Abstract
AIM: To examine the incidence of hepatitis E (HepE) in individuals with acute liver injury severe enough to warrant treatment at a transplant unit.
METHODS: Hepatitis E virus (HEV) is an emerging pathogen in developed countries causing severe illness, particularly in immunocompromised patients or those with underlying chronic liver disease. HepE infection is often under diagnosed, as clinicians can be reluctant to test patients who have not travelled to regions traditionally considered hyperendemic for HepE. There are few data regarding the significance of HEV in patients with very severe acute liver injury in developed countries. Eighty patients with acute severe liver injury attending the Scottish Liver Transplant unit were tested for HEV and anti-HEV IgG and IgM. Severe acute liver injury was defined as a sudden deterioration in liver function confirmed by abnormal liver function tests and coagulopathy or presence of hepatic encephalopathy. Eighty percent of these patients were diagnosed with paracetomol overdose. No patients had a history of chronic or decompensated chronic liver disease at time of sampling. IgG positive samples were quantified against the World Health Organization anti-HEV IgG standard. Samples were screened for HEV viral RNA by quantitative reverse transcription polymerase chain reaction.
RESULTS: Four cases of hepatitis E were identified. Three of the four cases were only diagnosed on retrospective testing and were initially erroneously ascribed to drug-induced liver injury and decompensated chronic liver disease, with the cause of the decompensation uncertain. One case was caused by HEV genotype 1 in a traveller returning from Asia, the other three were autochthonous and diagnosed on retrospective testing. In two of these cases (where RNA was detected) HEV was found to be genotype 3, the most prevalent genotype in developed countries. Three patients survived, two of whom had been misdiagnosed as having drug induced liver injury. The fourth patient died from sepsis and liver failure precipitated as a result of hepatitis E infection and previously undiagnosed cirrhosis. Histopathology data to date is limited to mainly that seen for endemic HepE. All patients, with the exception of patient 1, demonstrated characteristics of HepE infection, as seen in previously described locally acquired cases.
CONCLUSION: In patients with acute severe liver injury, HEV testing should be part of the initial diagnostic investigation algorithm irrespective of suspected initial diagnosis, age or travel history.
Keywords: Virology, Infection, Acute liver injury, Hepatitis E virus
Core tip: Misdiagnosis of hepatitis E infection in drug induced liver injury has been noted in patients previously in South East England (13%) and the United States (3%). However, hepatitis E virus is still not given precedence when diagnosing these individuals. In our study, 5% of individuals tested were misdiagnosed and viraemic. It is an important clinical point that the diagnosis of drug induced liver injury is not secure without first excluding hepatitis E, irrespective of travel history, particularly in patients with elevated transaminases.
INTRODUCTION
Hepatitis E has previously been considered a disease of developing countries. In these hyperendemic settings hepatitis E often occurs in large outbreaks involving hundreds or thousands of cases, such as the recent epidemic in south Sudan[1,2]. In such geographical settings hepatitis E virus (HEV) is spread oro-faecally via infected water supplies. Most patients recover, but the mortality rate is high in pregnant females and patients with underlying chronic liver disease[2]. Over recent years, locally acquired hepatitis E has been reported from many developed countries, where it is considered to be a porcine zoonosis[3]. Locally acquired acute hepatitis E is more common in middle aged and elderly males, and in most patients causes a self-limiting hepatitis which last 4-6 wk[4].
In some European countries such as England, France and Germany, a large number of sporadic cases of locally acquired hepatitis E have been documented. For example, in 2011, 454 cases of laboratory-confirmed cases were documented in England and Wales[5] (http://www.hpa.org.uk/hpr/archives/2012/news3212.htm#hev), and these were mostly locally acquired. In contrast, in the United States only a handful of cases have been documented[6] despite an anti-HEV seroprevalence of 21%[7]. This suggests that sub-clinical and/or unrecognised infection is common.
In developed countries, there have been very few previous studies of HEV in patients with acute liver injury severe enough to warrant assessment and treatment at a liver transplant unit. The aim of this study was to retrospectively determine the role and contribution of HEV infection in patients presenting with acute severe liver injury to the Scottish Liver Transplantation Unit (SLTU), Edinburgh, Scotland.
MATERIALS AND METHODS
The SLTU admits patients from hospitals in Scotland with severe acute liver injury for assessment and treatment, and covers a population of 5254800 (http://www.gro-scotland.gov.uk/files2/stats/annual-review-2011/rgar 2011.pdf). The cohort studied included 80 patients with severe acute liver injury admitted to the SLTU between December 2008 and May 2012 (Tables 1 and 2). Severe acute liver injury was defined as a sudden deterioration in liver function confirmed by abnormal liver function tests and coagulopathy or presence of hepatic encephalopathy[8]. No patients had a history of chronic or decompensated chronic liver disease. The majority (80%) of cohort patients were referred to SLTU in the context of paracetamol overdose (POD). The other aetiologies are reflective of the diversity of patients referred to the unit. Despite the large proportion of POD cases within the cohort we felt HEV testing was justified given that infection with hepatitis A, hepatitis C andthere are several publications implicating HEV in the misdiagnosis of POD and DILI.[9-14]. Also, paracetamol ingestion is common in patients with viral hepatitis and may lead to confusion as to the cause liver injury[15].
Table 1.
Patient cohort
| n |
Gender |
Age | ALT | Bilirubin | Creatinine | PT | WBC | Liver | Outcome | |
| Male | Female | mean ± SD | (10-50 IU/L) | (< 17 μmol/L) | (45-110 μmol/L) | (8-12 s) | (4.3-10.8 ×109 cells/L) | failure1 | ||
| 80 | 36 (45%) | 44 (55%) | 38.7 ± 14.1 | 5112 ± 3492 | 118 ± 96 | 181 ± 136 | 52 ± 34 | 9.96 ± 6.51 | 47 (58.8%) | SWOTX 54 (67.5%) SWTX 11 (18.3%) Died 15 (13.8%) |
Defined as loss of hepatic cellular function and subsequent development of coagulopathy, jaundice and encephalopathy. Normal range indicated in brackets. ALT: Alanine aminotransferase; PT: Prothrombin time; WBC: White blood cell; SWOTX: Survived without transplant; SWTX: Survived with transplant.
Table 2.
Prevalence of patient
| Diagnosis | POD | Acute viral hepatitis | Autoimmune hepatitis | Post LTX graft nonfunction | Fatty liver of pregnancy | Malignancy | DILI | Acute porphyria | Ischaemic hepatitis |
| Prevalence | 64 (80%) | 61 (7.5%) | 3 (3.75%) | 2 (2.5%) | 1 (1.25%) | 1 (1.25%) | 1 (1.25%) | 1 (1.25%) | 1 (1.25%) |
The causes of acute viral hepatitis prior to retrospective testing were acute hepatitis B (n = 3), acute hepatitis C (n = 1), and acute hepatitis E (n = 1, case 4 who had travelled to India and was tested for hepatitis E virus at presentation). The diagnoses described are the diagnoses before retrospective testing for hepatitis E virus was undertaken. POD: Paracetamol overdose; LTX: Liver transplant; DILI: Drug induced liver injury.
Serum samples from all 80 patients, taken at presentation and stored at -80 °C[16], were tested for the presence of anti-HEV IgM and IgG antibodies and HEV RNA. Antibody screening was carried out using commercial assays for anti-HEV IgM and IgG (Wantai, Beijing, PR China) according to manufacturer’s instructions. IgG positive samples were quantified against the World Health Organization (WHO) anti-HEV IgG standard. HEV RNA screening was carried out using a HEV pan-genotype quantitative reverse transcription polymerase chain reaction assay with taqman probe and primer sequences targeting the open reading frame (ORF)2/3 region of the HEV genome described by Jothikumar et al[17]. RNA positive samples were quantified against the WHO HEV RNA standard and the limit of detection of the assay was determined to be 250 WHO IU/mL. Positive samples underwent conventional PCR using primer sequences targeting the ORF2 region previously described by Erker et al[18]. Cloning of the ORF2 amplicons was performed using the pGem-T-Easy vector (Promega, Southampton, United Kingdom) and sequenced (GATC, Konstanz, Germany). Sequence data was aligned against known HEV genotype sequences using alignment software ClustalW2 (http://www.ebi.ac.uk/Tools/msa/clustalw2/). The Health Protection Agency guidelines for HEV diagnosis were followed when assigning diagnoses in this study. Briefly, the criteria for diagnosing an acute HEV infection is defined as; clinical and/or biochemical findings consistent with acute viral hepatitis together with virology laboratory markers consistent with acute infection; this must include the detection of HEV RNA. Laboratory markers of probable cases must include the detection of anti-HEV IgG and IgM antibodies but allows for the absence or non-testing of HEV RNA (http://www.hpa.org.uk/webc/HPAwebFile/HPAweb_C/1287146735973).
RESULTS
From the 80 patients cohort; 72 (90%) patients tested anti-HEV IgG negative, anti-HEV IgM negative and HEV RNA negative; 4 (5%) patients tested anti-HEV IgG positive, anti-HEV IgM negative and HEV RNA negative; 3 (3.75%) patients tested anti-HEV IgG positive, ant-HEV IgM positive and HEV RNA positive; 1 (1.25%) patient tested anti-HEV IgG positive, anti-HEV IgM positive and HEV RNA negative (Table 3). No patient diagnosed with hepatitis B, hepatitis C, autoimmune hepatitis, post liver transplant graft non-function, fatty liver of pregnancy, ischaemic hepatitis, malignancy or acute porphyria tested positive for hepatitis E (Table 1). The 4 patients with corresponding anti-HEV IgM positive results, suggestive of active infection at time of testing, are described in further detail below.
Table 3.
Hepatitis E virus immunoglobulin M positive patients
| Patient ID | Gender | Age |
Liver function tests (normal range) |
HEV |
Travel history | Initial/ | Outcome | ||||||||
| ALT | Billirubin | ALP | Gamma GTP | Albumin | PT | IgG | IgM | RNA | Genotype | retrospective | |||||
| (10-50 IU/mL) | (< 17 μmol/L) | (40-125 IU/L) | (5-35 IU/mL) | (30-50 g/L) | (8-12 s) | (IU/mL) | (IU/mL) | diagnosis | |||||||
| 1 | Female | 58 | 3648 | 92 | 540 | 480 | 35 | 16 | 48.4 | + | 6.4 × 104 | 3 | Spain, Cornwall | DILI/hepatitis E | Survived |
| 2 | Female | 67 | 98 | 516 | 256 | Icteric1 | 19 | 14 | 36.49 | + | 1.4 × 103 | 3 | Spain | Alcohol, T2Diabetes, obesity, CLD/hepatitis E | Died |
| 3 | Male | 27 | 5288 | 140 | 186 | 368 | 27 | 35 | 24.7 | + | - | - | London | POD/hepatitis E | Survived |
| 4 | Male | 27 | 4044 | 269 | 253 | Icteric1 | 38 | 25 | 42.05 | + | 1.9 × 104 | 1 | India | Hepatitis E | Survived |
GTP could not be calculated due to high serum bilirubin levels. Values obtained from serum samples taken on admission to SLTU. ALT: Alanine aminotransferase; ALP: Alkaline phosphatase; GTP: Glutamyl transpeptidase; PT: Prothrombin time; HEV: Hepatitis E virus; Ig: Immunoglobulin; RNA: Ribonucleic acid; DILI: Drug induced liver injury; CLD: Chronic liver disease; POD: Paracetamol overdose.
Patient 1
A 58-year-old female presented with a 24 h history of jaundice and itch. She complained of generalised malaise/fatigue for 1 wk and dark tea-coloured urine for 3 d, but no abdominal pain, nausea or vomiting. The patient had travelled to Ibiza (Spain) 1 mo and Cornwall (England) 2 wk previously. After returning with a dry cough, she visited her General Practitioner, who prescribed a short course of clarithromycin. The patient had also recently begun taking simvastatin and diclofenac and was a regular user of aspirin and nifedipine. The patient had no history of liver problems and only light alcohol consumption (< 48 g/wk, maximum recommended limit for females = 112 g/wk). Liver function tests showed highly elevated transaminases (Table 3). Tests for hepatitis A, B, C and autoantibodies were negative, alpha-1-antitrypsin and ceruloplasmin were normal, serum ferritin 1871 ug/L (normal range 14-150), iron 15 μmol/L (normal range 10-28), transferrin 2.1 g/L (normal range 2-4), transferrin saturation 27%. An ultrasound scan showed no focal abnormality, contracted gall bladder, no biliary dilatation, normal kidneys/spleen and no free intra-abdominal fluid.
After withdrawal from all her medication, the patient’s liver function tests improved. The patients liver dysfunction was therefore attributed to drug induced liver injury (DILI). However, in retrospect a diagnosis of acute hepatitis E was made, as she was anti-HEV IgM and IgG positive, and her serum contained a high titre of HEV RNA (Table 3). Sequencing of the patient’s viral RNA showed it to be of genotype 3 (Figure 1).
Figure 1.
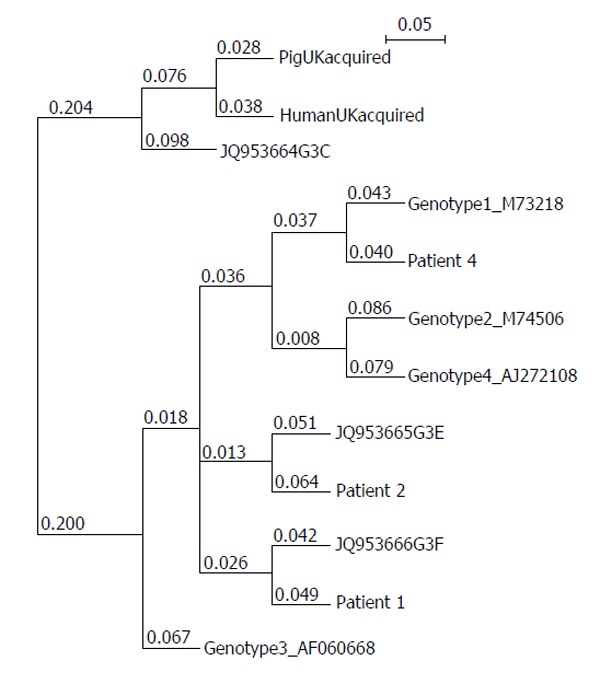
Phylogenetic relationship between the 4 hepatitis E virus genotype reference sequences and those isolated from a United Kingdom swine (AF503512), a United Kingdom patient with locally acquired hepatitis E virus (AY362357), genotype 3 subtypes described in[19] and the patients discussed in this paper. Sequences were assembled using ClustalW and the phylogenetic tree expressed in the Newick format using NJ plot[20]. The 121 bp sequences correspond to nucleotides 6332-6476 of hepatitis E virus genotype 3 reference strain AF060668.
Patient 2
A 67-year-old female presented to the referring hospital with acute hepatitis after returning from Spain 4 wk earlier. She had significant comorbidity; non-insulin dependent diabetes, hypertension, chronic kidney disease and alcohol excess (224-258 g/wk). Because of developing hepatic encephalopathy, increasing fluid overload and renal injury the patient was transferred to SLTU. The patient underwent a transjugular liver biopsy to clarify the diagnosis. The biopsy showed cirrhosis with sparse steatohepatitis and a low grade cholestatic hepatitis (Figure 2). She developed sepsis complicated by multi-organ failure and died despite supportive care, including dialysis and norepinepherine. This patient was anti-HEV IgM and IgG positive. Retrospective RNA screening and sequencing showed this patient demonstrated HEV genotype 3 in her stored blood sample (Figure 1 and Table 3).
Figure 2.
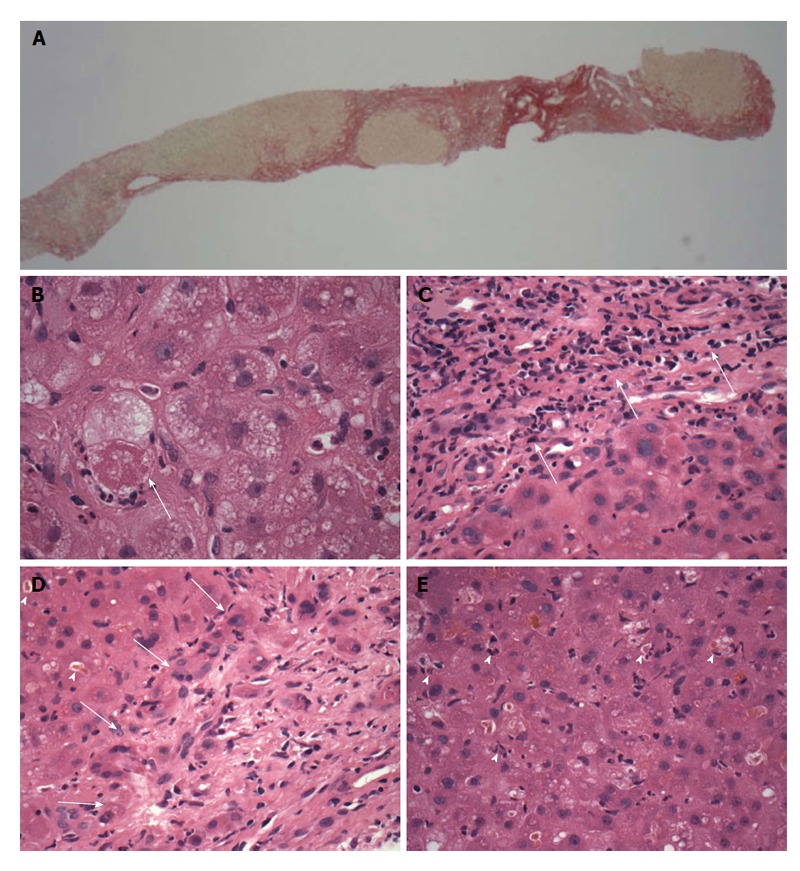
Patient 2, transjugular needle biopsy. A: Low magnification view of part of the biopsy, showing red-stained nodular fibrosis indicating cirrhosis (x 20 original magnification, picrosirius red stain); B: Ballooned hepatocyte (arrow) containing a Mallory-Denk body and with surrounding neutrophils (satellitosis), features of steatohepatitis. (× 600 original magnification, H and E stain). Small clusters of these cells were present in the biopsy, with sparse small droplet macro-steatosis; C: Low grade hepatitic infiltrate (arrows) of lymphocytes with occasional plasma cells in the portal area (× 400 original magnification, H and E stain); D: Prominent cholangiolitis (periportal ductules with oedema and neutrophils) (region indicated by arrows), with adjacent liver parenchyma showing canalicular cholestasis (arrowheads); E: Lobule showing mild disarray with cholestasis, increased lymphocytes and Kupffer cells within sinusoids and scattered apoptotic/necrotic cells (arrowheads).
Patient 3
A 27-year-old male Polish immigrant living in London travelled to Scotland to stay with a relative. Without suicidal intent, and in conjunction with excessive alcohol, he ingested 8 g of liquid paracetamol. He was transferred to SLTU because of deranged liver function tests (Table 3) and confusion. He developed hepatic encephalopathy and acute kidney injury with oliguria and peak creatinine 600 μmol/L which resolved spontaneously, without renal replacement therapy. Twelve days after admission he was discharged to the referring hospital with the following blood tests (normal range indicated in brackets); prothrombin time 35 s (8-12 s), bilirubin 343 μmol/L (< 17 μmol/L), alanine aminotransferase 97 IU/L (10-50 IU/L), alkaline phosphatase 160 IU/L (40-150 IU/L), gamma glutamyl transpeptidase 190 IU/L (5-35 IU/L), Albumin 19 g/L (30-50 g/L). In retrospect, this patient tested positive for anti-HEV IgM and IgG antibodies but no viral RNA could be detected in his serum.
Patient 4
A 27-year-old male experienced a short self-limiting episode of nausea and diarrhoea just before returning to Scotland from working at a sanitation project in Northern India. He rapidly became jaundiced and fatigued. He was febrile, had no stigmata of chronic liver disease, but was deeply jaundiced with a palpable non-tender liver. Upper abdominal ultrasound was normal and other liver diseases excluded by serology, biochemistry and immunology. A transjugular liver biopsy was performed, revealing a severe acute lobular hepatitis (Figure 3). Due to the patient’s travel history he was contemporaneously tested for HEV, and was IgM, IgG and PCR positive. Sequencing performed in retrospect showed the patient to be infected with HEV genotype 1 (Figure 1).
Figure 3.
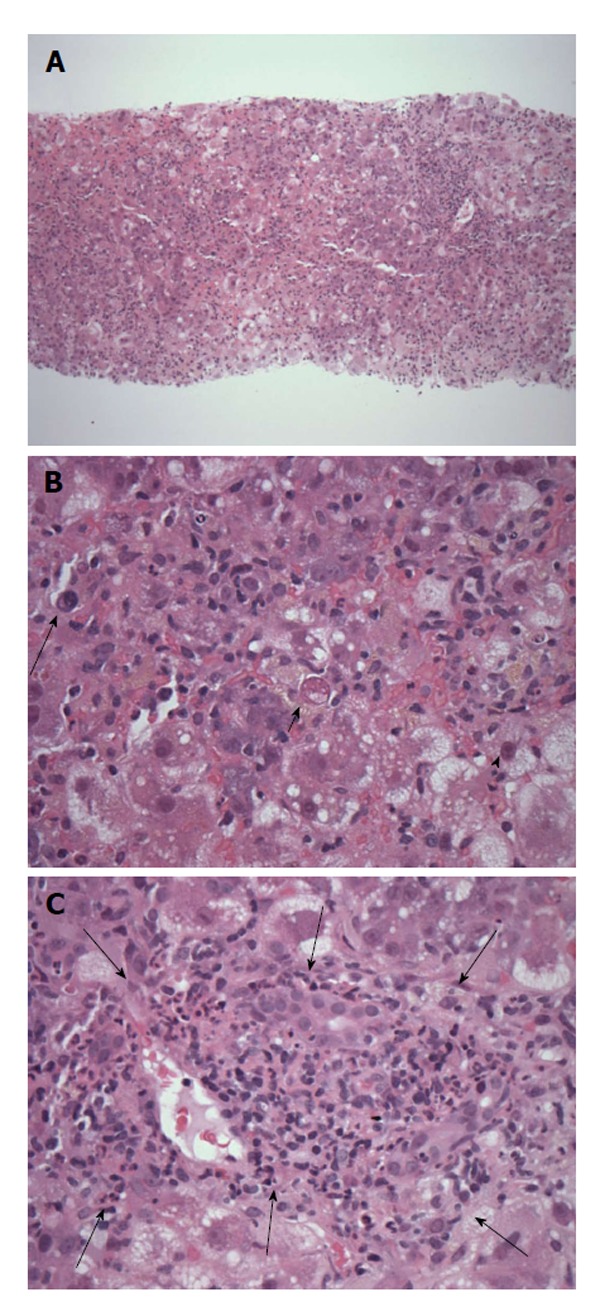
Patient 4, transjugular needle biopsy showing severe acute lobular hepatitis. A: Low magnification view showing the diffuse nature of the liver inflammation and injury (original magnification × 40, H and E); B: Severely inflamed lobule with numerous infiltrating inflammatory cells, including occasional plasma cells (long arrow), hepatocyte cell death (short arrow) and ballooning injury (arrowhead) (original magnification × 400, H and E); C: Shows an inflamed portal tract (delineated by arrows) expanded within by mononuclear inflammatory cells without bile duct injury and with only rare plasma cells or eosinophils. There is neutrophil cholangiolitis around the portal tract (just within the arrows) but no prominent interface hepatitis (original magnification × 200, H and E).
DISCUSSION
In developed countries there have been few previous studies of HEV in patients with acute liver injury severe enough to warrant assessment and treatment at a liver transplant unit[13]. The current study shows that in four of 80 (5%) of patients with acute severe liver injury the cause was hepatitis E, thus making HEV the commonest cause of viral hepatitis in this cohort. Three of the four cases were only diagnosed on retrospective testing and were initially erroneously ascribed to drug-induced liver injury (n = 2) and decompensated chronic liver disease, with the cause of the decompensation uncertain (n = 1). These findings suggest that in patients with acute severe liver injury HEV testing should be part of the initial diagnostic investigation algorithm, irrespective of suspected initial diagnosis, age or travel history.
In the case of patient 1, we initially misdiagnosed the case as DILI because, at the time, we did not consider hepatitis E as a diagnostic possibility. A study from England showed that 6/47 (13%) of patients with criterion-referenced drug-induced liver injury had been misdiagnosed, as they had locally-acquired hepatitis E infection[12]. A similar study from the United States showed that 9/318 (3%) had been similarly misdiagnosed[13]. More recently, Chen et al[14] described another case of hepatitis E which had been erroneously diagnosed as “DILI”. An accurate diagnosis of drug-induced liver injury depends on excluding of all other possible cases of hepatocellular injury[21]. Patient 1 case illustrates the important clinical point that the diagnosis of drug-induced liver injury is not secure without first excluding hepatitis E, irrespective of travel history, particularly in patients with highly elevated transaminases.
Patient 2, although presenting with severe acute liver injury, had previously undiagnosed cirrhosis, likely due to a combination of alcoholic and fatty liver disease, and died from multi-organ failure precipitated by hepatitis E infection. Studies from Europe and Southeast Asia show, that hepatitis E infection in patients with underlying chronic liver disease, have a poor prognosis, with a 12-mo mortality rate from subacute liver failure of up to 70%[22,23]. The diagnosis of acute hepatitis E infection in such patients is easily overlooked, and may commonly be ascribed to other causes such as alcoholic hepatitis[24]. Patient 2 illustrates this diagnostic difficulty, as there were no specific clinical or laboratory clues which prompted consideration of hepatitis E as a diagnostic possibility, and the liver biopsy appearances could easily have been ascribed simply to decompensated alcoholic cirrhosis in a previously undiagnosed patient. Often the only clue in such hepatitis E cases is the elevation of transaminases at presentation[25]. Within a week, the alanine aminotransferase declines to the range seen in alcoholic hepatitis[24,25], as was the case in patient 2 (98I U/mL) (Table 3). Despite the difficulties in identifying cases, it is important to establish an early diagnosis of hepatitis E infection in patients with underlying chronic liver disease, as the prognosis may be improved by early anti-viral therapy with ribavirin[26,27]. Indeed, this case highlights the poor prognosis in older patients with underlying liver disease and acute hepatitis E infection.
In the case of patient 3 we were unable to detect HEV RNA, despite the patient being anti-HEV IgM positive. However, the absence of detectable HEV RNA does not exclude recent infection as peak viremia occurs during incubation and the window of detectable RNA is narrow (approximately 2-3 wk)[28,29]. Also, studies show patients with a history of alcohol abuse who are exposed to HEV are significantly more likely to develop clinically apparent hepatitis[30], as this patient did. Interestingly, this patient was originally considered to have paracetamol induced liver necrosis, developing significant coagulopathy and an acute kidney injury as is commonly observed in such cases. Although the stated dose of paracetamol was relatively low and more recent studies have reported the validity of patient history in the context of hepatotoxicity, the reported dose of paracetamol is not related to eventual outcome[31,32]. It is possible that HEV, like other viral infections, can augment the hepatotoxicity of paracetamol[9-11]. However, coexisting acute hepatitis E in patients with paracetamol hepatotoxicity in this cohort was an uncommon finding (1.6%) and it is not possible to make comparisons with other cases of paracetamol hepatotoxicity based on a single case.
Of the four cases of hepatitis E identified in this study, only 1 patient (patient 4) had travelled to a region considered hyperendemic for HEV (India). Phylogenetic analysis revealed this patient to be infected with HEV genotype 1 (Figure 1 and Table 2), supporting the hypothesis that this was an imported case of HEV infection. This was the only case that was diagnosed contemporaneously, as HEV testing was prompted by the travel history. The remaining 3 patients had travelled outside of Scotland, although only to regions previously considered non-endemic for HEV (England and Spain). Phylogenetic analysis of patient’s 1 and 2 samples revealed these patients were infected with HEV genotype 3, the most prevalent genotype in cases of autochthonous hepatitis E infection in developed countries[2]. It is not possible to determine for certain whether these patients contracted their HEV infection in Scotland or the other “non-endemic” regions they visited prior to onset of symptoms. However, given the absence of cases of hepatitis E in patients in this series who had not recently travelled outside of Scotland, it suggests that locally acquired hepatitis E infection in Scotland is uncommon. This notion is supported by a low IgG seroprevalence rate of 4.5% in blood donors from southeast Scotland and, at least compared to other European countries, a modest rate of asymptomatic viraemia at the time of donation (1 in 14500)[33].
Patient 4, aligned with Genotype 1 to confirm the acquisition of HepE during travel. However, HEV3 infection in developed countries is commonly associated with the ingestion of contaminated food products such as undercooked pork, game meat and molluscs cultivated in contaminated water, as well as occupational exposure to pigs or their effluent[2]. Patient 1 and patient 2 had genotypes with homology to genotype 3f and 3e respectively. These genotypes were isolated from European swine, however, pre-infection exposure to defined environmental and dietary risk factors is unknown and so we cannot narrow their possible source of infection further. Infection via blood transfusion has also been documented[2] and it was confirmed that none of the patients had recently undergone a blood transfusion.
The liver biopsy findings deserve comment given the differing genotypes. There are only limited previously published data on the liver biopsy appearances of endemic and locally acquired acute hepatitis E[23,34-36], as such cases usually have a self-limiting illness and so a liver biopsy is not commonly clinically indicated. There is a lobular hepatitis of varying severity between patients 2 and 4, from mild lobular disarray with Kupffer cell hypertrophy and scattered individually necrotic hepatocytes with adjacent neutrophils or lymphocytes, through to severe lesions with confluent necrosis and collapse. A cholestatic element is often present within lobules and portal tracts, including canalicular cholestasis, mild bile duct inflammation and typically quite prominent neutrophilic cholangiolitis around the portal tracts as seen in patient 2 (Figure 2D and E). Similar pathology has been reported by Malcolm et al[35] in their locally acquired cases and by others[36]. These features can easily be mis-attributed to a drug-related cholestatic hepatitis. When occurring in patients with chronic liver disease such as alcoholic cirrhosis the viral effects may be overshadowed by or mis-attributed to steatohepatitis-related changes or sepsis-related decompensation. A plasma cell-rich portal, interface and lobular hepatitis such as characterises flares of autoimmune hepatitis is not normally seen in acute hepatitis E, although loose lymphoid aggregates in portal tracts have been described in occasional patients, which might misdirect when there is pre-existing liver fibrosis. In patient 4, the absence of a prominent interface hepatitis and neutrophil cholangiolitis was comparable to a recent study on acute endemic HEV[34]. Whether autochthonous and endemic hepatitis E differ qualitatively in histological characteristics, remains uncertain given the small number of case comparisons including this study[34,35,37]. The variable underlying severity of the hepatitis and other selection factors prompting biopsy could skew the comparison and more data is required[38].
In summary, in 4 of 80 (5%) of patients with acute liver injury severe enough to warrant assessment and treatment at the Scottish Liver Transplant Unit, the cause was hepatitis E. Only one of these patients had a history of travel to an area traditionally considered hyperendemic for HEV. This is in line with the sero-prevalence in the Scottish population and higher than the rate of viraemia[31]. This study shows that clinicians should have a low threshold for considering hepatitis E as a possible diagnosis in any patient with severe acute liver injury. This should include those with possible paracetamol hepatotoxicity, irrespective of their age or travel history.
COMMENTS
Background
Hepatitis E virus (HEV), the etiological agent responsible for hepatitis E infection, is now recognised as an emerging zoonotic disease in industrialized countries. HEV genotypes 3 and 4 are responsible for sporadic cases of autochthonous hepatitis E infection in countries such as the United Kingdom, United States, France, Italy and Japan. HEV can cause a mild, self-limiting infection but it can also cause more serious health problems such as cirrhosis of the liver and fulminant hepatitis. The ability of HEV genotype 3 and 4 strains to cross the species barrier has been documented and there is a growing body of evidence that HEV can be transmitted to humans via the consumption of infected or contaminated food products.
Research frontiers
In developed countries, there have been very few previous studies of HEV genotype 3 in patients with acute liver injury severe enough to warrant assessment and treatment at a liver transplant unit.
Innovations and breakthroughs
Recent reports have highlighted the importance of HEV diagnosis in a number of clinical situations. In this study, we confirm the need for increased diagnostic testing in patients presenting with drug induced liver injury. In addition, liver pathogenesis clearly differs with the genotype causing the infection. Finally, routes of infection need further clarification.
Applications
Misdiagnosis of hepatitis E infection in drug induced liver injury has been noted in patients previously in South East England (13%) and the United States (3%). However, hepatitis E virus is still not given precedence when diagnosing these individuals. In the authors’ study, 5% of individuals tested were misdiagnosed and viraemic. It is an important clinical point that the diagnosis of drug induced liver injury is not secure without first excluding hepatitis E, irrespective of travel history, particularly in patients with elevated transaminases. This data contributes to the increasing need to screen patients for the presence of the HEV.
Terminology
HEV is a member of the Hepeviridae and Genotype 3 recognised as a zoonotic infection. The role of HEV in severe acute liver disease has yet to be defined.
Peer review
This is a well written manuscript, dealing with the prevalence of hepatitis E among a series of patients subjected to liver transplantation, in whom the etiology of liver failure was masked by coexisting cirrhosis and/or drug overdose. Authors correctly stress the importance of excluding HEV infection in Western countries, irrespective of the travel story.
Footnotes
Supported by Chief Scientist Office Scotland (under project ETM/32)
P- Reviewers: Gatselis NK, Gonzalez-Reimers E, Komatsu H S- Editor: Ji FF L- Editor: A E- Editor: Liu SQ
References
- 1.Investigation of hepatitis e outbreak among refugees-upper nile, South Sudan, 2012-2013. MMWR. 2013;62:581–586. [PMC free article] [PubMed] [Google Scholar]
- 2.Scobie L, Dalton HR. Hepatitis E: source and route of infection, clinical manifestations and new developments. J Viral Hepat. 2013;20:1–11. doi: 10.1111/jvh.12024. [DOI] [PubMed] [Google Scholar]
- 3.Meng XJ. From barnyard to food table: the omnipresence of hepatitis E virus and risk for zoonotic infection and food safety. Virus Res. 2011;161:23–30. doi: 10.1016/j.virusres.2011.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dalton HR, Bendall RP, Rashid M, Ellis V, Ali R, Ramnarace R, Stableforth W, Headdon W, Abbott R, McLaughlin C, et al. Host risk factors and autochthonous hepatitis E infection. Eur J Gastroenterol Hepatol. 2011;23:1200–1205. doi: 10.1097/MEG.0b013e32834ca4da. [DOI] [PubMed] [Google Scholar]
- 5.Ijaz S, Vyse AJ, Morgan D, Pebody RG, Tedder RS, Brown D. Indigenous hepatitis E virus infection in England: more common than it seems. J Clin Virol. 2009;44:272–276. doi: 10.1016/j.jcv.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 6.Hoofnagle JH, Nelson KE, Purcell RH. Hepatitis E. N Engl J Med. 2012;367:1237–1244. doi: 10.1056/NEJMra1204512. [DOI] [PubMed] [Google Scholar]
- 7.Kuniholm MH, Purcell RH, McQuillan GM, Engle RE, Wasley A, Nelson KE. Epidemiology of hepatitis E virus in the United States: results from the Third National Health and Nutrition Examination Survey, 1988-1994. J Infect Dis. 2009;200:48–56. doi: 10.1086/599319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Craig DG, Lee A, Hayes PC, Simpson KJ. Review article: the current management of acute liver failure. Aliment Pharmacol Ther. 2010;31:345–358. doi: 10.1111/j.1365-2036.2009.04175.x. [DOI] [PubMed] [Google Scholar]
- 9.Prandota J. Important role of prodromal viral infections responsible for inhibition of xenobiotic metabolizing enzymes in the pathomechanism of idiopathic Reye’s syndrome, Stevens-Johnson syndrome, autoimmune hepatitis, and hepatotoxicity of the therapeutic doses of acetaminophen used in genetically predisposed persons. Am J Ther. 2002;9:149–156. doi: 10.1097/00045391-200203000-00009. [DOI] [PubMed] [Google Scholar]
- 10.Nguyen GC, Sam J, Thuluvath PJ. Hepatitis C is a predictor of acute liver injury among hospitalizations for acetaminophen overdose in the United States: a nationwide analysis. Hepatology. 2008;48:1336–1341. doi: 10.1002/hep.22536. [DOI] [PubMed] [Google Scholar]
- 11.Rezende G, Roque-Afonso AM, Samuel D, Gigou M, Nicand E, Ferre V, Dussaix E, Bismuth H, Féray C. Viral and clinical factors associated with the fulminant course of hepatitis A infection. Hepatology. 2003;38:613–618. doi: 10.1053/jhep.2003.50366. [DOI] [PubMed] [Google Scholar]
- 12.Dalton HR, Fellows HJ, Stableforth W, Joseph M, Thurairajah PH, Warshow U, Hazeldine S, Remnarace R, Ijaz S, Hussaini SH, et al. The role of hepatitis E virus testing in drug-induced liver injury. Aliment Pharmacol Ther. 2007;26:1429–1435. doi: 10.1111/j.1365-2036.2007.03504.x. [DOI] [PubMed] [Google Scholar]
- 13.Davern TJ, Chalasani N, Fontana RJ, Hayashi PH, Protiva P, Kleiner DE, Engle RE, Nguyen H, Emerson SU, Purcell RH, et al. Acute hepatitis E infection accounts for some cases of suspected drug-induced liver injury. Gastroenterology. 2011;141:1665–1672.e1-e9. doi: 10.1053/j.gastro.2011.07.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen EY, Baum K, Collins W, Löve A, Merz M, Olafsson S, Björnsson ES, Lee WM. Hepatitis E masquerading as drug-induced liver injury. Hepatology. 2012;56:2420–2423. doi: 10.1002/hep.26158. [DOI] [PubMed] [Google Scholar]
- 15.Ajmera V, Xia G, Vaughan G, Forbi JC, Ganova-Raeva LM, Khudyakov Y, Opio CK, Taylor R, Restrepo R, Munoz S, et al. What factors determine the severity of hepatitis A-related acute liver failure. J Viral Hepat. 2011;18:e167–e174. doi: 10.1111/j.1365-2893.2010.01410.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bendall R, Ellis V, Ijaz S, Thurairajah P, Dalton HR. Serological response to hepatitis E virus genotype 3 infection: IgG quantitation, avidity, and IgM response. J Med Virol. 2008;80:95–101. doi: 10.1002/jmv.21033. [DOI] [PubMed] [Google Scholar]
- 17.Jothikumar N, Cromeans TL, Robertson BH, Meng XJ, Hill VR. A broadly reactive one-step real-time RT-PCR assay for rapid and sensitive detection of hepatitis E virus. J Virol Methods. 2006;131:65–71. doi: 10.1016/j.jviromet.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 18.Erker JC, Desai SM, Mushahwar IK. Rapid detection of Hepatitis E virus RNA by reverse transcription-polymerase chain reaction using universal oligonucleotide primers. J Virol Methods. 1999;81:109–113. doi: 10.1016/s0166-0934(99)00052-x. [DOI] [PubMed] [Google Scholar]
- 19.Bouquet J, Cherel P, Pavio N. Genetic characterization and codon usage bias of full-length Hepatitis E virus sequences shed new lights on genotypic distribution, host restriction and genome evolution. Infect Genet Evol. 2012;12:1842–1853. doi: 10.1016/j.meegid.2012.07.021. [DOI] [PubMed] [Google Scholar]
- 20.Perriere G, Gouy M. WWW-query: an on-line retrieval system for biological sequence banks. Biochimie. 1996;78:364–369. doi: 10.1016/0300-9084(96)84768-7. [DOI] [PubMed] [Google Scholar]
- 21.Benichou C. Criteria of drug-induced liver disorders. Report of an international consensus meeting. J Hepatol. 1990;11:272–276. doi: 10.1016/0168-8278(90)90124-a. [DOI] [PubMed] [Google Scholar]
- 22.Dalton HR, Hazeldine S, Banks M, Ijaz S, Bendall R. Locally acquired hepatitis E in chronic liver disease. Lancet. 2007;369:1260. doi: 10.1016/S0140-6736(07)60595-9. [DOI] [PubMed] [Google Scholar]
- 23.Péron JM, Bureau C, Poirson H, Mansuy JM, Alric L, Selves J, Dupuis E, Izopet J, Vinel JP. Fulminant liver failure from acute autochthonous hepatitis E in France: description of seven patients with acute hepatitis E and encephalopathy. J Viral Hepat. 2007;14:298–303. doi: 10.1111/j.1365-2893.2007.00858.x. [DOI] [PubMed] [Google Scholar]
- 24.Dalton HR. Hepatitis: hepatitis E and decompensated chronic liver disease. Nat Rev Gastroenterol Hepatol. 2012;9:430–432. doi: 10.1038/nrgastro.2012.121. [DOI] [PubMed] [Google Scholar]
- 25.Lockwood GL, Fernandez-Barredo S, Bendall R, Banks M, Ijaz S, Dalton HR. Hepatitis E autochthonous infection in chronic liver disease. Eur J Gastroenterol Hepatol. 2008;20:800–803. doi: 10.1097/MEG.0b013e3282f1cbff. [DOI] [PubMed] [Google Scholar]
- 26.Péron JM, Dalton H, Izopet J, Kamar N. Acute autochthonous hepatitis E in western patients with underlying chronic liver disease: a role for ribavirin. J Hepatol. 2011;54:1323–134; author reply 1323-1334;. doi: 10.1016/j.jhep.2011.01.009. [DOI] [PubMed] [Google Scholar]
- 27.Goyal R, Kumar A, Panda SK, Paul SB, Acharya SK. Ribavirin therapy for hepatitis E virus-induced acute on chronic liver failure: a preliminary report. Antivir Ther. 2012;17:1091–1096. doi: 10.3851/IMP2317. [DOI] [PubMed] [Google Scholar]
- 28.Gupta P, Jagya N, Pabhu SB, Durgapal H, Acharya SK, Panda SK. Immunohistochemistry for the diagnosis of hepatitis E virus infection. J Viral Hepat. 2012;19:e177–e183. doi: 10.1111/j.1365-2893.2011.01498.x. [DOI] [PubMed] [Google Scholar]
- 29.Aggarwal R. Hepatitis E: clinical presentation in disease-endemic areas and diagnosis. Semin Liver Dis. 2013;33:30–40. doi: 10.1055/s-0033-1338112. [DOI] [PubMed] [Google Scholar]
- 30.Dalton HR, Bendall RP, Pritchard C, Henley W, Melzer D. National mortality rates from chronic liver disease and consumption of alcohol and pig meat. Epidemiol Infect. 2010;138:174–182. doi: 10.1017/S0950268809990306. [DOI] [PubMed] [Google Scholar]
- 31.Gregory B, Larson AM, Reisch J, Lee WM. Acetaminophen dose does not predict outcome in acetaminophen-induced acute liver failure. J Investig Med. 2010;58:707–710. doi: 10.231/JIM.0b013e3181db8764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Waring WS, Robinson OD, Stephen AF, Dow MA, Pettie JM. Does the patient history predict hepatotoxicity after acute paracetamol overdose. QJM. 2008;101:121–125. doi: 10.1093/qjmed/hcm139. [DOI] [PubMed] [Google Scholar]
- 33.Cleland A, Smith L, Crossan C, Blatchford O, Dalton HR, Scobie L, Petrik J. Hepatitis E virus in Scottish blood donors. Vox Sang. 2013;105:283–289. doi: 10.1111/vox.12056. [DOI] [PubMed] [Google Scholar]
- 34.Agrawal V, Goel A, Rawat A, Naik S, Aggarwal R. Histological and immunohistochemical features in fatal acute fulminant hepatitis E. Indian J Pathol Microbiol. 2012;55:22–27. doi: 10.4103/0377-4929.94849. [DOI] [PubMed] [Google Scholar]
- 35.Malcolm P, Dalton H, Hussaini HS, Mathew J. The histology of acute autochthonous hepatitis E virus infection. Histopathology. 2007;51:190–194. doi: 10.1111/j.1365-2559.2007.02756.x. [DOI] [PubMed] [Google Scholar]
- 36.Drebber U, Odenthal M, Aberle SW, Winkel N, Wedemeyer I, Hemberger J. Holzmann H and Dienes H-P (2013) Hepatitis E in liver biopsies from patients with acute hepatitis of clinically unexplained origin. Front. Physiol. 2013;4:351. doi: 10.3389/fphys.2013.00351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Peron JM, Danjoux M, Kamar N, Missoury R, Poirson H, Vinel JP, Mansuy JM, Bureau C, Izopet J, Brousset P, Selves J. Liver histology in patients with sporadic acute hepatitis E: a study of 11 patients from South-West France. Virchows Arch. 2007;450:405–410. doi: 10.1007/s00428-007-0382-y. [DOI] [PubMed] [Google Scholar]
- 38.Aggarwal R. Diagnosis of hepatitis E. Nat Rev Gastroenterol Hepatol. 2012;10:24–33. doi: 10.1038/nrgastro.2012.187. [DOI] [PubMed] [Google Scholar]


