Abstract
PURPOSE
To investigate social support and network features in people with first episode psychosis, and to examine anxiety as a possible mediator between loneliness and a rating of paranoia.
METHOD
Thirty eight people with first-episode psychosis were recruited for a cross-sectional study. Self report questionnaires and structured interviews assessed symptoms, functioning, and qualitative social network and support features. A mood-induction task involved watching anxiety-inducing pictures on a computer screen. Visual analogue scales assessed changes in paranoia, anxiety and loneliness and a mediation analysis was conducted.
RESULTS
One third of the sample (34%) had no confidant (95% CI 18.4%, 50.0%). The average number of weekly contacts was 3.9, with 2.6 lonely days. Poor perceived social support, loneliness and the absence of a confidant were strongly associated with psychosis and depressive symptoms (.35<r’s<.60). The association between loneliness and paranoia was mediated through anxiety (ab=.43, z=3.5; p<.001).
CONCLUSIONS
Even at first episode, a large proportion of people with psychosis have poor perceived support, no confidant and report several lonely days a week. Patients without a confidant appear to be more susceptible to feeling lonely and anxious. Anxiety may be one pathway through which loneliness affects psychosis. Interventions which focus on this are indicated.
Keywords: Social networks, loneliness, anxiety, confidant, first-episode psychosis
Introduction
People with psychosis commonly struggle to develop and maintain functioning relationships and tend to miss out on good social support [1]. While the majority of support and network studies in psychosis have been carried out with long-standing psychosis samples, evidence is accumulating that poor support and network functioning is already demonstrable by, or shortly after, onset [2].
Most studies examining support in first-episode psychosis have focused on quantitative features of the social network such as size and reciprocity rather than more qualitative and functional aspects such as satisfaction with relationships, absence or presence of a confidant, or loneliness. This is important, because objective features of social networks are related but different to these more subjective aspects of social relationships. For example, someone with a large network may actually feel lonely, and perceived social support is not necessarily higher in larger networks [3].
Perceived social support and its satisfaction
People with psychosis tend to perceive their social support to be lower than people from the general population. These findings are particularly convincing for populations with long-standing psychosis [2], but are somewhat mixed for people with a first episode. While some studies found that first-episode samples reported lower levels of perceived support than controls [4, 5], others did not find this [6, 7].
Loneliness in Psychosis
Loneliness results from the discrepancy between the social relationships one wishes to have and those one actually perceives to have [8]. While loneliness is influenced by quantitative aspects of social networks it is predominantly influenced by subjective appraisals [see also 9]. Loneliness has been associated with lower life satisfaction [10], psychosocial problems (e.g. poorer social competence) [11], and mental health difficulties including anxiety and psychosis [12-14]. Although loneliness has been described as a fundamental problem in psychosis [15], very few studies have investigated it.
The importance of a confidant
Another qualitative network feature is the presence or absence of a confidant. Having a confidant has been found to be protective against loneliness, and conversely, its absence is likely to increase feelings of loneliness [16]. In the few studies that examined the role of confidants in first-episode psychosis, patients had significantly fewer confidants compared to controls [6, 17]. Morgan et al. [18] found that first-episode groups were seven times more likely not to have a confidant than the general population.
Mechanisms of social support and networks in psychosis
Mechanisms through which poor social networks and support affect mental health are poorly understood. While recent theoretical attempts have been undertaken [19, 20] the possible links between social support and psychosis symptoms were not addressed. Thus, the question remains: what are the mechanisms through which poor social support and network functioning such as loneliness or low perceived social support make psychosis symptoms worse? Below we hypothesise about two potential pathways and set out to explore anxiety as a potential mediator between loneliness and paranoia.
Loneliness, anxiety and paranoia
A number of pathways linking loneliness and symptoms such as distressing voices or unusual ideas are conceivable. For example, loneliness may directly increase anxiety and depression [11] which in turn may exacerbate symptoms of psychosis [21]. The connections formed with other people often provide a source of belongingness and companionship [19]; unfulfillment of these basic needs may lead to depression and anxiety [22]. Equally, perceiving oneself as socially excluded may directly trigger anxiety [23]. Furthermore, loneliness may distort thinking processes thereby increasing anxiety. For example, everyday events have been found to elicit threat appraisals in lonely, but not in non-lonely people [24]. Also, feeling lonely may make it harder to think of alternatives to unusual ideas and worries which may raise anxiety levels.
Anxiety and psychosis symptoms
Garety et al [25] proposed that anxiety drives a number of dysfunctional processes and behaviours that contribute to psychosis symptoms, such as selective attention (to experiences supporting psychotic beliefs and minimising disconfirmatory evidence), safety behaviours (preventing disconfirmation of beliefs), or meta-cognitive beliefs (e.g. uncontrollability of thoughts). Furthermore, anxiety can produce threat anticipation thus triggering emotional reasoning [26].
Aims of the study
This study examined qualitative aspects of social support and networks in people with first-episode psychosis. We explored one potential pathway (anxiety) between loneliness and paranoia. The following hypotheses were investigated:
Hypothesis 1: Positive and negative symptoms of psychosis and overall functioning are related to qualitative aspects of social networks and social support. Specifically, low satisfaction with social support, loneliness and the absence of a confidant are related to psychosis symptoms.
Hypothesis 2: Predicted associations between reports of feeling lonely and feeling paranoid are significantly reduced when controlling for anxiety (mediation analysis).
2. Material and methods
2.1 Participants
Thirty eight individuals with a first episode in psychosis were recruited from NHS outpatient services within a South London NHS Foundation Trust between October 2011 and April 2012. This study collaborated with a large ongoing epidemiological study of first-episode psychosis which is recruiting all people with a first-episode psychosis presenting within a catchment area in south-east London; those who were interested in participating in further research were recruited into this study. Eligibility criteria were: presence of first-episode psychosis (F20-29; F30-33), no previous contact for psychosis with mental health services; resident in catchment area; age 18-64. Exclusion criteria were: organic psychosis; acute intoxication as defined by ICD.
2.2 Measures
Psychosis symptoms were assessed with the Scale for the Assessment of Positive Symptoms [SAPS, 27] and the Scale for the Assessment of Negative Symptoms [SANS, 28].
Time budget measure
[TBM, 29]. The TBM is an indicator of social functioning and is completed as a structured interview during which the interviewer probes for activities and social contact (see [29] for a detailed description). Scores range from 0-112 with higher scores indicating better functioning.
Center for Epidemiologic Studies Depression Scale (CES-D)
The CES-D is a widely used 20-item self-report questionnaire to measure depressive symptomatology in adults [30]. The clinical cut-off is 16.
The Multidimensional Support Scale (MDSS)
[31] is a self-report scale assessesing availability of social support (listening, trying to understand) and perceived adequacy and satisfaction with it from three different groups: confidants (family and close friends), peers (e.g. others suffering the same illness), and mental health professionals (psychologist, psychiatrists and key workers). Reliability and validity are good [31].
Loneliness
This 1-item question asks individuals about how many days they felt lonely and in need of companionship in the past week. Similar single-item measures of loneliness were used in past studies [32].
Confidant
This 1-item question asks individuals whether they have anyone to confide in (previously used successfully in psychosis studies, e.g. [33]).
2.3 Mood induction task
Participants watched two picture sets (15 pictures each): “Mild anxiety-provoking pictures” and “Neutral/happy pictures” on a computer screen. Pictures were drawn from the International Affective Picture System [IAPS, 34] and from an online picture database1. Pictures were randomised and presented for 6 seconds followed by a 1 second interval using the experimental software PsychoPy2. Pre-post changes in affect, loneliness and paranoia3 were measured with visual analogue scales that were filled out prior to the presentation of the pictures (baseline) and after each picture set. Participants indicated how they were feeling right now with regards to each of the items on a scale from 0-100.
2.4 Procedure
The study was approved by the local research ethics committee. Participants first completed the SAPS, SANS, and TBM, followed by the CES-D, MDSS and the loneliness and confidant items. Next, the picture viewing task was carried out. At the end of the session, participants were debriefed and reimbursed. Each participant was contacted by telephone one week after the assessment to enquire about their mental health and signpost them to relevant services and support, if required. However, none of the participants reported being negatively affected by the session.
2.5 Data Analysis
Statistical analyses were performed with SPSS version 19. Hypothesised relationships between loneliness, paranoia and anxiety were tested with a simple mediation model using Preachers and Hayes’ [35] SPSS Sobel-test with bootstrapping4. It was tested whether the predicted relationship between loneliness and paranoia was significantly reduced when controlling for anxiety. This would indicate that anxiety may be a potential mediator between loneliness and paranoia. We report two-tailed levels of significance; values of p < 0.05 were considered significant.
3. Results
Demographic information of the sample is provided in Table 1. The sample was predominantly young and male, with around one third from an ethnic minority background. Forty nine participants were referred to this study, and 11 refused to participate because they either moved away or lost their interest in participating in further research thus resulting in an overall sample size of 38.
Table 1.
Demographic and clinical characteristics of the sample (N=38)
| Variable | N (%) | Mean (SD) |
|---|---|---|
| Sex | ||
| Male | 23 (60.5%) | |
| Female | 15 (39.5%) | |
| Age | 32.3 (9.6) , [range 21-56] | |
| Ethnic origin | ||
| White | 20 (52.6%) | |
| Black | 13 (34.2%) | |
| Other | 5 (13.3%) | |
| Years of education | 14.5 (3.9) | |
| English Language | ||
| Native | 32 (84.2%) | |
| Non-native | 6 (15.8%) | |
| Duration of untreated | (N=36) | Median: 12 |
| psychosis (DUP)* | Min: 0, Max: 2652 | |
| CES-D | 21.5 (12.9) |
DUP is defined here as time elapsed from onset of symptoms till beginning of treatment in weeks. The distribution of this sample was skewed because of two outliers with extremely long DUPs with onset of symptoms before the age of 16. Therefore, the Median is reported as it represents a more accurate measure of central tendency than the mean DUP. Data is missing for two participants.
Clinical characteristics of the sample and social network and social support measures are presented in Table 2. On average, participants had 3.9 contacts a week, with 2.6 lonely days a week. Thirty four percent (n=13) of the sample did not have a confidant (95% CI 18.4%, 50.0%). A paired t-test showed, that at the time of assessment, participants had significantly fewer positive symptoms (SAPS) than during the worst part of their first episode (t (36) = 8.7, p < .001) indicating that many were in remission. The sample reported clinically depressive symptoms. Overall functioning as measured with the Time Budget Measure was relatively high compared to more long term psychosis samples (Jolley et al.[29]; mean score of high activity sample = 53), however, activities varied, with some participants spending their time mostly lying in bed compared to others working full time and having an active social life.
Table 2.
Clinical characteristics and social support measures of sample
| Variable | Mean (SD), [range] |
|---|---|
| Psychosis symptoms | |
| SAPS – worst episode | 9.4 (4.2), [0-15] |
| SAPS - current | 2.9 (4.3), [0-15] |
| SANS – current | 5.8 (5.5), [0-19] |
| Overall functioning | |
| Time Budget Measure | 58.8 (22.9), [11-108] |
| Depressive Symptoms | |
| CES-D | 21.5 (12.9), [3-52] |
| Multidimensional Support Scale | |
| Perceived availability social support - friends & family | 15.8 (4.7, [9-24] |
| Satisfaction with social support - friends & family | 13.9 (3.9) , [6-18] |
| Perceived availability social support - experts | 13.9 (4.3) , [5-20] |
| Satisfaction with social support - experts | 12.3 (3.4), [5-15] |
| Number friends and family seen in the past week | 3.9 (4.4), [0-25] |
| Number of lonely days in the past week | 2.6 (2.7), [0-7] |
| Confidant (Frequency) | No: 13 (34.2%) |
| Yes: 25 (65.8%) |
3.1 Associations of symptoms with social network and support variables
Table 3 presents the correlations between clinical and social support variables. Hypothesis 1 was well supported by the data. Current psychosis symptoms strongly correlated with social support measures. More specifically, low ‘satisfaction with social support from friends and family’ was associated with more and severe current positive and negative symptoms. Equally, feeling lonely and not having a confidant related strongly to severe positive and negative symptoms and poorer functioning.
Table 3.
Associations of current psychosis symptoms, overall functioning and depressive symptoms with social support and network variables. Significant correlations are presented in bold.
| Symptoms and functioning | Perceived availability of social support (family & friends) | Satisfaction with social support (family & friends) | Perceived availability of social support (experts) | Satisfaction with social support (experts) | Number of lonely days in past week | Confidant** |
|---|---|---|---|---|---|---|
| SAPS | −.22 | −.35* | −.30 | −.28 | .41* | −.40* |
| SANS | .09 | −.38* | .08 | .06 | .46** | −.43** |
| Time Budget | −.00 | .29 | −.03 | .00 | −.30 | .29 |
| CES-D | −.24 | −.60** | −.30 | −.45** | .66** | −.49** |
Spearman’s rank correlations are reported
Point-biseral correlation; binary variable coded with 0=no confidant, 1=confidant, hence negative correlations with symptom scores indicate participants with no confidant have more symptoms. Positive correlations with the Time Budget Measure indicate that those without a confidant have poorer functioning.
Note, significant correlations are indicated with * p<.05, ** p<.01
Control analyses
Control analyses were carried out with a number of potential confounds, namely ‘Duration of untreated psychosis’ (DUP), ‘Gender’, and ‘Age of onset’. First, it was tested whether any of the potential confounds correlated with either the support, network or symptom variables. In case of significant correlations, partial correlations tested whether significant associations between support and symptom variables were affected by potential confounds. DUP was significantly associated with more current positive symptoms (SAPS, r = .59, p < .001), and depression (CES-D, r = .43, p = .01) but not with current negative symptoms (SANS, r = .26, p = .13). DUP was also negatively associated with ‘Perceived availability of support by friends and family’ (r =−.48, p = .003) and ‘Satisfaction with support by friends and family’ (r = −.39, p = .02), but not with ‘Number of lonely days’ (r = .27, p = .1) and ‘Confidant’ (r = −.31, p = .07). Associations of ‘Satisfaction with support by friends and family’ with SAPS and CES-D were not affected by DUP. Neither, ‘Gender’ and ‘Age of onset’ were associated with any of the support, network or symptom variables (.07 < p < .95).
Exploratory analysis
An exploratory t-test compared participants with and without a confidant on number of lonely days in the previous week. Those participants without a confidant reported significantly more lonely days than those with a confidant (t (36) = 3.25, p = 0.002, η2= .23).
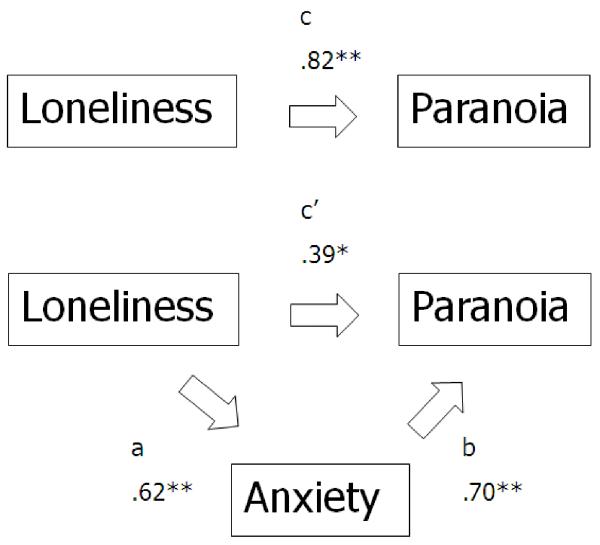
The following section describes the analysis of the hypothesised relationships between feelings of loneliness, paranoia and anxiety. First, Pearson correlations showed, as expected, that feelings of loneliness were significantly associated with feelings of paranoia after anxiety-induction (r = .71, p < .001). Second, the Sobel test was carried out with loneliness as the independent variable, paranoia as the dependent variable and anxiety as the putative mediator variable. In line with the hypothesis, the Sobel test was confirmed the indirect mediation effect (ab= .43, z = 3.5; p < .001) suggesting that the pathway between feeling lonely and feeling paranoid was at least partially mediated by anxiety. The mediation model is shown in Figure 1.
Figure 1.
Results of the hypothesised mediation model with anxiety as a mediator between loneliness and paranoia (numbers represent the partial regression coefficients). The correlation between loneliness and paranoia dropped significantly when controlling for anxiety thus suggesting that anxiety may function as a partial mediator. **p< .01
4. Discussion
Even at first-episode, participants reported high levels of loneliness and one third did not have a confidant. These finding underline that even at onset, people with psychosis are having to deal with poor levels of social support and some isolation, a finding confirmed by a recent systematic review [2].
As predicted, low satisfaction with social support, loneliness and the absence of a confidant were significantly associated with current psychosis and depressive symptoms in people with a first episode. These results replicate previous findings [1, 38] and extend these by further highlighting the importance of qualitative experiences of supportive relationships for current psychotic and depressive symptomatology.
Perceived social support
Satisfaction with perceived social support was more strongly related to current symptoms than perceived availability of it. Those participants who were unsatisfied with their social support had more psychosis symptoms and were significantly more depressed than those who were satisfied. This finding is in line with Norman et al.’s [1] study and is also consistent with Winefield and colleagues’ [31] original data which showed that higher satisfaction with supportive relationships was inversely related to depression. It is likely that many people with psychosis do in fact have social support in place [39], but this may not be beneficial for their mental-health if the social support is seen as poor and inadequate.
Loneliness
In line with Hypothesis 1, both psychosis symptom clusters were associated with loneliness. This finding further extends the current literature and links in with Neelman and Power’s [13] study showing that people with psychosis felt lonelier than other patient groups and highlights the overall importance that loneliness has for our mental well-being [19].
Confidant
More than one third of the sample did not have a confidant, and it was these people who had elevated current psychosis and depressive symptoms. Not having a confidant and feeling lonely are highly related [16], and those without a confidant reported significantly more lonely days. Although this study did not obtain quantitative data on the distress associated with not having a confidant, some participants reported that they found the absence of a confidant upsetting.
Ibarra-Rovillard and Kuiper [40] suggested that it is the fulfilment of psychological needs through which social relationships exert their effect on our well-being. Being without someone to confide in, or feeling lonely and isolated, may be illustrative of how this very basic need may be thwarted continuously in this particular population.
Functioning and social support
This study also incorporated an indicator of overall functioning [41]. Low overall functioning was not statistically associated with the social support and variables. This is in contrast to previous studies [42]. However, the pattern of the direction of the non-significant correlations pointed in the hypothesised direction, with most correlations reaching near significance, hence those analyses may have been under-powered.
Anxiety as a mediator between loneliness and paranoia
Loneliness was associated with a main symptom of psychosis, a rating of paranoia, and, in line with Hypothesis 2, this effect was partially mediated by anxiety. This suggests that anxiety may indeed be one potential pathway through which loneliness may drive paranoia. It was suggested that loneliness may distort thinking processes by exaggerating threat appraisals [24]. Alternatively, lonely people may find it harder to think of alternatives to their unusual ideas because they have no one to discuss them with; this may raise anxiety levels thus exacerbating paranoia [25, 26].
Limitations
The current study has limitations.
Firstly, this study is cross sectional and its correlations need to be seen as indicative. Secondly, we showed a large number of correlations between social support and symptom measures thereby significantly increasing the risk of false positive findings due to multiple testing. Thirdly, the sample size was relatively small (N = 38) thus potentially limiting the generalizability of the findings. Nevertheless, reported correlations between symptoms and support and network measures are in line with other first-episode studies [1].
Fourthly, it would have been desirable to include a healthy control group. This would have allowed an investigation of whether mood induction would trigger feelings of paranoia and loneliness in the general population.
Clinical implications
Given the brevity of the support measures, they may be suitable for routine clinical practice. The results particularly suggest focusing on measuring actual experience (perceptions) of social support (satisfaction, loneliness). Asking service users whether they have a confidant may provide particularly useful clinical information.
Results from the mediation analysis are in line with cognitive models of psychosis [25] emphasising the role of individual appraisals of the unusual experience in the formation and maintenance of symptoms. Since directly addressing poor social network functioning in therapy (e.g. by improving social skills) has proven to be difficult [14, 43], alternative approaches should be considered. These results suggest that it may be more fruitful to directly target dysfunctional appraisals of relationships and of loneliness, as discussed by Sündermann et al. [44] and Meltzer et al. [14]. This is also in line with research showing that loneliness is more influenced by subjective appraisals of the social relationships than by its objective features [11].
Concluding remarks
Social support networks and social support have been found to be relatively low shortly after a first episode of psychosis, and relate to feelings of loneliness, and affective and psychosis symptoms, particularly if the person does not have a confidant, which was true of more than one third of this sample. Intervening to develop more adaptive appraisals of loneliness, more positive appraisals of the perceived social support, and to improve activity levels to reduce isolation and access to a confidant, is indicated.
Acknowledgments
This work was supported by the Wellcome Trust (Grant Number: WT087417) and the Department of Health via the National Institute for Health Research (NIHR) Specialist Biomedical Research Centre for Mental Health award to South London and Maudsley NHS Foundation Trust (SLaM) and the Institute of Psychiatry at King’s College London. Craig Morgan is supported by funding from the Medical Research Council (Ref: G0500817), Wellcome Trust (Grant Number: WT087417) and European Union (European Community’s Seventh Framework Program (grant agreement No. HEALTH-F2-2009-241909) (Project EU-GEI)).
Footnotes
Paranoia was broadly defined as “feeling a sense of threat” and clarified whenever participants were unclear to the terms.
The Sobel test [36] tests the indirect effect the independent variable has on the dependent variable via the mediator. Bootstrapping is recommended for inference about indirect effects, especially in small to moderate sample sizes (20-80) [35, 37].
Declaration of interests
None.
References
- 1.Norman RMG, Malla AK, Manchanda R, et al. Social support and three-year symptom and admission outcomes for first episode psychosis. Schizophr Res. 2005;80(2):227–234. doi: 10.1016/j.schres.2005.05.006. [DOI] [PubMed] [Google Scholar]
- 2.Gayer-Anderson C, Morgan C. Social networks, support and early psychosis: a systematic review. Epidemiol Psichiat S. 2012;1(1):1–16. doi: 10.1017/S2045796012000406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Macdonald EM, Jackson HJ, Hayes RL, et al. Social skill as determinant of social networks and perceived social support in schizophrenia. Schizophr Res. 1998;29(3):275–86. doi: 10.1016/s0920-9964(97)00096-0. [DOI] [PubMed] [Google Scholar]
- 4.Veling W, Hoek HW, Wiersma D, Mackenbach JP. Ethnic Identity and the Risk of Schizophrenia in Ethnic Minorities: A Case-Control Study. Schizophrenia Bulletin. 2010;36(6):1149–1156. doi: 10.1093/schbul/sbp032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Song YY, Kim KR, Park JY, et al. Associated Factors of Quality of Life in First-Episode Schizophrenia Patients. Psychiatr Invest. 2011;8(3):201–206. doi: 10.4306/pi.2011.8.3.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Macdonald EM, Hayes RL, Baglioni AJ. The quantity and quality of the social networks of young people with early psychosis compared with closely matched controls. Schizophrenia Research. 2000;46(1):25–30. doi: 10.1016/s0920-9964(00)00024-4. [DOI] [PubMed] [Google Scholar]
- 7.Pruessner M, Iyer SN, Faridi K, et al. Stress and protective factors in individuals at ultra-high risk for psychosis, first episode psychosis and healthy controls. Schizophr Res. 2011;129(1):29–35. doi: 10.1016/j.schres.2011.03.022. [DOI] [PubMed] [Google Scholar]
- 8.Peplau LA, Perlman D. Loneliness: A sourcebook of current theory, research, and therapy. John Wiley & Sons Inc; 1982. [Google Scholar]
- 9.Asher SR, Paquette JA. Loneliness and peer relations in childhood. Curr Dir Psychol Sci. 2003;12(3):75–78. [Google Scholar]
- 10.Schumaker JF, Shea JD, Monfries MM, Groth-Marnat G. Loneliness and life satisfaction in Japan and Australia. The Journ of Psych. 1993;127(1):65–71. doi: 10.1080/00223980.1993.9915543. [DOI] [PubMed] [Google Scholar]
- 11.Heinrich LM, Gullone E. The clinical significance of loneliness: A literature review. Clin Psychol R. 2006;26(6):695–718. doi: 10.1016/j.cpr.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 12.DeNiro DA. Perceived Alienation in Individuals with Residual-Type Schizophrenia. Issues in Mental Health Nursing. 1995;16(3):185–200. doi: 10.3109/01612849509006934. [DOI] [PubMed] [Google Scholar]
- 13.Neeleman J, Power MJ. Social support and depression in three groups of psychiatric patients and a group of medical controls. Soc Psychiatry Psychiatr Epidemiol. 1994;29(1):46–51. doi: 10.1007/BF00796448. [DOI] [PubMed] [Google Scholar]
- 14.Meltzer H, Bebbington P, Dennis M, et al. Feelings of loneliness among adults with mental disorder. Soc Psychiatry Psychiatr Epidemiol. 2012;48(1):5–13. doi: 10.1007/s00127-012-0515-8. [DOI] [PubMed] [Google Scholar]
- 15.Fromm-Reichmann F. Loneliness. Psychiatry: Journal for the Study of Interpersonal Processes. 1959 [Google Scholar]
- 16.Green LR, Richardson DS, Lago T, Schatten-Jones EC. Network correlates of social and emotional loneliness in young and older adults. Pers Soc Psychol Bull. 2001;27(3):281–288. [Google Scholar]
- 17.Erickson DH, Beiser M, Iacono WG, et al. The role of social relationships in the course of first-episode schizophrenia and affective psychosis. Am J Psychiat. 1989;146(11):1456–1461. doi: 10.1176/ajp.146.11.1456. [DOI] [PubMed] [Google Scholar]
- 18.Morgan C, Kirkbride J, Hutchinson G, et al. Cumulative social disadvantage, ethnicity and first-episode psychosis: a case-control study. Psych Med. 2008;38(12):1701–1715. doi: 10.1017/S0033291708004534. [DOI] [PubMed] [Google Scholar]
- 19.Thoits PA. Mechanisms linking social ties and support to physical and mental health. J Health Soc Behav. 2011;52(2):145. doi: 10.1177/0022146510395592. [DOI] [PubMed] [Google Scholar]
- 20.Lakey B, Orehek E. Relational regulation theory: A new approach to explain the link between perceived social support and mental health. Psych Rev. 2011;118(3):482. doi: 10.1037/a0023477. [DOI] [PubMed] [Google Scholar]
- 21.Freeman D, Garety PA. Connecting neurosis and psychosis: the direct influence of emotion on delusions and hallucinations. Behaviour research and therapy. 2003;41(8):923–947. doi: 10.1016/s0005-7967(02)00104-3. [DOI] [PubMed] [Google Scholar]
- 22.Weeks DG, Michela JL, Peplau LA, Bragg ME. Relation between loneliness and depression: A structural equation analysis. J Pers Soc Psychol. 1980;39(6):1238. doi: 10.1037/h0077709. [DOI] [PubMed] [Google Scholar]
- 23.Leary MR. Responses to social exclusion: Social anxiety, jealousy, loneliness, depression, and low self-esteem. J Soc Clin Psychol. 1990;9(2):221–229. [Google Scholar]
- 24.Hawkley LC, Burleson MH, Berntson GG, Cacioppo JT. Loneliness in everyday life: Cardiovascular activity, psychosocial context, and health behaviors. J Pers Soc Psychol. 2003;85(1):105–120. doi: 10.1037/0022-3514.85.1.105. [DOI] [PubMed] [Google Scholar]
- 25.Garety PA, Kuipers E, Fowler D, et al. A cognitive model of the positive symptoms of psychosis. Psych Med. 2001;31(2):189–95. doi: 10.1017/s0033291701003312. [DOI] [PubMed] [Google Scholar]
- 26.Freeman D. Suspicious minds: the psychology of persecutory delusions. Clinical Psychology Review. 2007;27(4):425–57. doi: 10.1016/j.cpr.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 27.Andreasen NC. Scale for the Assessment of Positive Symptoms (SAPS) City of Iowa, Iowa City: 1984. [Google Scholar]
- 28.Andreasen NC. Scale for the Assessment of Negative Symptoms (SANS) City of Iowa, Iowa City: 1984. [PubMed] [Google Scholar]
- 29.Jolley S, Garety PA, Ellett L, et al. A validation of a new measure of activity in psychosis. Schizophr Res. 2006;85(1):288–95. doi: 10.1016/j.schres.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 30.Radloff LS. The CES-D Scale: A Self Report Depression Scale for Research in the General. Applied psychological measurement. 1977;1(3):385–401. [Google Scholar]
- 31.Winefield HR, Winefield AH, Tiggemann M. Social support and psychological well-being in young adults: The Multi-Dimensional Support Scale. J Pers Assess. 1992;58(1):198–210. doi: 10.1207/s15327752jpa5801_17. [DOI] [PubMed] [Google Scholar]
- 32.Rook KS. Social support versus companionship: effects on life stress, loneliness, and evaluations by others. J Pers Soc Psychol. 1987;52(6):1132–47. doi: 10.1037//0022-3514.52.6.1132. [DOI] [PubMed] [Google Scholar]
- 33.Onwumere J, Kuipers E, Bebbington P, et al. Patient perceptions of caregiver criticism in psychosis: links with patient and caregiver functioning. J Nerv Ment Dis. 2009;197(2):85–91. doi: 10.1097/NMD.0b013e3181960e57. [DOI] [PubMed] [Google Scholar]
- 34.Lang PJ, Bradley MM, Cuthbert BN. International affective picture system (IAPS): Technical manual and affective ratings. NIMH Center for the Study of Emotion and Attention; 1997. [Google Scholar]
- 35.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Beh Res M. 2004;36(4):717–731. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 36.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Soc Method. 1982;13:290–312. 1982. [Google Scholar]
- 37.Preacher KJ, Leonardelli GJ. Calculation for the Sobel test: An interactive calculation tool for mediation tests. 2001 Retrieved September 10, 2005.
- 38.Horan WP, Subotnik KL, Snyder KS, Nuechterlein KH. Do recent-onset schizophrenia patients experience a “social network crisis”? Psychiatry. 2006;69(2):115–29. doi: 10.1521/psyc.2006.69.2.115. [DOI] [PubMed] [Google Scholar]
- 39.Forrester-Jones R, Carpenter J, Coolen-Schrjiner P, et al. Good friends are hard to find? The social networks of people with mental illness 12 years after deinstitutionalisation. J Ment Health. 2012;21(1):4–14. doi: 10.3109/09638237.2011.608743. [DOI] [PubMed] [Google Scholar]
- 40.Ibarra-Rovillard M, Kuiper NA. Social support and social negativity findings in depression: Perceived responsiveness to basic psychological needs. Clin Psych Rev. 2011;31(1):342–352. doi: 10.1016/j.cpr.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 41.Jolley S, Garety P, Dunn G, et al. A pilot validation study of a new measure of activity in psychosis. Soc Psychiatry Psychiatr Epidemiol. 2005;40(11):905–911. doi: 10.1007/s00127-005-0982-x. [DOI] [PubMed] [Google Scholar]
- 42.Faccincani C, Mignolli G, Platt S. Service utilisation, social support and psychiatric status in a cohort of patients with schizophrenic psychoses:: A 7 year follow-up study. Schizophr Res. 1990;3(2):139–146. doi: 10.1016/0920-9964(90)90047-b. [DOI] [PubMed] [Google Scholar]
- 43.Kawachi I, Berkman LF. Social ties and mental health. J Urban Health. 2001;78(3):458–67. doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sündermann O, Onwumere J, Bebbington P, Kuipers E. Social networks and support in early psychosis: potential mechanisms. Epidemiology and Psychiatric Sciences. 2012;1(1):1–4. doi: 10.1017/S2045796012000601. doi: 10.1017/S2045796012000601. [DOI] [PMC free article] [PubMed] [Google Scholar]