Summary
Background
Homecare is an important and effective way of managing chronic illnesses using skilled nursing care in the home. Unlike hospitals and ambulatory settings, clinicians visit patients at home at different times, independent of each other. Twenty-nine percent of 10,000 homecare agencies in the United States have adopted point-of-care EHRs. Yet, relatively little is known about the growing use of homecare EHRs.
Objective
Researchers compared workflow, financial billing, and patient outcomes before and after implementation to evaluate the impact of a homecare point-of-care EHR.
Methods
The design was a pre/post observational study embedded in a mixed methods study. The setting was a Philadelphia-based homecare agency with 137 clinicians. Data sources included: (1) clinician EHR documentation completion; (2) EHR usage data; (3) Medicare billing data; (4) an EHR Nurse Satisfaction survey; (5) clinician observations; (6) clinician interviews; and (7) patient outcomes.
Results
Clinicians were satisfied with documentation timeliness and team communication. Following EHR implementation, 90% of notes were completed within the 1-day compliance interval (n = 56,702) compared with 30% of notes completed within the 7-day compliance interval in the pre-implementation period (n = 14,563; OR 19, p <. 001). Productivity in the number of clinical notes documented post-implementation increased almost 10-fold compared to pre-implementation. Days to Medicare claims fell from 100 days pre-implementation to 30 days post-implementation, while the census rose. EHR implementation impact on patient outcomes was limited to some behavioral outcomes.
Discussion
Findings from this homecare EHR study indicated clinician EHR use enabled a sustained increase in productivity of note completion, as well as timeliness of documentation and billing for reimbursement with limited impact on improving patient outcomes. As EHR adoption increases to better meet the needs of the growing population of older people with chronic health conditions, these results can inform homecare EHR development and implementation.
Keywords: Evaluation studies, technology evaluation, clinical information systems, patient care team, aged, homecare
1. Background
For older people who transition from hospital to home, homecare is an important and effective way of managing chronic illnesses using skilled nursing care in the home. Homecare engages providers from multiple disciplines to work together as a team, communicating as they provide care. However, unlike hospitals and ambulatory settings, clinicians visit patients at home at different times, independent of each other. As in hospitals and ambulatory sites, point-of-care electronic health records (EHR) in homecare are intended to enable clinicians’ access to the most current patient health information at the appropriate time during the clinical process.
Almost one-third (29%) of 10,000 homecare agencies in the United States (US) have adopted point-of-care EHRs [1]. Yet, relatively little is known about the growing use of homecare EHRs [2]. The few empirical studies available were qualitative involving homecare clinician focus groups [3]. We lack knowledge about similarities and differences between EHRs used in hospitals, physician offices, and homecare. Such comparisons will provide new knowledge related to both Meaningful Use and barriers and facilitators to homecare EHR adoption. Meaningful Use is objectives and measures to improve health outcomes and efficiency (including transition in care from hospital to home) that align with the American Recovery and Reinvestment Act of 2009 (ARRA) standards, certification criteria, and implementation specifications. ARRA provides financial incentives for hospitals and medical practices to adopt qualified and certified EHRs [4].
2. Objective
It is important to contribute to our understanding of EHR use in this unique and increasingly important setting. The study objective was to assess the impact of attaining efficiency and health goals of a point-of-care EHR in home care. To realize this objective, this study compared clinical documentation workflow, financial time-to-billing, and patient physiological and behavioral outcomes to evaluate its impact before/after point-of-care EHR implementation.
3. Methods
We investigated EHR impact on clinical process in homecare at clinician, patient, and organization (agency) levels using mixed methods. The point-of-care EHR deployment is the focusing event. In the quantitative portion (QUAN, capitalized to indicate primary data in mixed methods analysis), we used a pre/post study design embedded in a mixed methods study to measure EHR implementation impact. Quantitative data were collected retrospectively to assess the pre-implementation period (pre-period). At this time, clinicians completed documentation for billing that clerical staff then entered in the EHR (i.e., January 2008-February 2009). Quantitative data for post-implementation observations (post-period) were already available as the clinicians used the EHR at that time (i.e., August 2009-February 2010; March 2010-April 2011). Excluded from the analysis was the transition period when the EHR was being implemented team-by-team, as it was less comparable to the pre-period.
This study provided findings from a not-for-profit, Medicare-certified, skilled homecare agency. The agency, part of an academic, integrated health system, provided homecare services to 1,200 patients monthly in a five county urban/suburban area. Typical of homecare operations, patient visits included developing care plans, performing interventions, and documenting outcomes against the care plan. Medicare reimbursements were based on completed documentation of approximately 120 items in a Medicare mandated assessment instrument called the Outcome and Assessment Information Set (OASIS) [5] and congruence with care documentation. OASIS was designed to promote quality improvement in Medicare homecare through the collection of critical physiological, functional, cognitive, and emotional/behavioral indicators of health status at set intervals in the home-care episode [6, 7]. Four historic events occurred during the study period:
(1) management changes that spanned the pre-period through the first post-period;
(2) EHR implementation February 2009-August 2009 (i.e., transition period);
(3) a Medicare mandated move from OASIS B version to OASIS C which required software upgrade and extensive staff education; and
(4) implementation of an internal quality improvement team to review clinical documentation for completeness and accuracy February 2010 (i.e., second post-period).
3.1. EHR Implementation
The point-of-care EHR, RoadNotes, was a commercially available client-server application from the Cerner Corporation. The EHR functionality supported documentation of clinical information (e.g., assessment, intervention, outcome). However, care planning was not integrated with the documentation such that documentation (e.g., problems) did not populate the related care plan fields. Eight staff members supported the EHR.
Clinicians’ intended EHR use was as follows. Start their day at home; (i) connect laptop to agency’s server via a data card and view the day’s patient schedule, (ii) access information about entering a patient’s home or approaching a patient, and (iii) read team members’ messages. Travel to their patients’ homes: (i) find a space for laptop setup, and (ii) documented patient’s care in EHR. Return home; (i) connect laptop to the agency’s server and upload the patient’s EHR information, (ii) check the next day’s schedule, and (iii) read team members’ messages.
The point-of-care EHR replaced an office-based version in which non-clinical office staff entered information from clinicians’ paper records. Following point-of-care EHR implementation, these office staff members were re-deployed to other operational functions not related to clinical documentation (e.g., scheduling clinician visits).
3.2 Data Collection and Analysis
The following section outlines the collection and analysis of the study’s nine measures. Clinician-level EHR impact on clinical workflow (i.e., documentation completion timeliness) was assessed with EHR usage data (QUAN), EHR documentation completion data (QUAN), and clinician satisfaction with EHR impact on workflow using a clinician survey (QUAN), observation (Qual), and clinician interview (Qual) data. Organizational-level impact was assessed for productivity and finances. Productivity impact was assessed with EHR documentation completion data (QUAN) and payroll data (QUAN) which indicated the number of clinicians. Financial impact was assessed with financial system reimbursement data (QUAN). Patient outcome impact was assessed with EHR OASIS data that enabled comparison of patient outcomes (QUAN). Mixed methods analysis involved the researchers’ (PS,KB) sorting findings from each data source by theme, referring to the HIT Reference-based Evaluation Framework (HITREF) [8], and summarizing themes in a matrix. The HITREF is a comprehensive HIT evaluation framework firmly grounded in research evidence that identifies a range of HIT characteristics and dimensions to be measured. The HITREF provides 20 criteria, as shown in ►Figure 1, against which to evaluate HIT products and implementations.
Fig. 1.
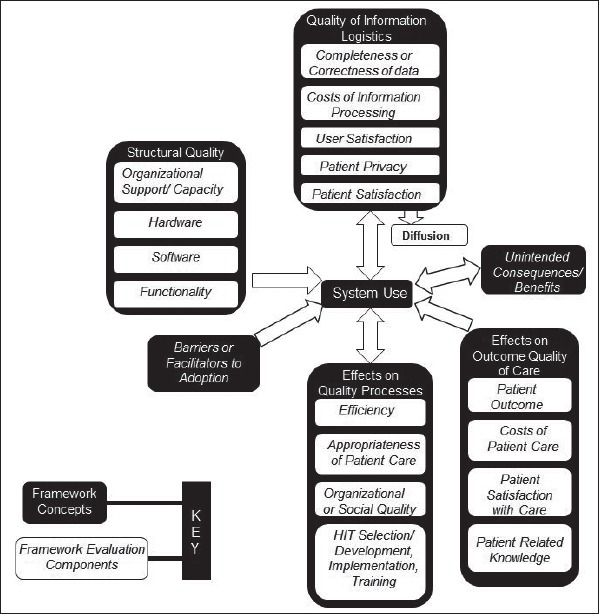
Conceptual model developed by Ammenwerth and de Keizer [24]. Modified and adapted by Sockolow [25]
The researchers and agency expert (MA) focused on the matrix to integrate the results from the quantitative and qualitative segments and identify how the qualitative themes contributed to understanding the quantitative findings.
Longitudinal analysis of EHR data was focused on three time periods – pre-period (duration 14 months) and two post-periods (durations 7 months and 14 months). The analysis methods were: (1) Analysis of Variance (ANOVA) for continuous outcomes; and (2) logistic regression for binary outcomes with adjustments for serial correlations over time and comparisons between the pre- and post-periods. Clinicians and patients in the post-periods were not matched to those in the pre-period. Differences or lack of differences between those time periods were interpreted as the impact of the EHR on the outcome of interest. Clinician turnover between time periods was low; therefore, the same clinicians were likely represented in each time period. For the longitudinal analyses and the survey response analysis, we entered and analyzed all quantitative data using SAS,[9] setting the significance level at alpha = 0.05.
3.2.1 Workflow Outcomes
The team measured two aspects of EHR impact on workflow: clinician perception and actual usage. The method for assessing clinician satisfaction is described here and was also used for the following financial and patient outcome measures, except where noted.
Clinician Satisfaction with EHR impact on workflow was measured using workflow-related items on a validated survey instrument, the EHR Nurse Satisfaction (EHRNS) survey. Each item had a six-point Likert-type response indicating the magnitude of agreement or disagreement with 22 items [10]. Researchers distributed the EHRNS for self-administration to clinicians during staff meetings and via postal mail during the second post-period. Due to limited resources, there was no follow up for non-respondents. Survey responses were analyzed for general associations and tests of trends between satisfaction and participant characteristics such as age, years of experience, and specific nursing profession. Specifically, cross-tabulations and odds ratios were generated followed by formal Chi-square or Fisher’s Exact tests. Concurrently the qualitative data from observations and interview responses related to workflow were analyzed using NVivo [11]. Using principles of thematic content analysis, data about (i.e., observations) and from (i.e., interview responses) clinicians were analyzed inductively to identify descriptive or topical categories. The HITREF was used to guide the initial organization of the categories as well as their development; however, HITREF use did not exclude possibilities for new organization. Researchers (PS, KB) coded each interview independently. They met regularly to compare their application of the categories and to resolve any differences in their analyses.
The researcher (PS) conducted observations during a patient visit when a clinician provided direct patient care. Clinicians selected for observation were chosen using work sampling [12] – sorting clinicians into categories by role, to assure that there were observations on each clinical discipline from each geographic team. Clinicians who were observed were also interviewed. The open-ended interview questions embodied the major themes identified in a previous study in a different setting [10]. Responses (anonymous) were recorded and transcribed. Clinicians were interviewed until saturation (i.e., responses offered no new information or a concept was heard at least three times) [13].
EHR Usage/Timeliness of Clinical Documentation was measured using de-identified EHR usage data for all clinicians who documented direct patient care in the EHR. Patient visit records included in the analysis contained a service date and units/hours. The agency had guidelines stating the maximum time to completion for the clinicians’ documentation. The homecare agency’s expectation was that clinician EHR use would reduce the proportion of charts with clinical documentation completions later than agency guidelines. To assess this hypothesis, the study included all clinicians who provided direct patient care and documented in the EHR (N = 137 at survey administration).
Clinician time-to-completion of clinical notes was computed as the time elapsed between the patient visit time and EHR note completion. Patient visit time was defined as user input time indicating when a clinician documented that he/she left the patient home, Leave Time. EHR note completion time was defined with the computer time-stamp, Attached Date. Due to the skewed data distribution, elapsed time-to-completion was calculated for each note, and a median time was calculated for each month. Late clinical documentation was treated as a continuous measure; late documentation was being out of compliance with agency guidelines (i.e., after 7 days in the pre-period or after 1 day post-period).
Statistical analysis entailed analyzing the proportion of clinicians who completed their documentation within guidelines. In order to estimate trends over time, longitudinal data analysis techniques were employed on the monthly time-to-completion and monthly proportion of records completed within guidelines.
We used compliance guidelines to indicate clinical significance. We compared the likelihood of documentation being in compliance in the pre-, first post-, and second post-periods for three groups: all clinicians, nurses, and physical and occupational therapists. We conducted the analysis with the Genmod procedure in SAS which applies a Generalized Estimating Equations method to account for the within-subject correlation [14].
Productivity related to clinician completion of documentation was computed for each study time period (i.e., pre-, first post-, second post-) as a ratio. The numerator was the total number of completed notes. The denominator was the total full time equivalent (FTE) contribution. An FTE of 1.0 is an employee who was paid for working full-time during the pay period: if the employee was paid for overtime, the FTE was greater than 1.0; if the employee was paid for less than full-time hours or worked part-time, the FTE was less than 1.0. The FTE contribution was computed as the average FTE during the study time period multiplied by the number of months in the study period. The rationale for the use of this calculation was to account for the months of missing data in the FTE data files.
3.2.2 Financial Claims
Reduced time to file Medicare claims combined with timelier clinician documentation was expected to result in increased, faster Medicare reimbursement. The financial system provided summarized data on days-to-final-claim, an internally reported metric for monitoring cash flow.
3.2.3 Patient Outcomes
EHR OASIS data was used to assess impact on patient outcomes by collecting data on critical physiological, cognitive, and emotional/behavioral health status indicators [5, 6]. Nurses or therapists used observation and information gathered directly from the patient or caregiver to collect OASIS data at admission, every 60 days, and at discharge, transfer, or death at home for every Medicare beneficiary. Patients with an (i.e., an admission and a reassessment, discharge, or transfer) in the study time period were included in the analysis. Where a patient had multiple admissions, reassessments, and discharges, the first admission or reassessment and the first discharge in the study time period were used in the calculation to minimize selection bias. Outcomes of interest were chosen because they reflected a realistic potential for homecare services’ impact. All outcomes used in the homecare-based quality improvement efforts were required by CMS [15], and they were consistently measured in the two OASIS versions used during the study’s timeframe. The specific OASIS items for this study were dyspnea, urinary tract infection, bowel incontinence, confusion, anxiety, cognitive functioning, and behavioral symptoms. Clinicians assessed OASIS outcomes as either single items measured on a Likert scale (anchored at asymptomatic) or yes/no. A logistic regression using the Genmod procedure in SAS [14] for binary outcome data was used to assess whether outcomes remained the same/improved, or declined. For each patient outcome, the two post-periods were compared to the pre-period.
3.2.3 Combined Quantitative/Qualitative Analysis
Final analytic activities delineated the content of specific coding categories and explored the linkages across the categories. All data for each category for clinicians, the organization, and patients were retrieved using NVivo and SAS. The data were then summarized in a matrix [16, 17] and organized using HITREF criteria.
4. Results
Each clinician was eligible to participate in the study with different levels of participation in each method. All were included in EHR documentation completion analysis (N = 137): only consented clinicians (n = 77) were observed (n = 8), surveyed (n = 71), and interviewed (n = 6). Agency staff were mostly women (90%) and mostly Caucasian (71%) with a minority who were African-American (20%). All de-identified patient data were included in the patient outcome analysis.
4.1 Workflow Outcome
4.1.1 Clinician Satisfaction with EHR Impact on Workflow
Of the 137 clinicians invited to participate in the study, 71 (52%) completed surveys. Respondents had a median of 21 years work experience in healthcare and a median age of 49 years; 88% were women, 54% were nurses, 34% physical therapists, 10% occupational therapists, 1% social workers, and 1% speech pathologists. Some respondents (35%) had previous EHR experience outside the research site, averaging 3 years of prior EHR experience. Respondents self-rated their computer skills as average.
Responses to survey items related to EHR impact on workflow are reported here. All survey items responses are reported elsewhere [18]. Survey responses ranged from Strongly Disagree (0) indicating most dissatisfied to Strongly Agree (5) indicating most satisfied. Average survey scores, with the standard deviations (SD) are provided as mean scores where the distribution is normal, and as median scores otherwise. Clinicians reported they were satisfied with the Completeness/Correctness of Data (Item 6; 3.7 median, SD 1.1) as well as EHR impact on Team Communication (Item 11; 4.0 median, SD 1.0) as shown in ►Table 1.
Table 1.
Survey, Observation, Interview, and EHR Data Analysis Results of Selected HITREF Workflow and Patient Outcome Criteria
| HITREF Criteria |
EHRNS Survey (Dissatisfaction: 0–2.5; Satisfaction: 3.5–5) |
Observation | Interview (% of all responses) |
EHR Data Analysis |
|---|---|---|---|---|
| Quality of data | Completeness/Correctness of Data (Item 6): mean 3.7, SD 1.1 |
Documented as discrete data elements with some free text input | 5%: satisfaction: incomplete data: medication, hospital stay; satisfied with data timelines | Documentation 19 times more likely to be in compliance fin the 1st post-period compared to the pre-period |
| Team communication | (Item 11) median 4.0, SD 1.0 |
Team communication via EHR | 22%: satisfaction: EHR facilitated communication, similar to in-person communication | Not applicable |
| Impact on patient outcomes | Patient safety (Item 10) mean 3.4, SD 1.1; Patient outcome (Item 12) mean 3.4, SD 1.2 |
Display of most recent blood pressure reading | 1%: neutral: dissatisfaction about EHR use taking time away from patient care related to patient care | No discernable impact on physiological indicators; impact on some behavioral indicators |
Of the 77 clinicians who consented, we purposefully selected 26 to be observed (34%) until we observed 8 clinicians (10%) to meet our goal of representing each team and clinical role; 18 clinicians refused to be observed or did not reply to email requests. Clinicians observed were men and women who were nurses, physical therapists, and occupational therapists. Their ages ranged from mid-twenties with under 5 years of healthcare experience to middle-aged with greater than 10 years of experience.
Clinician observations were conducted as they documented in the EHR in the patient home during the visit or on paper and later updated the EHR. Clinicians were observed recording the majority of EHR data in pull-down menus (e.g., blood pressure); providing free text input only to the narrative visit note; and incorporating previous EHR blood pressure information in their care decisions. Although nurses and therapists documented in separate areas of the EHR, they were observed accessing each other’s documentation. Clinician EHR communications were observed among and between clinical roles.
Clinicians were satisfied with Completeness/Correctness of Data (Item 6; 3.7 mean, SD 1.1). PS interviewed four nurses and two therapists. Completeness/Correctness of Data accounted for 5% of comments, with most comments about completeness and timeliness of data. Overall clinicians were satisfied. However, some comments indicated dissatisfaction with incomplete medication and hospital stay information. In addition, there were comments about incomplete start-of-care documentation, especially when originated by a nurse opening the case, but not the nurse performing follow-up care. Interview responses (22% of comments) also indicated satisfaction with Team Communication. Respondents claimed the EHR facilitated team communication and that communication via the EHR was similar to in-person communication.
4.1.2 EHR Usage/Timeliness of Clinician Documentation Completion
Every clinical discipline and every staff clinician who provided and documented patient care used the point-of-care EHR during the post-periods. Clinicians completed their notes sooner relative to the patient visit during the post-periods as compared to the pre-period. Furthermore, there was an increase in the number of notes documented each month due to increasing census. In the 14-month pre-period, 14,563 notes were documented. The proportion of clinicians who were in compliance pre-period ranged between 0 and 30%, as indicated on ►Figure 2. The mean hours to completion in the pre-period oscillated between 600 and 1,200 hours. Following implementation, 56,702 notes were completed in the 7-month first post-period and 168,782 notes completed in the 14-month second post-period. The proportion of documents completed within 1 day rose in a random walk upward from 50% to above 90%, with mean hours to completion moving from 24 in the first post-period to 10 hours in the second post-period.
Fig. 2.
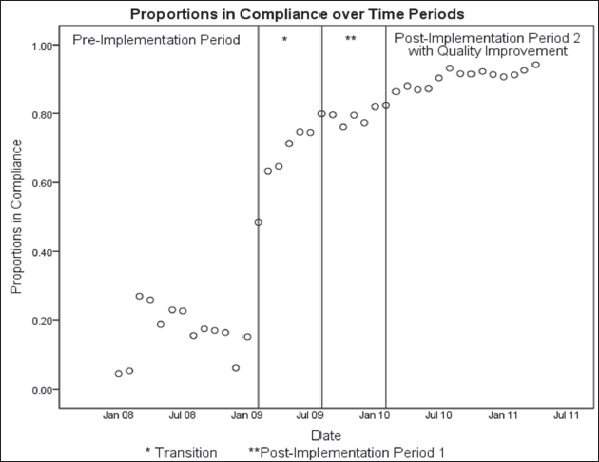
Proportion of Documents Completed Within the Compliance Guidelines (i.e., 7 days in Pre-period, 1 day in Post- periods) During the Study Period
Keeping in mind the different compliance guidelines in the pre- and post-periods, documentation was significantly (p<0.01) more likely to be in compliance for a post-period compared to the pre-period as shown in ►Table 2. Comparing the first post-period to the pre-period, documentation was about 19 times as likely to be in compliance and was statistically significant.
Table 2.
Multivariate Logistic Regression Odds Ratio of Compliance with Each Time Period’s Documentation Guidelines by Clinical Role (Odds Ratio [95% CI; p-value])*
| Clinical Role | 1st Post- vs. Pre- | 2nd Post- vs. Pre- | 2nd Post- vs. 1st Post- |
|---|---|---|---|
| All clinicians | 18.8 (17.9–19.7; p<0.001) |
44.4 (42.4 – 46.5; p<0.001) |
2.4 (2.3–2.4; p<0.001) |
| Nurses | 15.4 (14.6–16.2; p<0.001) |
35.4 (33.8–37.2; p<0.001) |
2.3 (2.2–2.4; p<0.001) |
| Therapists | 114.7 (89.5–147.0; p<0.001) |
269.3 (210.4–344.7; p<0.001) |
2.3 (2.2–2.5; p<0.001) |
*n = 14,563 notes in pre-period; n = 56,702 notes in post-period 1; n = 168,782 notes in post-period 2
In the pre-period, productivity related to documentation completion was 12.38 completed notes per FTE contribution. Following EHR implementation, productivity in the first post-period was 95.76 and productivity in the second post-period was 127.06 per FTE contribution.
4.2 Financial Claims
4.2.1 Clinician Satisfaction with EHR Features Related to Time to Generate Financial Claims
Clinicians did not remark in interviews about the EHR impact on reimbursement or patient care costs. Clinicians were observed using two EHR functions that impacted outcomes related to cost. Clinicians documented the date/time of the patient visit at the point-of-care. This function supported scheduling patients and staff and enabled the agency to allocate clinical resources more efficiently. The function also ensured that each patient visit had a valid start time as required for Medicare reimbursement. Also, a clinician was observed accessing the number of visits allowable by the patient’s insurance to plan the patient discharge. The agency’s finances have depended on clinicians’ providing care within the reimbursable number of visits.
4.2.2 Time to Filing Financial Claims
The number of days required to process clinician documentation into final claims oscillated between 40 and 100 days in the pre-period and between 100 and 30 days in the first post-period; they plateaued at under 20 days in the second post-period as shown in ►Figure 3. This substantial decrease in the second post-period coincided with implementation of the quality improvement team, which reviewed completed clinical documentation for completeness and accuracy. The peak and trough remained unexplained by financial administrators. Considering that the number of staff who processed claims was fixed, the number of days to final claim may have been impacted by increased or decreased volumes of claims to process. However, in the pre-period, the Medicare census remained relatively steady varying from 400 to 500 patients. Following implementation, the Medicare census began to increase toward 700 patients, while days to final claim fell, as shown in ►Figure 3.
Fig. 3.
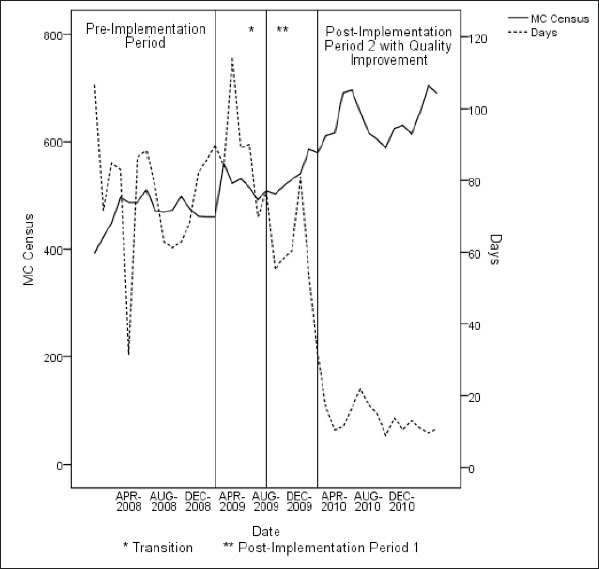
Trends in Medicare Census (MC) and Elapsed Days to Filing of Final Claim During Pre-EHR Implementation, Transition, Post-EHR Implementation, and Post-EHR Implementation with Quality Improvement Periods
4.3 Patient Outcomes
4.3.1 Clinician Satisfaction with EHR Impact on Patient Outcomes
Clinicians were neither satisfied nor dissatisfied with EHR impact on either Patient Safety (Item 10; 3.4 mean, SD 1.1) or Patient Outcome (Item 12; 3.4 mean, SD 1.2). Interview responses were few (1% of responses) and mostly neutral. One comment expressed dissatisfaction about EHR use taking time away from patient care.
4.3.2 EHR OASIS Data
OASIS assessment records for 31,363 patients and 69,932 assessments (78% of the data) were included in the analysis. The 7-month pre-period and the 14-month first post-period each had approximately 20% of the patients and assessments. Less than 2% of the health status indicators data was missing from assessments; this likely did not introduce bias into the analysis.
For all the selected physiological conditions, the assessed patient population was neither more nor less likely to remain the same or improve in health outcome in the first post-period as compared to the pre-period (e.g., odds ratio near 1.0) as shown in ►Table 3. The odds ratio indicating patients stayed the same or had an improvement in dyspnea was statistically significant, although probably not clinically significant and may be a consequence of large sample size. Patients assessed for selected cognitive (i.e., level of alertness, orientation, comprehension, concentration, and immediate memory for simple commands.) or behavioral conditions (i.e., anxiety or confusion) were more likely to stay the same/improve in health outcome. All other behavioral, cognitive, and psychiatric conditions remained unchanged. Comparing the post-periods, patients were likely to stay the same/ improve, except those with urinary tract infections. In each comparison, an indicator (i.e., dyspnea in the first comparison, behavioral assessment in the second comparison), while statistically significant, is probably not clinically significant and may also be a consequence of large sample size.
Table 3.
Odds Ratio of Patient Outcomes Staying the Same or Improving Between Study Periods, Comparing Initial and Discharge Assessments
| Physiological/Behavioral Condition | 1st Post- vs. Pre-OR (95% CI; p-value) |
2nd Post- vs. Pre-OR (95% CI; p-value) |
2nd Post- vs. 1st PostOR (95% CI; p-value) |
|---|---|---|---|
|
Dyspnea (Shortness of Breath) (n = 1,419 patients) |
1.1 (1.02,1.36; p = 0.028) |
2.7 (2.3, 3.1; p<0.0001) |
2.3 (1.9, 2.7; p<0.0001) |
|
Bowel Incontinence Frequency (n = 455) |
1.0 (0.8,1.2; p = 0.8) |
6.6 (4.8, 9.0; p<0.0001) |
6.8 (4.9, 9.4; p<0.0001) |
|
Urinary Tract Infection (n = 148) |
1.0 (0.6, 1.7; p = 0.9) |
0.8 (0.5, 1.2; p = 0.2) |
0.8 (0.5, 1.3; p = 0.3) |
|
Anxiety (n = 1,955) |
1.6 (1.4, 1.8; p<0.0001) |
2.4 (2.1, 2.6; p<0.0001) |
1.5 (1.3, 1.7; p<0.0001) |
|
Awareness (n = 938) |
2.1 (1.7–2.6; p<0.0001) |
4.0 (3.35, 4.72; p<0.0001) |
1.9 (1.5, 2.3; p<0.0001) |
|
Behavior Assessments (n = 9,564) |
1.0 (0.96, 1.13; p = 0.3) |
1.2 (1.10, 1.25; p<0.0001) |
1.1 (1.05,1.21; p = 0.0009) |
|
Confusion (n = 1,141) |
1.9 (1.6, 2.3; p<0.0001) |
3.3 (2.8, 3.8; p<0.0001) |
1.7 (1.4, 2.1; p<0.0001) |
4.4 Mixed Methods Results
Findings related to workflow and financial outcomes were convergent indicating positive EHR impact. Clinicians used the EHR universally, including functions that supported completeness of documentation, as well as clinician scheduling and reimbursement. Clinicians were satisfied with EHR impact on workflow characteristics. The EHR had a positive impact on timeliness of documentation and billing, shown in ►Figure 3.
Patient outcomes findings were also convergent, indicating minimal EHR impact. Clinicians used functions that supported workflow related to team communication and patient care. They were satisfied with EHR impact on team communication and had a neutral perception of EHR impact on patient outcomes. EHR impact on patient outcomes was limited to positive impact on some behavioral measures (►Figure 4).
Fig. 4.
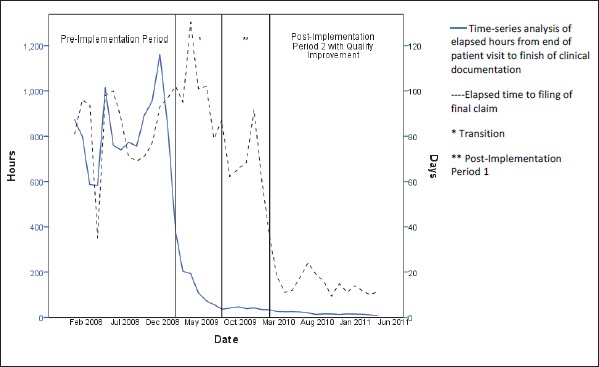
Elapsed Time to Completing Clinical Documentation and Filing Reimbursement Claim Before and After Electronic Health Record Implementation
5. Discussion
In this paper, we have presented a homecare EHR impact evaluation on timeliness of clinician documentation and agency reimbursement for patient care and on patient outcomes. In searching the literature, we have not identified any comparable prior studies of home health EHR systems. Clinicians communicated and demonstrated that they were satisfied with EHR impact on workflow and financial outcomes. Clinicians documented at the point-of-care, as intended, and also documented after the patient visit.
Implementation of the point-of-care EHR improved timeliness of clinical documentation completion resulting in greater compliance with timeliness guidelines compared to prior paper documentation, as well as timelier Medicare reimbursement. However, clinicians’ perception of EHR impact on patient outcomes was neutral, and EHR impact on patient outcomes was minimal.
Clinicians’ point-of-care EHR use enabled elimination of paper documentation processes and provided real-time, actionable data for managing compliance with documentation timeliness guidelines. The EHR enabled managers to have tools to improve clinician accountability and productivity, although documenting in the EHR required more clinician time than documenting on paper. Increased clinician accountability and productivity yielded a nearly 10-fold increase in documentation. The FTE figures indicated that this improvement could not be attributed solely to an increase in staff
In addition to enabling sustained process improvement in clinical documentation timeliness, clinician EHR use ensured the visit was reimbursable. By adding the documentation quality improvement team during the second post-period, billing was further improved. The combined effect on clinical documentation timeliness was to reduce the number of days required to create a final reimbursement bill improving agency cash flow even as census was increasing. The sustained increase in documentation timeliness suggests that EHR implementation can be credited with enabling this process improvement[19] by providing the quality improvement team with timely feedback thereby affording a return on the agency’s investment in EHR.
Real-time EHR data availability supported clinicians in their provision of homecare and communication among team members. The point-of-care EHR, when used as intended, displayed patient visit documentation to clinicians as they made clinical care decisions. Despite access to timelier point-of-care documentation, the EHR had minimal effect, consistent with HIT systematic reviews [20, 21]. We suggest that the improvement in selected patient outcomes may be due to the difference in the two versions of OASIS instrument used during the study. Although we carefully selected outcome measures that remained the same across the versions, the later version had more items that assessed cognitive impairment and depression. This emphasis, combined with increased education about depression, may have triggered nurses to be more aware of behavioral symptoms and to provide better documentation. The additional OASIS behavioral questions may have confounded the analysis resulting in improvement in some outcomes due to improved documentation.
We do not believe the change between versions in the format of the selected OASIS items impacted the patient outcome results. Four of the seven questions had changes in OASIS C, and these changes were semantic in nature (e.g. add “within the last 14 days,” drop “never,” add “cognitive” and “psychiatric” to the behavior assessment question). In addition, the lack of an association between a changed item and the presence or absence of a change in patient outcomes indicates that the change in items between versions was not related to patient outcome findings. However, it is possible that other patient outcomes, not selected due to substantive differences in questions between OASIS versions, might be more sensitive to EHR impact on clinical process.
Changes related to the substantive improvement in patient outcomes in the second post-period may be attributable to: 1) the implementation of the documentation quality improvement team; and 2) the use of analytic software which replaced the previous manual process. The software looked for: (i) inconsistencies within an OASIS document (e.g., both ‘no need for ambulatory assistance’ and ‘need help toileting’ documented), (ii) inconsistencies between OASIS documents in an episode of care, and (iii) significant declines between a start of care and a subsequent assessment. The software prioritized cases that the quality improvement team members reviewed with clinicians, resulting in improved documentation of patient outcomes.
The finding that improvement across all patient outcomes was not detected between the pre-period and the first post-period is consistent with the most recent systematic review. This review underscored the need for better interventions for the homecare population [22]. The lack of improvement is likely due to the tendency of homecare patients to be elderly and to have multiple chronic conditions with a natural downward trajectory.
We also suggest that the absence of features intended to support better nursing care and decision making (e.g., standardized care plans, guidelines, automated alerts) [2, 23] may have decreased EHR impact on patient outcomes. However, the evidence for this suggestion is weak [21].
5.1 Study Strengths and Limitations
This study has the potential to stimulate more comprehensive informatics research in homecare by increasing knowledge about EHR impact on clinical process. A strength is its generalizability to homecare agencies that implement a leading commercial EHR, as the EHR was similar in functionality to other commercially available homecare EHRs. However, this generalizability may be specific to the software and urban/suburban homecare agencies. Given the lack of a comparison group, the research design may not have controlled sufficiently for other parallel changes at the site. We were able to control for patient demographic differences in the analyses. However, we were unable to control for changes in patient acuity. The absence of homecare workflow studies is a challenge to interpreting these results within the larger context of homecare agencies in general. Looking forward, given an increasingly aging US population, findings regarding the impact of a point-of-care EHR offer insights about use of real-time actionable EHR data. This EHR data could support increased clinician productivity and accommodate increased patient census in community-based healthcare settings.
6. Conclusion
This is the first known study of EHRs in homecare to provide evidence-based findings about EHR use. These findings indicate that EHR use: (1) significantly improved the timeliness of clinical documentation and billing for reimbursement; and (2) had limited impact on improving patient outcomes. EHR data enabled administrators to manage clinician documentation timeliness and improve the workflow process thereby increasing clinician productivity with no increase in staff to care for increasing number of patients. While these findings are consistent with those from studies in hospitals, further study is warranted to confirm our findings in larger study populations and other study settings. These evaluation results can inform EHR development and implementation in home-care settings as EHR adoption increases to better meet needs of the growing population of older people with chronic health conditions.
Acknowledgements
We thank Barbara Granger for her editorial assistance and John Aleckna of Aleckna and Associates, LLC for his patience and programming expertise in extracting the data. We also thank the clinicians who participated in the study and the agency management who enabled the team to conduct this research. This work was supported by the Agency for Healthcare Research and Quality grant number 1R21HS021008– 01 and the Drexel University Career Development Award.
Footnotes
7. Clinical Relevance Statement
Implementation of the homecare point-of-care EHR resulted in greater compliance with timeliness guidelines compared with prior paper documentation, as well as timelier Medicare reimbursement. The EHR enabled managers to have tools to improve clinician accountability and productivity, which yielded a nearly 10-fold increase in notes documented, as well as ensuring the visit was reimbursable. Real-time EHR data availability supported clinicians in their provision of homecare and communication among team members, although there was little impact on patient outcomes.
Conflict of Interest
The authors declare that they have no conflicts of interest in the research.
Human Subjects Protection
The Institutional Review Boards of Drexel University and the University of Pennsylvania approved the study.
References
- 1.Resnick HE, Alwan M.Use of health information technology in home health and hospice agencies: United States, 2007. JAMIA 2010;17: 389–395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Staggers N, Weir C, Phansalkar S.Patient Safety and Health Information Technology: Role of the Electronic Health Record. 2008; Available at:http://origin.www.ahrq.gov/qual/nurseshdbk/docs/StaggersN_PSHIT.pdf Accessed January 11, 2010 [PubMed] [Google Scholar]
- 3.Stolee P.The use of electronic health information systems in homecare: facilitators and barriers. Home Healthcare Nurse 2010; 28: 167. [DOI] [PubMed] [Google Scholar]
- 4.American Recovery and Reinvestment Act. ARRA 2009Jan 9; PL111–5 [Google Scholar]
- 5.OASIS. 2011; Available at:www.cms.gov/OASIS/ Accessed February 16, 2012 [Google Scholar]
- 6.Schlenker RE, Powell MC, Goodrich GK.Initial home health outcomes under prospective payment. Health Serv Res 2005; 40: 177–193 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shaughnessy PW, et al. Improving patient outcomes of home health care: findings from two demonstration trials of outcome-based quality improvement. J Am Ger Soc 2002; 50: 1354–1364 [DOI] [PubMed] [Google Scholar]
- 8.Sockolow PS, Weiner JP, Bowles KH, Abbott P, Lehmann HP.Advice for decision makers based on an electronic health record evaluation at a Program for All-inclusive Care for Elders site. Appl Clin Inf 2011; 2: 18–38 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.SAS Institute Inc. SAS/STAT® 9.2 User’s Guide. Cary, NC: SAS Institute; 2008 [Google Scholar]
- 10.Sockolow PS, Weiner JP, Bowles KH, Lehmann HP.A new instrument for measuring clinician satisfaction with electronic health records. Comput Inform Nurs 2011; 29: 574–585 [DOI] [PubMed] [Google Scholar]
- 11.QSR International. NVIVO. 2008;8 [Google Scholar]
- 12.Sittig DF.Work-sampling: a statistical approach to evaluation of the effect of computers on work patterns in healthcare. Methods Inf Med 1993; 32: 167–174 [PubMed] [Google Scholar]
- 13.Burns N, Grove SK.The Practice of Nursing Research. 7th ed Philadelphia: W. B. Saunders; 2013 [Google Scholar]
- 14.Allison PD.Logistic regression using the SAS system: theory and application. Cary: SAS Institute Inc.; 1999 [Google Scholar]
- 15.Twiss A, Pierce M, Schwien T, Ottersburg T, Khuc T.The effect of the prospective payment system on home health quality of care. 2004; Available at:http://oig.hhs.gov/oei/reports/oei-01-04-00160.pdf Accessed January 25, 2011 [Google Scholar]
- 16.Milles MB, Huberman AM.Qualitative data analysis: an expanded sourcebook. 2nd ed Thousand Oaks: Sage Publishers; 1994 [Google Scholar]
- 17.Deatrick J, Alderfer M, Knafl G, Knalf K.Identifying patterns of managing chronic conditions. Crane R, Marshall E, Families and health: interdisciplinary perspectives. Thousand Oaks: Sage, 2006: p.62–80 [Google Scholar]
- 18.Sockolow PS, Bowles KH, Adelsberger MC, Chittams JL, Liao C.Challenges and facilitators to adoption of a point-of-care electronic health record in home care. Home Health Care Services Quarterly 2013; 192: 939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Walker JM, Carayon P, Leveson N.EHR safety: the way forward to safe and effective systems. JAMIA 2008; 15: 272–277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lau F, Kuziemsky C, Price M, Gardner J.A review on systematic reviews of health information system studies. JAMIA 2010; 17: 637–645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Black AD, et al. The impact of eHealth on the quality and safety of health care: a systematic overview. PLOS Med 2011; 8: 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murtaugh C, Peng T, Totten A, Costello B, Moore S, Aykan H.Complexity in geriatric home healthcare. J Healthcare Qual 2009; 31: 34–43 [DOI] [PubMed] [Google Scholar]
- 23.Bakken S.Informatics for patient safety: a nursing research perspective. Annu Rev Nurs Res 2006; 24: 219–254 [PubMed] [Google Scholar]
- 24.Ammenwerth E, de Keizer N.An inventory of evaluation studies of information technology in health care – Trends in evaluation research 1982–2002. Methods Inf Med 2005; 44(1): 44–56 [PubMed] [Google Scholar]
- 25.Sockolow PS, Crawford PR, Lehmann HP.Broadening a general framework for evaluating health information technology through health services research evaluation principles. Methods of Medical Information 2012; 51(2): 122–130 [DOI] [PubMed] [Google Scholar]


