Abstract
Erdheim-Chester disease (ECD) is a rare inflammatory syndrome in which systemic infiltration of non-Langerhans cell histiocytes occurs in different sites. Both the etiology and pathophysiology of ECD are unknown, but CD68 positive CD 1a/S100 negative cells are characteristic. The presentation of ECD differs according to the involved organs. This case report describes a patient with ECD and the gastrointestinal manifestations and unique endoscopic appearance as seen in gastroscopy and colonoscopy with histological proof of histiocyte infiltration of the lamina propria. The clinical and endoscopic findings of this unique case, to our knowledge, were never described before, so were the features of the gastrointestinal involvement in this disease.
Keywords: Erdheim chester, Histiocytes, Lamina propria, Colon, Stomach
Core tip: This case report describes a patient with Erdheim-Chester disease with gastrointestinal manifestations and unique endoscopic appearance as seen both in gastroscopy and colonoscopy with histological proof of histiocyte infiltration of the lamina propria. The clinical and endoscopic findings of this unique case, to the best of our knowledge, were never described before, so were the features of the gastrointestinal involvement in this disease.
INTRODUCTION
Erdheim-Chester disease (ECD) is a rare inflammatory disease in which systemic infiltration of non-Langerhans cell histiocytes occurs in different sites. Both the etiology and the pathophysiology of ECD are unknown, but CD68 positive CD1a/ S100 negative cells are characteristic[1]. The presentation of ECD differs according to the involved organs. In most cases, lesions of long bones are present, but CNS[2-4], heart[5] and lung[6,7] manifestations in this disease were previously described as well. Gastrointestinal involvement in ECD seems to be extremely rare[8], unlike other histiocytosis[9], and to the best of our knowledge, there are only three case reports published describing hepatic billiary and pancreatic manifestations[8,10,11] of this disease.
Here we describe a case of a 36-year-old female patient who presented to the ER with prolonged diarrhea polyuria, fatigue and weight loss.
CASE REPORT
A 36-year-old female, previously healthy with the exception of an anxiety disorder, and treated with Fluoxetine, was admitted to hospital due to diarrhea, weight loss, nausea and vomiting, prolonged fever and weakness for the last 3 mo. She reported significant weight loss of more than 10 kg in the last year with increased thirst and polyuria. The patient denied any cardiac, respiratory or bone pain but did complain of joint pain with no evidence of arthritis. On admission, the patient’s fever was 38.3, but other vital signs were normal. She had body mass index of 19 kg/m2. Physical examination showed notable cachexia with palpable groin lymph nodes.
The laboratory test showed anemia with hemoglobin level of 9. Her hemoglobin was within a normal range over the past 6 mo. White cell count was normal with no deviation in differentiation. The blood chemistry was normal besides mild elevation of transaminases. Alanine aminotransferase was 68 IU/L, and aspartate aminotransferase was 164 IU/L; both were documented at a normal range two mo before. Serum lactate dehydrogenase was 2200 U/L (normal range, 230-480), serum iron was 21 μg/dL (normal range, 40-145) with transferrin level of 148 (normal range, 200-360). Albumin was 3.3 g/dL (normal range 3.5-5.2) and C reactive protein was increased to 3.43 mg% (normal range, up to 0.5), antinuclear Ab, rheumatoid factor, DNA Ab celiac screen and ANCA were negative as well as serology for viral hepatitis.
Computerized tomography of chest, abdomen and pelvis revealed mildly enlarged axillary and retroperitoneal lymph nodes, mild splenomegaly, few small hypodense hepatic lesions and sclerotic lesions in both sternum and iliac crest.
A month prior to the current admission, she was evaluated at another medical center where bone marrow was aspirated, resulting in suspicion of histiocytosis. An auxiliary lymph node was surgically obtained, and showed almost complete replacement of lymph node by a monotonous population of CD68 positive , CD1a and S-100 protein negative histiocytes. PAS and polymerase chain reaction for different mycobacteria were negative. Bone marrow showed hypercellularity with the presence of non-necrotizing epithelial granulomas. The pathologist conclusion was an adult form of ECD.
Due to the weight loss, prolonged diarrhea and recurrent vomiting, and in light of the pathologist conclusion, an endoscopic evaluation of the upper gastrointestinal tract was performed by gastroscopy and colonic evaluation by colonoscopy with intubation of the ileocecal valve and examination of the terminal ileum.
The gastroscopy showed a cobblestone-like raised nodular gastritis of the entire stomach (Figure 1). Pylorus and duodenum were normal. Gastric biopsy showed chronic follicular inflammation associated with patchy infiltration of CD68 positive foamy histiocytes (Figure 2). Colonoscopy revealed numerous small round hyper-pigmented lesions with decreased vascularity in the surrounding mucosa extending from the rectum to the cecum (Figure 3).
Figure 1.
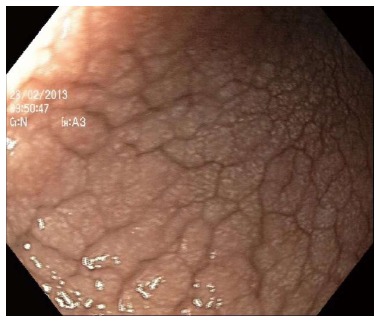
Endoscopic appearance of the stomach body.
Figure 2.
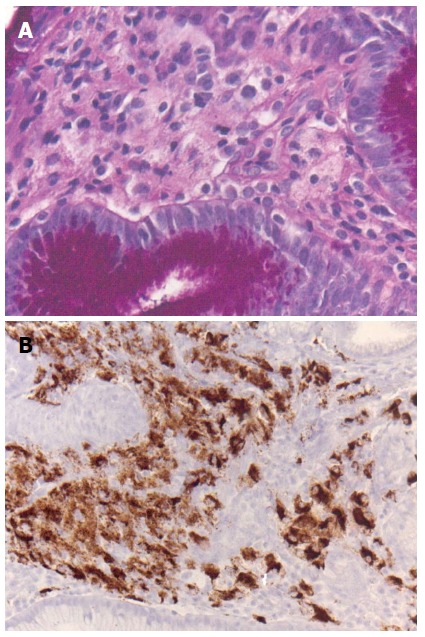
Histological findings in gastric biopsy. A: Lamina propria infiltrated by foamy histiocytes negative for PAS (PAS stain, × 200); B: Foamy cells stained positive for CD 68 (CD68 stain, × 100).
Figure 3.
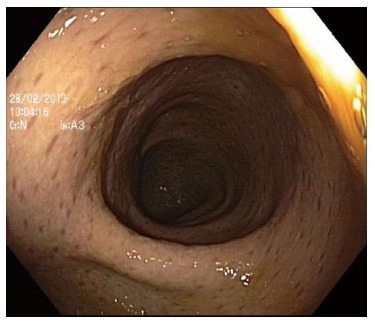
Colonoscopy showing numerous small round hyper-pigmented lesions.
The terminal ileum was normal as well. Biopsies subsequently taken showed colonic mucosa with preserved crypt architecture and patchy infiltration of foamy histiocytes. PAS and Giemsa stains were negative for micro-organisms (Figure 4). The biopsies taken from the terminal ileum were normal. After the diagnosis of ECD was made, the patient was treated with interferon which is the current standard of treatment[12]. The patient began a course of combined vinblastine and prednisone and achieved partial response. Unfortunately, no further follow-up is available.
Figure 4.
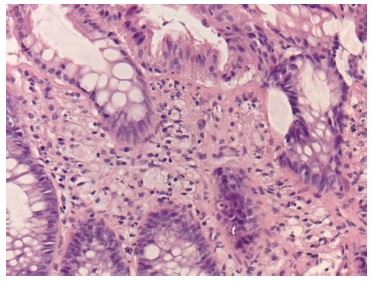
Histology of colonic mucosa showing histiocytic infiltration of lamina propria (HE stain, × 100).
DISCUSSION
ECD is a systemic type of non-Langerhans cell histiocytosis. It was first described by Jacob Erdheim and William Chester in 1930. There were approximately 400 cases reported in literature with extremely rare gastrointestinal involvement. There has been no endoscopic description of gastrointestinal features so far.
Here, for the first time, we discuss the endoscopic findings revealed by both gastroscopy and colonoscopy in a patient with gastrointestinal involvement of ECD.
Although extremely rare, this case suggests that physicians should always keep in mind the diagnosis of infiltrating systemic disease such as ECD when dealing with prolonged unexplained gastrointestinal complains along with systemic symptoms of chronic disease.
Footnotes
P- Reviewer: Haroche J S- Editor: Zhai HH L- Editor: Ma JY E- Editor: Wang CH
References
- 1.Haroche J, Arnaud L, Amoura Z. Erdheim-Chester disease. Curr Opin Rheumatol. 2012;24:53–59. doi: 10.1097/BOR.0b013e32834d861d. [DOI] [PubMed] [Google Scholar]
- 2.Lachenal F, Cotton F, Desmurs-Clavel H, Haroche J, Taillia H, Magy N, Hamidou M, Salvatierra J, Piette JC, Vital-Durand D, et al. Neurological manifestations and neuroradiological presentation of Erdheim-Chester disease: report of 6 cases and systematic review of the literature. J Neurol. 2006;253:1267–1277. doi: 10.1007/s00415-006-0160-9. [DOI] [PubMed] [Google Scholar]
- 3.Wright RA, Hermann RC, Parisi JE. Neurological manifestations of Erdheim-Chester disease. J Neurol Neurosurg Psychiatry. 1999;66:72–75. doi: 10.1136/jnnp.66.1.72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mascalchi M, Nencini P, Nistri M, Sarti C, Santoni R. Failure of radiation therapy for brain involvement in Erdheim Chester disease. J Neurooncol. 2002;59:169–172. doi: 10.1023/a:1019649201324. [DOI] [PubMed] [Google Scholar]
- 5.Haroche J, Amoura Z, Dion E, Wechsler B, Costedoat-Chalumeau N, Cacoub P, Isnard R, Généreau T, Wechsler J, Weber N, et al. Cardiovascular involvement, an overlooked feature of Erdheim-Chester disease: report of 6 new cases and a literature review. Medicine (Baltimore) 2004;83:371–392. doi: 10.1097/01.md.0000145368.17934.91. [DOI] [PubMed] [Google Scholar]
- 6.Arnaud L, Pierre I, Beigelman-Aubry C, Capron F, Brun AL, Rigolet A, Girerd X, Weber N, Piette JC, Grenier PA, et al. Pulmonary involvement in Erdheim-Chester disease: a single-center study of thirty-four patients and a review of the literature. Arthritis Rheum. 2010;62:3504–3512. doi: 10.1002/art.27672. [DOI] [PubMed] [Google Scholar]
- 7.Allen TC, Chevez-Barrios P, Shetlar DJ, Cagle PT. Pulmonary and ophthalmic involvement with Erdheim-Chester disease: a case report and review of the literature. Arch Pathol Lab Med. 2004;128:1428–1431. doi: 10.5858/2004-128-1428-PAOIWE. [DOI] [PubMed] [Google Scholar]
- 8.Pan A, Doyle T, Schlup M, Lubcke R, Schultz M. Unusual manifestation of Erdheim-Chester disease. BMC Gastroenterol. 2011;11:77. doi: 10.1186/1471-230X-11-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Singhi AD, Montgomery EA. Gastrointestinal tract langerhans cell histiocytosis: A clinicopathologic study of 12 patients. Am J Surg Pathol. 2011;35:305–310. doi: 10.1097/PAS.0b013e31820654e4. [DOI] [PubMed] [Google Scholar]
- 10.Gundling F, Nerlich A, Heitland WU, Schepp W. Biliary manifestation of Erdheim-Chester disease mimicking Klatskin’s carcinoma. Am J Gastroenterol. 2007;102:452–454. doi: 10.1111/j.1572-0241.2006.00893.x. [DOI] [PubMed] [Google Scholar]
- 11.Gupta A, Aman K, Al-Babtain M, Al-Wazzan H, Morouf R. Multisystem Erdheim-Chester disease; a unique presentation with liver and axial skeletal involvement. Br J Haematol. 2007;138:280. doi: 10.1111/j.1365-2141.2007.06642.x. [DOI] [PubMed] [Google Scholar]
- 12.Arnaud L, Hervier B, Néel A, Hamidou MA, Kahn JE, Wechsler B, Pérez-Pastor G, Blomberg B, Fuzibet JG, Dubourguet F, et al. CNS involvement and treatment with interferon-α are independent prognostic factors in Erdheim-Chester disease: a multicenter survival analysis of 53 patients. Blood. 2011;117:2778–2782. doi: 10.1182/blood-2010-06-294108. [DOI] [PubMed] [Google Scholar]


