Summary
Background
Emergency departments (EDs) routinely struggle with gaps in information when providing patient care. A point to point health information exchange (HIE) model has the potential to effectively fill those gaps.
Objective: To examine the utility, perceived and actual, of a point-to-point HIE tool called Care Everywhere (CE) and its impact on patient care in the ED.
Methods
This mixed methods study was performed at four large hospital EDs between January 2012 and November 2012. Retrospective data was extracted from the electronic health record (EHR) to evaluate CE utilization since implementation. ED notes data were extracted from ED visits occurring between January 2012 and June 2012 and were reviewed to evaluate the impact of exchanged information on patient care.
Results
Per focus group discussions, physicians thought the information received via CE was of value to patient care, particularly laboratory results, imaging, medication lists, discharge summaries and ECG interpretations. They feel the greatest impact of HIE is the avoidance of duplicative diagnostic testing and the identification of drug-seeking behavior. Nursing and ancillary staff expressed somewhat less enthusiasm but still felt HIE positively impacted patient care. Over a period of six months, CE was used in approximately 1.46% of ED encounters. A review of ED provider notes over that time period revealed CE use resulted in 560 duplicate diagnostic procedures being avoided and 28 cases of drug seeking behavior identified.
Conclusion
Our study provides insight into the perceived value of HIE from the point of view of our ED physicians and staff. It also demonstrates that a point-to-point HIE tool such as Epic System’s Care Everywhere has the potential to generate greater efficiencies within the ED and impact to patient care through elimination of duplicative diagnostic imaging or testing and resource utilization associated with those procedures.
Keywords: Health information exchange, HIE, emergency department, ED
1. Introduction
Health information exchange (HIE) is the sharing of patient information across disparate and/or competing healthcare service providers [1]. As Americans increasingly seek healthcare from multiple organizations [2], HIE has the potential to improve continuity of care between healthcare organizations and providers, improve quality [3], enhance patient safety [4-6]], increase efficiency, and result in cost savings [7-12]]. Unification of information networks and data sharing across providers will empower caregivers to make therapeutic decisions with a more holistic perspective. Although this vision of a healthcare infrastructure, where a patient’s medical records are fully available to the caregiver at the point of care, is not yet fully realized, developing systems capable of complete information exchange remains a primary goal in the field of health informatics. To that end, the framework to support HIE is evolving [13, 14]; standards are being established to facilitate exchange between disparate systems, legislation has been enacted to require exchange, and up to $27 billion in Medicare and Medicaid incentive payments over 10 years has been made available for providers who employ electronic health records (EHRs) and demonstrate meaningful use [15]. Indeed, financial incentives from the American Recovery and Reinvestment Act (ARRA) are bolstering the development of state, regional and national infrastructure required to support HIE [16]. Currently, the majority of these incentives are targeted towards federated models of HIE which involve the creation, support and maintenance of record locator services [17], but meaningful use criteria have also fostered a demand for point-to-point record exchange tools such as Epic Systems Corporation’s Care Everywhere (CE). While statewide, regional and national federated models of HIE are ultimately the goal of legislation, the long-term financial sustainability of such systems, the loss of provider revenue from reduced duplicative diagnostic procedures, discomfort with test results from other institutions, and the reduced value of diagnostic and procedural competitive advantages across providers constitute considerable barriers to stakeholder adoption [10, 11, 16, 18, 19]. Until the financial obstacles to creating federated HIEs can be resolved, we hypothesize existing and readily available point-to-point HIE tools may have equal clinical merit, and positively impact patient care.
2. Objective
The objective of this study was to investigate the following at four large metropolitan EDs:
Physician’ perceptions of the utility and impact of CE on patient care,
Nursing and ancillary staff perceptions of the utility and impact of CE on patient care,
The frequency of CE use, and
The actual impact of CE on patient care as documented by ED physicians in the patient record.
2.1 Background and Significance
EDs routinely struggle with gaps in patient information and may frequently provide care without complete knowledge of the patient’s past medical history [5, 20-24]. Indeed, in 2003, Finnell and colleagues reported that 25% of emergency department patients had medical information stored in another hospital system [23]. This is concerning because emergency departments are the arena where timely access to information regarding past medical history can be most critical to patient care and successful outcomes [3, 5]. Outdated methods for obtaining patient information such as faxed records, phone calls to providers and/or other health systems, and patient or family recall can be very time intensive, deficient in detail, and inaccurate or incomplete when the patient makes a poor historian. Accordingly, we believe HIE holds enormous potential for eliminating clinically relevant health information gaps in a timely, cost effective, and consistent way.
Three primary models for HIE have been developed: centralized, decentralized (or federated), and point-to-point. These models represent significant change in the architecture of HIEs [25]. The centralized model stores all patient data in a central repository and provides information to health care providers on an as needed basis. In the decentralized or federated model, the data remain stored locally in the source EHR of the provider and the external providers query the source record utilizing a record locator service [17]. Concerns have been raised for both of these models with regards to initial resource investment and financial sustainability [26, 27]. The third method of information exchange, point-to-point HIE, sometimes referred to as a non-federated peer-to-peer network, consists of a consortium of providers that have agreed to participate in a point-to-point HIE. In this model there is no central repository or record locating service therefore locating patient records is dependent upon the patient informing the provider about care received at outside institutions. CE can be used to exchange records with other Epic or non-Epic sites assuming the other EHR supports the same standards-based messaging. Epic supports both „pull“ and „push“ transactions endorsed by HealtheWay™ and the Direct Project. The infrastructure for communicating with a non-Epic organization is the same as that used for communicating with an Epic organization.
3. Methods
Allina Health is a non-profit system of hospitals, clinics, and other care services in Minnesota and western Wisconsin. Allina facilities include 11 hospitals, more than 80 primary care and specialty clinics, 15 community pharmacy sites, and 3 ambulatory care centers. In 2012 Allina hospitals had 107,701 inpatient admissions, 1.2 million outpatient admissions, and 273,817 emergency care visits.
In 2004, Allina Health began the implementation of the Epic® Systems Corporation EHR system (branded Excellian®) at all hospitals and clinics. The implementation was a phased roll-out and by early 2008 the EHR was operational at all hospital and clinic sites. All of the information needed to care for the patient is accessed through Excellian®. Allina’s philosophy is “One Patient, One Record” with the goal being that the patients complete health history should be accessible from a single chart. The CE functionality was implemented in the Allina EDs in August 2010. The roll-out included communications to end users, mandatory on-line training in the use of CE and the provision of tip sheets to facilitate use. The general workflow associated with CE involves determining whether a patient has received care outside of the Allina Health system, obtaining written consent from the patient or legal guardian and uploading that consent into the EHR, performing a query to the site(s) of previous care, and uploading remote records into the Allina EHR. There was no shared or consistent workflow between the Allina ED sites and any staff member in the ED may consent and request records through CE. Once a site is live with CE they can immediately begin exchanging of information with any other Epic CE site. Allina Health primarily exchanges information via CE with 6 other health systems located in Minnesota and the surrounding states. When CE results are uploaded into the EHR, a menu item appears on the front page of the chart to indicate to the user that CE records are available for viewing. It is important to note, written consent to query CE must be obtained at each patient encounter within Minnesota due to privacy laws surrounding the exchange of protected health information.
3.1 Project Overview
This study was approved by Allina’s Institutional Review Board and began in February 2012. Our objectives were to describe utilization of CE in the ED setting, garner physician, nurse, and ancillary staff perceptions of CE in the ED, and evaluate the impact of CE on patient care. The study population included ED physicians, nurses, and ancillary staff, and patients who visited 4 large metro hospital EDs throughout the study period. These four community hospitals are the largest of the Allina Health network and are distributed between urban and suburban areas of Minneapolis and St. Paul. Allina Health shares coverage of these geographic areas with four other community health systems as well as a large county hospital. During the study period, Allina exchanged health information with most of these organizations using CE, however, exchange was not regularly being performed with non-Epic EHR sites. This study consisted of four components; face-to-face focus groups with physicians, administration of online surveys to nurses and ancillary staff, CE utilization analysis, and ED clinical note review.
3.2 Focus groups
Focus groups were held at regularly scheduled ED physician staff meetings at each of the 4 hospital sites. A set of scripted, open-ended questions was developed that reflected aspects of the workflow associated with the use of CE: discovery of care outside Allina, consent process, query process, quality and accessibility of information, perceptions of value, and need for enhancements or modifications to the tools. Comprehensive notes were taken by an investigator assisting the facilitator, but the sessions were not recorded.
3.3 Survey
A link to a web-based 34-item electronic survey was emailed to all non-physician ED staff including nurses, unit coordinators, and registration staff. The survey focused on the same 7 topical areas covered in the focus group sessions and included many of the same questions modified slightly to accommodate a survey format.
3.4 CE Utilization and Clinical Notes Review
The EHR database was queried to identify the set of all ED encounters at the four hospitals that occurred between January 1, 2012 and June 30, 2012 (n = 102,002). This set was then reduced to include only encounters where
CE consents had been scanned;
CE records had been imported into the EHR, and
Patients had consented to having their records used in research.
The provider notes from those (n = 1488) encounters were then screened by a non-clinician reviewer with health informatics training who flagged records containing any explicit reference to CE in the ED provider notes. An explicit reference was defined as a statement or statements in the note whereby the clinician indicated he/she reviewed the records received via CE and based on that information made a decision not to perform a diagnostic test or, in the case of drug seeking, stated overtly that using records received via CE provided evidence of drug-seeking behavior. In most cases the words “Care Everywhere” or some variation were included in the note. However, if the note referenced records stating the outside facilities name name rather than explicit reference to CE and records from that hospital were obtained during that visit we counted it as a positive result as well. This subset of encounters (n = 523) was then independently reviewed by both the initial and second non-clinician reviewer, with advanced clinical informatics training, who enumerated instances where diagnostics were avoided or drug-seeking behavior detected as a result of CE. Two ED physicians also reviewed a random sample of 100 of the 523 charts (50 each) to evaluate the accuracy of the findings of the non-clinician reviewers. Where discrepancies were noted in this subsample, results were adjudicated to arrive at the final counts of duplicate diagnostics or the identification of drug seeking behavior. Inter-observer agreement was calculated between the two non-clinician reviewers and between the reviewers and each ED physician.
4. Results
4.1 Focus Groups
A total of 49 Emergency Medicine practitioners from the four EDs participated in the focus groups. Hospital 1 had 13 participants, hospital 2 had 14, hospital 3 had 9, and hospital 4 had 13. Thirty four of the 49 participants were male, average respondent age was 41.7 with a range of 28–64 years, and on average they had 4.75 years experience using Allina’s EHR. Of the total 49 participants 40 were physicians, 4 physician assistants, 4 registered nurses, and 1 pharmacist.
Discovery of Care Provided Elsewhere: Not all patients are asked about care provided at facilities outside of Allina. Approaching a patient is highly dependent upon presentation, e.g. unconscious or incompetent, and history, and prognosis. Occasionally the patient’s family, care taker, or associate may inform ED staff of care elsewhere.
CE Consent: Although nurses or health unit coordinators (HUCs) usually obtain patient consent for CE during the ED encounter, feedback about consent was highly consistent across all staff types. Overwhelmingly, respondents stated they would prefer a more streamlined consent process that does not require written patient consent for each encounter in order to query for outside records. Staff also reported most patients do give consent when asked and the presence of patient’s family does not negatively impact the consent process.
CE Query Process: Most often the HUC or Nurse does query, but MDs will also do it occasionally. There were some complaints about the user interface to CE and general “clunkiness” of query process. However, most of the time when a query is performed data is present.
Accessibility of information: Respondents stated they would like to see the presentation of information from CE be more stylistically consistent with how information is presented elsewhere throughout the EHR. Of interest, they felt it was difficult to sort through notes received via CE. While the majority of respondents felt retrieved information is always reviewed, when asked if retrieved information is ever not reviewed, staff mentioned that the physician may not be aware data is available if a nurse or HUC performs the query. Under such circumstances, the results would not be reviewed.
Quality of information retrieved: The most valuable information available in retrieved records was laboratory results, imaging interpretation, ECG interpretation, medication list, and discharge summaries. The least valuable were the daily inpatient notes. When asked what information was missing that would be of value, respondents unanimously agreed that seeing the actual ECG scan would be more beneficial than just the interpretation.
When asked how CE assisted in patient care, respondents most frequently stated CE reduced the need for lab testing, imaging procedures, and other diagnostics.
Not surprisingly, having a more complete patient chart available at the time of care was thought to increase throughput by improving diagnostic efficiency. When collecting a patient’s history, information retrieved through CE eliminates the need to use less efficient or dependable methods of information retrieval. Additionally, eligible professionals felt having the complete medication lists available assisted in avoiding medication errors. An interesting finding was the providers consider CE to be a two-way communication tool. That is, practitioners realize the information put into a patient’s chart will be seen by providers outside of the Allina Health system and accordingly can be used to communicate with those outside providers.
When asked, “What would you most like to change about CE?” Focus group participants consistently mentioned the burden of having to get patient consent at every visit as required by Minnesota law. Given this, respondents were very much in favor of a single overarching consent. A single consent was thought to be a key step towards increasing the efficacy of health information exchange while also reducing the administrative burden normally associated with a clinical encounter. Lastly, focus groups mentioned the desire to have information collected from CE be more seamlessly integrated into Epic’s user interface.
4.2 Surveys of ED nurses and ancillary staff
A link to a web-based survey was sent to 408 ED staff including nurses, nit coordinators and registration staff. 118 responses were received (RR = 28.9%). Respondents were 22% male (n = 26) and 78% female (n = 90). Respondent location was fairly evenly distributed across the four locations. 69% of respondents had over 7 years working experience at Allina and 83.3% of respondents had over 4 years’ experience using Epic EHR The survey was almost identical to the focus group questions and was formatted into the same 7 areas. Approximately half (48.6% n = 51) of respondents thought that all patients are asked if they have received care at a non-Allina facility. However, if a patient was not asked about care outside of Allina, respondents usually stated the presence of an operational barrier, i.e. the patient was unconscious or uncooperative (►Figure 1).
Fig. 1.
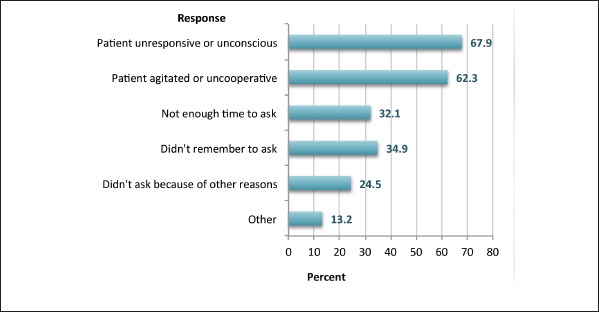
Nursing/Staff Survey: Barriers to discovery of care at an outside facility
Less frequently reported were reasons such as the ED staff forgetting to ask or not having time to ask. Interestingly, asking a patient about care received elsewhere is a necessary, but not sufficient criterion for using CE. Of the staff surveyed, 72.1% stated there are times when a patient has confirmed receiving care elsewhere, yet a CE query is not performed. The reasons for not doing a CE query when the patient has stated they have received care elsewhere are shown in ►Figure 2. Under these circumstances, the ED staff is consciously electing to forego performing a CE query. Surprisingly, the most selected response for this was perceived lack of physician interest with the CE results. This is a direct contradiction to the physician’s focus group results (►Figure 2).
Fig. 2.
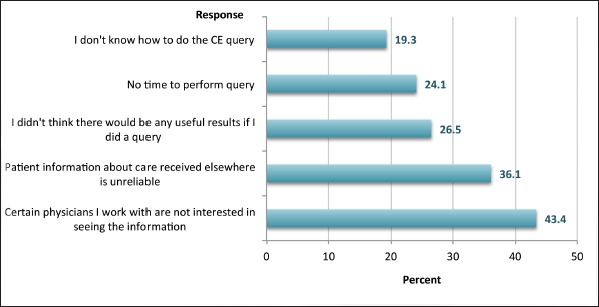
Reasons for not performing a CE query even if patient stated care was received elsewhere
When asked who routinely obtains consent for CE in the ED, 52.8% stated it was the ED nurse, 31.1% stated registration, and 28.3% thought another ED staff member and 16.0% stated the physician usually obtains consent. A total of 86.6% of respondents thought that when patients are asked they provide consent most or all of the time. In addition, 52.4% agreed or strongly agreed that the CE tools were easy to use, 65.1% thought once the information has been pulled in the EHR that it was easily accessible and 62.5% responded that it was always viewed. When asked if they felt information retrieved through CE was of value in patient care 26.9% stated sometimes but 72.1% stated almost always or always.
In response to the question “Has the information received via CE assisted you in the care of the patient?” 74.5% agreed or strongly agreed. In a series of questions users were asked if they thought CE eliminated the need for any procedures to be performed, lab tests, imaging or helped to identify drug seeking behavior. Respondents were asked if they felt CE saved them time in caring for their patients 57.4% agreed or strongly agreed.
4.3 Care Everywhere Utilization
During the 6 month study period there were 102,202 ED encounters, of which CE was used in 1488 instances (1.46%), affecting 1419 patients (►Figure 3). Within instances where CE was used, a reduction in diagnostic tests/procedures occurred in 234 of 1419, or 16% of patients. ►Figure 3 presents overall CE utilization by ED site since August 2010, the ED notes review study period is denoted between the vertical line markers. Utilization demonstrated a strong upward trend at one location, but had stagnant growth at the other three sites.
Fig. 3.
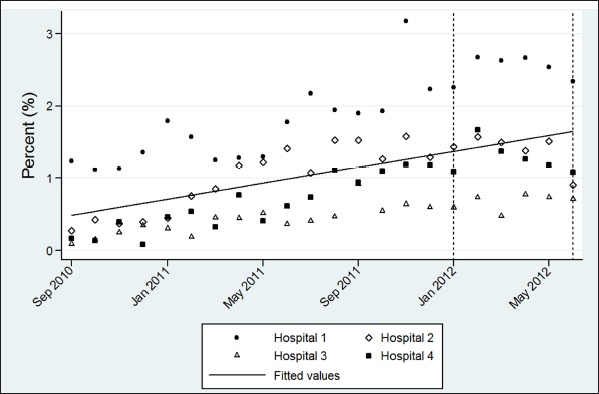
Overall CE Utilization by ED site
4.4 Clinical notes review
EHR ED clinical notes from patients who had CE used during their visits were reviewed to determine impact of CE on patients care. Out of 102,202 ED encounters, 1488 encounters (1419 patients) had utilized Care Everywhere. Corresponding ED encounter notes from this sample were manually reviewed for references to information provided by external sources. References to outside information were checked against the patient’s CE query results. For each validated reference, the type and number of tests avoided was recorded. Results are summarized in ►Figure 4 and ►Figure 5. Inter-observer agreement was substantial between non-clinician reviewers (71.1%) as well as each non-clinician reviewer and clinicians (74.7% NF, 72.5%TW). ED clinical notes revealed CE provides a notable impact to patient care, primarily in the avoidance of duplicate imaging as well as enhancing providers’ ability to identify patients with drug seeking patterns. In total, provider notes from the four hospitals revealed 560 duplicate diagnostic tests and procedures, impacting 234 patients, were avoided by the use of CE (►Table 2 for example quotes). Additionally, CE assisted in the identification drug seeking behavior in 28 encounters from 25, unique patients (not shown).
Fig. 4.
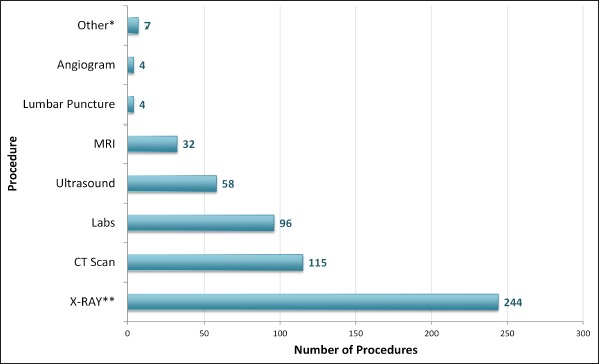
Impact of CE on avoidance of duplicate procedures and diagnostic testing. *Additional results not shown: 1 EGD, 2 EKG, 2 TTE, 2 Stress Echo; **Count represents X-Ray views performed, not unique orders
Fig. 5.
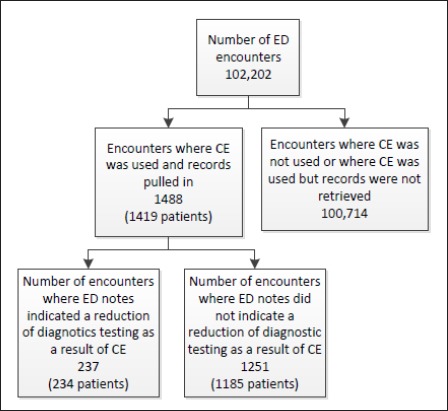
ED Encounters and Utilization and Impact of CE
Table 2.
Quotes from ED Note Review
| Category | Quote |
|---|---|
| Drug Seeking | Of note, the patient is prescribed the Oxycodone by his primary physician. His daily dose includes three 10 mg tablets. At present, he no longer has any pills left and reports that his most recent prescription „did not cover the whole month.“ Per medical records, there is a unique treatment plan for the patient that states he is not to receive narcotic prescriptions in the ED. |
| X-Ray | This year old male presents with ongoing chronic knee pain in which a recent xray was done at [hospital X]. Upon viewing this xray, it is noted that there is bone spurring as well as degeneration. His main complaint is increasing pain and locking of the knee. There is no redness or swelling suggestive of infection. No recent trauma, so no need for a repeat xray. |
| CT Scan | I was concerned about intracranial process including epidural/subdural s/p trauma as well as dissection…I was however, reassured by recent Normal head CT at outside hospital. Recent CT imaging 2 days ago makes tumor/pseudotumor less likely. |
| Labs, Ultrasound | Care everywhere evaluated labs and ultrasound performed recently at [hospital Y] hospital. Felt no need to repeat basic blood tests or her urine test. |
| CT Scan and Ultrasound | Patient has had workup for this including CT and ultrasound, I reviewed the results in care everywhere, the only finding was gastric inflammation of the CT scan. His laboratory were unremarkable and he had repeat labs today at [hospital X] which were reviewed and unremarkable. His exam is consistent with gastritis or ulcer and I don’t think he needs repeat imaging or labs today. |
| CT Scan | The patient’s Care Everywhere [hospital X] records suggest the patient is a poor historian in that her MVC apparently took place on [date] as opposed to [date]. During her post MVC evaluation, CT scans of her head and cervical spine were unremarkable. |
| US and Labs | She also had an ultrasound at [hospital X] that was read as negative. She also had GC chlamydia and wet prep a couple of days ago, therefore I did not repeat these. |
| US | US from [hospital X] reviewed and as above. I do not feel that repeat us is indicated as pain has not changed. |
| CT Scan | Recent CT scan as of 4 days ago at [hospital X] showed no acute abnormality, no evidence for obstruction, and a report of significant fecal material in the colon but no mention of obstipation. CT scan 4 days ago does not show extrinsic compression, abnormal pathologic findings external to the colon. I do not see any point in repeating a CT scan today. |
| CT Scan | Care Everywhere was reviewed which demonstrated that the patient has been evaluated by pulmonology for recurrent pneumonia…Further imaging did not appear to be indicated as the patient had a CT scan within the past month. |
5. Discussion
Our results show that physicians perceive HIE, specifically CE, to be an invaluable asset in the ED. They felt that CE provides a mechanism to mitigate gaps in information, assist in the reduction of duplicative diagnostic testing and procedures and ultimately save time and improve patient outcomes. However they indicated the process for obtaining patient records has room for improvement. Specifically Minnesota consent laws which mandate repetitive consent requests across providers are perceived to be a limitation to workflow efficiency by practitioners. When compared to their physician counterparts, non-physician staffs have a slightly less positive outlook on the impact of CE. However, such an outlook is not unexpected as physicians are the primary information users and as such they can more readily see the impact CE has on patient care.
We found utilization of CE was and still is much lower than expected. This study found 1.46% of ED patients have queries performed to obtain CE information. Previous studies found information exchange rates of 2.3-6.8% [11, 16, 28]. Yet, determining expected utilization levels is a challenge because HIE, and by extension CE, has several key dependencies. Moreover, studies examining HIE use determinants have produced counterintuitive and inconsistent results [4, 16, 29]. First and foremost, CE use is likely to be dependent on the expected utility of use. Utility in turn is dependent upon a transient patient population seeking care from multiple providers across separate networks. Accordingly, it’s logical that an inverse relationship exists between the size of an organization and the potential utilization/impact of CE. If a health system has many facilities in a region, as Allina Health does, and those facilities share a common EHR, then subsequently the probability a given patient has obtained care from outside the network is lower than for a single provider or smaller provider network. Notably, CE is a measure of information exchange between different provider networks and not reflective of efficiency gains from the use of an EHR system. Furthermore, using CE is also highly dependent upon patient consent. In Minnesota, laws consider this type of HIE to be medical record disclosure and, as such, patient consent is required for every time a query is done for outside records. Lastly, the benefit from CE is dependent upon the clinical presentation and history of present illness. For example, CE is less likely to have an impact for initial ED encounters related to an acute injury. Conversely, CE may have a significant impact in aiding in the treatment of patients with an underlying chronic condition or in follow up encounters after an acute traumatic event [30].
Although the utilization rate of 1.46% found in this study is lower than we expected (CE used in 1488/102,002 visits/total ED visits in study period), the potential impact of information exchange can still be significant. CE reduced diagnostic testing, helped to identify drug seeking behavior, and facilitated a higher degree of provider connectedness. Less invasive procedures such as EKGs and lab tests were minimally reduced by CE which correlates with previous studies [30]. However, our investigation noted CE’s ability to provide outside test results used for serial comparison throughout the differential diagnostic process. Accordingly, CE may allow providers to reach a diagnosis more quickly and with more confidence by providing supplemental information. This benefit has implications for the quality of care offered to patients and may reduce the need for follow up appointments required to gather more information. Nevertheless, compared to mixed results of previous studies, the largest impact we found of CE use in the ED was the reduction of the more costly and time consuming imaging tests such as CT Scans, MRIs, and X-rays [19].
The strength of this study is that it provides a solid quantification of the impact of health information exchange in terms of reduction of duplicate diagnostic testing and discovery of drug-seeking behavior. It also provides insight into the perceived value of HIE from the ED physicians and ED staff point of view. However, this study is not without limitations. Variable free-text documentation practices within and across hospital groups necessitated a manual review study methodology. Accordingly, provider failure to document and reviewer failure to perceive or interpret use of CE may be sources of bias in this analysis. However, eliminating such errors would likely demonstrate a higher value of CE given the majority of encounters were non-revealing. Nevertheless, caution should be used when extrapolating the results of this study. Notably, the relatively low survey response rates, and dependence on patient consent to use CE are factors that conceivably obscure the true opinions, impact, and potential of CE in the ED. Furthermore, patient motivation to obscure medical history or treatments, particularly in the case of drug seeking patients, cannot be ruled out as a source of bias.
In conclusion, our study has demonstrated that a point-to-point HIE tool such as Epic System’s Care Everywhere is currently an underutilized feature with the potential to generate greater efficiency gains within the ED through elimination of duplicative diagnostic imaging or testing and resource utilization associated with those procedures.
Moving forward, we plan to provide this feedback to ED staff which will hopefully lead to increased utilization and improve documentation practices around role of CE in clinical decision making. In addition we plan on continuing the review of clinical notes for an eventual financial analysis of savings to the patient and the health system.
Table 1.
CE Impact on Patient Care
| Yes | No | IDK | |
|---|---|---|---|
| Has CE eliminated the need for certain procedures to be performed | 60.2% (n = 62) | 10.7% (n = 11) | 29.1% (n = 30) |
| Has CE eliminated the need for a laboratory test to be performed | 53.4% (n = 55) | 13.6% (n = 14) | 33.0% (n = 34) |
| Has CE eliminated the need for an imaging procedure to be performed | 69.7% (n = 69) | 7.1% (n = 7) | 23.2% (n = 23) |
| Has CE helped identify a drug seeking patient | 73.8% (n = 76) | 2.9% (n = 3) | 23.3% (n = 24) |
Footnotes
Clinical Relevance
This research demonstrates the utility of a point-to-point HIE in reducing the amount of diagnostic testing needed in the emergency department. The providers felt that the HIE was a valuable tool as it assisted them in providing more efficient care and increasing throughput in the ED.
Human Subjects Protections Statement
The study was performed in compliance with the World Medical Association Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Subjects, and was reviewed by the Allina Health Institutional Review Board (IRB #3502–1E.)
Funding Statement
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing Interests Statement
The authors have no competing interests to declare.
Contributorship Statement
All authors have contributed to this work in design, acquisition, analysis, interpretations or data and in drafting and reviewing this manuscript.
References
- 1.Vest JR.More than just a question of technology: factors related to hospitals’ adoption and implementation of health information exchange. International journal of medical informatics 2010; 79(12): 797–806 [DOI] [PubMed] [Google Scholar]
- 2.National Center For Health Statistics. Health, United States, 2012 : With Special Feature on Emergency Care,. Hyattsville MD, 2013. Hyattsville MD: National Center For Health Statistics, 2004 [PubMed] [Google Scholar]
- 3.Hripcsak G, Sengupta S, Wilcox A, Green RA.Emergency department access to a longitudinal medical record. Journal of the American Medical Informatics Association 2007; 14(2): 235–238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Institute of Medicine. Hospital-Based Emergency Care: At the Breaking Point. Washington DC: National Academy Press, 2006 [Google Scholar]
- 5.Stiell A, Forster AJ, Stiell IG, van Walraven C.Prevalence of information gaps in the emergency department and the effect on patient outcomes. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne 2003; 169(10): 1023–108 [PMC free article] [PubMed] [Google Scholar]
- 6.Smith PC, Araya-Guerra R, Bublitz C, Parnes B, Dickinson LM, Van Vorst R, Westfall JM, Pace WD.Missing clinical information during primary care visits. JAMA 2005; 293(5): 565–571 [DOI] [PubMed] [Google Scholar]
- 7.Minnesota Department of Health. State Health Information Exchange Cooperative Agreement – Minnesota 2012 Strategic and Operation Plan Update. In: Technology MDoHOoHI, editor,2012 [Google Scholar]
- 8.Overhage JM, Dexter PR, Perkins SM, Cordell WH, Mc Goff J, Mc Grath R, Mc Donald CJ.A randomized, controlled trial of clinical information shared from another institution. Annals of Emergency Medicine 2002; 39(1): 14–23 [DOI] [PubMed] [Google Scholar]
- 9.Vest JR.Health information exchange and healthcare utilization. Journal of Medical Systems 2009; 33(3): 223–231 [DOI] [PubMed] [Google Scholar]
- 10.Frisse ME, Holmes RL.Estimated financial savings associated with health information exchange and ambulatory care referral. Journal of Biomedical Informatics 2007; 40(6Suppl.): S27-S27 [DOI] [PubMed] [Google Scholar]
- 11.Johnson KB, Unertl KM, Chen Q, Lorenzi NM, Nian H, Bailey J, Frisse M.Health information exchange usage in emergency departments and clinics: the who, what, and why. Journal of the American Medical Informatics Association 2011; 18(5): 690–697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tzeel A, Lawnicki V, Pemble KR.The Business Case for Payer Support of a Community-Based Health Information Exchange : A Humana Pilot Evaluating Its Seeking Emergency Department Care. American Health & Drug Benefits 2011; 4: 207–216 [PMC free article] [PubMed] [Google Scholar]
- 13.Dixon BE, Zafar A, Overhage JM.A Framework for evaluating the costs, effort, and value of nationwide health information exchange. Journal of the American Medical Informatics Association 2010; 17(3): 295–301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Office of the National Coordinator. Nationwide Health Information Network,2013 [Google Scholar]
- 15.Gold MR, Mc Laughlin CG, Devers KJ, Berenson Ra, Bovbjerg RR.Obtaining providers’ ’buy-in’ and establishing effective means of information exchange will be critical to HITECH’s success. Health affairs (Project Hope) 2012; 31(3): 514–526 [DOI] [PubMed] [Google Scholar]
- 16.Vest JR, Zhao H, Jasperson J, Jaspserson J, Gamm LD, Ohsfeldt RL.Factors motivating and affecting health information exchange usage. Journal of the American Medical Informatics Association 2011; 18(2): 143–149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Healthcare Information and Management Systems Society (HIMSS). Topic Series: HIE Technical Models,2009 [Google Scholar]
- 18.Brailer DJ.From Santa Barbara to Washington: a person’s and a nation’s journey toward portable health information. Health Aff (Millwood) 2007; 26(5): w581–w588 [DOI] [PubMed] [Google Scholar]
- 19.Bailey JE, Pope RA, Elliott EC, Wan JY, Waters TM, Frisse ME.Health Information Exchange Reduces Repeated Diagnostic Imaging for Back Pain. Annals of Emergency Medicine 2013; 62(1): 16–24 [DOI] [PubMed] [Google Scholar]
- 20.Cordell WH OJ, Waeklerle JF.Strategies for Improving Information Management in Emergency Medicine to Meet Clinical, Research, and Administrative Needs. Academic Emergency Medicine 1998: 2–8 [PubMed] [Google Scholar]
- 21.Kalra J.Medical errors: an introduction to concepts. Clinical biochemistry 2004; 37(12): 1043–1051 [DOI] [PubMed] [Google Scholar]
- 22.Shapiro JS, Kannry J, Kushniruk AW.Emergency physicians’ perceptions of health information exchange. Journal of the American Medical Informatics Association 2007(14): 700–705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Finnell JT, Overhage JM, Dexter PR, Perkins SM, Lane KA, Mc Donald CJ.Community Clinical Data Exchange for Emergency Medicine Patients Regenstrief Institute for Health Care. AMIA … Annual Symposium proceedings / AMIA Symposium. AMIA Symposium 2003: 235–238 [PMC free article] [PubMed] [Google Scholar]
- 24.Connelly DP, Park YT, Du J, Theera-Ampornpunt N, Gordon BD, Bershowv BA, Gensinger RA, Shrift M, Routhe DT, Speedie SM.The impact of electronic health records on care of heart failure patients in the emergency room. Journal of the American Medical Informatics Association 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lenert L, Sundwall D, Lenert ME.Shifts in the architecture of the Nationwide Health Information Network. Journal of the American Medical Informatics Association 2012; 19(4): 498–502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.HIMSS 2008–2009 HIE Work Group. A HIMSS Guide to Participating in Health Information Exchange.2009 [Google Scholar]
- 27.Vest JR, Gamm LD.Health information exchange: persistent challenges and new strategies. Journal of the American Medical Informatics Association 2010; 17(3): 288–294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Frisse ME, Johnson KB, Nian H, Davison CL, Gadd CS, Unertl KM, Turri PA, Chen Q.The financial impact of health information exchange on emergency department care. Journal of the American Medical Informatics Association 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Unertl KM, Johnson KB, Lorenzi NM.Health information exchange technology on the front lines of healthcare: workflow factors and patterns of use. Journal of the American Medical Informatics Association 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ross SE.The effects of health information exchange adoption on ambulatory testing rates. Journal of the American Medical Informatics Association 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]


