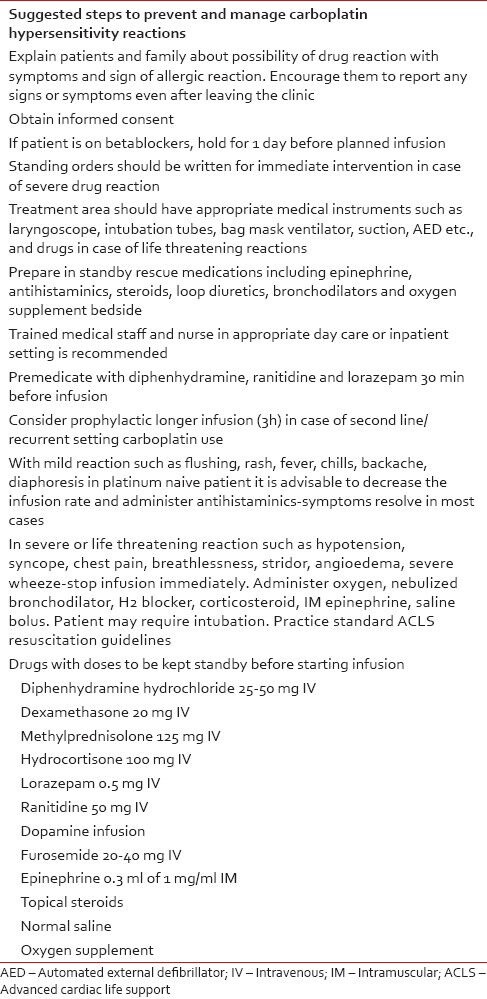
Considering the significance of HSR to carboplatin it is strongly recommended that institution should formulate model protocols to handle severe life-threatening reaction in busy day care or inpatient care. Certain suggestions aimed at preemptive, prophylactic, and primary prevention of HSR are listed in Table 2.
Table 2.
Suggestions for preemptive, prophylactic and primary prevention in management of platinum hypersensitive reactions
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Aabo K, Adams M, Adnitt P, Alberts DS, Athanazziou A, Barley V, et al. Chemotherapy in advanced ovarian cancer: Four systematic meta-analyses of individual patient data from 37 randomized trials. Advanced Ovarian Cancer Trialists’ Group. Br J Cancer. 1998;78:1479–87. doi: 10.1038/bjc.1998.710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Parmar MK, Ledermann JA, Colombo N, du Bois A, Delaloye JF, Kristensen GB, et al. Paclitaxel plus platinum-based chemotherapy versus conventional platinum-based chemotherapy in women with relapsed ovarian cancer: The ICON4/AGO-OVAR-2.2 trial. Lancet. 2003;361:2099–106. doi: 10.1016/s0140-6736(03)13718-x. [DOI] [PubMed] [Google Scholar]
- 3.Ozols RF, Bundy BN, Greer BE, Fowler JM, Clarke-Pearson D, Burger RA, et al. Phase III trial of carboplatin and paclitaxel compared with cisplatin and paclitaxel in patients with optimally resected stage III ovarian cancer: A Gynecologic Oncology Group study. J Clin Oncol. 2003;21:3194–200. doi: 10.1200/JCO.2003.02.153. [DOI] [PubMed] [Google Scholar]
- 4.Markman M. Hypersensitivity reactions to carboplatin. Gynecol Oncol. 2002;84:353–4. doi: 10.1006/gyno.2001.6513. [DOI] [PubMed] [Google Scholar]
- 5.Sliesoraitis S, Chikhale PJ. Carboplatin hypersensitivity. Int J Gynecol Cancer. 2005;15:13–8. doi: 10.1111/j.1048-891x.2005.14401.x. [DOI] [PubMed] [Google Scholar]
- 6.Robinson JB, Singh D, Bodurka-Bevers DC, Wharton JT, Gershenson DM, Wolf JK. Hypersensitivity reactions and the utility of oral and intravenous desensitization in patients with gynecologic malignancies. Gynecol Oncol. 2001;82:550–8. doi: 10.1006/gyno.2001.6331. [DOI] [PubMed] [Google Scholar]
- 7.Shukunami K, Kurokawa T, Kawakami Y, Kubo M, Kotsuji F. Hypersensitivity reactions to intraperitoneal administration of carboplatin in ovarian cancer: The first report of a case. Gynecol Oncol. 1999;72:431–2. doi: 10.1006/gyno.1998.5273. [DOI] [PubMed] [Google Scholar]
- 8.Rose PG, Fusco N, Fluellen L, Rodriguez M. Second-line therapy with paclitaxel and carboplatin for recurrent disease following first-line therapy with paclitaxel and platinum in ovarian or peritoneal carcinoma. J Clin Oncol. 1998;16:1494–7. doi: 10.1200/JCO.1998.16.4.1494. [DOI] [PubMed] [Google Scholar]
- 9.Schwartz JR, Bandera C, Bradley A, Brard L, Legare R, Granai CO, et al. Does the platinum-free interval predict the incidence or severity of hypersensitivity reactions to carboplatin? The experience from Women and Infants’ Hospital. Gynecol Oncol. 2007;105:81–3. doi: 10.1016/j.ygyno.2006.10.047. [DOI] [PubMed] [Google Scholar]
- 10.Markman M, Zanotti K, Kulp B, Peterson G, Markman M. Relationship between a history of systemic allergic reactions and risk of subsequent carboplatin hypersensitivity. Gynecol Oncol. 2003;89:514–6. doi: 10.1016/s0090-8258(03)00155-0. [DOI] [PubMed] [Google Scholar]
- 11.Zanotti KM, Rybicki LA, Kennedy AW, Belinson JL, Webster KD, Kulp B, et al. Carboplatin skin testing: A skin-testing protocol for predicting hypersensitivity to carboplatin chemotherapy. J Clin Oncol. 2001;19:3126–9. doi: 10.1200/JCO.2001.19.12.3126. [DOI] [PubMed] [Google Scholar]
- 12.Markman M, Zanotti K, Peterson G, Kulp B, Webster K, Belinson J. Expanded experience with an intradermal skin test to predict for the presence or absence of carboplatin hypersensitivity. J Clin Oncol. 2003;21:4611–4. doi: 10.1200/JCO.2003.05.539. [DOI] [PubMed] [Google Scholar]
- 13.McAlpine JN, Kelly MG, O’malley DM, Azodi M, Coombe K, Schwartz PE, et al. Atypical presentations of carboplatin hypersensitivity reactions: Characterization and management in patients with gynecologic malignancies. Gynecol Oncol. 2006;103:288–92. doi: 10.1016/j.ygyno.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 14.Rose PG, Fusco N, Smrekar M, Mossbruger K, Rodriguez M. Successful administration of carboplatin in patients with clinically documented carboplatin hypersensitivity. Gynecol Oncol. 2003;89:429–33. doi: 10.1016/s0090-8258(03)00178-1. [DOI] [PubMed] [Google Scholar]
- 15.Markman M. Letter to editor. Gynaec Oncol. 2002;84:353. [Google Scholar]
- 16.O’Cearbhaill R, Zhou Q, Iasonos A, Hensley ML, Tew WP, Aghajanian C, et al. The prophylactic conversion to an extended infusion schedule and use of premedication to prevent hypersensitivity reactions in ovarian cancer patients during carboplatin retreatment. Gynecol Oncol. 2010;116:326–31. doi: 10.1016/j.ygyno.2009.10.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Callahan MB, Lachance JA, Stone RL, Kelsey J, Rice LW, Jazaeri AA. Use of cisplatin without desensitization after carboplatin hypersensitivity reaction in epithelial ovarian and primary peritoneal cancer. Am J Obstet Gynecol. 2007;197:199.e1–4. doi: 10.1016/j.ajog.2007.04.044. [DOI] [PubMed] [Google Scholar]
- 18.Dizon DS, Sabbatini PJ, Aghajanian C, Hensley ML, Spriggs DR. Analysis of patients with epithelial ovarian cancer or fallopian tube carcinoma retreated with cisplatin after the development of a carboplatin allergy. Gynecol Oncol. 2002;84:378–82. doi: 10.1006/gyno.2001.6519. [DOI] [PubMed] [Google Scholar]


