Summary
Background
Alcohol use is a significant part of a patient’s history, but details about consumption are not always documented. Electronic Health Record (EHR) systems have the potential to improve assessment of alcohol use and misuse; however, a challenge is that critical information may be documented primarily in free-text rather than in a structured and standardized format, thereby limiting its use.
Objective
To characterize the use and contents of free-text documentation for alcohol use in the social history module of an EHR.
Methods
This study involved a retrospective analysis of 500 alcohol use entries that include structured fields as well as a free-text comment field. Two coding schemes were developed and used to analyze these entries for: (1) quantifying the reasons for using free-text comments and (2) categorizing information in the free-text into separate elements. In addition, for entries indicating possible alcohol misuse, a preliminary review of other structured parts of the EHR was conducted to determine if this was also documented elsewhere.
Results
The top three reasons for using free-text were limited ability to describe alcohol use frequency (75%), amount (22%), and status (18%) with available structured fields. Within the free-text, descriptions of frequency were most common (79%) using words or phrases conveying occasional (61%), daily (13%), or weekly (12%) use. Of the 36 cases suggesting alcohol misuse, 44% had mention of alcohol problems in the problem list or past medical history.
Conclusions
Based on the early findings, implications for improving the structured collection and use of alcohol use information in the EHR are provided in four areas: (1) system enhancements, (2) user training, (3) decision support, and (4) standards. Next steps include examining how alcohol use is documented in other parts of the EHR (e.g., clinical notes) and how documentation practices vary based on patient, provider, and clinic characteristics.
Keywords: Alcohol drinking, alcoholism, medical history taking, electronic health records
1. Background
The lifetime prevalence of alcohol use disorders is approximately 30% in the United States and costs the nation nearly $224 billion a year [1, 2]. Chronic alcohol abuse and dependence not only lead to debilitating medical conditions such as liver cirrhosis, Wernicke-Korsakoff syndrome, fetal alcohol syndrome, and alcoholic cardiomyopathy, but can also contribute to traffic accidents, violence, suicide, and crime [3]. Though alcohol use is a significant part of a patient’s history, details about alcohol consumption are not always documented in the health record [4, 5]. In one study, older patients with undocumented alcohol abuse issues were found to be more likely to be hospitalized and have higher mortality rates [6]. Having an accurate picture of each patient’s alcohol use—past and present—is essential for clinicians to provide the best care.
The latest recommendation by the U.S. Preventive Services Task Force is to screen adults and provide brief behavioral counseling interventions to reduce alcohol misuse [7]. The National Institute on Alcohol Abuse and Alcoholism has published a guide that provides an evidence-based approach for supporting primary care clinicians in the screening, assessment, and treatment of alcohol use disorders [8, 9]. For screening, preferred tools include the single-question screen, Alcohol Use Disorders Identification Test (AUDIT), and abbreviated AUDIT-Consumption (AUDIT-C) that include questions about frequency of drinking, typical amount, and frequency of heavy drinking [10-12]. If there is suspected risk drinking, assessment by the clinician could include evaluating consumption patterns (e.g., number of days per week, number of drinks on a typical day, maximum number of drinks consumed on an occasion, and number of days per month of heavy drinking), checking the Diagnostic and Statistical Manual of Mental Disorders criteria for alcohol use disorders, and documenting alcohol-related history for those with an alcohol use disorder (e.g., other substance abuse, previous treatment attempts, periods of sobriety, and stability of the patient’s environment) [13].
The increased prevalence of Electronic Health Record (EHR) systems has the potential for improved availability and completeness of patient information [14]. With regards to alcohol use, the EHR could play a valuable role in identification, prevention, and treatment of alcohol misuse and related conditions. Documentation of alcohol and substance abuse in the EHR has been shown to help predict suicide risk in depressed patients [15] and electronic clinical reminders for alcohol counseling have been associated with moderate decreases in drinking in AUDIT-C positive patients [16]. While some studies have reported issues with no or poor alcohol documentation in the health record over 50–75% of the time for specific settings (e.g., emergency clinic [17] and primary care [18]) and populations (e.g., cancer [19] and psychiatric in-patients [20]), recent studies have emerged describing the use of EHRs for improving alcohol screening and brief interventions [21-23]. Further research is needed to study and improve clinical documentation processes with the EHR in order to better support clinical workflow and decision-making [14].
A continuous challenge is the use of free-text documentation versus structured documentation and determining the optimal mix for maximizing usability and usefulness [24] where further studies are needed to understand the effect of particular documentation styles on quality of care [25]. For example, the benefit of computerized provider order entry (CPOE) for reducing medication errors is limited when orders are entered as free-text [26]. In response to this challenge, there have been numerous efforts to develop automated natural language processing (NLP) approaches for extracting, structuring, and encoding information within full-text clinical notes in the EHR [27, 28], including for smoking status [29]. Fewer studies have focused on free-text in other parts of the EHR such as problem lists [30, 31], medications [26, 31], and family history [32]. Once extracted, information captured within free-text could potentially be leveraged to improve patient care and decision support as well as support secondary uses such as quality and research.
2. Objectives
As part of a broader goal to understand and improve alcohol use documentation in the EHR, the focus of this study is to examine the current use and contents of free-text documentation for alcohol use in the social history module of an EHR. Characterizing why free-text is being used and what is being captured within free-text could provide guidance for enhancing the structured and standardized collection of alcohol use information to support patient care and research. In addition, examining how potential alcohol issues are documented in the social history module compared with other parts of the EHR could inform the development of integrated decision support tools.
3. Methods
3.1 Setting
This study involved a retrospective analysis of patient records at Fletcher Allen Health Care (FAHC), the academic health center affiliated with the University of Vermont [33, 34]. The Epic EHR has been in use at FAHC since 2009 and provides a range of functionality including ambulatory and in-patient clinical documentation, CPOE, clinical decision support, and reporting and analysis capabilities [35]. Within this EHR, alcohol use and misuse can be documented in various parts of the record including the problem list, past medical history, social history, and within clinical notes. In the social history module, there are dedicated areas for the structured documentation of substance use (tobacco, alcohol, and illicit drug use), which may be used to automatically pre-populate the social history section in clinical notes using defined templates.
For alcohol use, four structured fields are available for documenting: status (“Yes,” “No,” or “Not asked”), use/week (e.g., “2” or “3–4”) regarding four different types of alcohol that are associated with varying alcohol content (“cans of beer” [12 oz], “glasses of wine” [5 oz], “shots of liquor” [1.5 oz], and “drinks containing 0.5 oz of alcohol”), and amount of alcohol/week in ounces, which is automatically computed based on use/week and type. In addition to these structured fields, clinicians are able to comment in a free-text field, which is the focus of this study (►Table 1). In 2013, this free-text comment field for alcohol use was used for 33.7% of patients who had information documented using the social history module.
Table 1.
Examples of Alcohol Use Entries
| Status | Use/week | Type | Amount of alcohol/week* | Comment |
|---|---|---|---|---|
| Yes | 14 | Glasses of wine | 70 oz | wine, beer, scotch/1–2 glasses per day |
| Yes | 2 | Shots of liquor | 3 oz | Occasionally 2 x monthly |
| No | - | - | - | quit many years ago |
| Not Asked | 1 | Cans of beer | 12 oz | rarely |
| Yes | - | - | - | alcohol abuse |
* Calculated field based on Use/week and Type
3.2 Coding Schemes
Two coding schemes were developed for: (1) identifying and quantifying reasons for using the free-text comment field for alcohol use and (2) categorizing information captured within the free-text into separate elements for identifying common words or phrases. An iterative and consensus-based process was used to generate the coding schemes, which involved the analysis of 200 alcohol use entries from October 1, 2012 to November 30, 2012 by two reviewers (MGW [fourth-year medical student at the time of the study] and ESC [biomedical informatician]). The final coding scheme for “reasons” included twelve potential explanations for why the free-text comment field was used where a comment may be associated with one or more reasons (►Table 2). For example, the comment “Quit in 1970” would be coded with two reasons: (1) Limited ability to describe status and (2) Unable to specify age or date.
Table 2.
Coding Scheme for Reasons
| Reason | Description | Example Comments |
|---|---|---|
| Misplaced – use Use/week field | Should use available structured field (Use/week) | • 3 glasses of wine per week • 4–6 glasses of wine a week |
| Misplaced – use Type field | Should use available structured field (Type) | • glasses of wine • cans of beer |
| Limited ability to specify Use/ week | Use/week field cannot be used without a value specified for Type field | • One or two per week • 3 /?/x week |
| Limited ability to describe frequency | Frequency of alcohol use cannot be described using available fields | • occasional • rarely 6 times a year • 1 every other month |
| Limited ability to describe amount | Amount of alcohol cannot be described using available fields | • 1 drink per month • few beers • 1.5 pint whiskey/day |
| Limited ability to describe type | Alcohol type is not among the available values for Type field | • martinis • mixed drinks • drinks |
| Limited ability to describe status | Current status or context of alcohol use cannot be described using available fields or values for Status field | • Social • Quit in 1984 • None since pregnancy |
| Unable to specify age or date | Age or date related to alcohol use (e.g., when quit) cannot be specified | • Quit at age 32 • Quit in 2010 • Stopped 1983 |
| Unable to specify duration or timepoint | Duration or timepoint related to alcohol use cannot be specified | • None for seven years • Last drink on Saturday • sober /?/x 7months |
| Unable to indicate potential issues | Entry suggests the patient has (or had) a problem with alcohol | • occasionally binges on weekends • 2–6 beers per night • trying to be a recovering alcoholic |
| Multiple statements | Entry includes multiple pieces of information | • Previously heavy, currently rare • 6 beers daily. None today. |
| Other | Does not fit under any other reason | • Dilutes with water and ice • no smokers in the house |
The second coding scheme was adapted and expanded from previous studies that involved analyzing social history information, including alcohol use, in free-text clinical notes from multiple institutions as well as public health surveys for identifying a common set of data elements and values [36, 37]. Of the eight elements identified in those studies for describing the different aspects of alcohol use, five were found to be applicable to the present study and a new element for describing the situation or context of alcohol use was added. The final version of the coding scheme for “elements” included six elements where the contents of each comment may be categorized into one or more elements (►Table 3). For example, the comment “One beer infrequently” would be coded as Amount = “one,” Type = “beer,” and Frequency = “infrequently”.
Table 3.
Coding Scheme for Elements
| Element | Description | Example Comments |
|---|---|---|
| Status | Word or phrase describing current status of alcohol use | • quit many years ago • past alcohol use, quit 1990 |
| Temporal | Word or phrase indicating an age, date, or duration related to alcohol use (e.g., when started or when quit). May be specific or estimated. | • quit many years ago • past alcohol use, quit 1990 |
| Amount | Word or phrase describing amount of alcohol consumed. May be specific or estimated. | • few glasses wine/day • beer or wine 1–2 per month |
| Type | Word or phrase describing type of alcohol consumed. May be specific or vague. | • few glasses wine/day • beer or wine 1–2 per month |
| Frequency | Word or phrase indicating how often alcohol is consumed. May be specific or vague. | • one every 2 months • occasional beer |
| Situation | Word or phrase providing context in which alcohol is or is not consumed. | • none since pregnancy • wine nightly with meals |
Using the final versions of the coding schemes for reasons and elements, the two reviewers analyzed an additional set of 50 alcohol use entries from January 1, 2013 to January 31, 2013 to ensure consistency in coding. Inter-rater reliability was calculated using Cohen’s kappa, achieving κ (0.96) for coding reasons and κ (0.97) for coding elements. One reviewer (MGW) then performed the main analysis of 500 alcohol use entries.
3.3 Main Analysis
Alcohol use entries from February 1, 2013 to February 28, 2013 were obtained and randomized using a combination of Unix awk and sed commands. From the total of 12,976 entries including a free-text comment (for 9,720 unique patients), a subset of 500 entries was used for the main analysis where this number represents a sample size needed for a confidence level of 95% and estimated precision exceeding 5% (n=373). Each entry was analyzed using the two coding schemes to determine the most frequent reasons for using free-text and most common words or phrases for each element, which were subsequently grouped based on similar meaning or pattern. For example, the words “stopped” and “abstaining” were considered variations of “quit” for the Status element and the pattern “n years” covers phrases like “30 years ago” and “36 years” for the Temporal element.
In addition to coding the reasons and elements, any free-text comment indicating potential alcohol misuse (e.g., “currently drinking heavily,” “1/2 gallon vodka daily,” and “1 case beer daily”) was flagged to determine whether this suspected alcohol misuse was reflected in other pertinent structured areas of the patient’s record. For these cases, entries from the problem list and past medical history modules in the EHR were obtained and analyzed for alcohol-related conditions (e.g., “Alcohol abuse” [mapped to ICD-9-CM code 305.00], “Alcohol dependence in remission” [mapped to ICD-9-CM code 303.93], or “Current drinker of alcohol” [mapped to V69.8 for “Other problems related to lifestyle”] in the system).
4. Results
Based on the analysis of 500 alcohol use entries, ►Figure 1 depicts the distribution of reasons for using free-text and ►Table 4 includes the distribution of elements, total and unique values, and groups of values along with some example words and phrases.
Fig. 1.
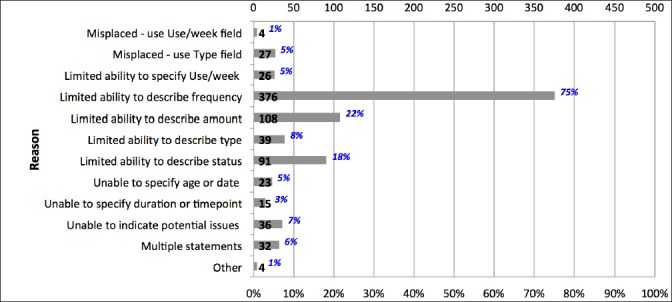
Distribution of Reasons
Table 4.
Distribution of Elements, Values, and Groups of Values
| Element | Total | #Entries | Total # Values | # Unique Values [# Groups] | Top 3 Groups of Values (Examples) | Frequency | |
|---|---|---|---|---|---|---|---|
| Status | 50 | (10.0%) | 61 | 41 [13] | • quit (quit, stopped, abstaining) | 23 | (37.7%) |
| • past or history of use (former alcohol abuse, h/o dependence, recovered alcoholic, past alcohol use) | 15 | (24.6%) | |||||
| • no (no, not, no alcohol) | 7 | (11.5%) | |||||
| Temporal | 45 | (9.0%) | 51 | 44 [14] | • specific or estimated year (1970, 1980s, since 2010) |
11 | (21.6%) |
| • specific or estimated number of years (14 years, 30 years ago, many years ago) |
10 | (19.6%) | |||||
| • specific date (mm/dd/yyyy) | 8 | (15.7%) | |||||
| Amount | 132 | (26.4%) | 138 | 67 [11] | • specific or estimated numeric amount (3, 2 glasses, 1 bottle, about 4, less than 2) |
69 | (50.0%) |
| • numeric range (4–6, 1 or 2, 2–3 glasses) | 49 | (35.5%) | |||||
| • none | 10 | (7.2%) | |||||
| Type | 93 | (18.6%) | 107 | 16 [10] | • wine (wine, red wine, white wine) | 39 | (36.4%) |
| • drink (drink, drinks, etoh) | 31 | (29.0%) | |||||
| • beer (beer, beers) | 28 | (26.2%) | |||||
| Frequency | 396 | (79.2%) | 406 | 105 [17] | • occasional (infrequent, intermittent, occasionally, rare, rarely, seldom) | 247 | (60.8%) |
| • daily or per day (/day, day, nightly, per day, per night) | 53 | (13.1%) | |||||
| • weekly or per week (/week, 3–4 times a week, couple times a week, weekly) | 49 | (12.1%) | |||||
| Situation | 61 | (12.2%) | 63 | 25 [15] | • social (social, social drinker, socially) | 35 | (55.6%) |
| • weekends (during the weekends, on weekends, weekends only) | 9 | (14.3%) | |||||
| • with meals (with dinner, with meals) | 5 | (7.9%) | |||||
Free-text was most often used due to limited ability to describe frequency of alcohol use using available structured fields (75%) and most frequently included words or phrases describing frequency of use (79%). Of the 406 total values (105 unique values) that were categorized into 17 groups, 61% were words conveying occasional use such as “occasional,” “occasionally,” “rare,” “rarely,” or “seldom”; 13% were words or phrases describing daily use such as “daily,” “n/day,” or “n per night” where n is a specific number or range; and, 12% were variations describing weekly use such as “weekly,” “n/week,” “n times a week,” “nxweek,” or “n per week”.
The next most frequent reason for using free-text was limited ability to describe amount using available structured fields (22%) with 26% of the entries containing 138 total values (67 unique values) for describing amount of use that were categorized into 11 groups. The most common words or phrases used were for describing a specific or estimated numeric amount such as “3” or “less than 2” (50%), numeric range such as “4–6” (36%), or none (7%).
Thirdly, there was limited ability to describe status using available structured fields (18%) with free-text describing details about status across the entries (10%) as well as details about a particular situation or context (12%). Of the 61 total values (41 unique) used for status, 38% of the words or phrases described quitting, 25% described past use or history of use, and 12% indicated no alcohol use. The 63 total values (25 unique) reflecting situations in which patients drank were categorized as words or phrases describing patients who drank socially (56%), on weekends (14%), or with meals (8%).
From the set of 500 alcohol use entries, 36 (7%) entries were identified as suggesting potential alcohol misuse. For the patients associated with these entries, a total of 16/36 (44%) had entries indicating alcohol problems in the problem list only (5/36 [14%]), past medical history only (6/36 [17%]), and both the problem list and past medical history (5/36 [14%]).
5. Discussion
This study has provided insights to the current use and contents of free-text documentation for alcohol use in the social history module of the Epic EHR at FAHC. Based on the early findings, implications for improving the collection and use of alcohol use information in the EHR are provided in four areas: (1) system enhancements, (2) user training, (3) decision support, and (4) standards. While limited to a single institution and social history module within a particular EHR system, it is anticipated that the recommendations provided below will be generalizable to other institutions that have the same or other EHR system. In addition, the methodology used in this study, including the two coding schemes, could be adapted and applied to other parts of the EHR (e.g., clinical notes) as well as to address institutional variations (including cultural and organizational practices) and EHR-specific differences.
5.1 System Enhancements
Analysis of the alcohol use entries revealed that free-text is most often used to have flexibility in describing frequency, amount, status, and type of alcohol use. In addition, the free-text was found to include temporal information such as ages, dates, or durations (e.g., quit date or duration since quitting), which could not be documented using available structured fields. The collective frequency of these reasons highlights the need for additional structured fields and values for existing fields to capture the full breadth of information associated with alcohol use. While there may continue to be a need to use free-text for specific details, these enhancements have the potential to significantly increase structured alcohol use documentation and limit the use of free-text.
In the current system, while structured fields are available for documenting number of drinks per week and subsequently calculating amount per week, clinicians are using free-text to record non-numeric amounts (e.g., “few”) and frequencies (e.g., “occasional”) as well as alcohol use for other frequency levels (e.g., per day or per month). Enhancing the system with additional structured data entry options could enable the capture of statements such as “2 cans of beer daily” and “occasional 2 beers” in addition to “2 cans of beer/week”. However, in allowing for more flexibility, considerations include how this might limit the ability to assess use/week (one of the more common methods of screening alcohol misuse) and the need for clear definitions and guidelines for ensuring consistent use (e.g., how is occasional use defined?).
In addition to guiding the development of structured fields, iterative analysis of the free-text comments could be used to inform modifications or additions to the lists of values associated with existing fields. For example, for status, more descriptive values such as “Current Drinker,” “Former Drinker,” “Never Drinker,” or “Never Assessed” could be used, which would be analogous to what is available for tobacco use status. Similarly, the list of alcohol types could be continuously enhanced and refined with values that appear more frequently in free-text (e.g., “red wine” and “white wine” in addition to the general “wine”).
5.2 User Training
While occurring less frequently, several reasons suggest that use of structured data entry where possible and limitations of free-text entry could be further emphasized as part of user training. For example, for cases where free-text was used rather than the available structured fields for use/week and type, training materials could include reminders of existing capabilities in the EHR and scenarios demonstrating use of available fields, including the role of the free-text comment field. Further assessment is needed to understand current workflows, including existing policies and procedures, which may affect how alcohol use is documented. In addition to performing retrospective EHR data analyses as was done in this study, future studies could involve the use of qualitative methods such as interviews and focus groups to understand current needs and workflow issues for further informing system enhancements and training. Other next steps include studying documentation patterns based on patient, provider, and clinic characteristics to determine if there are context-specific differences and potentially guide tailored training.
In the process of analyzing the 500 entries, several types of data quality issues were observed, including misspellings (6%) and abbreviations (13%) in the free-text comments. For example, there were six different misspellings for occasional or occasionally (e.g., “ocasional” and “occassionally“) and use of five different abbreviated forms (e.g., “occ” and “occas.”). Other examples include “v rare” for very rare, “reg” for regular, and “ETOH” for alcohol. In addition, 9% of the entries were found to include potentially ambiguous information with multiple interpretations. For example, do the comments “2–3 per month” and “1–2 daily” refer to number of drinks or number of times? The availability of additional structured fields and values as described earlier offers one option for addressing some of these issues (e.g., inclusion of a pre-defined value for “occasional” for frequency). In addition, as part of user training and education, the impact of these data quality issues could be highlighted and guidance provided for supporting consistent documentation going forward (e.g., avoiding abbreviations and reducing ambiguity).
5.3 Decision Support
Within the EHR, the incorporation of decision support mechanisms could play a valuable role in supporting alcohol use screening and assessment of alcohol misuse. Such mechanisms rely on the availability of accurate, consistent, and up-to-date information in structured form. For example, the AUDIT-C includes three questions with five possible responses related to frequency of use, amount per day, and frequency of heavy drinking [10, 11]. In the current system, these questions could be partially addressed by what is collected in the structured use/week field (i.e., responses of “2–3 times a week” and “4 or more times a week” to the first question “How often do you have a drink containing alcohol?”). In addition, development of automated NLP techniques could enable use of information captured within the free-text comments to provide other responses (e.g., “Monthly or less” or “2–4 times a month” for the first question) or address other questions (e.g., “How many standard drinks containing alcohol do you have on a typical day?). Next steps include exploring how to enable such integration with screening tools to provide alerts for positive screening results.
Among the entries, the contents of free-text for 36 (7%) cases suggested potential alcohol misuse. Based on a preliminary comparison with other structured parts of the EHR, 56% of these patients did not have documentation of alcohol problems in either the problem list or past medical history. This finding suggests the potential value of including an indicator within the social history module that could serve as a reminder of possible medical/surgical risks in relation to alcohol use. Further analysis is needed to determine how alcohol use is documented across the EHR, the consistency of documentation, and how to coordinate among the different parts of the EHR (e.g., social history, problem list, past medical history, and clinical notes).
5.4 Standards
With respect to alcohol use, there have been some efforts to define a standardized set of data elements and corresponding set of values to support interoperability both within and across EHR systems. For example, implementation guides associated with the HL7 Clinical Document Architecture [38, 39] include a general “social history observation” that can be used to represent alcohol use while openEHR includes archetypes for “Alcohol Consumption” and “Alcohol Use Summary” [40, 41]. Collectively, these standards specify the collection of elements such as status, method of use, substance (or type), amount, frequency, start date or age, and quit date or age. In addition, these standards specify particular values (e.g., “daily use,” “weekly use,” “irregular use,” and “no use” for frequency) and use of standard terminologies (e.g., Systematized Nomenclature of Medicine Clinical Terms [SNOMED CT] [42]).
In previous work, alcohol use information in clinical notes from multiple institutions as well as public health surveys (Behavioral Risk Factor Surveillance System [43], National Health and Nutrition Examination Survey [44], and National Health Interview Survey [45]) was analyzed to assess the adequacy of the aforementioned standards and inform potential enhancements [37]. The present study builds upon these previous efforts and suggests the need for additional elements (e.g., situation) and values (e.g., “monthly use” and “yearly use” for frequency). Future studies involving more extensive analysis of the EHR as well as other sources (e.g., alcohol use screening tools) could be used to further inform the development of standards for alcohol use documentation.
6. Conclusions
The overall goal of this study was to understand current alcohol use documentation in the EHR with a focus on use of free-text in the social history module. Based on the early findings, implications for improving the collection and use of alcohol use information in the EHR include enhancing the structured collection of the different aspects of alcohol use (e.g., frequency, amount, and status), informing user training, integrating decision support mechanisms, and contributing to existing standards for alcohol use documentation. Next steps include examining how alcohol use is documented in other parts of the EHR (e.g., clinical notes) and how documentation varies based on patient, provider, and clinic characteristics.
Acknowledgements
The authors thank Indra Neil Sarkar, PhD, MLIS for valuable comments on an earlier draft of this manuscript and Diantha Howard, MS for statistical assistance. This work was presented as a poster at the University of Vermont College of Medicine Scholarly Project Day on May 13, 2013. Research reported in this publication was supported in part by the National Library of Medicine of the National Institutes of Health under award number R01LM011364. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Clinical Relevance
The accurate and comprehensive collection of a patient’s alcohol use history is essential for supporting clinicians in the screening, assessment, and treatment of alcohol use disorders. As a first step, understanding current documentation practices in the EHR could contribute to guiding system enhancements, user training, integrated decision support tools, and standards for alcohol use documentation.
Conflicts of Interest
The authors declare that they have no conflicts of interest in the research.
Protection of Human Subjects
The study was performed in compliance with the World Medical Association Declaration of Helsinki on Ethical Principles for Medical Research Involving Human Subjects. Approval was obtained from the Institutional Review Board at the University of Vermont/Fletcher Allen Health Care and informed consent was waived.
References
- 1.Bouchery EE, Harwood HJ, Sacks JJ, Simon CJ, Brewer RD.Economic costs of excessive alcohol consumption in the U.S., 2006. American journal of preventive medicine 2011; 41(5): 516–524 [DOI] [PubMed] [Google Scholar]
- 2.Hasin DS, Stinson FS, Ogburn E, Grant BF.Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of general psychiatry 2007; 64(7): 830–842 [DOI] [PubMed] [Google Scholar]
- 3.Eckardt MJ, Harford TC, Kaelber CT, Parker ES, Rosenthal LS, Ryback RS, Salmoiraghi GC, Vanderveen E, Warren KR.Health hazards associated with alcohol consumption. JAMA : the journal of the American Medical Association 1981; 246(6): 648–66 [PubMed] [Google Scholar]
- 4.Bradley KA, Lapham GT, Hawkins EJ, Achtmeyer CE, Williams EC, Thomas RM, Kivlahan DR.Quality concerns with routine alcohol screening in VA clinical settings. Journal of general internal medicine 2011; 26(3): 299–306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jaworowski S, Raveh D, Golmard JL, Gropp C, Mergui J.Alcohol use disorder in an Israeli general hospital: sociodemographic, ethnic and clinical characteristics. The Israel Medical Association journal 2012; 14(5): 294–298 [PubMed] [Google Scholar]
- 6.Callahan CM, Tierney WM.Health services use and mortality among older primary care patients with alcoholism. Journal of the American Geriatrics Society 1995; 43(12): 1378–1383 [DOI] [PubMed] [Google Scholar]
- 7.Moyer VA, Preventive Services Task F. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: U.S. preventive services task force recommendation statement. Annals of internal medicine 2013; 159(3): 210–218 [DOI] [PubMed] [Google Scholar]
- 8.National Institute on Alcohol Abuse and Alcoholism. Helping Patients Who Drink Too Much: A Clinician’s Guide. [December 2013]; Available from:http://www.niaaa.nih.gov/guide [Google Scholar]
- 9.Willenbring ML, Massey SH, Gardner MB.Helping patients who drink too much: an evidence-based guide for primary care clinicians. American family physician 2009; 80(1): 44–50 [PubMed] [Google Scholar]
- 10.Bush K, Kivlahan DR, Mc Donell MB, Fihn SD, Bradley KA.The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Archives of internal medicine 1998; 158(16): 1789–1795 [DOI] [PubMed] [Google Scholar]
- 11.Babor T, Higgins-Biddle J, Saunders J, Monteiro M.The Alcohol Use Disorders Identification Test Guidelines for Use in Primary Care. 2001[December 2013]; Available from:http://whqlibdoc.who.int/hq/2001/WHO_MSD_MSB_01.6a.pdf [Google Scholar]
- 12.Smith PC, Schmidt SM, Allensworth-Davies D, Saitz R.Primary care validation of a single-question alcohol screening test. Journal of general internal medicine 2009; 24(7): 783–788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Friedmann PD.Clinical practice. Alcohol use in adults. The New England journal of medicine 2013; 368(4): 365–373 [DOI] [PubMed] [Google Scholar]
- 14.Cimino JJ.Improving the electronic health record--are clinicians getting what they wished for? JAMA : the journal of the American Medical Association 2013; 309(10): 991–992 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kim HM, Smith EG, Ganoczy D, Walters H, Stano CM, Ilgen MA, Bohnert AS, Valenstein M.Predictors of suicide in patient charts among patients with depression in the Veterans Health Administration health system: importance of prescription drug and alcohol abuse. The Journal of clinical psychiatry 2012; 73(10): e1269–e1275 [DOI] [PubMed] [Google Scholar]
- 16.Williams EC, Lapham G, Achtmeyer CE, Volpp B, Kivlahan DR, Bradley KA.Use of an electronic clinical reminder for brief alcohol counseling is associated with resolution of unhealthy alcohol use at follow-up screening. Journal of general internal medicine 2010; 25 (Suppl. 1): 11–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Seppa K, Lahtinen T, Antila S, Aalto M.Alcohol drinking among emergency patients – alcometer use and documentation. Alcohol and alcoholism 2004; 39(3): 262–265 [DOI] [PubMed] [Google Scholar]
- 18.Torti J, Duerksen K, Forst B, Salvalaggio G, Jackson D, Manca D.Documenting alcohol use in primary care in Alberta. Canadian family physician Medecin de famille canadien 2013; 59(10): 1128, e473–e474 [PMC free article] [PubMed] [Google Scholar]
- 19.Polednak AP.Documentation of alcohol use in hospital records of newly diagnosed cancer patients: a population-based study. The American journal of drug and alcohol abuse 2007; 33(3): 403–409 [DOI] [PubMed] [Google Scholar]
- 20.Bell J, Kilic C, Prabakaran R, Wang Y, Wilson R, Broadbent M, Kumar A, Curtis V.Use of electronic health recoprds in identifying drug and alcohol misuse among psychiatric in-patients. The Psychiatrist 2013; 37: 15–20 [Google Scholar]
- 21.Freedy JR, Ryan K.Alcohol use screening and case finding: screening tools, clinical clues, and making the diagnosis. Primary care 2011; 38(1): 91–103 [DOI] [PubMed] [Google Scholar]
- 22.Clifford A, Shakeshaft A, Deans C.Training and tailored outreach support to improve alcohol screening and brief intervention in Aboriginal Community Controlled Health Services. Drug and alcohol review 2013; 32(1): 72–79 [DOI] [PubMed] [Google Scholar]
- 23.Lapham GT, Achtmeyer CE, Williams EC, Hawkins EJ, Kivlahan DR, Bradley KA.Increased documented brief alcohol interventions with a performance measure and electronic decision support. Medical care 2012; 50(2): 179–187 [DOI] [PubMed] [Google Scholar]
- 24.Middleton B, Renner K, Leavitt M.Ambulatory practice clinical information management: problems and prospects. Healthcare information management : journal of the Healthcare Information and Management Systems Society of the American Hospital Association 1997; 11(4): 97–112 [PubMed] [Google Scholar]
- 25.Linder JA, Schnipper JL, Middleton B.Method of electronic health record documentation and quality of primary care. Journal of the American Medical Informatics Association 2012; 19(6): 1019–1024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhou L, Mahoney LM, Shakurova A, Goss F, Chang FY, Bates DW, Rocha RA.How many medication orders are entered through free-text in EHRs?--a study on hypoglycemic agents. AMIA Annual Symposium proceedings / AMIA Symposium AMIA Symposium 2012; 2012: 1079–1088 [PMC free article] [PubMed] [Google Scholar]
- 27.Friedman C, Hripcsak G.Natural language processing and its future in medicine. Academic medicine : journal of the Association of American Medical Colleges 1999; 74(8): 890–895 [DOI] [PubMed] [Google Scholar]
- 28.Meystre SM, Savova GK, Kipper-Schuler KC, Hurdle JF.Extracting information from textual documents in the electronic health record: a review of recent research. Yearbook of medical informatics. 2008: 128–44 [PubMed] [Google Scholar]
- 29.Uzuner O, Goldstein I, Luo Y, Kohane I.Identifying patient smoking status from medical discharge records. Journal of the American Medical Informatics Association 2008; 15(1): 14–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang SJ, Bates DW, Chueh HC, Karson AS, Maviglia SM, Greim JA, Frost JP, Kuperman GJ.Automated coded ambulatory problem lists: evaluation of a vocabulary and a data entry tool. International journal of medical informatics 2003; 72(1–3): 17–28 [DOI] [PubMed] [Google Scholar]
- 31.Zheng K, Hanauer DA, Padman R, Johnson MP, Hussain AA, Ye W, Zhou X, Diamond HS.Handling anticipated exceptions in clinical care: investigating clinician use of ’exit strategies’ in an electronic health records system. Journal of the American Medical Informatics Association 2011; 18(6): 883–889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen ES, Melton GB, Burdick TE, Rosenau PT, Sarkar IN.Characterizing the use and contents of free-text family history comments in the Electronic Health Record. AMIA Annual Symposium proceedings / AMIA Symposium AMIA Symposium 2012; 2012: 85–92 [PMC free article] [PubMed] [Google Scholar]
- 33.Fletcher Allen Health Care. [January 2014]; Available from:http://www.fletcherallen.org/ [Google Scholar]
- 34.Mc Dowell SW, Wahl R, Michelson J.Herding cats: the challenges of EMR vendor selection. Journal of healthcare information management 2003; 17(3): 63–71 [PubMed] [Google Scholar]
- 35.Epic Systems Corporation. [January 2014]; Available from:http://www.epic.com/ [Google Scholar]
- 36.Chen ES, Manaktala S, Sarkar IN, Melton GB.A multi-site content analysis of social history information in clinical notes. AMIA Annual Symposium proceedings / AMIA Symposium AMIA Symposium 2011; 2011: 227–236 [PMC free article] [PubMed] [Google Scholar]
- 37.Melton GB, Manaktala S, Sarkar IN, Chen ES.Social and behavioral history information in public health datasets. AMIA Annual Symposium proceedings / AMIA Symposium AMIA Symposium. 2012; 2012: 625–634 [PMC free article] [PubMed] [Google Scholar]
- 38.Health Level Seven International (HL7). [December 2013]; Available from:http://www.hl7.org/ [Google Scholar]
- 39.Dolin RH, Alschuler L, Boyer S, Beebe C, Behlen FM, Biron PV, Shabo Shvo A.HL7 Clinical Document Architecture, Release 2. Journal of the American Medical Informatics Association 2006; 13(1): 30–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.openEHR. [December 2013]; Available from:http://www.openehr.org/ [Google Scholar]
- 41.openEHR Clinical Knowledge Manager. [December 2013]; Available from:http://www.openehr.org/ckm/ [Google Scholar]
- 42.SNOMED Clinical Terms (SNOMED CT). [December 2013]; Available from:http://www.ihtsdo.org/snomed-ct/ [Google Scholar]
- 43.Behavioral Risk Factor Surveillance System. [December 2013]; Available from:http://www.cdc.gov/brfss/ [Google Scholar]
- 44.National Health and Nutrition Examination Survey. [December 2013]; Available from:http://www.cdc.gov/nchs/nhanes.htm [Google Scholar]
- 45.National Health Interview Survey. [December 2013]; Available from:http://www.cdc.gov/nchs/nhis.htm [Google Scholar]


